-
Medical journals
- Career
3D maxillofacial surgery planning – one decade development of technology
Authors: D. Hrušák; L. Hauer; J. Genčur; A. Pěnkava; Ch. Micopulos
Authors‘ workplace: Department of Stomatology, University Hospital and Faculty of Medicine in Pilsen, Charles University in Prague, Czech Republic
Published in: ACTA CHIRURGIAE PLASTICAE, 65, 3-4, 2023, pp. 128-139
doi: https://doi.org/10.48095/ccachp2023128Introduction
The term computer-aided design (CAD) was first used by Douglas T. Ross, a researcher at Massachusetts Institute of Technology in the early 1950s. Pierre Bézier, an engineer at Renault, created the first true 3D CAD/computer-aided manufacturing (CAM) program between 1966 and 1968 [1].
The progress in computer technology overwhelmed the “Moore’s law” (a prediction made by American engineer Gordon Moore in 1965 that the number of transistors per silicon chip doubles every year) is closely followed by software (SW) improvement [2].
For medical use, another 3D invention was essential, the computed tomography scanner (usually abbreviated to a CT scan; formerly called computed axial tomography scan or CT scan) awarded in 1979 Nobel prize in Medicine to Hounsfield and Cormack [3].
At the beginning, all CT images (2D images only) were available on large plain film sheets, a true 3D evaluation and views was possible only in person beside the CT console. True 3D evaluation of CT data started around 2003 when the hardware (HW) and SW tools enabled the export of digital imaging and communications in medicine (DICOM) data to local computers and 3D DICOM viewers became standard.
From rapid prototyping (RP) in 1981, when Hideo Kodama was trying to find a way to develop a RP system. It was just a short way to 1983 and Chuck Hull’s first-ever 3D printed part using stereolithography (STL) (patented 1984) [4].
In 1991, the first 3D scull model was printed. Progress in computer capacity and technologies made 3D easy, accessible for everyone’s purpose and was proven as precise and safe for medical use. Recent progress in virtual surgery planning (VSP), CAD/CAM and 3D printing technologies including 3D laser sintering became accessible and offers the possibility to produce complex patient specific implants (PSI).
1. The past. Plain fi lm analysis. Neither adjustments of the picture nor any other tools like distance measurement were possible. 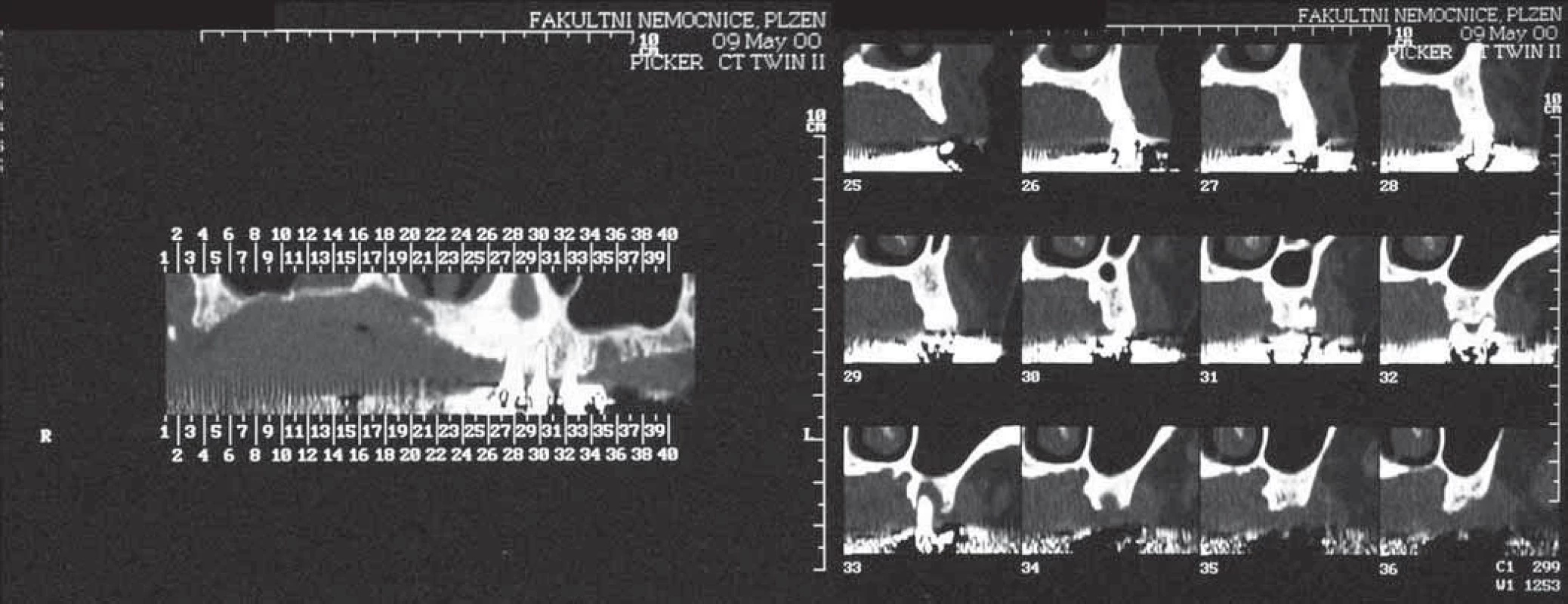
2. CT console at the Radiological department enabled window level setting, (WL – also known as grey-level mapping, or brightness/contrast enhancement), and more detailed analysis by adjustable sectional images and measurements. 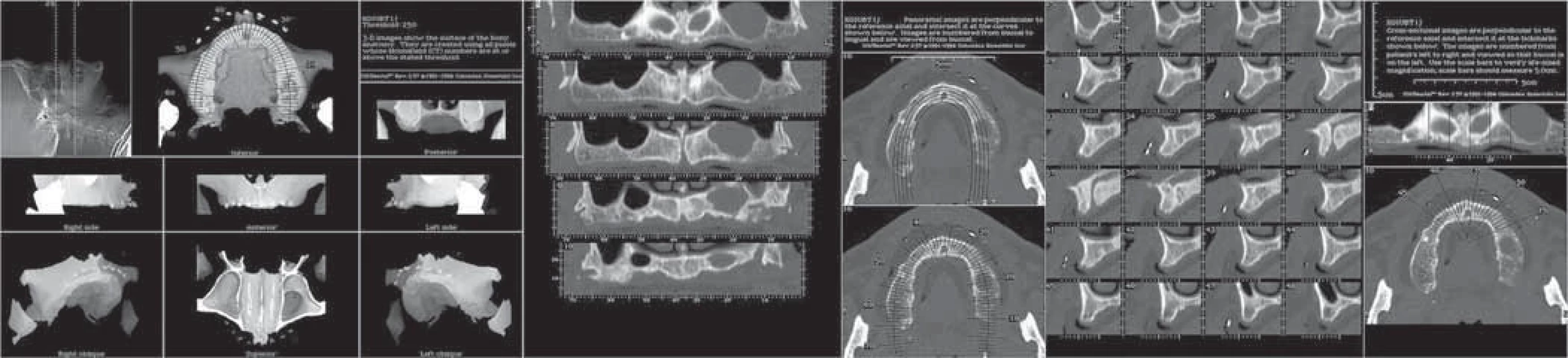
