-
Medical journals
- Career
When and why to consider the diagnosis of myasthenia gravis in neurological practice, and what treatment options do we currently have?
2. 5. 2023
Myasthenia gravis (MG) is a clinically heterogeneous disease characterized by fluctuating muscle weakness and fatigability that worsens after physical exertion or mental stress. Accurate diagnosis is essential because treatment can lead to permanent remission and full functional capacity of the patient.
Pathogenesis
Myasthenia gravis is a chronic autoimmune disease. In a large portion of patients, antibodies against specific targets on the postsynaptic membrane can be identified and characterized. In most (nearly 85%) patients with generalized MG, these are antibodies against the acetylcholine receptor. Approximately 5% of patients have antibodies against muscle-specific kinase (MuSK), about 2% have antibodies against lipoprotein-related protein 4 (LRP4), and less than 1% have antibodies against agrin. The remaining 5–8% of the population with generalized disease are considered seronegative, unable to find any currently known antigenic targets or antibodies.
Epidemiology
Acquired MG is the most common disease affecting neuromuscular transmission. The prevalence is around 130–150 patients per 1 million inhabitants, with an increasing incidence trend. MG is a disease that can occur at any age but more often affects women. The incidence peaks in women in the 2nd–3rd decade, and in men in the 6th decade.
Clinical Presentation
Typical issues in MG are fluctuating muscle weakness and fatigability of preferentially affected muscle groups. These primarily involve extraocular, facio-pharyngeal, neck, girdle, and possibly respiratory muscles. In MG, there are no sensory disturbances, pain, autonomic dysfunction, or other signs of central or peripheral motoneuron lesions. Initial muscle atrophy or hypotonia is also not typical.
Diagnosis
The diagnosis of MG is based on clinical examination and thorough medical history. No symptom complex is characteristic of MG. The clinical picture may be slightly different for each patient, but it is essential that all dominant symptoms can be explained by weakness of specific muscles or muscle groups. Typical accentuation of muscle weakness occurs in the afternoon and evening hours. Standard neurological examination with MG can show physiological results; hence, it is essential to perform stress tests focusing on commonly affected muscles: Simpson's test, Gorelick's test, Seeman's test. Suspicion of MG can be confirmed by laboratory tests. These include electrophysiological examination, determination of antibodies against acetylcholine receptor (AChR), or CT of the mediastinum, which can reveal thymoma in 12–15% of MG cases.
Common diagnostic errors in MG include underestimating history, especially when patients do not emphasize muscle weakness and fatigability. Diagnosis may be complicated by purely ocular MG, present in approximately 20% of patients, asymmetrical or unilateral involvement in early stages, or weakening of ocular and faciobulbar muscles in older patients, which can mislead to a diagnosis of cerebrovascular disease. Negative antibodies against AChR do not rule out MG if other diagnostic criteria are met. CT of the mediastinum is sufficient to document potential thymoma; MRI is not necessary.
Basic Treatment Strategies
The prognosis of MG depends on early diagnosis and the introduction of appropriate therapy. With timely intervention, clinical remission can be achieved in over 90% of patients, either with pharmacological support or entirely without therapy. The best prognosis is for young patients without comorbid conditions with thymic hyperplasia following thymectomy.
There are four primary therapeutic options for MG. These include acetylcholinesterase inhibitors, which increase the availability of acetylcholine at the neuromuscular junction – a symptomatic treatment. Due to the autoimmune nature of the disease, most patients also receive chronic immunotherapy such as glucocorticoids, non-steroidal immunosuppressants, and immunomodulatory drugs, or short-term but rapidly acting immunomodulatory treatment – therapeutic plasmapheresis and i.v. immunoglobulins. In cases of thymic hyperplasia, thymectomy may be considered.
The goal of therapy is to minimize symptoms with minimal side effects. It is also necessary to avoid administering drugs that can exacerbate MG (fluoroquinolones, aminoglycosides, i.v. lidocaine, magnesium, PD-L1 inhibitors, etc.).
