-
Medical journals
- Career
Pressure injuries prevention is better than solving of their complications
Authors: L. Veverková; K. Krejsová; M. Kacafírková; M. Reška; P. Vlček; J. Žák; J. Konečný; I. Čapov
Authors‘ workplace: First Department of Surgery, Faculty of Medicine, Masaryk University and St. Anne´s University Hospital, Brno, Czech Republic
Published in: Cesk Slov Neurol N 2018; 81(Suplementum 1): 32-37
Category: Original Paper
doi: https://doi.org/10.14735/amcsnn2018S32Overview
Aim:
Target of this study was to analyse occurrence of pressure ulcers (PUs) in patients hospitalized at First Department of Surgery of St. Anne’s University Hospital between 2015 and 2017, identify their dependency on neurological comorbidities. Especially in group of eight patients with developed position PUs to analyse the possibility to influence their origin.
Methodology:
Retrospective analysis of the data from the hospital information system and an electronic tool (i-hojeni.cz). Statistical analysis was carried out by means of Pearson’s chi-square test, level of significance 0.05.
Results:
In the period 2015 – 2017 in total 9,550 patients out of 11,028 hospitalized patients underwent surgery. The PUs developed during hospitalization in 115 hospitalized patients (62 women and 53 men), out of which 104 underwent surgery. Average age of these patients was 81.61 (36 – 97) years of age, the average body mass index (BMI) was 24.93 and average length of hospitalization was 23.4 days. The time between admission to hospital and surgery was 2.82 (0 – 16) days. On average, there occurred 1.41 PUs per patient. The most frequent location of PUs were heels and buttocks. We found no statistically significant relation between BMI and occurrence of PUs (p > 0.05). On the contrary, the patients’ age and length of hospitalization related to the occurrence of PUs (p < 0.05). We proved non-statistic relation between development of pressure ulcer in operated patients and existence of neurological anamnesis. In total, 15 patients died, nevertheless 9 of them died with symptoms of sepsis with no direct relation to the PU lesions. A special group of evaluated patients were eight patients who had PUs after position trauma. The six of them died (75%) of septic development due to PUs.
Conclusion:
In spite of all preventive measure, PUs develop in surgically treated patients, especially those with neurological diseases in patient history (71.30%). Measures preventing development of PUs need to be applied not only in hospitals and institutes of social care but also in home care. Consequences of falls – especially of elderly with frequently insufficient social background may be ultimately fatal.
Key words:
decubitus – pressure lesion – incidence – trauma patient – position pressure ulcers
Introduction
Statistic clearly shows that approximately 2 – 5% of surgical interventions result in development of infection. These infections may have serious impact not only on patient’s health and their return to active lives but also on hospital operations and increased financial burden for the healthcare providers. Up to 5% cases of infections associated with health care may result in death of a patient. This group of patients includes also patients suffering from pressure ulcers (PUs) development during their hospitalization [1 – 3]. In spite of all preventive measures the PUs still occurs, and they will keep doing, so we speak here about so-called non-avoidable hospital acquired PUs. Their treatment is extremely costly and lengthy. As a result of falling, so-called “position trauma“ can develop – it is a muscle damage with consequent rhabdomyolysis, damage of nerves, cardiovascular system with skin defect development. This condition is a consequence of any long-term imposed position, e. g. in elderly with poor social background. Worsened recovery of defect may be caused by a number of factors such as age, nutrition conditions, cardiovascular diseases, infection, other comorbidities but also neurological diseases.
Materials and methods
Retrospective analysis of data from the hospital information system and an electronic tool (i-hojeni.cz) during the period between 2015 and 2017. Statistical analysis was carried out by means of Pearson’s chi--square test with level of significance of 0.5.
Results
Out of the total number of 11,028 patients hospitalized at First Department of Surgery of St. Anne’s University Hospital between 2015 and 2017 in total 9,550 (86.59%) patients underwent surgery.
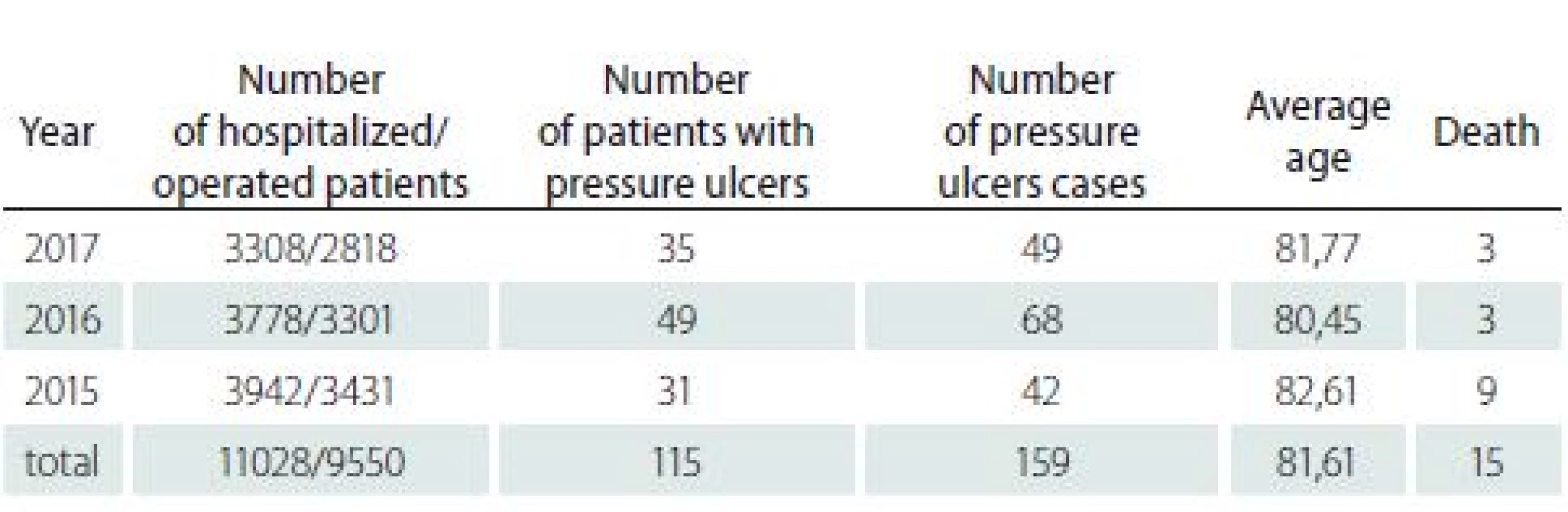
Within the monitored period, new PUs developed during hospitalization in First Department of Surgery in 115 patients, out of which 104 underwent surgery. An independent group consisted of eight patients who were admitted with the position trauma symptoms. Average age of patients was 81.61 (36 – 97) years and the group consisted of 62 women and 53 men (Tab. 1; Fig. 1, 2).