Evaluation of the topic
Surgery planning is as old as the surgery procedures themselves. Any good surgeon, before entering the operating theatre, has a plan for how to proceed. It’s based on knowledge and experience in combination of evaluation all case relevant information.
Thus far, VSP is not a new concept; it can be understood in the traditional way of mindful thinking about how a surgeon proceeds in preparation for and during any surgical procedure.
The recent VSP concept is in the same extent based on the surgeons experience and knowledge, but additionally using high tech SW and HW tools, to achieve a predictable outcome [5–8]
The VSP process includes several stages:
- Input data acquisition is necessary. This requires instant and unlimited access to imaging techniques and data. Imaging in dentistry, dental implantology, orthodontic and orthognathic surgery has evolved from medical CT imaging to cone beam CT (CBCT), providing satisfactory data about bone and teeth structures at minimal irradiation dose.
- The appropriate SW tools must be available. Both commercial SW and freeware data viewers + CAD/CAM SW tools are satisfactory to view raw data, create 3D reconstructions, eventually export file in other 3D formats for specific purposes.
- The most important idea of the surgical procedure and its desired outcome is in the surgeon’s hands. Although the commercial SW companies are offering “treatment planning on demand” by performing standardized procedures and delivering a full package of guaranteed step by step instructions and surgical guides at a price paid by the “per case” principle, the exceptional surgeons role remains irreplaceable. SW robots performing treatment plans based on artificial intelligence and even robotic surgery without human interaction are reported to be just around the corner. In contrary to some enthusiastic reports, I agree with the quote [9], it “is still too little to let the robot “independently” decide the course of the operation”. Seriously, I do believe in human capabilities.
- Output from VSP could be either a visualisation of the procedure or some tool facilitating the preparation for surgery (3D models of surgery steps etc.), perhaps devices used during surgery like cutting guides, templates and similar.

Dental implant simulation SW (eg. SIMplant®) allows virtual positioning of dental implants in the digital image of jaws with possible analysis of the implant/bone dimensions, bone density, prosthetic components positions and much more. 
Sinus lift and implant placement plan using evaluation SW SIMplant® – panoramic view. 3. 
Ridge expansion of the maxilla, CT scan and clinical photograph correlation. 4. 
