-
Medical journals
- Career
Comparison of creatinine clearance and estimated glomerular filtration rate in patients with chronic kidney disease
Authors: T. Šálek 1; V. Palička 2
Authors‘ workplace: Department of Clinical Biochemistry, Tomas Bata Regional Hospital in Zlín a. s., Havlíčkovo nábřeží 600, 76 75 Zlín, Czech Republic 1; Institute of Clinical Biochemistry and Diagnostics, Charles University in Prague, Faculty of Medicine and University Hospital, Hradec Králové, Czech Republic 2
Published in: Klin. Biochem. Metab., 22 (43), 2014, No. 3, p. 123-126
Overview
Aim:
The aim of the study is to compare creatinine clearance (CrCl) as old marker of glomerular filtration rate (GFR) with estimated glomerular filtration rate (eGFR) in patients with chronic kidney disease (CKD). We compared the impact of CrCl and eGFR on classification of CKD. We also looked at correlation between GFR tests and albuminuria.Design:
retrospective cross section design.Methods:
GFR was determined by CrCl and estimated from serum creatinine (eGFRcreatinine), from cystatin C (eGFRcystatinC) and combined equation (eGFRcreatinine+cystatinC). Creatinine and cystatin C were determined by standardized methods. We used new Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations.Results:
The median (interquartile range) of creatinine clearance was 1.21 ml/s per 1.73 m2 (0.76-1.72). All eGFR give lower results, eGFRcreatinine 1.01 ml/s per 1.73 m2 (0.63-1.42) (p<0.05), eGFRcystatinC 0.93 ml/s per 1.73 m2 (0.55-1.59) (p<0.05), eGFRcreatinine+cystatinC 0.96 ml/s per 1.73 m2 (0.90-1.05) (p<0.05). ClCr identified CKD by GFR criterion in 130 patients, eGFRcreatinine in 173 patients, eGFRcystatinC in 189 patients and eGFRcreatinine+cystatinC in 185 patients.Conclusions:
CrCl gives higher values than all eGFR. It has an impact on staging of CKD and drug dosing. eGFRcreatinine values and eGFRcystatinC have different association according to the range of GFR.Keywords:
creatinine, cystatin C, glomerular filtration rate, chronic kidney disease, creatinine clearance.Introduction
Since 1886, creatinine has been used as a marker of kidney function. It is a waste product of muscle metabolism. CrCl was usually used as the marker of GFR in the 20th century. This test needs 24 hour urine collection. Creatinine is produced at constant rate, freely filtered by glomerulus, but tubular secretion of creatinine overestimates true GFR [1]. Urine collection is difficult for patients and incomplete or falsely high urine collections are frequent.
Chronic kidney disease is currently defined according to Kidney Disease Improving Global Outcomes (KDIGO) guidelines from 2012. CKD is defined as abnormalities in kidney structure or function present for more than three months with implications for health. Six stages of GFR are defined according to the level of GFR: G1 ≥1.5 ml/s per 1.73 m2, G2 1.0 – 1.49 ml/s per 1.73 m2, G3a 0.75 – 0.99 ml/s per 1.73 m2, G3b 0.5 – 0.74 ml/s per 1.73 m2, G4 0.25 – 0.49 ml/s per 1.73 m2, G5 < 0.25 ml/s per 1.73 m2. Standardized serum creatinine and cystatin C are recommended for estimation of GFR. CKD-EPI working group established CKD-EPI equation for eGFRcreatinine in 2009. CKD-EPI equations for estimation of GFR from serum cystatin C and combined equation eGFRcreatinine+cystatinC were established by the same working group in 2012.
Albuminuria is the most important marker of kidney damage. Albuminuria usually precedes the decline of GFR [2].
Determination of GFR is important for detection and staging of CKD and adjustment of drug dosages excreted by kidney.
We compared old and current approaches to determination of GFR. We did not find this comparison in literature. We also looked at differences in detection rate of CKD (GFR bellow 1.0 ml/s per 1.73 m2) and compared eGFRcreatinine with eGFRcystatinC.
Methods
Patients
The cross-sectional retrospective study included 352 consecutive patients from outpatient nephrology clinic of Tomas Bata hospital in Zlín from January to December 2013. The group consisted of 174 males and 178 females. Age ranged from 20 to 88 years. Median of age was 54 years (41-66). Patients in chronic dialysis program were not in this study. They were at stages G1-G4 and patients before chronic dialysis program.
The study was approved by The Ethic Committee of Tomas Bata Hospital.
Laboratory tests and equations
Creatinine was determined by enzymatic method traceable to NIST SRM 967 reference material [3].
