-
Medical journals
- Career
Primary Branchiogenic Carcinoma
Authors: Horakova Zuzana 1; Velecky Lukáš 2; Pazourkova Marta 3; Urbánková Pavla 1; Smilek Pavel 1
Authors‘ workplace: Clinic of otorhinolaryngology head and neck surgery, Faculty of Medicine, Masaryk university, St. Anne’s University Hospital, Brno, Czech Republic 2 Department of pathology, Faculty of Medicine, Masaryk university, St. Anne’s University Hospital, Brno, Cz 1
Published in: Klin Onkol 2018; 31(4): 296-300
Category: Case Report
doi: https://doi.org/10.14735/amko2018296Overview
Background:
Primary branchiogenic carcinoma (BC) is an exceptional diagnostic entity. In most cases, suspicion of BC is confirmed to be a cystic lymph node metastasis of an occult primary tumor. Martin and Khafif therefore established diagnostic criteria, emphasizing above all the importance of a histologically assessed transformation of cystic lining epithelium into an invasive squamous cell carcinoma in one pathological lesion after the exclusion of a primary tumor.
Case report:
We present a case report of an 80-year-old patient who presented for a follow-up for an 8-year history of a benign lateral cervical cyst, which was not surgically treated due to the patient‘s high risk of complications from general anesthesia. In spite of the risk, the surgery was performed after a sudden clinical progression, and surprisingly, post-operative histology revealed BC.
Conslusion:
BC is a very rare entity, strictly defined by Martin’s and Khafif’s criteria. Recently, BCs have been presented in the literature only as unique case reports responding as in our patient to the above mentioned criteria, with particular emphasis on the histological aspect, imaging the cystic lining epithelium transforming into an invasive squamous cell carcinoma in one pathological lesion and a long history without evidence of primary tumor.
Key words:
branchiogenic carcinoma – lateral branchial neck cyst – occult carcinoma – metastasis of unknown primary origin
Introduction
Primary branchiogenic carcinoma (BC) is a malignant tumor arising in branchial cervical cysts. It was first described by Volmann in 1882, and criteria were defined by Martin in 1950, which were then modified by Khafif in 1989 [1,2]. Branchial cyst presents as a smooth, soft ovoid cystic structure of the lateral neck originating in the remnant of an incompletely closed branchial cleft at the anterior margin of the sternocleidomastoid muscle. The lining of the cyst consists of a layered squamous cell epithelium from which its malignancy (squamous cell carcinoma – SCC) develops. The BC diagnosis itself is accepted only when the strict criteria are met.
However, many authors still view the BC only as a cystic metastasis of an undiagnosed occult primary tumor.
Case Report
An 80-year-old patient had been monitored in an ear, nose and throat (ENT) outpatient department for several years. Eight years ago, he was first examined for a 6 × 6 cm, painless but slowly progressing lateral neck swelling of several months duration; otherwise he was symptom-free. A lateral cervical cyst was suspected (soft, elastic, fixed, painless, and located at the level of the middle third of the sternocleidomastoid muscle). The diagnosis was supported by ultrasound and CT scans – a thin-walled ovoid cystic formation with fluid content was displayed, without evidence of increased vascularization or pathological changes in the surrounding soft tissues, without neck lymphadenopathy; there was no other pathology under the regular (including endoscopic) ENT examination. As the patient was polymorbid, already suffering especially from cardiovascular diseases, the most conservative procedure was suggested. An aspiration biopsy was performed to reduce the volume and to exclude malignancy. The patient was regularly monitored. Regular aspiration of about 40–50 ml of a serous fluid was performed approximately 2–4 times a year. Cytology never indicated suspicious malignancy. After 8 years, however, there was a clinical reversal; the swelling progressed significantly faster, and a sudden bleeding complication emerged after the puncture. The CT showed an ovoid structure, 65 × 34 × 87 mm, but it was heterogenic, with a highly vascular wall of irregular width, pushing the neck vessel, deforming the hypopharynx (Fig. 1). Surgery was suggested despite the risk of general anesthesia.