1. Patient´s gender.
Obr. 1. Pohlaví pacientů.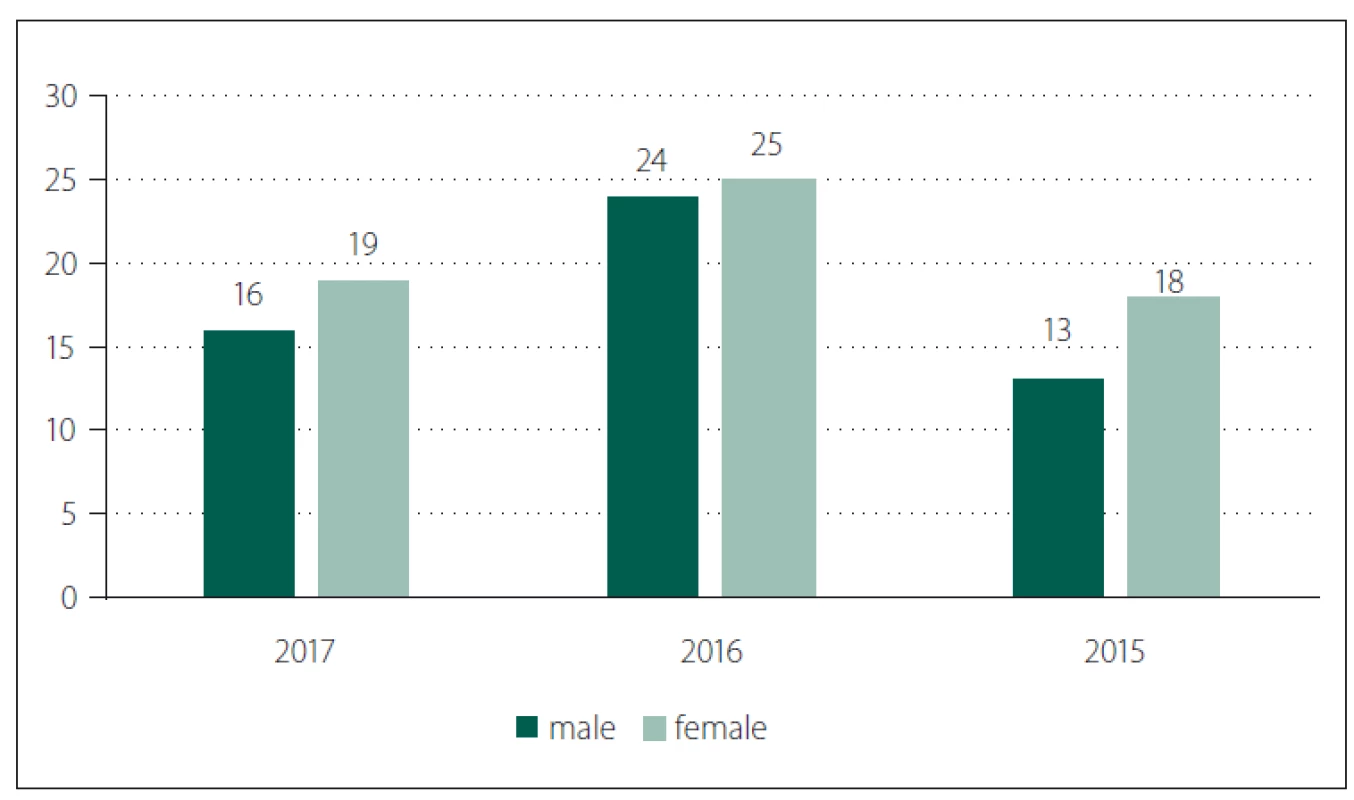
2. Patients’ age (distribution in given years).
Obr. 2. Věk pacientů (distribuce v daných letech).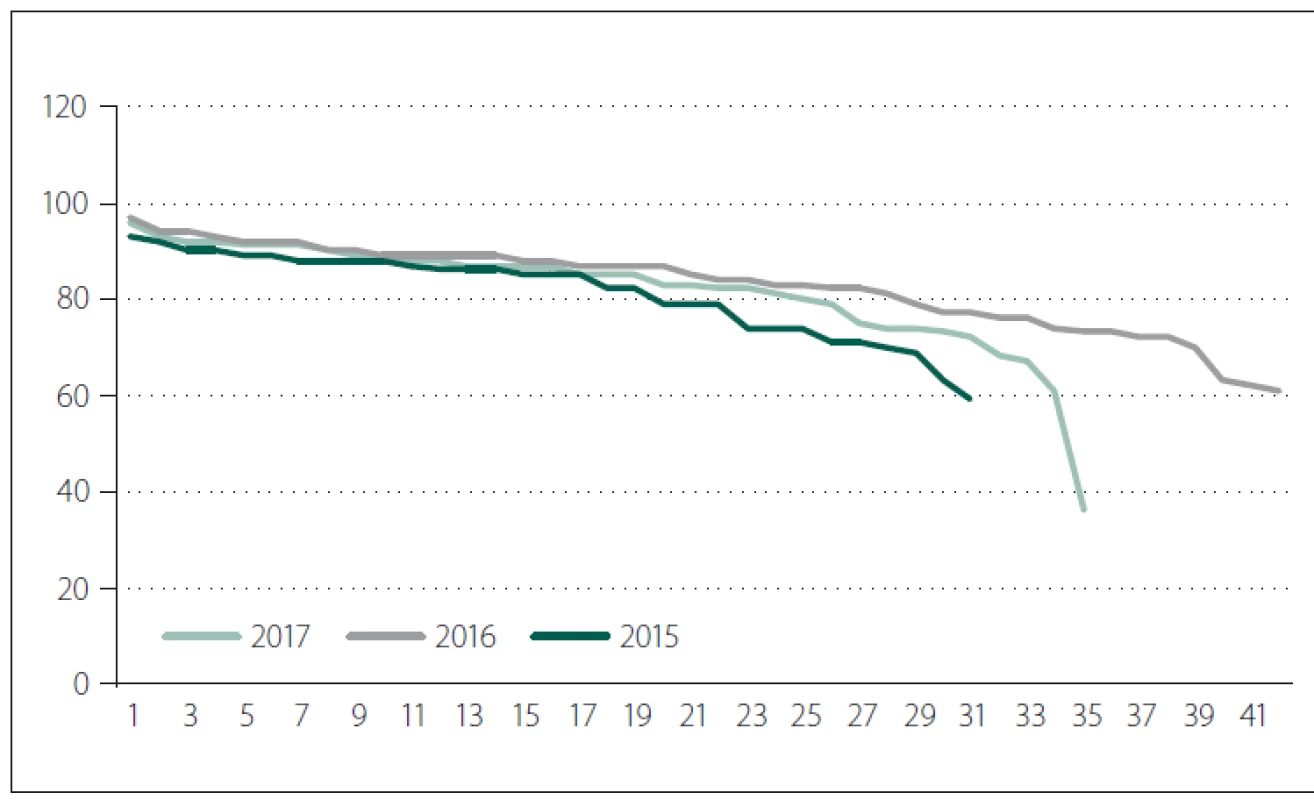
Body mass index (BMI) was on average 25.37 (16.7 – 41.2) kg/ m2. Average length of hospitalization was 25.7 (3 – 187) days. Period between admissions until the operation lasted on average for 2.79 (0 – 16 days). Although the factor of period between admissions until the day of operation seem to predict the development of PUs, in fact it did not in our group of patients.
Amongst patient suffering from PUs we observed occurrence of neurological diagnoses in patient history data. Regarding the fact that we had supposed that operated patients with neurological