First true 3D virtually planned surgeries example, laterogenia case; upper row – CT 3D reconstructions; middle row – 3D printed model used for measuring and planning the osteotomies, landmarks resection lines and motion distances drawn directly on the model; bottom row – postoperative CT 3D reconstructions. 5. First true 3D assisted surgery, a lateral mandibular body resection and preshaped load bearing reconstruction plate; upper row 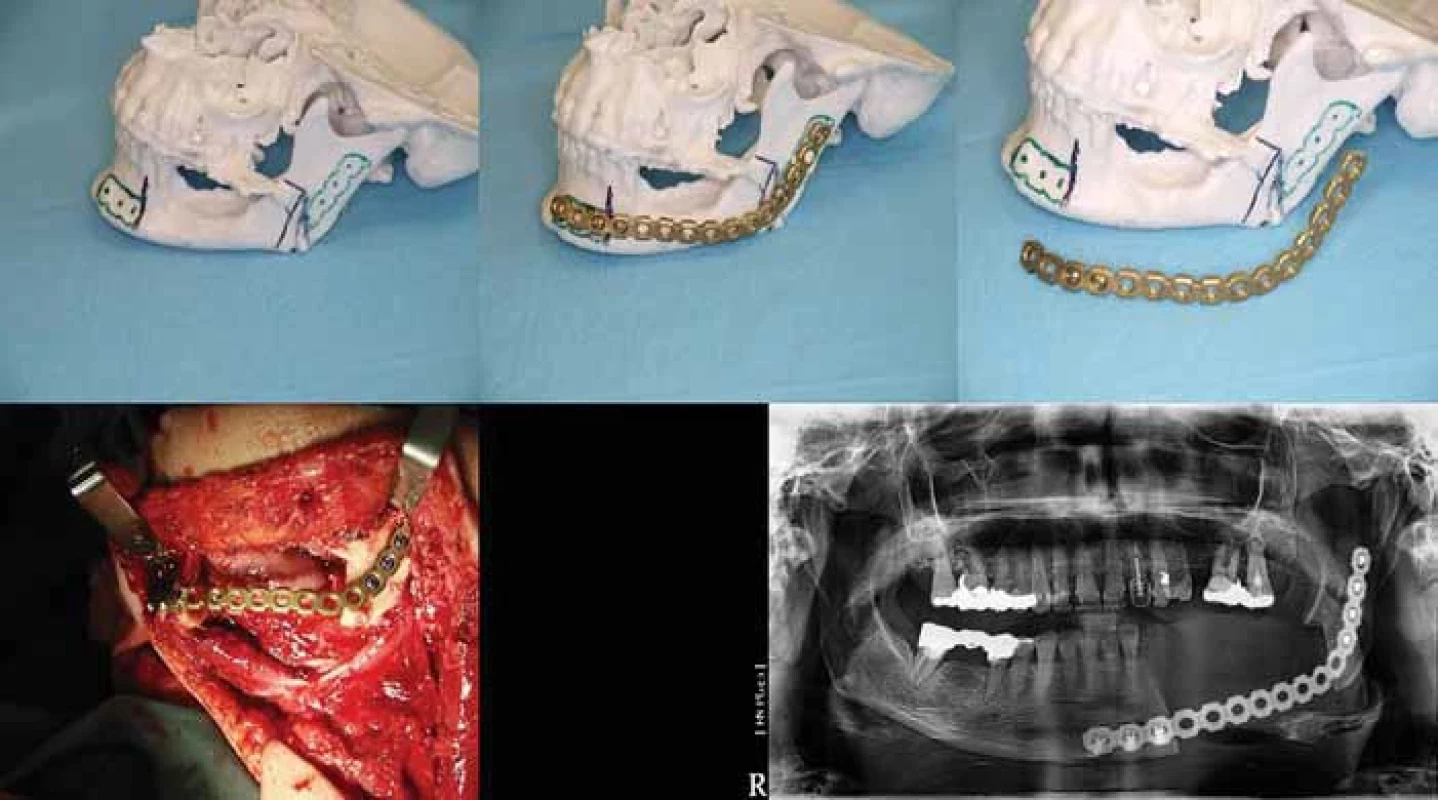
3D printed model with resection lines and reconstruction osteosynthesis plate adapted preoperatively to the mandible; bottom row – intraoperative view, reconstruction osteosynthesis plate bridging the resected part is positioned according to bone landmarks, postoperative OPG showing the correct position of the resected segments. 6. Formlabs Form 1+, a DLP printer; behind the laptop running the PreForm® SW and printed 3D mandible in front. 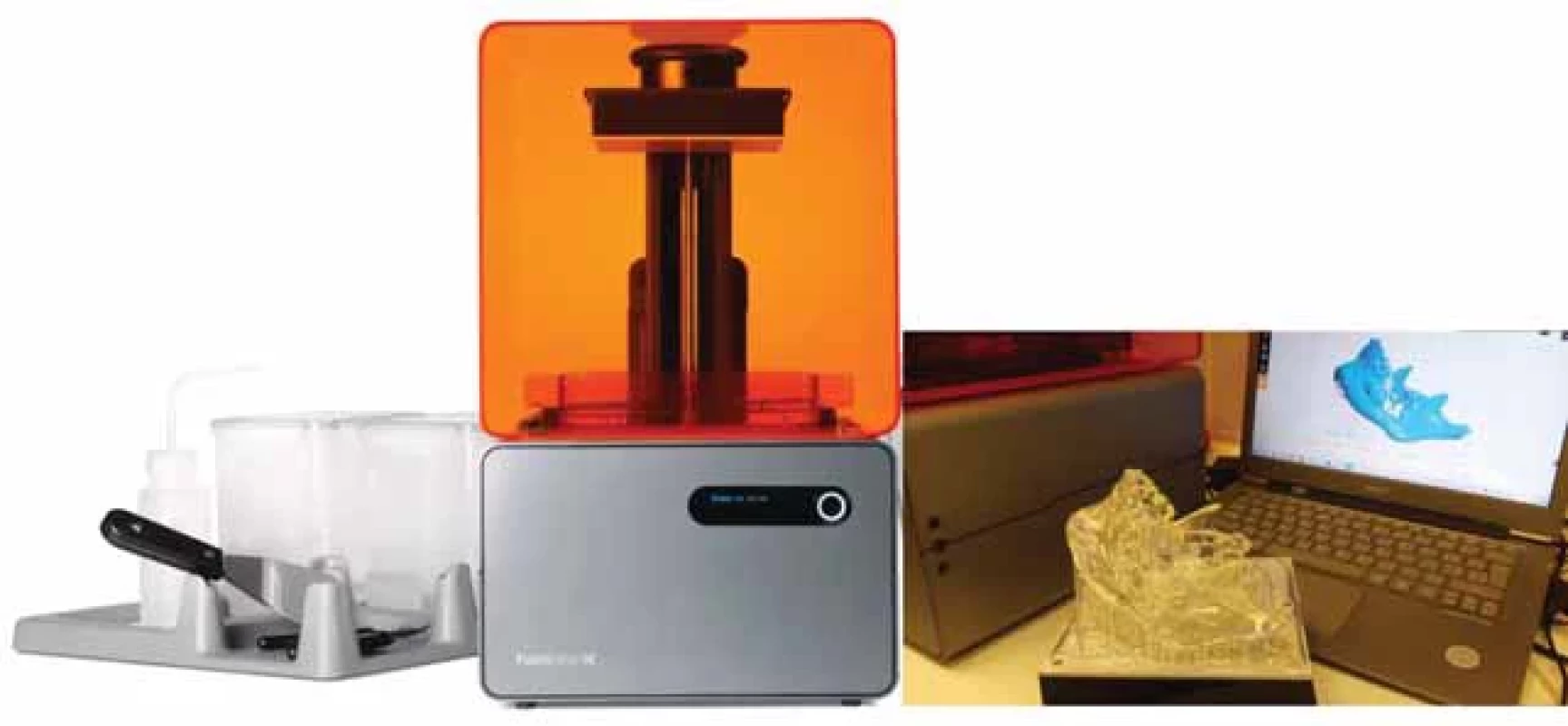
In the past 20 years, we made great progress in surgical techniques and at the same time, we have learned a lot about ways how to use 3D tools and what is behind the simple term VSP.
We like to share with you our experience in presenting the Milestones of 3D planning at the Department of Stomatology, Medical Faculty Pilsen Charles University Prague listed in short bellow:
- 1990–2002: visual inspection of CT scans (2D images only on large plain film sheets) for diagnostic purpose. Occasionally, we accomplished dental implant treatment plans based on plain film analysis (Fig. 1). In 2002–2004, it became possible to explore DICOM data retrieved from the CT directly at the CT console at the Radiological department (Fig. 2). Limited access to 3D data was the reason for occasional use of 3D planning in dental implantology.
- 2004–2009: the change arrived by the “ON demand” availability of DICOM data transfer on CD media. Freeware 3D DICOM viewers (Osirix®, 3Dslicer®, RadiAnt®, InVesalius® and many other) were accessible. Exploring 3D data and retrieving relevant medical information became quicker and easier. We continued the evaluation of dental implant simulation SW (e.q. SIMplant®) (Fig. 3) and it became obvious how useful the 3D imaging technology in planning advanced implant surgery is. Sinus lift (Fig. 4) and alveolar ridge expansion surgeries (Fig. 5) treatment planning have moved to a new level [10].