1. A) A native CT image in the transversal plane – a cyst located among musculus sternocleidomastoideus, submandibular gland and vascular bundle with a inhomogeneous dense content and with a wall slightly irregular in width, 5.5 × 3.3 × 8.5 cm in size. B) Enhacement of the dorsal cyst wall after contrast medium application. C) The vessel in the early arterial phase. D) Sagittal reconstruction in the early arterial phase. E) Sagittal reconstruction in the late arterial phase. 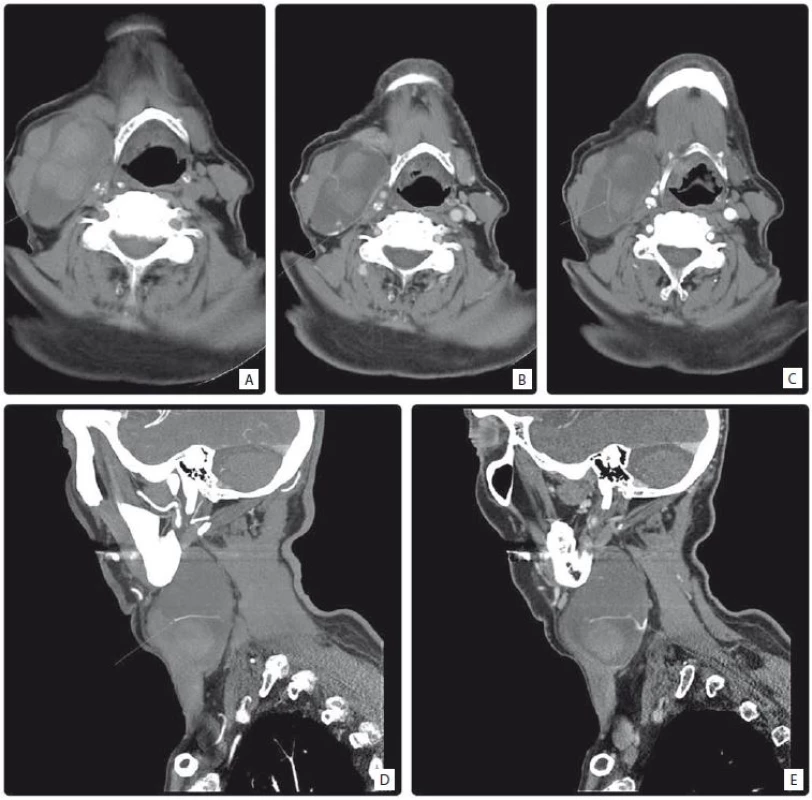
A large cystic structure, located between the jugular vein and the sterno-cleidomastoid muscle, with inflammation in the surrounding tissues, was removed. The histology of the structure was surprisingly determined to be BC, fulfilling the criterion of the presence of a squamous cyst in the lining of the epithelium, the transition zone, and an invasive SCC comprised in the vestige.
Histology macroscopically identified a cystic structure 70 × 35 × 30 mm in size, the inner surface with cauliflower formations and blood coagulants and a smooth outer surface. Microscopically, the cyst consisted of a fibrohyalinic wall, lined with a squamous epithelium with areas of heavy metaplasia transforming to in situ carcinoma and finally to invasive G2/G3 differentiated SCC with focal keratinization (p53+, CK5+) (Fig. 2). Due to a complete removal, assuming non-aggressive biological behavior and taking into account the age of the patient, no other general anesthesia associated with tonsillectomy and panendoscopy with guided biopsies were performed. For the same reason, adjuvant irradiation was not recommended. The patient has now been tumor-free for more than one year after finishing the treatment; he is under the follow-up care of a general practitioner.