diagnosis are exposed to higher risk of development of PUs. We identified increased percentage of occurrence of PUs in 71.30% (with 82 patients). Most typically these were patients following a stroke, patients suffering from Alzheimer disease or other type of cerebral insufficiency. Conditions following the brain tumour surgery or cervical spondylosis occurred only in three cases (Fig. 3).
3. Relation between diagnoses with occurrence of pressure ulcers and neurological diagnosis in anamnesis with operated patients 2015–2017.
Obr. 3. Vztah mezi diagnózou s výskytem dekubitů a neurologickou diagnózou v anamnéze u operovaných nemocných 2015–2017.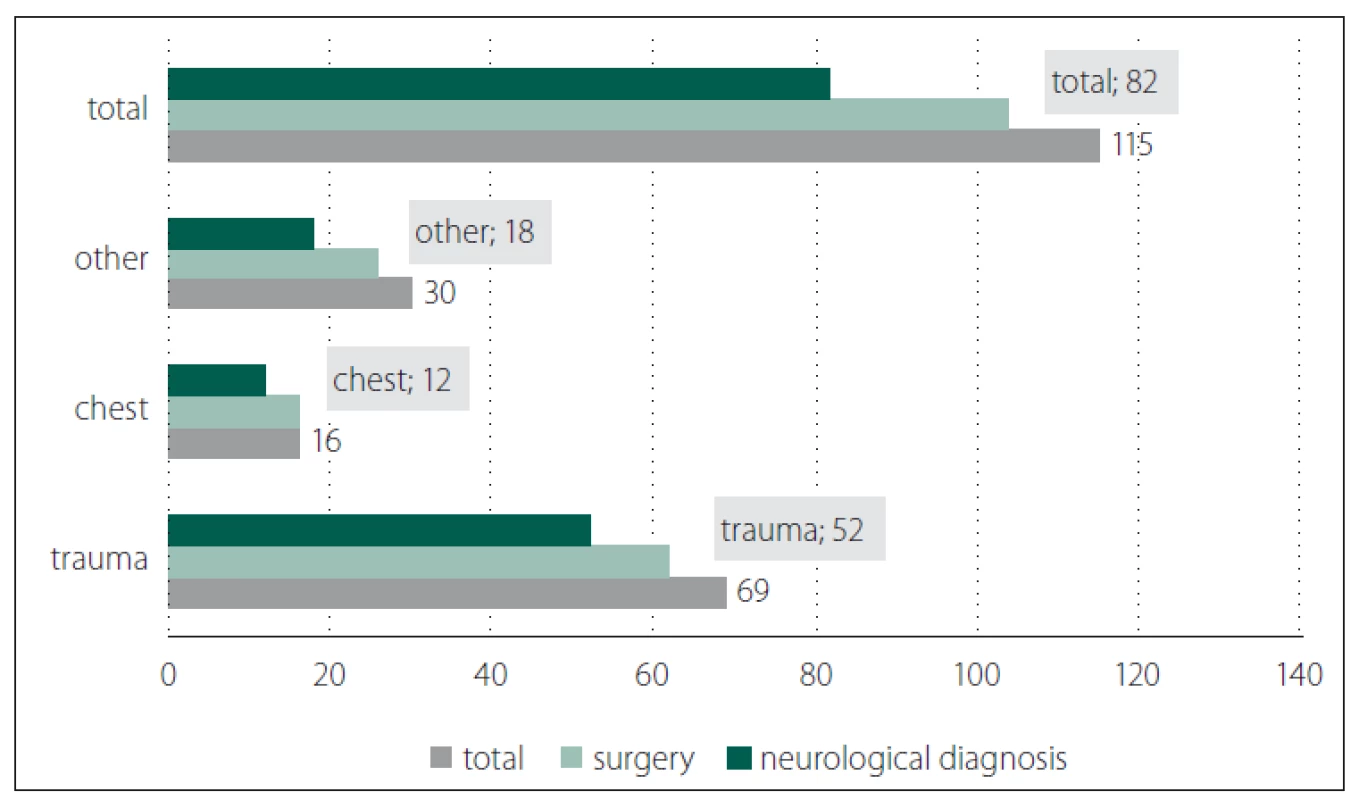
Pressure ulcers were most typically ranged between grade 1 and 2 (average of 1.68).
