-
Medical journals
- Career
Can Visual Function Be Affected by an Open Foramen Ovale?
Authors: P. Výborný 1; J. Čmelo 2
Authors‘ workplace: Oční klinika 1. Lékařské fakulty Univerzity Karlovy a Ústřední vojenské nemocnice - Vojenské fakultní nemocnice Praha 1; Centrum neurooftalmológie, Bratislava 2
Published in: Čes. a slov. Oftal., 76, 2020, No. 6, p. 274-277
Category: Case Report
doi: https://doi.org/10.31348/2020/38Overview
The authors present a relatively rare finding of pathological changes in the visual field, the emergence of homonymous hemianopia, in connection with trauma and paradoxical embolism in a subsequently diagnosed open foramen ovale in a 56-year-old otherwise healthy patient. Cardiac source of embolism is a significant etiology of vascular embolization.
The important group is the so-called paradoxical embolism, which occurs when a blood clot (embolus) is carried from the venous side of circulation to the arterial side via foramen ovale patens, what can manifests as ischemic stroke. Foramen ovale patens becomes a risk factor for the stroke development only if there is a peripheral source of embolism and at the same time there is a hemodynamically significant right-left short circuit. Therefore, screening for the causes of cryptogenic stroke should include not only the detection of foramen ovale patens but also evaluation of the peripheral venous system, coagulation parameters and hemodynamic severity of a right-left shunt. Neuroophthalmological aspects related to the described issues are discussed.
Keywords:
open foramen ovale – paradoxical embolism – homonymous hemianopia
INTRODUCTION
Malfunctions of the visual field are a significant problem in medicine, the solution of which requires the essential co-operation of a number of clinical disciplines. In daily practice they are encountered most frequently by a general practitioner, internal medicine specialist, endocrinologist, ophthalmologist, neurologist, paediatrician or neurosurgeon. Differential diagnostics sometimes also presents problems even for experienced professionals, because it requires good knowledge of anatomy and physiology, as well as experience. This theme is also frequently used by examiners when verifying the knowledge and practical judgement of tested students on all levels of study of medicine. There is an abundance of academic literature dealing with this theme, and the sources are available. The presentation of a relatively rare finding of homonymous hemianopia in connection with an open foramen ovale is therefore a contribution to the general contexts and better known cases. In accordance with the Czech-Slovak character of the journal, the theme is presented in the view of a Slovak neuro-ophthalmologist and a Czech glaucomatologist.
Case report – course of pathology and description of available findings
Man aged 56 years with no serious ailments, not using medications, without manifestations of allergy, not adhering to any diet, no significant family medical history.
Work history: university educated, construction technician.
Three weeks ago the patient experienced a prickling sensation in the upper limbs, accompanied by sudden deterioration of both distance and near vision in both eyes, as well as a blunt headache. He was immediately hospitalised in the neurological department. The patient stated that a few days before the onset of the complaints he had sustained a blow from a concrete block in the region of the left ankle when working on a building site, with the subsequent formation of a pronounced haematoma, which was drained at a surgical outpatient department. Among other matters, an ocular consultation was indicated, with suspected glaucoma. At an ophthalmological examination at another centre, left-sided homonymous hemianopia was determined (Fig. 1). Central visual acuity was within the norm (vision in right eye 1.0 naturally, vision in left eye 1.0 naturally), the finding on the anterior and posterior segment of both eyes corresponds to age, optic media transparent, colour perception unaffected, normotension. A further comprehensive examination determined anomalous heart configuration, and embolisation of a blood clot into the central nervous system (CNS). A patent foramen ovale (PFO) was diagnosed, and a surgical solution was indicated and performed. The current therapy as of the date of examination is Fraxiparin, Detralex and Lecithin. Vision gradually subjectively improved, the patient still has difficulty distinguishing the left edges of objects.