2. A) Branchial cleft cyst with epithelial dysplasia (40×). B) Branchial cleft cyst with high-grade epithelial dysplasia/squamous cell carcinoma in situ (100×). C) Invasive squamous cell carcinoma arising in the wall of branchial cleft cyst (100×). D) Epithelium with high-grade dysplasia/squamous cell carcinoma in situ (400×). E) Epithelium with high-grade dysplasia/squamous cell carcinoma in situ (400×). F) Nest of invasive squamous cell carcinoma, G3 (400×). 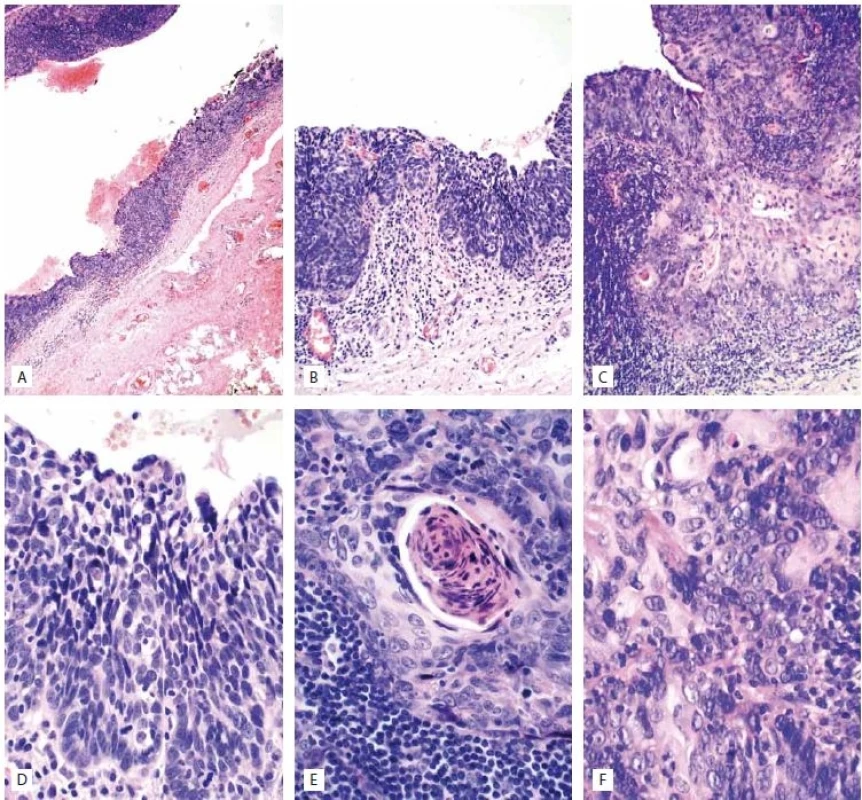
Discussion
Martin first proposed criteria for the diagnosis of BC (Tab. 1) [1] and Khafif later modified these criteria (Tab. 2) [2]. As he disagreed with the third criterion (e. g. an independent duplex tumor can be detected over 5 years or, on the contrary, an administered adjuvant radiotherapy could eliminate an occult primary tumor), he replaced it with different two criteria – the absence of a primary tumor in a different location and a clear histological identification of a cystic structure where the normal squamous cell epithelium of the lining with transition zone of dysplasia, carcinoma in situ and an invasive SCC. These criteria are widely accepted. Both authors emphasize the histological aspect of BC.
1. Criteria for the diagnosis of branchiogennic carcinoma by Martin [1]. ![Criteria for the diagnosis of branchiogennic carcinoma by Martin [1].](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image_pdf/a1732ef6f1fe46cb7529cd5e3abb4b81.jpeg)
2. Criteria modified by Khafi f [2]. ![Criteria modified by Khafi f [2].](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image_pdf/8f270830ca8bad8d28e4d23f1ba55474.jpeg)
BCs have been published in recent years as unique case reports that meet Martin’s and Khafif’s above-mentioned criteria. Zimmerman documented thein situ carcinoma stage without clear invasion, which confirms the above-mentioned etiopathogenetic theory [3]. The histological assessment was the strongest argument supporting the branchiogenic etiology in our case as well. Our patient met all of the criteria of localization, histological typeof an invasive SCC, absence of primary malignancy and, above all, a characteristic, histologically well-document-ed process of transition.
Diagnosis of BC is based on clinical, cytological and radiodiagnostic imaging. Ultrasound, CT and MRI reveal a characteristic image – a thin-walled cystic lesion with a back wall enhancement. However, an atypia may always arise (pseudosolid, anechogenous, heterogeneous, with debris and pseudocysts or an indistinguishable wall), which is associated with a change in cyst content in intracapsule bleeding or solidification, thickening of the wall caused by inflammation, or an increase in vascularization which may indicate a malignant transformation. We consider ultrasound to be an ideal follow-up method, as it is non-burdensome and applicable in regular intervals and allows for guided aspiration biopsy for cytological assessment [4].