- 2008–2010: we got first 3D scull models printed from CT scans by an external supplier (Rubeus s. r. o., Plzeň-Štáhlavy using the Z-Corp 3D printer – Binder jet 3D printing technology). Virtual 3D images enhanced the profile analysis, film images switched to digital, 3D printed bone models of the case substituted the plaster models and helped to understand the morphology of the deformity and with “hands on the bone”, it became easier to prepare the osteotomies. In this way, we performed the first true 3D virtually planed surgeries (Fig. 6) and reported some cases in printed papers [11,12] and on international forums and conferences [13–15].
- 2009: we achieved a massive progress in 3D technology by acquiring the first CBCT Vatech Picasso trio to our clinic. The large scale of FOV from 50 × 50 to 150 × 150 mm covered almost every need for facial skeleton and dental imaging. The device specific SW tools (SW Easy Dent®, Ez3D Plus Premium®, EZ3D Implant®) additionally to the diagnostic use enabled also maxillo-mandibular segmentation, simulation of dental implant placement and many other features.
- 2011: we started to use the Onyx Ceph® SW for Orthodontic treatment documentation and treatment plans.
- 2011: direct access to DICOM data implemented in the hospital information system became a great benefit. X-ray images and CBCT data available online with the possibility of importing data directly to the SW tools enhanced the plans for orthodontic and orthognathic procedures.
- 2012 September 25th: we accomplished the first true 3D assisted surgery, a lateral mandibular body resection and pre-shaped load bearing reconstruction plate (Fig. 7).
- 2013: the purchase of the 3shape R7003Shape’s R700™ scanner for orthodontists was a logical consequence of the new era of digital orthodontics. All captured plaster models and impressions since that are kept digitally.
- 2013: the first 3D printer (ultimaker 3D printer) was a fused deposition modelling type device. The outcomes were not suitable for medical purpose.
- 2014: the next printer, Formlabs Form 1+, a digital light processing (DLP) technology changed our lives dramatically. The door to rapid surgery plans was open. It is hard to believe this machine is still in service. Since we have learned how to use all the SW tools, the chain of VSP procedure became completed as a new standard in surgery planning (Fig. 8) [16,17].