Amongst patients suffering from position trauma the grades of PUs were between II. and IV. category.
Number of PUs per one patient in our group was 1.42. The patients with position traumas suffered from up to five locations or three locations with signs of pressure lesions. Fig. 4, 5 show PUs in two patients.
4. Patient, 73-years-old man, living alone, visited by son. Found unconscious in his garden. Admitted to hospital with position trauma, dehydration and rhabdomyolysis. After admission, hypotension, hyperthermia and large position trauma with max. changes on lateral dorsal side of torso and lower limbs. Patient is a chronic ethylic (A–D).
Obr. 4. Pacient, 73letý muž, žije sám, navštěvuje ho syn. Tři dny ležel na zahradě v bezvědomí, při přijetí hypotenze, hypertermie a rozsáhlé trauma s maximem změn v oblasti trupu laterodorzálně l.dx. a dolních končetin. Přijat jako poziční trauma s dehydratací a rhabdomyolýzou k terapii. Pacient závislý na alkoholu (A–D).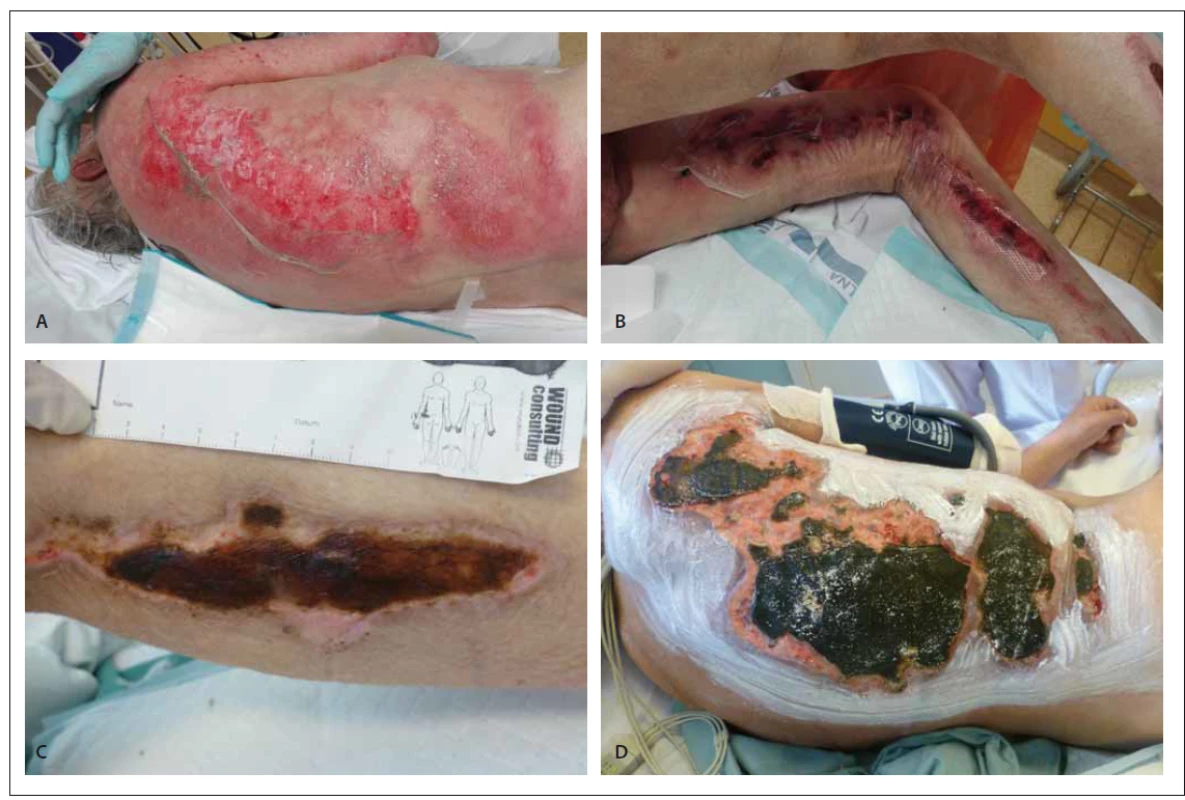
5. Patient, 64-years-old female, casus socialis. Moves around on the wheelchair, condition after amputation of right lower limb above knee (A–C).