1. Left-sided homonymous hemianopia (computer static perimetry) 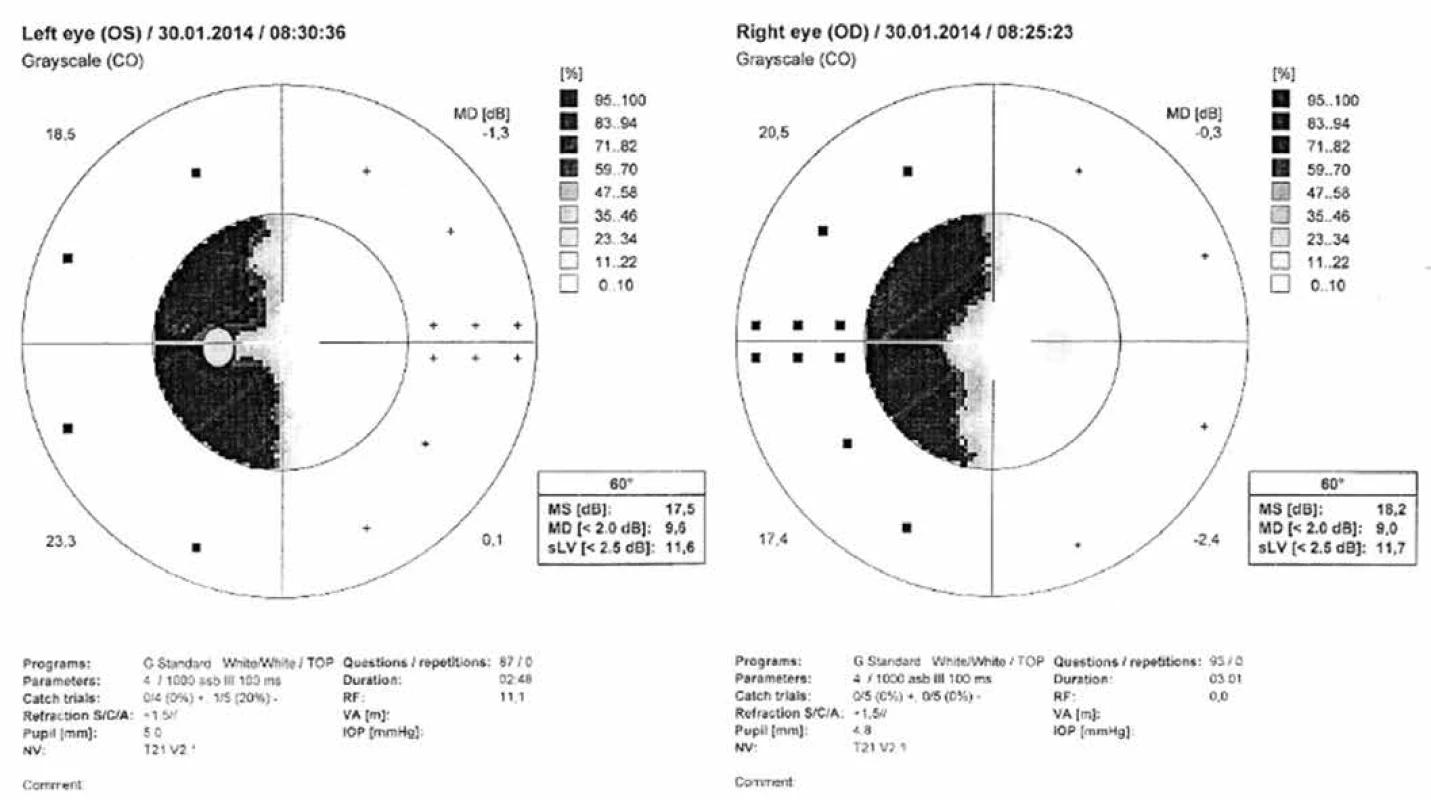
For a correct interpretation of the clinical finding in the case in question, it is necessary to understand the connected pathophysiological relations.
An open foramen ovale is significant for foetal blood circulation. Oxygenated blood flows through it from the lower hollow vein of the Eustachian valve from the left ventricle into the overall blood circulation. After birth, the foramen ovale closes anatomically during the first day of life in approximately 70 % of infants. A PFO is an opening in the interventricular septum, persisting postnatally. Mild form the defect in healthy adults may not be manifested whatsoever from a functional perspective in adults, because the incompletely grown valve closes the septum mechanically (persistent foramen ovale). Under normal circumstances, the pressure in the left ventricle is higher, and the pressure gradient is therefore directed from the left ventricle to the right. For blood to flow in the opposite direction an increase in pressure in the right ventricle and a reversal of the pressure gradient is required.