CT corresponded with the diagnosis of a benign cyst in our patient for a long period until a rapidly progressing symptomatology recently arose. This, however, was more suspected to be inflammation induced by a repeated Fine needle aspiration biopsy (FNAB) (cytology was always benign.)
For BC diagnostics, the issue is first and foremost to exclude an occult primary head and neck tumor metastasis; in the past, this diagnosis was probably overestimated, whereas nowadays some authors completely deny the existence of BC as a pathologic unit itself.
On the other hand, the histology illustrating a transition of the epithelium to the carcinoma is the strongest argument supporting the existence of this clinical unit, which has never been explained in another way [5–7].
Cancer of unknown primary origin (CUP) presenting with cervical metastasisaccounts for approximately 5% of all head and neck malignancies, over 90% of which, as it was later assessed, originate from the lymphatic tissue (tonsil, nasopharynx, root of the tongue).
Though recent theories suggest that a small primary tumor may be eliminated by the patient’s immune system, examination, including panendoscopy, biopsy from Waldeyer’s ring and bilateral tonsillectomy are vastly recommended. Positron-emission tomography imaging is indicated for excluding a primary tumor during the diagnostic procedure and subsequent follow-up, when a metastasis of unknown primary should be confirmed [8–10].
In recent years, oropharyngeal location is regarded as particularly susceptive considering the dramatic increase in incidence of human papillomavirus (HPV) -associated oropharyngeal carcinomas (OPC), known for its early cystic metastases of small primary tumors. OPC is finally diagnosed in up to 70% of cases. From the HPV point of view, an interesting case of HPV-associated BC was reported by Maeda [11–15].
In our patient, the immunohistochemistry was negative for p16, which also supports the non-HPV etiology.
In our patient, histology was a great surprise considering the long-lasting history with a benign FNAB cytology. We do not believe the malignancy could persist for such a long time.
Another theory might arise – the malign transformation could be brought on by repeating FNAB; however, this was not supported by any report in the reviewed literature.
Therefore, endoscopy followed, but a tonsillectomy was not performed. The patient had a very high risk of general anesthesia and there was no clinical suspicion of tumor. The 8-year history of cystic lesion in the lateral neck, free of progression even without any treatment, is a very strong argument against the theory of occult tumor metastasis.
Complete surgical excision and adjuvant radiotherapy is considered to be an adequate therapy; even though data are rare in a rare diagnosis, a good prognosis is assumed. In our patient, a complete excision of a large cyst was performed. On account of the patient’s performance status, recommended panendoscopy and tonsillectomy were not performed. However, even though the suggested adjuvant radiotherapy could not be performed, he is, after a year of follow-up, recurrence-free under regular clinical examination.
Conclusion
BC is a very rare entity, strictly defined by Martin’s and Khafif’s criteria. The existence of BC itself is denied by some authors and pathologists and is considered to be the cystic metastasis of an unknown primary tumor.
In recent years, BCs have been presented in the literature only as unique case reports responding to the above mentioned criteria, with particular emphasis on the histological aspect, imaging the cystic lining epithelium transforming into an invasive SCC in one pathological lesion.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE recommendation for biomedical papers.
MUDr. Zuzana Horakova
Department of otorhinolaryngology head and neck surgery
Faculty of Medicine of Masaryk university
St. Anne´s University Hospital
Pekařská 664/53 656 91 Brno
e-mail: zuhorakova@seznam.cz
Submitted: 22. 2. 2018
Accepted: 24. 4. 2018
Sources
1. Martin H, Morfit HM, Ehrlich H. The case for branchiogenic cancer (malignant branchioma). Ann Surg 1950; 132 (5): 867–887.
2. Khafif RA, Prichep R, Minkowitz S. Primary branchiogenic carcinoma. Head Neck 1989; 11 (2): 153–163.
3. Zimmermann CE, von Domarus H, Moubayed P. Carcinoma in situ in a lateral cervical cyst. Head Neck 2002; 24 (10): 965–969. doi: 10.1002/hed.10118.