Obr. 5. Pacientka, 64 letá žena, casus socialis. Pohybuje se na invalidním vozíku, stav po amputaci pravé dolní končetiny ve stehně, defekt na hýždi (A–C).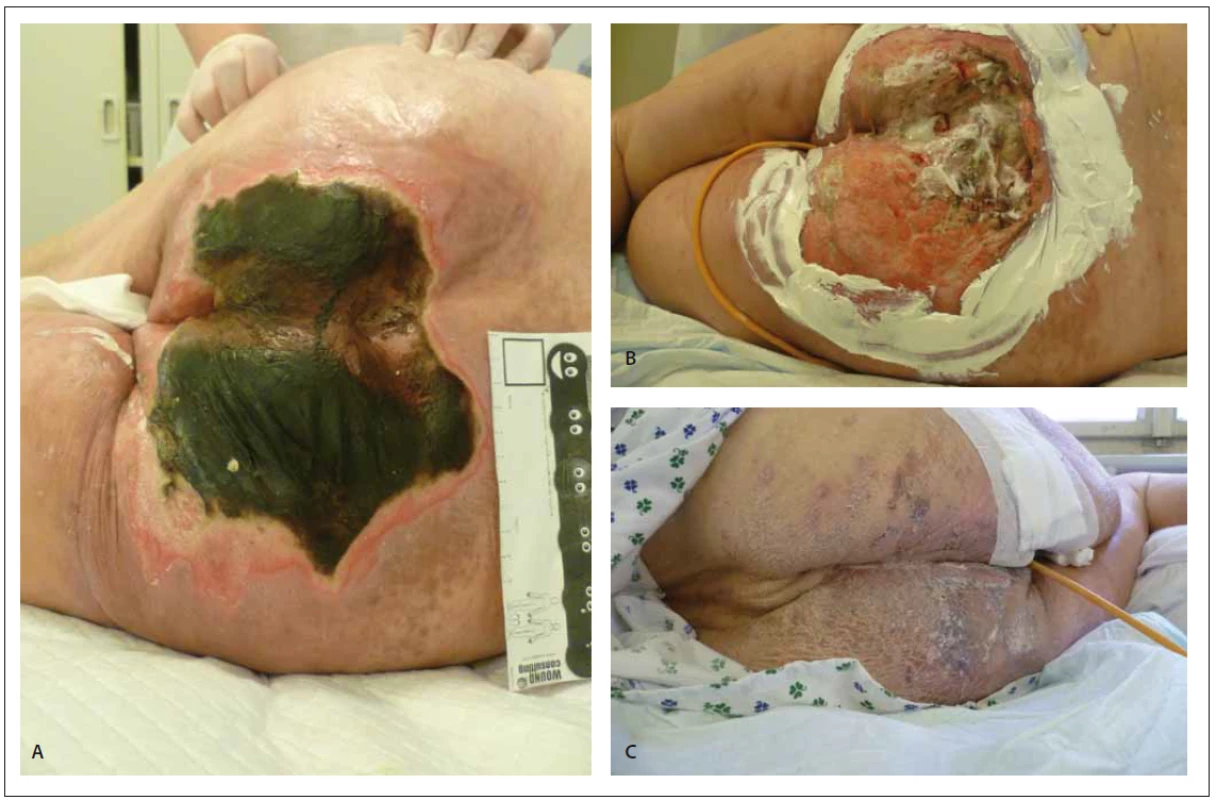
Most frequently, the PUs occurred in buttocks and then on the heels (Fig. 6).
6. Location of pressure ulcers in hospitalized patients in 2015–2017.
Obr. 6. Lokalizace dekubitů u hospitalizovaných nemocných v letech 2016–2017.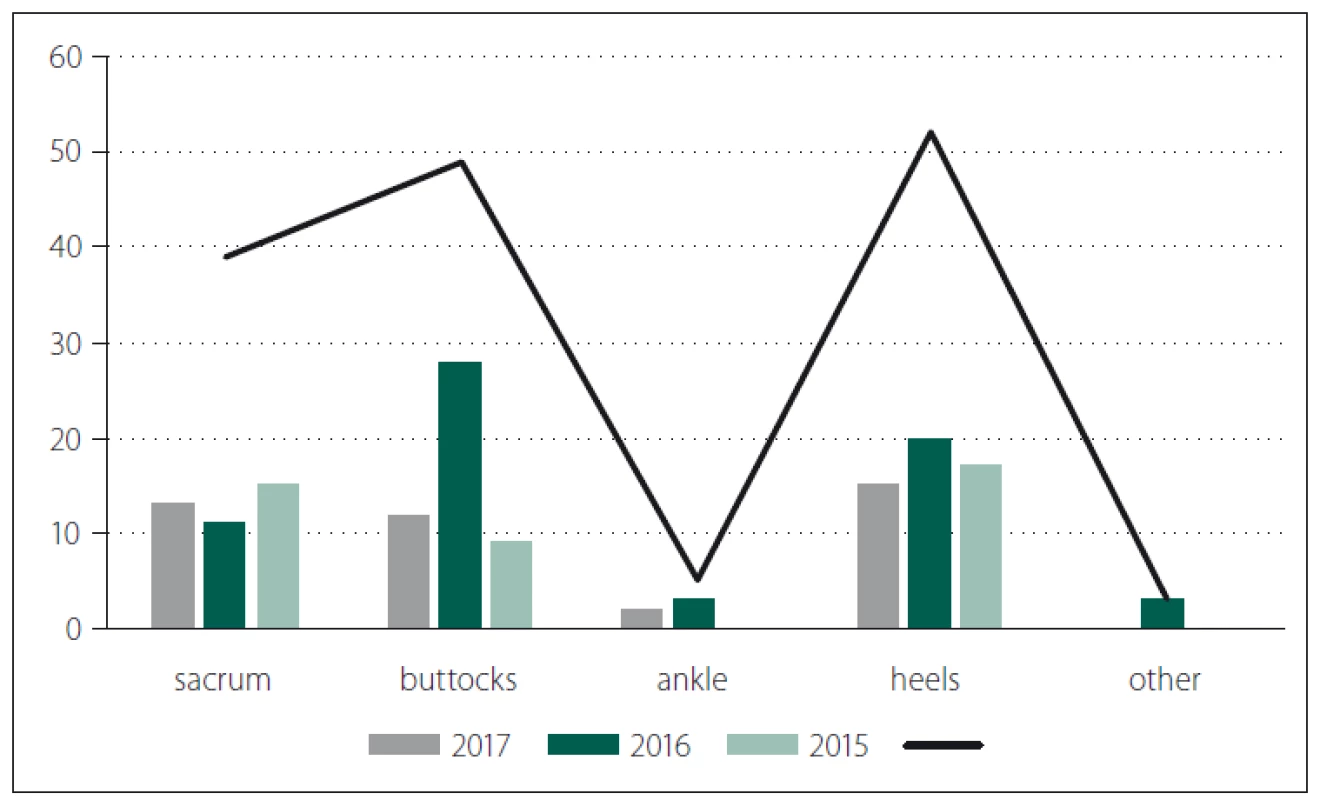
In relation with occurrence of PUs within the observed group of patients we focused on significance of some of the risk factors (BMI, age, length of hospitalization, comorbidity).