A paradoxical embolism is a particular type of embolism, in which embolisation of the thrombus into the arteries of systemic circulation takes place by means of a right-to-left cardiac shunt.
Blood clots from the deep veins of the lower limbs and from the pelvic veins may embolise first of all into the lungs, causing an increase of pressure in the right ventricle, and thereby facilitate a right-to-left shunt through the open foramen ovale. Even upon normal pressure in the right ventricle, a right-to-left shunt may intermittently occur, e.g. upon coughing, a Valsava manoeuvre or upon change of position. More frequent than embolisation of large blood clots is multiple embolisation of small blood clots with a size of a few millimetres, which are subject to spontaneous lysis in the pulmonary channel without greater clinical consequences. However, in the cerebral arterial channel embolisation may have severe consequences. A significant basic examination method upon suspicion of an embolisation stroke or transitory ischaemic attack is transesophageal echocardiography. It primarily demonstrates blood clots in the auricle of the left ventricle, in the left atrium and atherosclerotic plaques in the aorta. It is possible to evaluate right-to-left shunt according to the flow of echo-contrast micro-bubbles from the right ventricle into the left ventricle.
When considering changes of the visual field in dependency on the localisation of affliction in the CNS, it is necessary to keep in mind the following contexts. As a consequence of crossing of the nerve fibres in the optic chiasm, lesions localised retrochiasmally as a rule cause homonymous defects of the visual field, and therefore blind spots appearing in the same-sided halves of the visual field of both eyes. The congruence (identity) of blind spots increases in a direction from the optic tracts to the visual cortex. This is due to the arrangement of the nerve fibres in the individual parts of the visual pathway. The cause of left-sided homonymous hemianopia in the given case may be a lesion localised anywhere in the right retrochiasmal visual pathway – in the optic tract, in the corpus geniculatum laterale, in the optic radiations or in the primary visual cortex. Affliction of the right-sided upper parts of the optic radiations or the upper-right region above the fisura calcarina may cause left-sided lower homonymous quadrantanopia. For comprehensive information about possible further variants of changes of the visual field we present the following overview. Upon damage to the central part of the optic chiasm, damage is caused to the crossing nerve fibres, which leads to blind spots in the temporal parts of the visual fields of both eyes. These defects may be more or less symmetrical. Scotomas may occupy the entire temporal half of the visual field or only the upper and lower quadrants. Hypophyseal lesions are typified by bitemporal hemianopia in the upper quadrant, whereas by contrast, more pronounced lateral asymmetry and blind spots beginning in the lower temporal quadrants testify rather to non-hypophyseal origin (craniopharyngeoma, aneurysm of the circle of Willis, meningeomas, internal hydrocephalus). Upon damage in the region of the optic tracts, the findings on the perimeter of both eyes do not entirely overlap. In the case of lesions of the occipital visual cortex, blind spots in the afflicted halves of the visual field are practically identical. Lesions of the optic tracts are relatively rare, and as a rule cause contralateral homonymous hemianopia. Lesions of the corpus geniculatum laterale are usually linked with contralateral homonymous hemianpia – although less common defects (sectoranopia) may also appear [1,2,3,4,5].
