-
Medical journals
- Career
Total glenoid fractures
Authors: J. Bartonicek 1; M. Tucek 1; D. Klika 2; P. Obruba 3
Authors‘ workplace: Department of Orthopaedics, 1st Faculty of Medicine of Charles University and Central Military Hospital, Prague, Head of Department: Prof. MUDr. J. Bartoníček, DrSc. 1; Department of Radiology, Central Military Hospital, Prague, Head of Department: MUDr. T Belšan, CSc. 2; Department of Trauma of Masaryk Hospital and Jan Evengelista Purkyně University, Ustí nad Labem, Head of Department: MUDr. K. Edelmann, Ph. D. 3
Published in: Rozhl. Chir., 2016, roč. 95, č. 11, s. 386-393.
Category: Original articles
Overview
Introduction:
Fractures affecting the entire glenoid fossa are termed comminuted or total glenoid fractures. However, there are no detailed studies of total glenoid fractures, and only brief mentions can be found in the literature.Methods:
The group comprised 12 patients (mean age, 39 years), who sustained 13 fractures of the glenoid fossa. In all the fractures, all parts of the glenoid fossa were separated from the scapular neck or body. In total 5 patients (6 fractures) were treated non-operatively and 7 patients were operated on. The method of treatment was based on displacement of the fragments, the patient´s general and local conditions. Indication for operative treatment was displacement of articular fragments of more than 3mm. This criterion was met by 10 patients (11 fractures). Owing to the general or local condition, operation was contraindicated in 2 patients with 3 fractures; one patient refused the operation. One patient with a bilateral fracture was lost to follow-up.Results:
According to the site of separation of articular fragments, the fractures were divided into three groups – the separation line passed through the anatomical neck; through the coracoid process or surgical neck of the scapula; or through the scapular body. In 6 of the 7 operated patients, a good or very good result was achieved. In 2 patients with minimal fragment dislocation treated non-operatively, the fractures healed in an anatomical position and full range of motion was achieved. In 2 patients with severe fragment displacement treated non-operatively, the healing resulted in glenoid fossa incongruence and painful and limited range of motion.Conclusion:
Fractures of the entire glenoid fossa are the most severe injuries to scapula. Their diagnosis requires CT examination, including 3D CT reconstruction with subtraction of the surrounding bones. Displaced fractures are indicated for operative treatment from the Judet approach.Key words:
scapular fractures − glenoid fractures − classification, operative treatment − Judet approachIntroduction
Most intraarticular fractures involve only part of the glenoid fossa, with the intact portion of the articular surface remaining in normal anatomical relationship with the scapular neck or scapular body. Fractures affecting the entire glenoid fossa are termed comminuted or total glenoid fractures in the current classifications which present them mostly in a rather schematic and unrealistic manner [1−10]. However, there are no detailed studies of total glenoid fractures, and only brief mentions can be found in the literature in this respect. Our analysis of CT scans of 90 glenoid fractures revealed 10 cases when all fragments of the glenoid fossa were separated from the scapular neck or body [11]. Subsequently, we recorded another three similar cases. Analysis of the resulting group of 13 fractures in 12 patients was the subject of the present study.
Methods
Group of patients: The group comprised 12 patients (7 men, 5 women), with the mean age of 39.4 years (range, 17−71), who sustained 13 fractures of the glenoid fossa; 8 on the right and 5 on the left side (Tab. 1). In all fractures, all parts of the glenoid fossa were separated from the scapular neck or body.