We compared the monitored values with the number of finished hospitalization in our department, the average age 58.15, BMI 26.5 with average length of hospitalization – 5.92 days. We did not find any statistically significant relation between BMI and development of PUs (p > 0.05). Age of patients and length of hospitalization showed statistically significant relation with occurrence of PUs.
Very serious and probably absolutely fundamental factor predicting development of PUs was in 71.30% occurrence of neurological disease in anamnesis in trauma patients and patients following the chest surgery.
Out of the total 62 trauma-operated patients, in 52 patients we identified serious neurological diseases prior development of trauma (Tab. 2).
2. Group characteristics – patient with pressure ulcers. 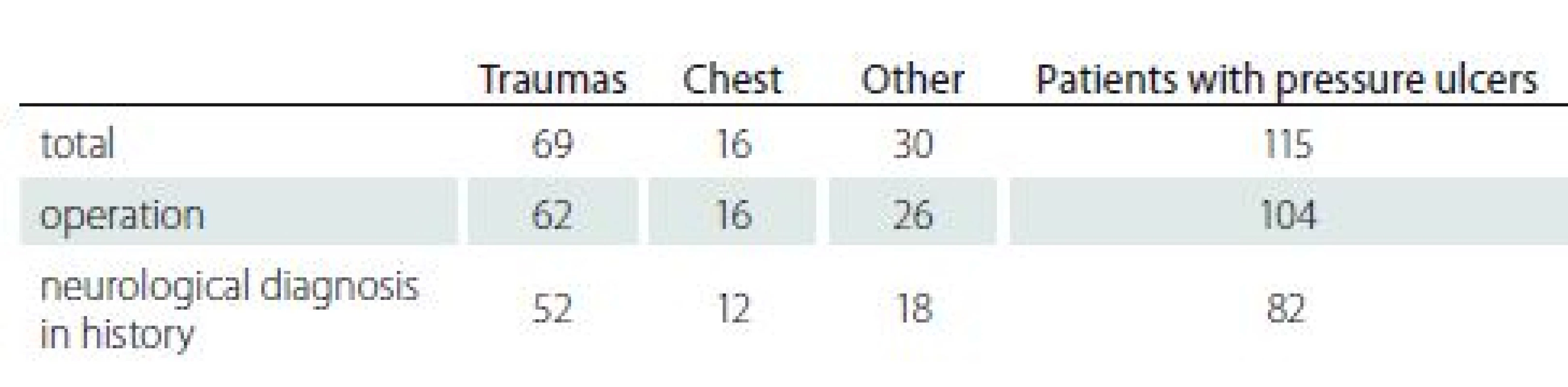
Similar situation occurred in a group of 16 patients suffering from PUs after chest surgery. In 75% patients following the chest surgery and consequently developed PUs, there was a neurological disease in their patient history (cerebral palsy, condition after meningioma surgery, paraplegia following stroke, spinal compression, Parkinson disease, polyneuropathy). Even though it is a relatively small percentage of patients in our presented group, it is obvious that in cases of patients suffering from PUs there were more frequent neurological diagnosis in their patient history. Statistical evaluation is presented in Tab. 3.