Cystatin C was determined by particle enhanced immunoturbidimetric method (PETIA) traceable to ERM DA 471 reference material [4].
eGFRcreatinine was calculated according to CKD-EPI equation, which was established in 2009 [5]. eGFRcystatinC and eGFRcreatinine+cystatinC were calculated according to CKD-EPI equations established in 2012 [6].CrCl was calculated according to equation:CrCl = urine creatinine x urine volume/serum creatinine (ml/s per 1.73 m2).Total protein in urine was determined using benzethoniumchloride reaction. Albumin in urine was determined employing immunoturbidimetric method traceable to serum certified material CRM 470. All tests were manufactured by the Abbott company and determined on automated clinical chemistry Abbott Architect analyzer.
Statistical tests
D’Agostino-Pearson test was used for an assessment of the normal distribution.
Results of GFR are expressed as median (interquartile range (IQR)).
Friedman test was used for comparison of four medians of GFR.
Bland-Altman plot was used for comparison of eGFRcreatinine and eGFRcystatinC.
The Spearman correlation coefficient was used for correlation analysis.
Results
D’Agostino-Pearson test for normal distribution rejected normality for CrCl and all eGFR (p< 0.0001).
The median (IQR) of creatinine clearance was 1.21 ml/s per 1.73 m2 (0.76-1.72). All medians of eGFR were statistically lower than the median of creatinine clearance, eGFRcreatinine 1.01 ml/s per 1.73 m2 (0.63-1.42) (p<0.05), eGFRcystatinC 0.93 ml/s per 1.73 m2 (0.55-1.59) (p<0.05), eGFRcreatinine+cystatinC 0.96 ml/s per 1.73 m2 (0.90-1.05) (p<0.05).
We did not find difference among medians eGFRcreatinine, eGFRcystatinC and eGFRcreatinine+cystatinC (p>0.05).
Fig. 1 shows the differences between eGFRcreatinine and eGFRcystatinC. We can see at GFR values bellow 1.0 ml/s per 1.73 m2 that eGFRcreatinine values are higher than eGFRcystatinC (p<0.0001). eGFRcystatinC gives higher values in the range of GFR above 1.0 ml/s per 1.73 m2 (p<0.0001).
Figure 1. Bland-Altman plot between CKD-EPI 2012 (cystatin C) and CKD-EPI 2009 (creatinine) 
ClCr identified CKD by GFR criterion in 130 patients, eGFRcreatinine in 173 patients, eGFRcystatinC in 189 patients and eGFRcreatinine+cystatinC in 185 patients.
We performed correlation analysis in 148 patients, who had also 24-hour urine tests for albuminuria and total proteinuria. Table 1 shows interesting relations. We can see greater correlation among eGFR than any eGFR and CrCl.
1. Spearman correlation coefficients among variables 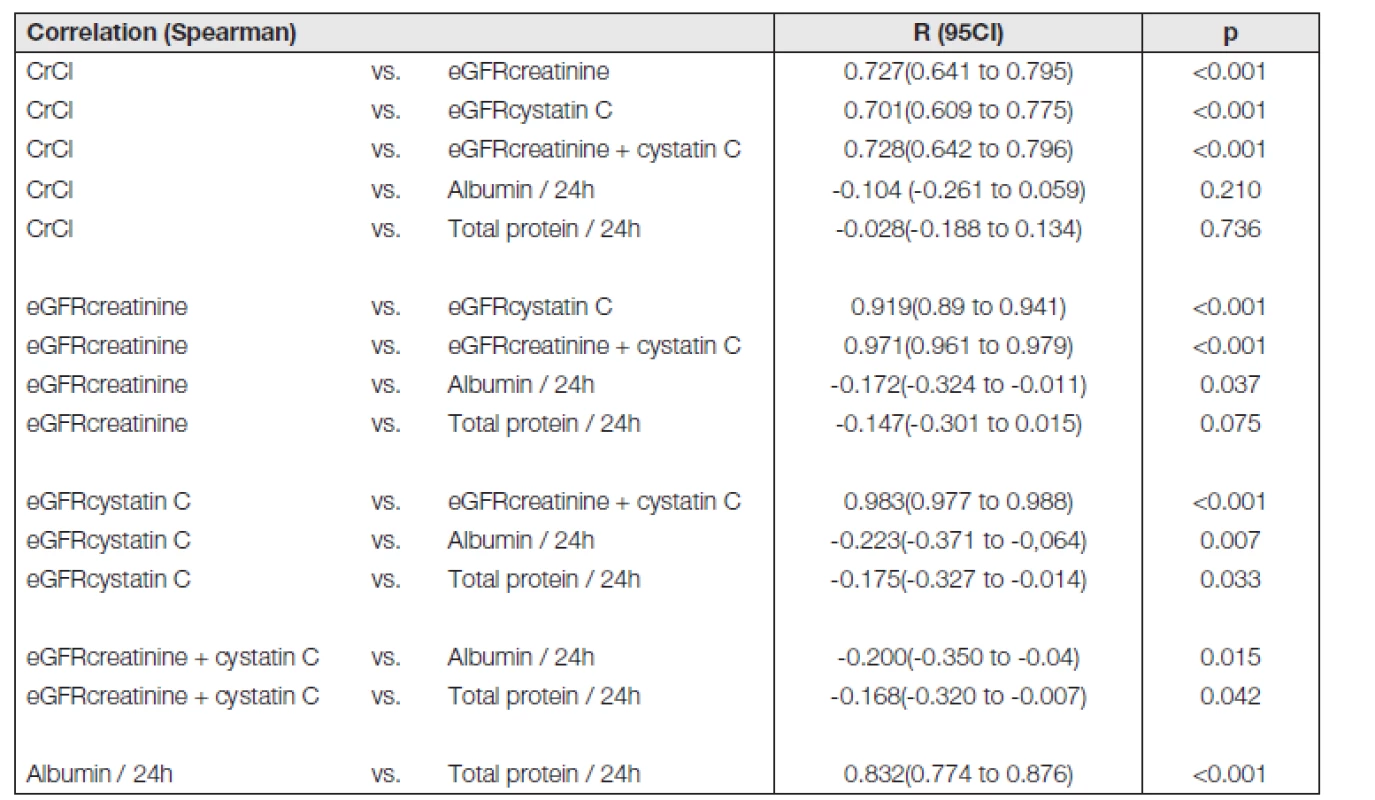
n = 148 Albuminuria and total proteinuria have no correlation with CrCl (p > 0.05).
There was no difference between correlation coefficients of albumin/24h vs. eGFRcystatinC and total protein/24h vs. eGFRcystatinC (p > 0.05).