4. Hu S, Hu Ch, Yang L et al. Atypical imaging observations of branchial cleft cysts. Oncol Lett 2014; 7 (1): 219–222. doi: 10.3892/ol.2013.1656.
5. Lin YC, Fang SY, Huang RH et al. Branchiogenic squamous cell carcinoma: a case report. Int J Oral Myillofac Surg 2004; 33 (2): 209–212.
6. Girvigian MR, Rechdouni AK, Zeger D et al. Squamous cell carcinoma arising in a second branchial cleft cyst. Am J Clin Oncol 2004; 27 (1): 96–100.
7. Nakano A, Misima K, Katase N. A case of squamous cell carcinoma arising from branchial cleft cyst. Oral Maxillofac Surg 2015; 73 (4): 781–785. doi: 10.1016/j.joms.2014.10.036.
8. Zdražil B, Profant M, Povinec P. Přínos PET CT vyšetrenia do diagnostiky neznámého primárného tumoru s metastázováním do krčných lymfatických uzlín – naše skúsenosti. Otorinolaryng Foniat 2012; 61 (1): 53–56.
9. National Comprehensive Cancer Network. [online]. Available from: https: //www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf.
10. Mackenzie K, Watson M, Jankowska P et al. Investigation and management of the unknown primary with metastatic neck disease: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; 130 (Suppl 2): S170–S175. doi: 10.1017/S0022215116000591.
11. Maeda H, Deng Z, Ikegami T et al. Branchiogenic carcinoma with high-risk-type human papillomavirus infection: a case report. Oncol Lett 2016; 12 (3): 2087–2091. doi: 10.3892/ol.2016.4907.
12. Chauhan A, Tiwari S, Pathak N. Primary branchiogenic carcinoma: report of a case and a review of the literature. J Can Res Ther 2013; 9 (1): 135–137. doi: 10.4103/0973-1482.110380.
13. Schmalbach CE, Miller FR. Occult primary head and neck carcinoma. Curr Oncol Rep 2007; 9 (2): 139–146.
14. Goldenberg D, Sciubba J, Koch WM. Cystic metastasis from head and neck squamous cell cancer: a distinct disease variant. Head Neck 2006; 28 (7): 633–638. doi: 10.1002/hed.20381.
15. Yasui T, Morii E, Yamamoto Y et al. Human papillomavirus and cystic node metastasis in oropharyngeal cancer and cancer of unknown primary origin. PLoS One 2014; 9 (4): e95364. doi: 10.1371/journal.pone.0095364.
Labels
Paediatric clinical oncology Surgery Clinical oncology
Article was published inClinical Oncology

2018 Issue 4-
All articles in this issue
- Use of Salivary MicroRNAs for Diagnosis of Solid Cancers
- Monoclonal Gammopathy of Undetermined Significance (MGUS)Monoclonal Gammopathy of Undetermined Significance (MGUS)
- Carcinoma of Unknown Primary in Head and Neck Region
- Occurrence and Antibiotic Resistance of Enterobacteriaceae in Acute Leukemia Patients
- Malignant Melanomas of the Skin Arising on the Feet
- Use of Fludarabine for the Treatment of Indolent Lymphoma with Chylothorax
- Expression Analysis of OIP5-AS1 in Non-Small Cell Lung Cancer
- A Combined Bioinformatics and Literature Based Approach for Identification of Long Non-coding RNAs That Modulate Vitamin D Receptor Signaling in Breast Cancer
- Metastases of a Breast Cancer to Skull Base
- Primary Branchiogenic Carcinoma
- The Therapeutic Effects of Specific CDK4/6-inhibitors in Treating HR-positive, HER2-negative Advanced Breast Cancer
- Clinical Oncology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Monoclonal Gammopathy of Undetermined Significance (MGUS)Monoclonal Gammopathy of Undetermined Significance (MGUS)
- Carcinoma of Unknown Primary in Head and Neck Region
- Occurrence and Antibiotic Resistance of Enterobacteriaceae in Acute Leukemia Patients
- Use of Salivary MicroRNAs for Diagnosis of Solid Cancers
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