Systematically, the process is as follows:
- We need to acquire/import the DICOM data into the proper viewing SW. Eventual segmentation or trimming according to the SW capabilities can be done already at this moment.
- We export the object of surgery (bone, mandible, maxilla, scull) to STL file format or perhaps OBJ (another geometry definition file format). Such as segmentation tools with STL export possibility is a part of most CBCT SW tools delivered in package of CBCT devices.
- The design of the surgical procedure follows. We can modify the objects by segmentation and various other manipulations, for example mirroring of healthy parts of the object into the damaged, modelling of osteosynthesis plates laying on the bone surface etc. (Fig. 9).
- The printout of the digitally planed situation becomes an additional benefit. Having the adequate printer in house makes the process a matter of hours. For successful 3D printing, more adjustments like solidifying the objects or adding sprues may be necessary. This is mainly of advantage in the reconstruction surgery of trauma cases where time plays an important role (Fig. 10).
- And at this time, the most advanced stage of VSP is the PSI design and production. This requires a standardized and certified process of medical device fabrication according to the Medical Device Regulation 2017/745 (MDR) [18].
7. Process of VSP step by step-mandibular resection and fi bula free fl ap reconstruction; upper row 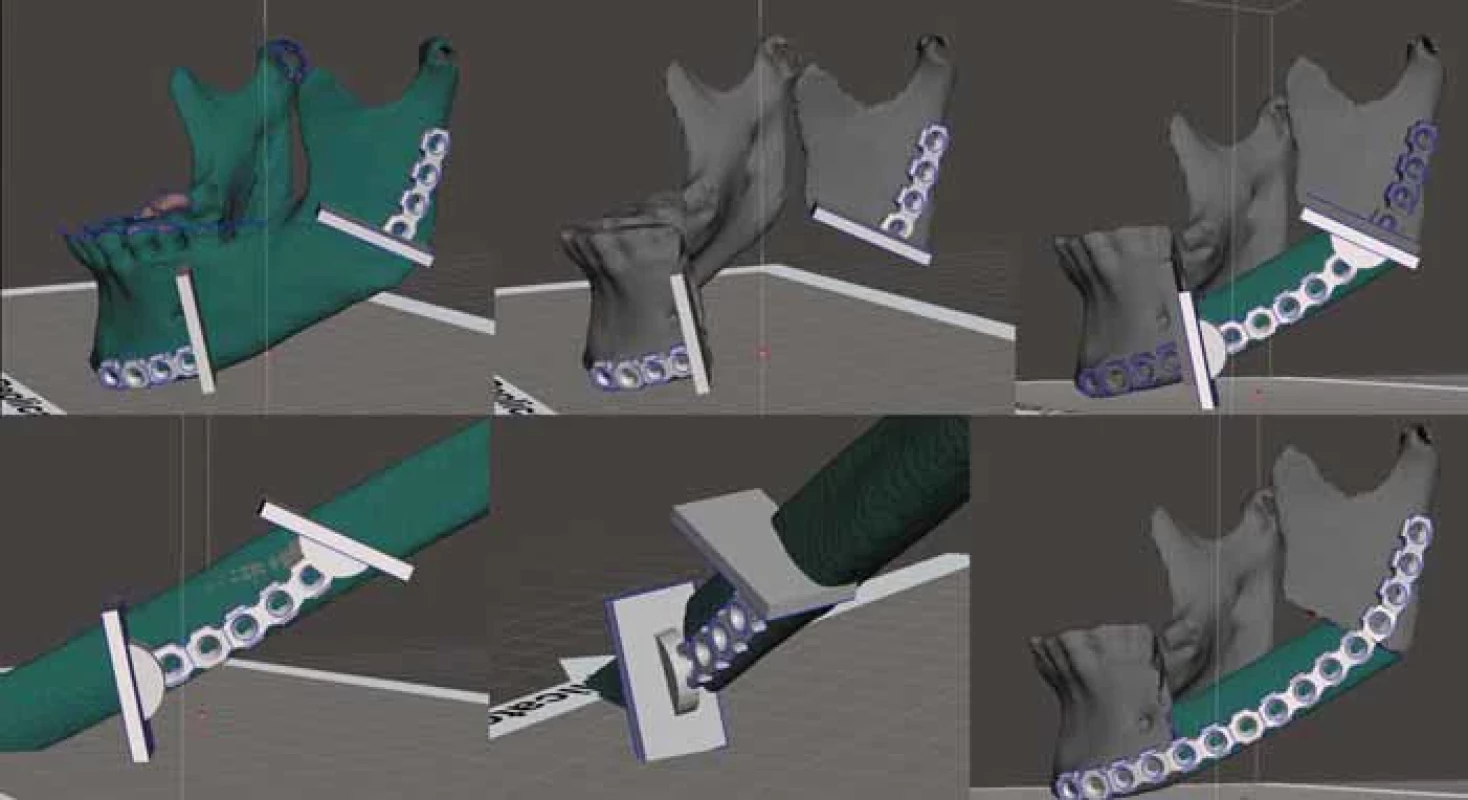
3D virtual model of the mandible + cutting guides, virtual mandibular resection, virtual fi lling the resected gap by fi bula graft with cutting guides on; bottom row – fi bula graft with cutting guide position, virtual plan fi nal situation, resection gap fi lled precisely by fi bula graft and proper shape of the reconstruction plate. Plan performed by the author using only open-source SW tools (Osirix®, FreeCAD, autodesk meshmixer). - 2016: obtaining of our first intraoral scanner (3 Shape TRIOS®) enabled the primary digitalization of dental arches and occlusion and finalised the complete process of digital orthodontics. At this time, we also explored the possibilities and usefulness of optical facial 3D scanners like Structure SDK® http: //structure.io/ or 3DmD® scanner https: //3dmd.com/ but we decided not to follow this thread.