View of neuro-ophthalmologist
A cardiac source of embolisation (CSE) is a significant cause of vascular embolisation. Today the most common CSE is ventricular fibrillation. Previously the most common causes included for example rheumatic endocarditis, valve defects, conditions following myocardial infarction or following replacement with artificial hart valves, often without sufficient anticoagulation therapy. A cardiac source of embolisation may also be the benign heart tumour myxoma, especially in young patients who do not have any other clear reason for embolisation. A significant group of CSE is so-called paradoxical embolisation, which occurs in the case that a blood clot (embolism) enters the arterial system from the venous system via the PFO, which may be manifested as an ischaemic stroke [6]. Sudden strokes can be divided schematically into ischemic brain lesions (IBL), transient ischemic attacks (TIA) and haemorrhagic strokes (subarachnoid and parenchymal haemorrhage). The cause of sudden stroke may be manifest (an etiopathogenetic connection can be found) or cryptogenic (etiology cannot be determined). PFO is the cause of cryptogenic sudden stroke in up to 40-50 % of patients aged under 55 years. In patients aged over 65 years, even if PFO at this age is much rarer, there is a 3x higher risk of IBL and TIA, which is probably connected with the size of the PFO [8]. PFO becomes a risk factor for the occurrence of sudden stroke only in cases where there is a peripheral source of embolisation and at the same time a haemodynamically significant right-to-left shunt. For these reasons, screening for the cause of cryptogenic sudden stroke should include not only detection of PFO, but also examination of the peripheral venous system, coagulation parameters and assessment of the haemodynamic severity of the right-to-left shunt [9]. However, in certain cases an embolus may form also upon stagnation of the blood flow directly in the PFO, or in the case of heart arrhythmias also directly in the left atrium [9]. The only evidence of an etiopathogenetic connection of PFO with IBL is a finding of a thrombus in transit wedged in the PFO or in the right atrium, often with the presence of further pathological structures. The diagnostic choice is echocardiographic transthoracic and transoesophageal examination with the application of contrast, and also transcranial ultrasonography. Sudden stroke etiopathogenetically linked with PFO was first described by Cohnheim in 1877, in a case report of a young female patient [8]. It was only with the advent of contrast echocardiography that it became possible to recognise the connection between sudden stroke and PFO mainly in young patients. The aim of the examination by a neuro-ophthalmologist in sudden stroke is to diagnose an occlusive pathology of the eye, or with the aid of thorough and repeated examination of the visual field to “guide” the neurologist to the possible localisation of the lesion (Table 1). Imaging techniques (magnetic resonance, computer tomography) precisely detect the damaged area, but with the aid of perimetry it is possible to observe the dynamic of changes continuously. PFO is also a risk factor in migraines. PFO is associated with migraines with aura, but not with migraines without aura. Meta-analyses have demonstrated that PFO appears in as many as 55 % of patients with migraines with aura, and has a substantially lower incidence (19 %) in patients without migraines [7].
1. Clinical manifestation of stroke in connection with localisation of affliction 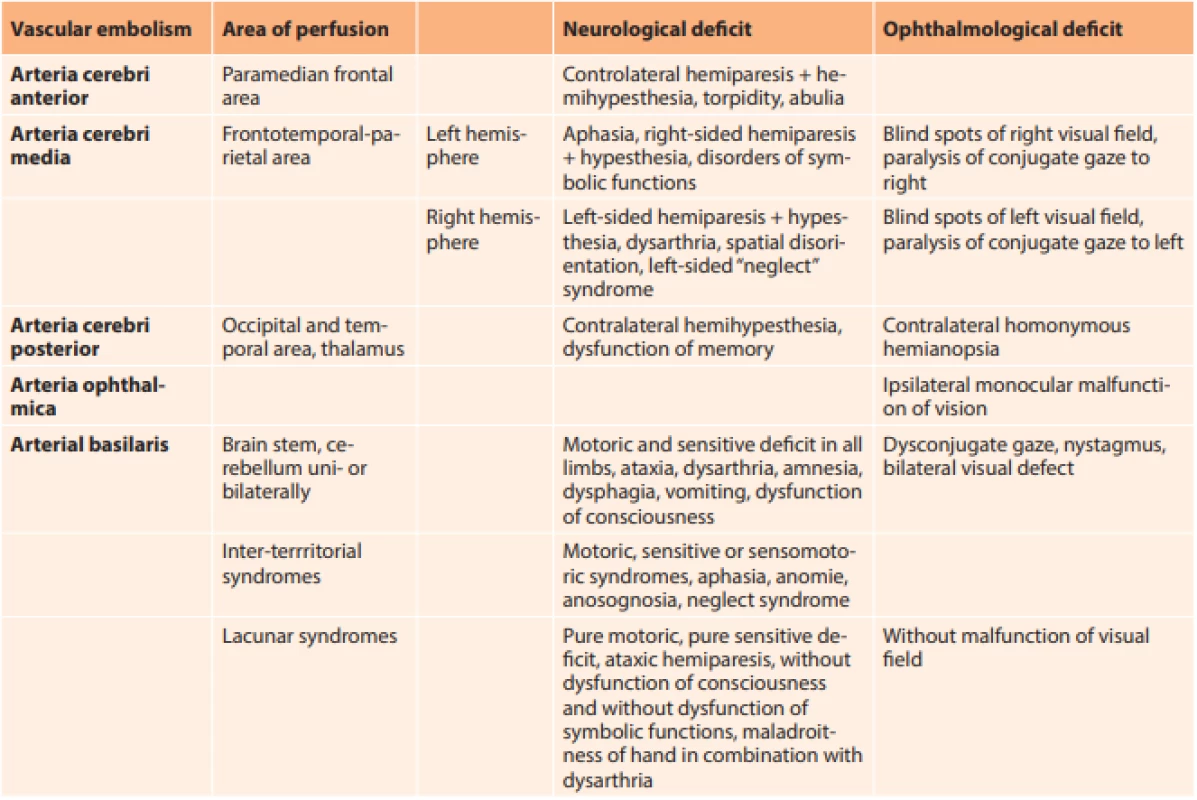
Therapy
In persons with a medical history of transitory ischemic attack or central stroke, who at the same time manifest right-to-left shunt upon PFO, four types of treatment are recommended: surgical closure or catheterising closure of the PFO, anti-aggregation or anticoagulation therapy.