There was no difference between correlation coefficients of albumin/24h vs. eGFRcreatinine+cystatinC and total protein/24h vs. eGFRcreatinine+cystatinC (p > 0.05).
Discussion
Creatinine clearance gave higher values than all eGFR in our study.
A lot of authors found similar results. Kumar et al. [7] shows similar results in a study with transplant recipients. Similar results were obtained in patients before bone marrow transplantation [8]. Studies with gold standard also found that creatinine clearance overestimate true GFR [9]. All these studies are consistent with our results. Tubular secretion is one of the possible explanations of these results.
Many drugs are excreted renally and their doses should be reduced in patients with CKD. Prescribers should take GFR into account when drug dosing. We should reduce dose or increase dosage interval in patients treated with aminoglycosides and GFR bellow 1.0 ml/s per 1.73 m2 according to KDIGO guidelines [10]. If we look at 352 patients of the study, creatinine clearance would recommend reduce drug dose in 130 patients. eGFRcreatinine in 174 patients, eGFRcystatinC in 189 patients and eGFRcreatinine+cystatinC in 185 patients. We can see that creatinine clearance performed lowest number of dose reductions which may decrease patient safety.
CrCl had no correlation with albuminuria. We found poor correlations between albuminuria and eGFR tests. Albuminuria usually precedes a decline of GFR [11]. This finding also confirms the need of both marker of GFR and marker of kidney damage for detection of CKD according to KDIGO guidelines [2].
We can see at Bland-Altman plot that at GFR values bellow 1.0 ml/s per 1.73 m2 eGFRcreatinine are higher than eGFRcystatinC. eGFRcystatinC gives higher values in the range of GFR above 1.0 ml/s per 1.73 m2. We can see similar trend in the work by Delanaye. This work uses the same traceable methods for determination of creatinine and cystatin C and three CKD-EPI equations [12]. The same results were found in diabetic patients [13,14]. Both works use standardised methods for creatinine and cystatin C and the same three CKD-EPI equations.
The major limitation of our study is that we did not use measured gold standard method for determination of GFR such as inulin clearance or isotopic method [15]. These methods are limited to specialized centres and are not used in routine clinical practice.
Another limitation is that patients did not have renal biopsies as reference method for accurate clinical diagnoses.
Conclusion
CrCl gives higher values than all eGFR. It has impact on detection rate of CKD and drug dosing.
Albuminuria has no correlation with CrCl.
eGFRcreatinine values and eGFRcystatinC have different associations according to the range of GFR.
