-
Medical journals
- Career
Digital Bridge Between the Brain and Spine: How an Implant Restored Walking Ability to a Paralyzed Patient − Case Study
4. 3. 2024
When a spinal cord injury occurs, communication between the brain and peripheral nerves is interrupted, causing paralysis. Until recently, it was not possible to restore mobility for most of these patients. Last year, however, a team led by specialists from Lausanne, Switzerland, published their results on an implant that digitally bridged the spinal injury of a tetraplegic patient.
Is it possible to walk with a disconnected brain?
When walking, the brain sends signals to the neurons stored in the lumbar region of the spine. Although most spinal cord injuries do not directly damage these nerve cells, the interruption of descending pathways practically disconnects this area from the brain, leading to permanent paralysis.
The authors of the cited publication in their previous work proved that direct electrical stimulation of the lumbosacral neurons can activate them, thus restoring the ability to stand and walk in paralyzed patients. However, the technique required a number of sensors that tried to "guess" the intent of the wearer based on residual movements or compensation strategies. The walk was thus not completely natural, and patients had difficulty adapting to changing terrain or their voluntary requirements.
Brain/Spine Communication Interface
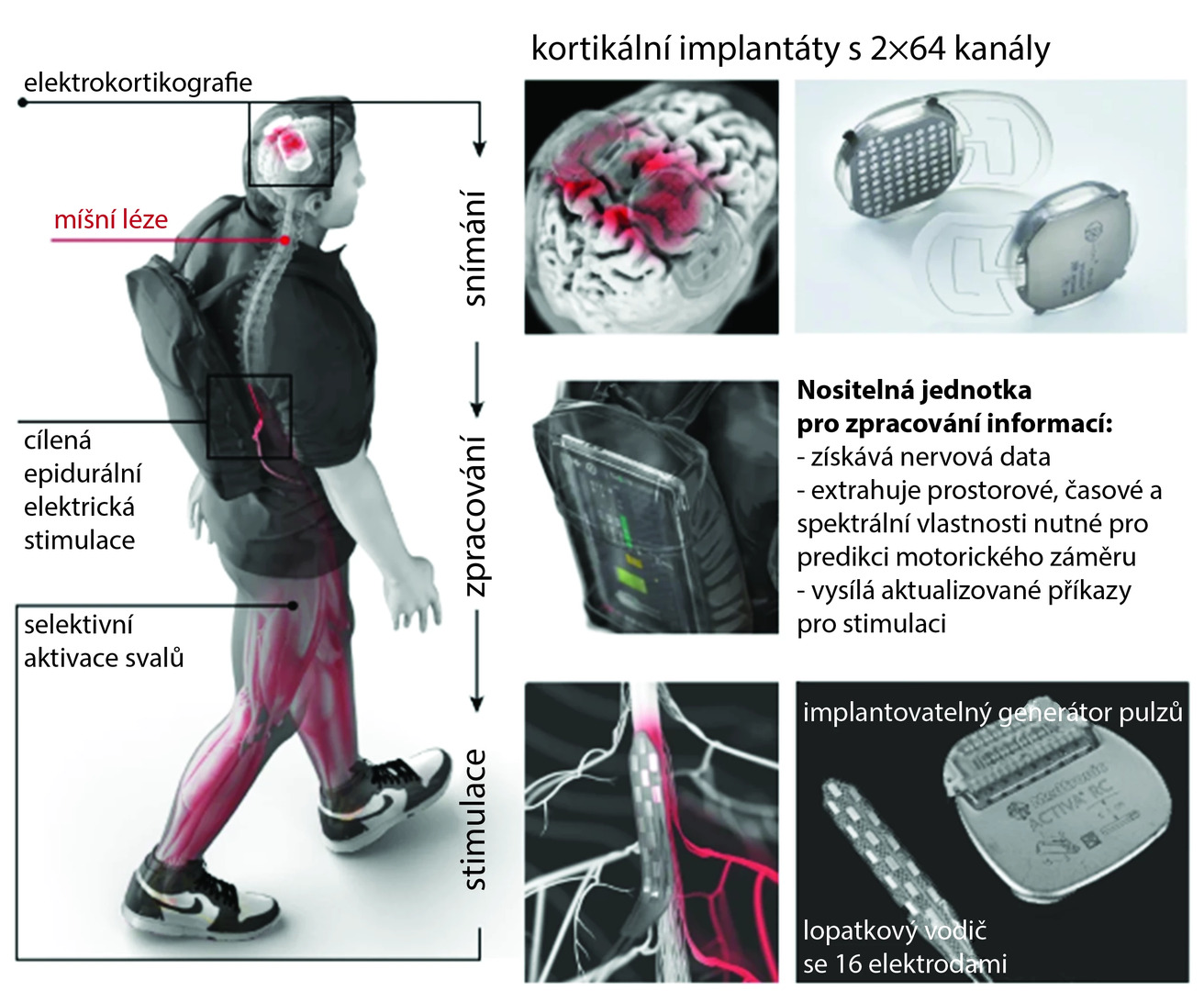
The researchers therefore proposed to digitally bridge the interrupted communication between the brain and spinal cord to enable the patient to control the timing and intensity of lower limb muscle activity voluntarily. They managed to integrate 2 fully implanted systems wirelessly, which together allow brain cortex activity to be monitored and lumbosacral spinal cord stimulation in real time (see fig.).