- 2018: purchase of additional i.o. scanners + dental lab equipment for dental CAD/CAM technology, scanner + SW + Milling station, changed the traditional prosthetic technologies to digital.
- 2019: buying our next DLP printer (EnvisioTec Vida M-Type) as an extension to the recent CAD/CAM prosthodontic laboratory equipment extended the digital workflow of many surgical procedures. Printing of occlusal splints, templates and surgical guides for dental implantology since that is a routine.
- 2019: first attempts for VSP in oncological resections and reconstruction using commercial services. At stage one the VSP was without PSI (Fig. 11).
- 2020: a new advanced CBCT device, (KaVo OP 3D Vision®) moved our capabilities to a higher level. Invivo6 Anatomage® advanced medical SW enclosing all necessary components, namely the dental implant-, orthognaticand medical design-planning module allowed us to perform instantly surgery plans.
- 2022: we got two advanced 3shape intraoral scanners for the prosthodontic department. This changed the practice for dental implant planning. The past principle “place implant first where possible, then adapt the prosthodontic” was substituted by the “backward planning” approach.
- 2022: first prosthetic PSI for dental rehabilitation of an atrophic edentulous jaw was implanted.
8. 
Trauma case 1. Severely displaced double mandibular fracture, virtual plan and surgery supported by 3D VSP; upper row – 3D view of DICOM data, virtually separated mandible exported to printer SW; bottom row – the 3D printed model of the fractured mandible is reduced under visual control and the reconstruction plate is aligned; perioperative view – the plate fi ts to the restored mandibular arch. 9. 
VSP in oncological resections and reconstruction supported by commercial 3D surgery planning support. Instructions for use delivered with the models and cutting guides. First cases supported by cutting guides and jaw reconstruction models for preoperative adjustment of the osteosynthesis plate without PSI. 10. 
Guided dental implant surgery (all on four VSP digital plan); upper row – 3D virtual implantation of four dental implants in the mandible, implant position determined by the favourite denture position, design of the drilling guide to maintain the precise implant position; bottom row – perioperative view – the drilling guide with drill sleeves and direction pins, postoperative CBCT shows that the position of the inserted implants correspond to the plan. Plan performed by the authors using licenced open-source SW tools (Anatomage®, Blenderfordental®, InLab®, FreeCAD®, Autodesk meshmixer®). Discussion
Recently, the focus of 3D VSP and advanced oral and maxillofacial surgery is in the application for:
Dental implantology
CBCT and 3D planning is the golden standard in dental implantology. Precise implant positioning according to the optimal prosthodontic restoration, respecting occlusal and aesthetic needs is mandatory. Combinations and virtual merging of CBCT data, occlusal scans, and virtual dental restoration plan models is necessary to become optimal results. The “backward planning” approach is an acronym for all the efforts made before surgery to achieve the desired outcome (Fig. 12) [19].
The number of dental implantation cases including sinus lift and augmentation surgeries since 2009 is uncountable. Cases of severe atrophic jaws represent the recent next level challenge in dental restoration [20]. Currently, we are on the way to patient specific subperiosteally placed implants. Simplified workflow begins with acquiring CBCT scans of the jawbone and later bone segmentation. For the segmented bone adjustments, smoothening and undercuts out blocking we use 3D SW simulation (InLab®, Exocad®). The virtual model of bone is exported to STL and merged with intraoral scans and teeth wax-up of the future prosthodontic restorations for the correct attachments support location. Finally, the PSI framework itself is virtually designed (CAD/CAM SW – Blenderfordental®) (Fig. 13) and we send the complete PSI file online to the production company. Manufacturing is done offsite by either milling or Laser sintering from medically approved titanium. Sterilised, we receive the PSI ready to use for implantation. After the surgical procedure, the immediate dental prosthodontic restoration is usually attached.
Orthognatic surgery
Since the CBCT is a regular part of the preoperative analysis in all orthognatic cases; the same in 3D surgery planning is standard [21]. Virtual 3D images of the facial bones, skeletal segmentations and simulations of segment movements to their predicted position to fulfil the profile analysis goals, 3D printed positioning devices (perioperative occlusal splints) eventually bone models of the case help to prepare for the osteotomies with “hands on the bone” prior to the real surgery (Fig. 14).
11. 
Patient specifi c subperiosteally placed dental implant case design. First, the 3D reconstruction of the mandible with marking the mandibular and mental nerve extracted from CBCT. Dental prosthodontic plan gives the necessary position of the abutment posts. The framework is designed to give suffi cient support and retention. Plan performed by the authors using licenced and open-source SW tools (Anatomage®, Blender for dental®, InLab®). 12. 