Supported by the programme PRVOUK P37/11 and Project SVV 267003
Do redakce došlo 4. 4. 2014
Adresa pro korespondenci:
MUDr. Tomáš Šálek
Záhumení 789
687 22 Ostrožská Nová Ves
e-mail: tsalek@seznam.cz
Sources
1. Jabor A, editor. Vnitřní prostředí. Praha: Grada Publishing a.s., 2008.
2. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney inter.,Suppl. 2013, 3, p. 19-62.
3. Dodder, N. G., Tai, S. S., Sniegoski, L. T., Zhang, N. F., Welch, M. J. Certification of Creatinine in a Human Serum Reference Material by GC-MS and LC-MS. Clin. Chem., 2007, 53(9), p. 1694–9.
4. Grubb, A., Blirup-Jensen, S., Lindström, V., Schmidt, C., Althaus, H., Zegers, I., IFCC Working Group on Standardisation of Cystatin C (WG-SCC). First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin. Chem. Lab. Med., 2010, 48(11), p. 1619-21.
5. Levey, A. S., Stevens, L. A., Schmid, C. H., Zhang, Y. L., Castro, A. F. 3rd, Feldman, H. I., Kusek, J. W., Eggers, P., Van Lente, F., Greene, T., Coresh, J., CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A New Equation to Estimate Glomerular Filtration Rate. Ann. Inter. Med. 2009, 150(9), p. 604–12.
6. Inker, L. A., Schmid, C. H., Tighiouart, H. et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl. J. Med., 2012, 367(1), p. 20–9.
7. Kumar, R., Pendyala, P., Attwood, K., Gray, V., Venuto, R., Tornatore, K. Comparison of 12-Hour Creatinine Clearance and Estimated Glomerular Filtration Rate in Renal Transplant Recipients. Ren. Fail., 2013, 35(3), p. 333–7.
8. Hahn, T., Yao, S., Dunford, L. M., Thomas, J., Lohr, J., Arora, P., Battiwalla, M., Smiley, S. L., McCarthy, P. L. Jr. A Comparison of Measured Creatinine Clea-rance versus Calculated Glomerular Filtration Rate for Assessment of Renal Function before Autologous and Allogeneic BMT. Biol. Blood Marrow Transplant., 2009, 15(5), p. 574–9.
9. Fotopoulos, A., Bokharhli, J. A., Tsiouris, S., Katsaraki, A., Papadopoulos, A., Tsironi, M., Theodorou, J. Comparison of six radionuclidic and non-radionuclidic methods for the assessment of glomerular filtration rate in patients with chronic renal failure. Hell. J. Nucl. Med., 2006, 9(2), p. 133–40.
10. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney inter.,Suppl. 2013, 3, p. 91-111.
11. Llinares-Tello F. Rational use of laboratory tests: albuminuria. Clin. Chem. Lab. Med., 2013, 51(4), e55–e56.
12. Delanaye, P., Cavalier, E., Moranne, O., Lutteri, L., Krzesinski, J. M., Bruyère, O. Creatinine-or Cystatin C-Based Equations to Estimate Glomerular Filtration in the General Population: Impact on the Epidemiology of Chronic Kidney Disease. BMC Nephrol., 2013,14(1), p. 57.
13. Jabor, A., Franeková, J., Kubíček, Z., Šálek, T. eGFR a problem interpretace rovnic CKD-EPI. Klin. Biochem. Metab., 2014, 22(43), p. 8-10.
14. Šálek, T., Ponížil, P. Estimated glomerular filtration rate in diabetic patiens. Klin. Biochem. Metab., 2014, 22(43), p. 4-7.
15. Jabor, A., Hornová, L., Fantová, L., Engliš, M. Vyšetření funkce ledvin: možnosti biochemické laboratoře. Postrgraduální Medicína, 2006, 8(1), p. 18–22.
Labels
Clinical biochemistry Nuclear medicine Nutritive therapist
Article was published inClinical Biochemistry and Metabolism

2014 Issue 3-
All articles in this issue
- Positive association of adiponectin with adipocyte fatty acid binding protein in patients with unfavourable dyslipidemic phenotype
- Quality requirements for the determination of glycated hemoglobin HbA1c and possibilities of its application for diagnostic purposes
- Unification and validation of reference intervals – pilot study
- Comparison of creatinine clearance and estimated glomerular filtration rate in patients with chronic kidney disease
- Clinical Biochemistry and Metabolism
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Comparison of creatinine clearance and estimated glomerular filtration rate in patients with chronic kidney disease
- Unification and validation of reference intervals – pilot study
- Quality requirements for the determination of glycated hemoglobin HbA1c and possibilities of its application for diagnostic purposes
- Positive association of adiponectin with adipocyte fatty acid binding protein in patients with unfavourable dyslipidemic phenotype
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