Fig. Design, technology, and implantation of the brain/spine digital interface
The interface was implanted in a 38-year-old man who suffered an incomplete spinal cord injury in the 5th and 6th cervical vertebrae area 10 years ago in a cycling accident. This patient had previously participated in a 5-month pilot neurorehabilitation program using direct epidural spinal stimulation. During this rehabilitation, he regained the ability to walk with the aid of a walker. However, despite daily stimulation for 3 years, no further progress was achieved.
Implant Placement and Calibration
For the implantation of the interface, it was first necessary to determine with maximum precision, using imaging techniques, which areas of the patient's brain respond best to the attempted movement of a given limb. During the neurosurgical procedure, 2 small sections of the patient's skull bone were replaced with the implanted recording device. The stimulation implant in the lumbar part of the spinal cord had already been implanted from the previous study.
Then, the researchers precisely mapped which areas of the intracranial implant corresponded to voluntary limb movements of the patient and configured the stimulation implant to respond correctly to these signals. They prepared a kind of library of targeted stimulation programs that mobilized the hip, knee, and ankle joints on the given side of the body and also allowed gradual control over the activity of the targeted muscle groups. They also developed adaptive algorithms capable of predicting the probability of intentional joint movement, its amplitude, and direction. The epidural stimulator received signals every 300 ms.
Gradual Progress and Return to (Almost) Normal Life
The researchers worked on the gradual calibration of the interface, and the patient gradually became able to walk with crutches with the free decision to start walking, walk continuously, or stop and remain standing. The interface allowed him to walk on inclined planes, up stairs, and on uneven terrain. The signal quality and decoding accuracy of the intracranial implant remained unchanged during almost a year of use.
However, the main goal of the study was to determine whether rehabilitation using the digital interface could improve neurological recovery. The epidural stimulator itself restored the patient's ability to voluntarily control previously paralyzed muscles and improved his ability to stand and walk, but during the 3 years of use, a plateau was reached.
After the interface was implanted, the patient underwent 40 rehabilitation training sessions, focusing particularly on the hip flexors most affected by the paralysis. Evaluations with the interface turned off improved in all assessed areas of standing and walking quality, and sensory sensitivity in the affected areas also improved. The patient reported a significant improvement in quality of life, such as being able to move independently around his home, get in and out of a car, or have a drink with friends standing at a bar.
(este)
Source: Lorach H., Galvez A., Spagnolo V. et al. Walking naturally after spinal cord injury using a brain-spine interface. Nature 2023; 618 : 126–133, doi: 10.1038/s41586-023-06094-5.
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
Popular this week- Oncology Care Coordinators Will Shorten Patients’ Journey Through the System
- AI Will Help Personalize the Treatment of Atrial Fibrillation
- How Could the Gut Microbiota Be Linked to a Higher Risk of Abdominal Aortic Aneurysm Progression?
- Czech Gastroenterology Keeps Up with the Times. For 80 Years
- Why Endometriosis Requires the Principles of Precision Medicine
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