CONCLUSION
The patient has ceased to attend follow-up ophthalmological examinations, because he does not expect any benefit from further observation and considers his condition to be stable. Due to the lack of co-operation on the part of the patient, we therefore do not have any further retrospective or prospective data available from the health documentation on the given case. In addition to other complications, PFO may also cause a significant deterioration of visual functions. The frequency of occurrence of ocular complications is relatively rare, but significant for the patient. Functional changes may significantly deteriorate the patient’s quality of life. In connection with changes of the visual field it is necessary to emphasise especially change of capability to drive motor vehicles and to perform certain professions. It is also necessary to mention the fact that in everyday clinical ophthalmological practice, upon interpretation of patients’ subjective complaints (headache, flashes, deterioration of vision, changes in the visual field), too often we continue to encounter a lax diagnosis of “suspected glaucoma” or “normal tension glaucoma”, without the presence of the corresponding morphological and functional changes, and without an endeavour to investigate further to determine a correct, even if in some cases rare, diagnosis.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company. The study has not been submitted to any professional journal or printed elsewhere.
The authors of the study further declare that the study has not been submitted for printing to any other journal or printed elsewhere, with the exception of congress abstracts and recommended procedures.
Sources
1. Popelová J. Otevřené foramen ovale a paradoxní embolizace – antiagregační léčba, antikoagulační léčba. Remedia online 2003 (2). Available from: www.remedia.cz.
2. Reif M. Foramen ovale patens v neurologii. Neurol. pro praxi. 2007;3 : 175-178.
3. Riedel M. Paradoxní embolie a kryptogenní cévní mozková příhoda. Interv Akut Kardiol. 2003;1(2):82-85.
4. Kuchynka P. a kol. Oční lékařství. Praha: Grada Publ; 2007. Kapitola 14, Neurooftalmologie; s. 501-547.
5. Vokurka M, Hugo J, et al. Velký lékařský slovník. 2. vyd.. Praha: Maxdorf; 2002. 923.
6. Breza J, et al. Princípy chirurgie. Bratislava: SAP; 2016, Kapitola IV, Cievna chirurgia; s. 597.
7. Dúbrava J. Foramen ovale patens a migréna. Kardiol. Prax. 2007;5(4):244-248.
8. Holmes DR jr, Cohen H, Katz WE, Reeder GS. Patent foramen ovale, systemic embolization and closure. Curr Probl Cardiol. 2004;29(2):56-94.
9. Berthet K, Lavergne T, Cohen A et al. Significant association of atrial vulnerability with atrial septal abnormalities in young patients with ischemic stroke of unknown cause. Stroke. 2000;31 : 398-403.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2020 Issue 6-
All articles in this issue
- Uveal Melanoma Biopsy. A Review
- VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
- Evaluation of Patients Presenting to the Ophthalmology Department of a Tertiary Hospital for Nonemergency Reasons During the Covid-19 Pandemic
- Changed Eye Functions and Quality of Life of Seniors with Diabetic Retinopathy
- Can Visual Function Be Affected by an Open Foramen Ovale?
- Late Functional and Morphological Findings after Methylalcohol Poisoning
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Can Visual Function Be Affected by an Open Foramen Ovale?
- VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
- Late Functional and Morphological Findings after Methylalcohol Poisoning
- Uveal Melanoma Biopsy. A Review
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