1. Total glenoid fractures 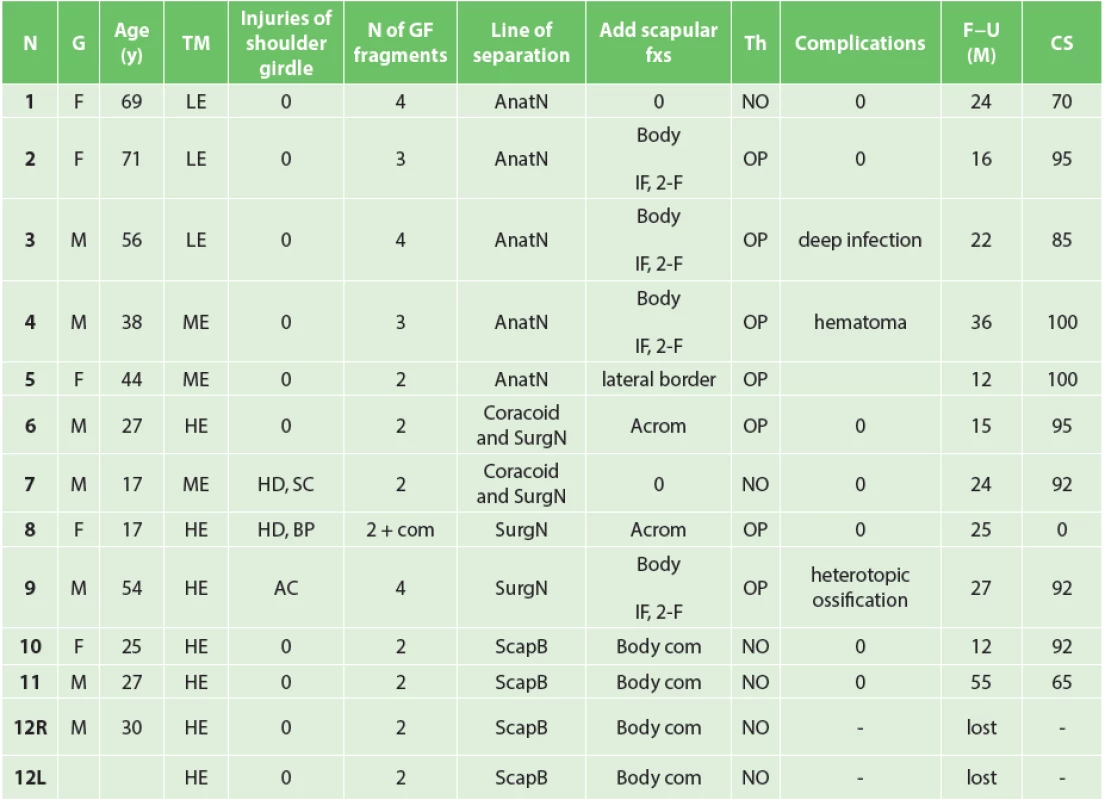
Group of patients. F – female, M – male, LE – low energy trauma, ME – mid energy trauma, HE – high energy trauma, HD – humeral diaphysis, SC – dislocation of sternoclavicular joint, AC – dislocation of acromioclavicular joint, BP – brachial plexus injury, com – comminuted, GF – glenoid fossa, AnatN – anatomic neck, SurgN – surgical neck, ScapB – scapular body, IF – infraspinous part, 2-F – two fragment, Acrom – Acromion, NO – non operative, OP – operative, Complic – complications, F-U – follow-up, lost – lost for follow-up, CS – Constant score. In 3 older patients (Pts 1, 2, 3), the fracture was caused by a simple fall, in another 3 patients by medium-energy trauma (Pts 4, 5, 6), namely by fall from a bicycle or motorcycle at low speed. In 6 patients (Pts 7−12), one of which sustained a bilateral fracture (Pt 12), the injury resulted from a high-energy mechanism; of these, 3 times from a vehicle car accident, once it was caused by fall from a motorcycle at high speed, once by fall from a great height, and once it was sustained by a girl walking along the railroad tracks, who was hit straight in her shoulder by railway carriage step (Pt 8). In 1 case of high-energy trauma the fracture was open (Pt 11).
Methods: In 6 non polytraumatized patients, AP radiographs of the affected shoulder girdle were taken, including Neer I and II views. All 12 patients underwent CT examination, including 3D CT reconstruction with subtraction of the humeral head, ribs and clavicle from the anterior and posterolateral views [12].