Orthognathic case 3D surgery planning using IPS® CaseDesigner; upper row – the DICOM data are imported into the SW, segmentation according to the type of surgery is made by the use of the application’s SW tools; bottom row – after the necessary manipulation of the segmented parts is done, to transfer the fi nal occlusal changes into the operating theatre, occlusal splints are printed. Traumatology
Comminuted facial fractures represent the most puzzling cases to obtain successful results following surgical treatment. 3D visualisation is mandatory to recognise the fracture pattern. Restoring the original shape of the bone profile is the key to functional and aesthetic outcomes. 3D processing of DICOM data by SW tools enable the surgeon to reconstruct virtually pre surgically the shape and position of any fragment eventually prepare a model of the restored area to prepare the appropriate HW (Fig. 15).
Reconstructive surgery
As reported above the process follows five steps:
- acquiring / import / manipulating the DICOM data;
- export the object of surgery (bone, mandible, maxilla, skull – to STL OBJ file);
- design of the procedure, segmentation and, adding components (HW plates, bone grafts);
- 3D print of the surgery plan, (incl. templates, cutting guides etc.);
- PSI design and production.
13. 
Trauma case 2. Reconstruction of a severely damaged orbito-zygomatic fracture; upper row – segmentation of the intact contralateral skeleton, mirroring and aligning it to the damaged location. The printed part is used as a template for osteosynthesis HW preparation. Bottom row – the printed and sterilized skull model is used during surgery as a reference to restore the shape of the comminuted skeleton. The number of cases since we have started with VSP of oncological resections (2012), supported by in house 3D printing (2014), attacks the one hundred hurdles. In 2017 we initiated the cooperation with the department of plastic surgery for microvascular flaps orofacial reconstructions. The fibula osteomyocutaneous flap for mandible reconstruction is a standardised and versatile enough procedure, which is excellent in combination with 3D VSP a PSI (Fig. 16). Since 2019 the commercial service of 3D VSP and PSI by a Czech based company at reasonable prices is available and we use PSI regularly. Up to now, there are 30 records of PSI surgeries (Tab. 1). Our own experience is in agreement with the conclusion the VSP surgeries of oncological/reconstruction cases reduces the operating times as reported in [22].
14. 
Advance in VSP in oncological resections and reconstruction. The fi bula osteomyocutaneous fl ap for mandible reconstruction in combination with 3D VSP a PSI. The commercial service of 3D VSP and PSI by a Czech based company with online interactive model consultation. Instructions for use delivered with the models cutting guides and sterilised PSI. 1. VSP + PSI procedures 2019–2023, types of surgeries. 
JRC – cutting guide and surgery models for presurgical bending of conventional reconstruction plates,
JRF – titanium cutting guide, individually designed and fabricated reconstruction plate patient specifi c implant (PSI), fi bula free fl ap,
JRI – titanium cutting guide, individually designed and fabricated reconstruction plate PSI, VSP – virtual surgery planning, SUM – total cases reviewedConclusion
In the past almost 20 years, we gathered some experience in using viewing and medical design SW tools. We have explored both commercial SW (e. g. Materialise Mimics®, ProPlan CMF®, CMF Connect®, SimPlant®, 3D Planner, Dolphin®, Onyx Ceph®, Ez3D Plus Premium®, InVivo6®, In Lab®, Blender®, Exocad®) and open-source data viewers SW (e. g. Osirix®, Radiant®, 3D slicer®, Automesh®, Meshmixer®, FreeCAD®, Shapr3D®).
Along the 3D SW dedicated tools, 3D printers proved to be precise enough to achieve perfect outcomes for surgery planning. The access to commercial 3D VSP and PSI becomes easy and affordable, surgeons must not overestimate the technology to prevent failures of surgeries [23].
It is comfortable, quick and easy to buy and use a bundled box of SW + commercial 3D surgery planning support (once you can afford). However, sometimes such approach, just executing instructions given by the designers, can make oneself blind and not capable to solve unexpected situations. The idea “let the company solve any problem for the money I have spent” does not work well in the operating theatre. It is always the surgeon’s responsibility for conducting the perfect outcome of any surgery. Hence, a close communication between the doctor and the technical designer/producer is necessary. On the other hand, using open-source SW promotes creativity, expands and grows new own ideas.
There is much to learn from the past, there are several reasons to review our own history and experience in looking forward and seeking new pathways. No matter how perfect the technology will grow, a skilled surgeon will always be indispensable. Myself, I have spent hundreds, maybe thousands of hours on my PC during the past 40 years simulating surgeries, exploring SW tools, and pioneering the use of 3D technologies in medicine. I never regret.
Roles of authors
Daniel Hrušák – main author, summarizing the topic, most of the performed VSP cases;Lukáš Hauer – VSP of reconstructive surgery cases;Jiří Genčur – VSP of orthognathic surgery cases;Adam Pěnkava – VSP of dental implantology cases;Christos Micopulos – reviewing patients records of VSP cases.Disclosure: The authors declare “no conflict of interest” and that all materials (schemas, images, charts, tables, etc.) in the paper are of own intellectual property of the authors. All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Sources
1. The history – and future – of CAD/CAM technology. [online]. Available from: https: //www.thomasnet.com/insights/the-history-and-future-of-cad-cam-technology/.
2. 60 years of CAD infographic: the history of CAD since 1957. [online]. Available from: https: //partsolutions.com/60-years-of-cad-infographic-the-history-of-cad-since-1957/.
3. Cormack AN., Godfrez N. The Nobel prize in physiology or medicine 1979. [online]. Available from: https: //www.nobelprize.org/ prizes/medicine/1979/press-release/.