New Therapeutic Options
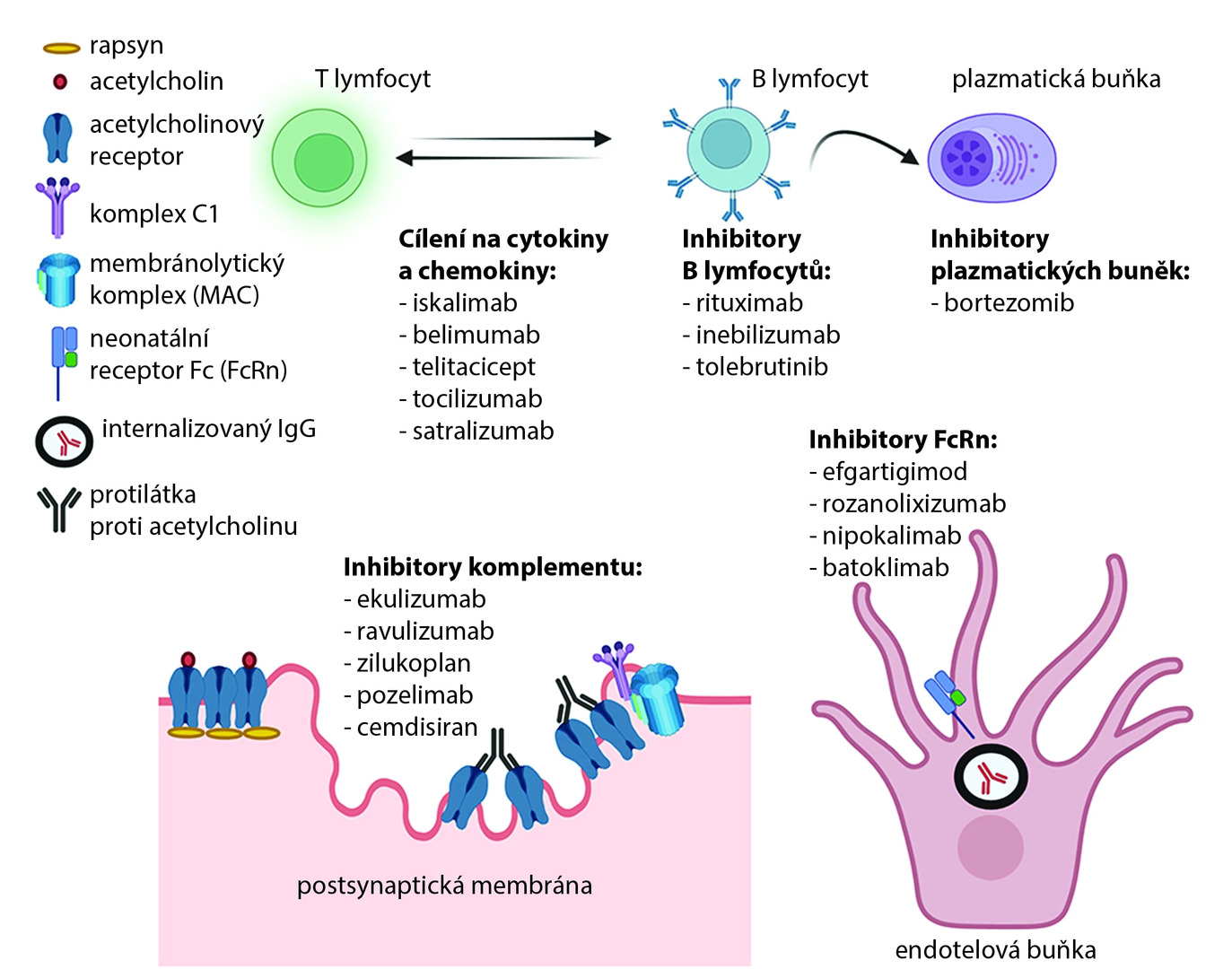
In the last decade, several new immunotherapies have been evaluated in clinical trials, mostly targeting specific cells and immune pathways implicated in MG pathogenesis. The most successful have been complement pathway inhibition and targeting the neonatal Fc receptor (FcRn), which inhibits IgG recycling. Successful inhibition of B and T lymphocytes has also been demonstrated, either through direct depletion or cytokine regulation. Several drugs (eculizumab, ravulizumab, and efgartigimod) have already received regulatory approval, yet most of these new molecules are still in various stages of clinical development.
Fig. Targets of new drugs in MG therapy (1)
Conclusion
MG is a chronic but treatable disease. Full remission can be achieved in most patients. Therefore, it is crucial to consider this disease in practice to allow timely diagnosis and treatment.
(zza)
Sources:
1. Nair S. S., Jacob S. Novel immunotherapies for myasthenia gravis. Immunotargets Ther 2023 Apr 4; 12 : 25–45, doi: 10.2147/ITT.S377056.
2. Bird S. J. Overview of the treatment of myasthenia gravis. UpToDate, 2023 Mar 31. Available at: www.uptodate.com/contents/overview-of-the-treatment-of-myasthenia-gravis
3. Týblová M., Piťha J. et al. List of risk drugs and toxins in MG. MyastheniaGravis.cz, 2023. Available at: www.myastheniagravis.cz/images/rizikov_lky_internet-2.doc
4. Piťha J. Practical experiences with clinical diagnosis of myasthenia gravis. Neurology for practice 2010; 11 : 90–94.
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Labels
Paediatric neurology Neurology
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