3. Relation of the neurological diagnose in history and surgical diagnose and pressure ulcers. Χ2 = 2.53, df = 2. Χ2/df =1.27, P (Χ2 > 2.36) = 0.2814. 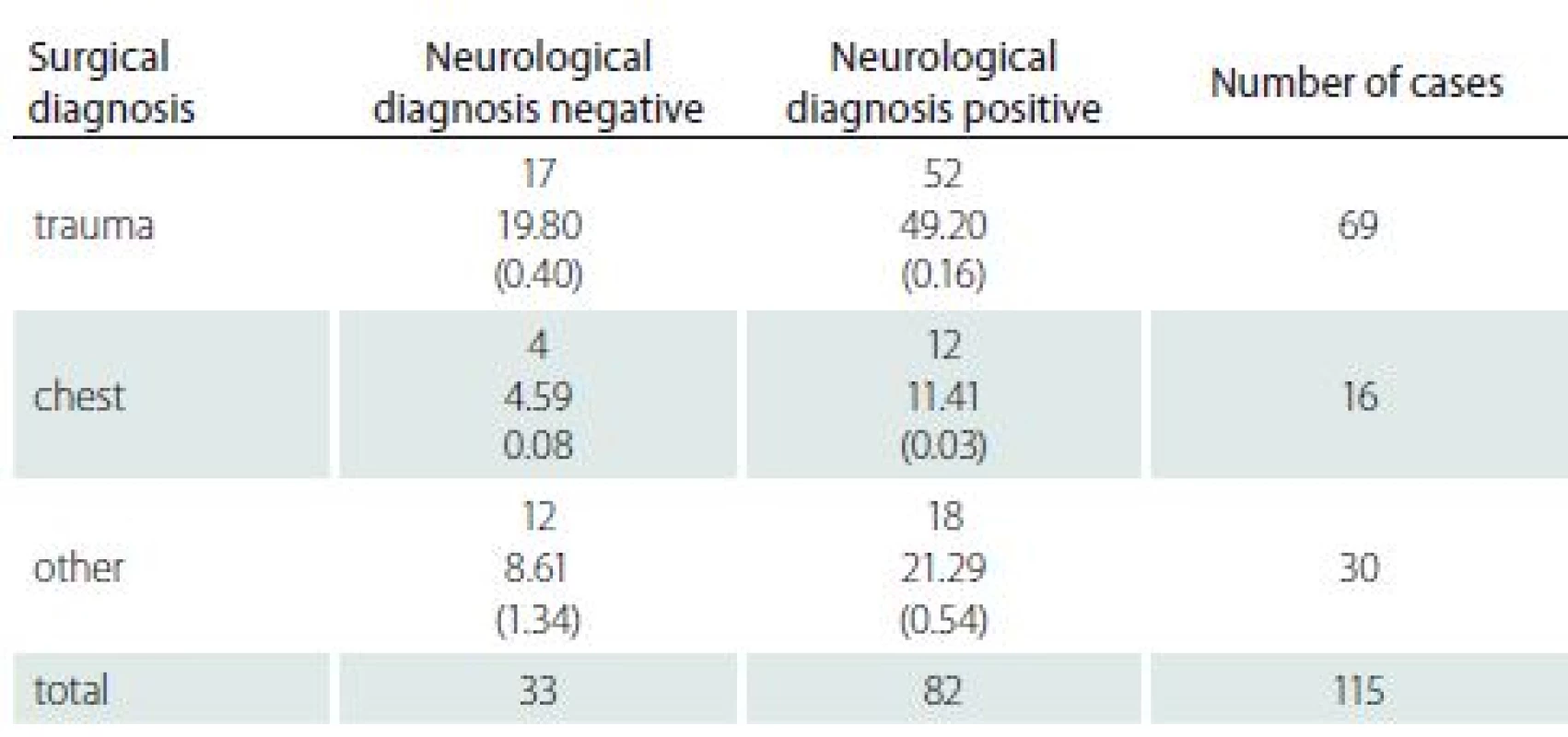
It is obvious that presence of neurological diagnosis represents a factor which shows very significant within our group.
Out of all analysed patients (n = 115) suffering from PUs 15 patients died (13.0%) (Fig. 7). Death was caused by sepsis, nevertheless only with 6 patients the sepsis was caused by and related to PUs. All these cases involved patients with position trauma. Out of total 8 patients with PUs and position trauma, 6 died – that is 75%. These were some of the “most expensive patients” in terms of costs of care. For example one patient was admitted after the fall with sun stroke and severe dehydration with necessary artificial lung ventilation with comorbidities, assessed grade 4 by American Society of Anaesthesiologists (ASA) physical status classification, have demonstrated a correlation between ASA classification and perioperative mortality. Average ASA value of our analysed patients was 3.17.
7. Chart of death of patients suffering from pressure ulcers.
Obr. 7. Graf úmrtí pacientů s dekubity.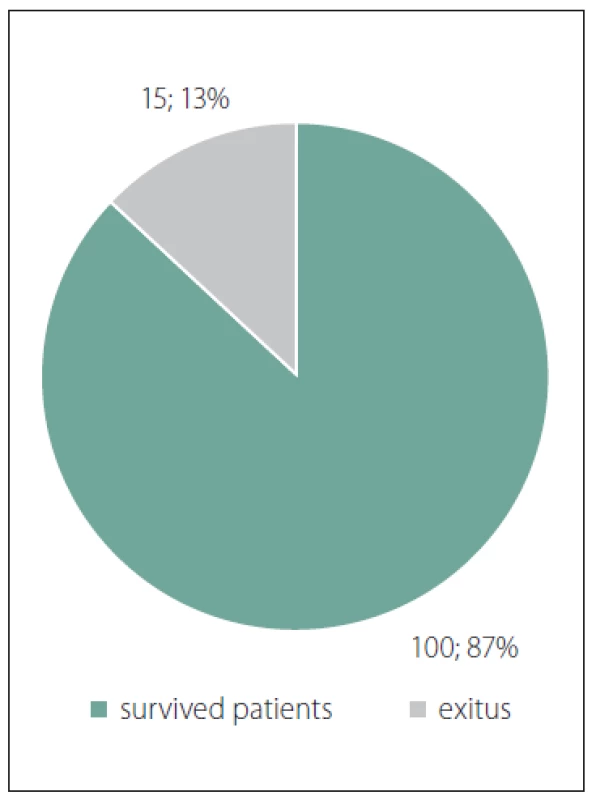
With other patients who died n = 9 (8.4%), the cause of death did not directly relate to PUs. These are patients operated for severe symptoms of peritonitis who suffered severe bronchopneumonia or urinary sepsis, osteomyelitis etc. following the surgery.
Discussion
Each developed pressure sore brings unpleasant complication both for the patient and the nursing staff. Treatment of developed PUs leads to prolonged hospitalization of the patient and, consequently, to increased financial burden for the system [1,2]. Compensation for hospitalization at the standard ward shows clearly descending tendency (1,260 CZK per one day between day 1 and 3; contrary to 586 CZK per day starting from day 13 until the release of patient from hospital). Subjectively, PUs cause pain relating to increase occurrence of hospital-acquired infections (worsening both local and general health status of the patient including the threat of development of sepsis) [3,4].