4. The history of 3D printing in 3 phases. [online]. Available from: https: //www.bcn3d.com/the-history-of-3d-printing-when-was-3d-printing-invented/.
5. Myers PL., Nelson JA., Rosen EB., et al. Virtual surgical planning for oncologic mandibular and maxillary reconstruction. Plast Reconstr Surg Glob Open. 2021, 9 (9): e3672.
6. Maisi S., Dominguez M., Charmaine Gilong P., et al. In-house virtual surgical planning for mandibular reconstruction with fibula free flap: case series and literature review. Ann 3D Printed Med. 2023, 10 : 100109.
7. Myers PL., Nelson JA., Rosen EB., et al. Virtual surgical planning for oncologic mandibular and maxillary reconstruction. Plast Reconstr Surg Glob Open. 2021, 9 (9): e3672.
8. Barr ML., Haveles CS., Rezzadeh KS., et al. Virtual surgical planning for mandibular reconstruction with the fibula free flap: a systematic review and meta-analysis. Ann Plast Surg. 2020, 84 (1): 117–122.
9. Strzelecki R. Artificial intelligence – for good health. [online]. Available from: https: //www. forbes.com/sites/forbestechcouncil/2023/06/ 09/artificial-intelligence-for-good-health/?sh=7f9d167a5525.
10. Hrušák D., Walter J., Ferda J. CT v dentální implantologii. Mezinárodní sympozium „Implantologie bez hranic“. 2004.
11. Hrušák D. 3D postupy v maxillofaciální chirurgii. V. Plzeňské pracovní dny. 2008.
12. Moztarzadeh O., Hrušák D., Bolek L., et al. On site 3D printing in oral and maxillofacial surgery. Plzen Lek Sborn. 2015, 81 : 29–32.
13. Hrusak D. Lateral mandibular body ostectomy in the treatment of laterogenia. 1st Baltic conference on orthognathic surgery (BSCOSO 2009). Baltic Dent Maxillofac. 2009, 11 (2).
14. Hrusak D. Surgical treatment of laterogenia – a report of four different surgery plans XX. EACMFS congress Brugges. 2010.
15. Hrusak D. On site 3D printing in oral and maxilofacial surgery for trauma and oncological bone reconstruction. Int J Oral Maxillofac Surg. 2015, 44: e225–e226.
16. Hrušák D. 3D technologie v maxilofaciální traumatologii. International Congress Prague dental days. 2016.
17. Jambura J., Hrušák D., Hauer L., et al. Využití 3D technologií v traumatologii obličejového skeletu. XIII. Plzeňské pracovní dny stomatologie. 2016.
18. Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC. [online]. Available from: https: //eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32017R0745.
19. Nilius M., Mueller C., Nilius MH., et al. Advanced backward planning with custom-milled individual allogeneic block augmentation for maxillary full-arch osteoplasty and dental implantation: a 3-year follow-up. Cell Tissue Bank. 2022, 23 (2): 335–345.
20. Mommaerts MY. Evolutionary steps in the design and biofunctionalization of the additively manufactured sub-periosteal jaw implant „AMSJI“ for the maxilla. Int J Oral Maxillofac Surg. 2019, 48 (1): 108–114.
21. Willinger K., Guevara-Rojas G., Cede J., et al. Comparison of feasibility, time consumption and costs of three virtual planning systems for surgical correction of midfacial deficiency. Maxillofac Plast Reconstr Surg. 2021, 43 (1): 2.
22. Dioguardi M., Spirito F., Quarta C., et al. Guided dental implant surgery: systematic review. J Clin Med. 2023, 12 (4): 1490.
23. López-Arcas JM., Arias J., Del Castillo JL., et al. The fibula osteomyocutaneous flap for mandible reconstruction: a 15-year experience. J Oral Maxillofac Surg. 2010, 68 (10): 2377–2384.
Daniel Hrušák, MD, PhD
Pod Stráží 21
323 00 Plzeň
e-mail: hrusak@fnplzen.czSubmitted: 17. 8. 2023
Accepted: 2. 2. 2024Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2023 Issue 3-4-
All articles in this issue
- Editorial
- Diagnosis and treatment of Eagle’s syndrome and possible complications
- Scalp arteriovenous malformations – 20 years of experience in a tertiary healthcare centre
- The comparison of effectivity in breast cancer prevention between skin sparing and subcutaneous mastectomy – 20 years of experience
- Avascular necrosis of the maxilla after orthognathic surgery, a devastating complication? A systematic review of reported cases and clinical considerations
- 3D maxillofacial surgery planning – one decade development of technology
- A primary cutaneous carcinosarcoma of the retro auricular region, how to treat and literature review
- Combination of cable ties and barbed sutures for fasciotomy closure – two case reports
- Skin grafting on amputated lower limb, norepinephrine-induced ischemic limb necrosis – case report
- Abdominal wall reconstruction for extensive necrosis following abdominoplasty in a patient with subcostal scars – case report
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Diagnosis and treatment of Eagle’s syndrome and possible complications
- Avascular necrosis of the maxilla after orthognathic surgery, a devastating complication? A systematic review of reported cases and clinical considerations
- 3D maxillofacial surgery planning – one decade development of technology
- Skin grafting on amputated lower limb, norepinephrine-induced ischemic limb necrosis – case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