In our retrospective study we confirmed that development of PUs does not relate to BMI of the patients, which nevertheless does not represent sufficient information concerning the nutrition status of the patient and may rather be used as a general value to assess the risk of PUs development. In case of other monitored variables, we proved dependence between the patient’s age and development of PUs or between development of PU and length of hospitalization and neurological diagnosis in patient history.
Our group of patients suffering with post-operative PUs is rather small compared to total number of hospitalised patients and patients undergoing surgery at the First Department of Surgery proves high quality of care provided by the medical and nursing staff.
Frequently, a common place fall of a polymorbid patients, who live alone and lack sufficient physical power to manage to care for themselves, may result in fatal consequences.
According to the data from the Institute of Health Information and Statistics of the Czech Republic (IHIS CZ), occurrence of death caused by PUs is on nation-wide range very low – only 5.6% [5]. In our group it was in 75% patients following the position trauma.
Our department employs various method of local wound treatment, including the negative pressure wound therapy [6]. We need to realize that, apart from the local therapy, in majority of cases we are unable to treat PUs of higher grade without corresponding systemic therapy. In case the patients are not treated systemic but locally, their overall health status may on contrary worsen. Wounds that are not treated adequately may cause significant suffering to patients and have negative impact on physical, social, emotional and financial aspects of their lives [7 – 9]. Generally, we can state that higher age and longer stay in hospital is linked with increased occurrence of PUs [10]. Prevention of falls represents a basic precaution of any trauma at home and prevention measure linked to the possible complication during hospitalization.
Conclusion
Occurrence of PUs in our department in hospitalized patients and patients undergoing surgery is repeatedly very low, which testifies very good quality and professional care for the patients. Undoubtedly, the benefits from the use of a specialized wound monitoring tool and database within our hospital information system, including implementation of preventive measures in line with World Union of Wound Healing Societies recommendations. Our study proved relation between development of PUs and existence of neurological disease in patient undergoing surgery and in their history at our department. Measures preventing development of PUs need to be applied not only in hospitals and institutes of social care but also in-home care setting. Consequences of falls and trauma – especially in elderly with frequently insufficient social background may be ultimately fatal and thus leading to the more complications during the hospitalization including PUs occurrence.
The authors declare they have no potential The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.conflicts of interest concerning drugs, products, or services used in the study.
doc. MUDr. Lenka Veverková, Ph.D.
First Department of Surgery
St. Anne’s University Hospital
Pekarská 664/53
656 91 Brno
Czech Republic
e-mail: lenka.veverkova@fnusa.cz
Accepted for review: 28. 6. 2018
Accepted for print: 16. 8. 2018
Sources
1. World Health Organization. WHO Guidelines for safe surgery 2009: safe surgery saves lives. [online]. Geneva: WHO Press 2009. Available from URL: http:/ / whqlibdoc.who.int/ publications/ 2009/ 9789241598552_eng.pdf.
2. National Institute for Health and Clinical Excellence. Appendix H: Methodology checklists: economic evaluations. The guidelines manual. London: NICE 2009; 195 : 200 – 207.
3. Gottrup F, Apelqvist J, Price P et al. Outcomes in controlled and comparative studies on non-healing wounds: recommendations to improve the quality of evidence in wound management. J Wound Care 2010; 19(6): 237 – 268. doi: 10.12968/ jowc.2010.19.6.48471.
4. Pokorna A, Saibertova S, Vasmanska S et al. Registers of pressure ulcers in an international context. Cent Eur J Nurs Midw 2016; 7(2): 444 – 452. doi: 10.15452/ CEJNM.2016.07.0013.
5. Mandal A. Role of topical negative pressure in pressure ulcer management. J Wound Care 2007; 16(1): 33 – 35. doi: 10.12968/ jowc.2007.16.1.26987.
6. Haesler E (ed). National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers: quick reference guide. Perth: Cambridge Media 2014.
7. Black JM, Cuddigan JE, Walko MA et al. Medical device related pressure ulcers in hospitalized patients. Int Wound J 2010; 7(5): 358 – 365. doi: 10.1111/ j.1742-481X.2010.00699.x.
8. Pokorna A, Benešová K, Mužik J et al. The pressure ulcers monitoring in patiens with neurological diseases – analyse of the National Register of Hospitalized Patient. Cesk Slov Neurol N 2016; 79 (Suppl 1): S8 – S14. doi: 10.14735/ amcsnn2016S8.
9. Haesler E (ed). National Pressure Ulcer Advisory Pa-nel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Osborne Park: Cambridge Media 2014.
Labels
Paediatric neurology Neurosurgery Neurology
Article was published inCzech and Slovak Neurology and Neurosurgery

2018 Issue Suplementum 1-
All articles in this issue
- Pressure lesion monitoring – data set validation after second pilot data collection
- Wound healing effects after application of polyunsaturated fatty acids in rat
- Pressure ulcers in outpatients of the Spinal Unit of University Hospital Brno 2013– 2016
- Supraclavicular flap in reconstruction of intraoral defects
- The pressure ulcers in patients with comorbid neurological disorders
- The factors of pressure ulcer’s healing in critically ill patients
- Factors influencing recurrence of the pressureulcers after plastic surgery – retrospective analysis
- Pressure injuries prevention is better than solving of their complications
- Chondroblastic osteosarcoma of maxilla, a patient with Li- Fraumeni syndrome
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- The pressure ulcers in patients with comorbid neurological disorders
- Chondroblastic osteosarcoma of maxilla, a patient with Li- Fraumeni syndrome
- Supraclavicular flap in reconstruction of intraoral defects
- Pressure lesion monitoring – data set validation after second pilot data collection
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career