In total, 5 patients (6 fractures) were treated non-operatively and 7 patients were operated on. The method of treatment was based on the degree of fragment displacement, the patient´s general condition and local condition of soft tissues. Two patients were primarily indicated for non-operative treatment due to only a minimal displacement of articular surfaces (Pts 7, 10). Indication for operative treatment was displacement of articular fragments (gap or step-off) of more than 3mm. This criterion was met by 10 patients (11 fractures). Owing to the general or local condition, operation was contraindicated in 2 patients (Pts 11, 12) with 3 fractures; one older female patient (Pt 1) refused the proposed operation. The first author performed 6 operations and the second author one operation, at an interval of 7−18 days after the injury (mean, 10 days).
Non-operative treatment followed the protocol described below, which if necessary was modified on a case-by-case basis. Immediately after the injury, treatment consisted of pain relief and three to four weeks of sling immobilization. Subsequently, passive ROM exercises by CPM machine were started, followed by active ROM exercises beginning from the 2nd month after injury and strengthening of the rotator cuff muscles and parascapular muscles beginning from the 3rd month. During the 4th month all restrictions were lifted.
The aim of operative treatment was to restore the continuity of the glenoid fossa and re-attach the reconstructed articular surface to the scapular neck or body, and to restore stability and pain-free motion of the shoulder. In all patients, the modified Judet posterior approach was used to expose the surgical site, including mobilizing the infraspinatus [13]. Where the posterior joint capsule was not ruptured, incision of the capsule ran parallel to the rim of the articular surface, in order to allow a visual check and palpation of the glenoid fossa and humeral head. During reconstruction of the glenoid fossa, the main emphasis was put on the two inferior thirds of the articular surface. Following anatomical reduction of the glenoid fossa and temporary fixation by K-wires, final fixation was performed with lag screws and 2.7 or 3.5mm standard (non LCP) plates. In most cases, these plates also helped reconstruct the lateral border (pillar) of the scapular body [14]. In 1 case, anatomical reduction and fixation of acromion fracture was performed in the next step (Pt 6). In 1 case acromioclavicular (AC) dislocation was treated from the extended Judet approach [15] by wire cerclage (Pt 9). All operated cases were documented by intraoperative photos.
Passive ROM exercises by CPM machine were started on the 1st postoperative day, followed by active ROM exercises as a rule 2-3 weeks postoperatively.
Patients were regularly followed up, including radiographic examination, at 6 weeks, 3, 6 and 12 months after the injury (operation). In 1 non-operatively treated female patient (Pt 1) and in 4 operated patients (Pts 3, 4, 6, 9), follow-up CT examination, including 3D CT reconstruction with subtraction of the humeral head was performed after bone union, i.e. in the interval between 6 and 50 months after injury.
Evaluation: All patients except for one (Pt 12 with a bilateral fracture) were followed up 12 to 55 months after injury (mean, 24 months).
In the basic group, i.e. in 12 patients (13 fractures), we evaluated the scapular fracture anatomy, including the associated injuries to the ipsilateral shoulder girdle. In the first round of assessment, all four authors reviewed all radiographs and CT scans independently. In the second round, in cases of differing classification, consensus was reached by reviewing the respective radiographs and scans jointly. In 11 patients (11 fractures), during the last follow-up we assessed radiological and functional results of the treatment, including complications. Functional assessment was based on the Constant score [16] and was always performed at the last follow-up.
Results
In assessing the findings, we focused on the fracture anatomy and on radiological and functional evaluation of the results of treatment.
Fracture anatomy: Despite a certain variability of findings we found a certain correlation between the site of separation of the glenoid fossa fragments, the number of fragments and their size and the patients´ age.
The site of separation of articular fragments: From this viewpoint we divided the fractures into three groups. In the first group, comprised of 5 fractures (Pts 1−5), the separation line passed through the anatomical neck. Fragments were small and formed only by parts of the glenoid fossa and anatomical neck of the scapula, with one exception of a fragment carrying the lower part of the glenoid fossa, which extended at variable distance into the lateral border of the scapular body (Fig. 1). In 4 of 5 cases, the glenoid fossa was fragmented into three to four parts, in 1 case into only two parts (Pt−5). In 3 cases, the glenoid fracture was associated with a transverse infraspinous fracture of the scapular body. The mean age of the patients was 55.6 years.
1. Glenoid fossa fractures (four fragments) with separation in the anatomical neck − CT 3D reconstructions (Pt − 1) 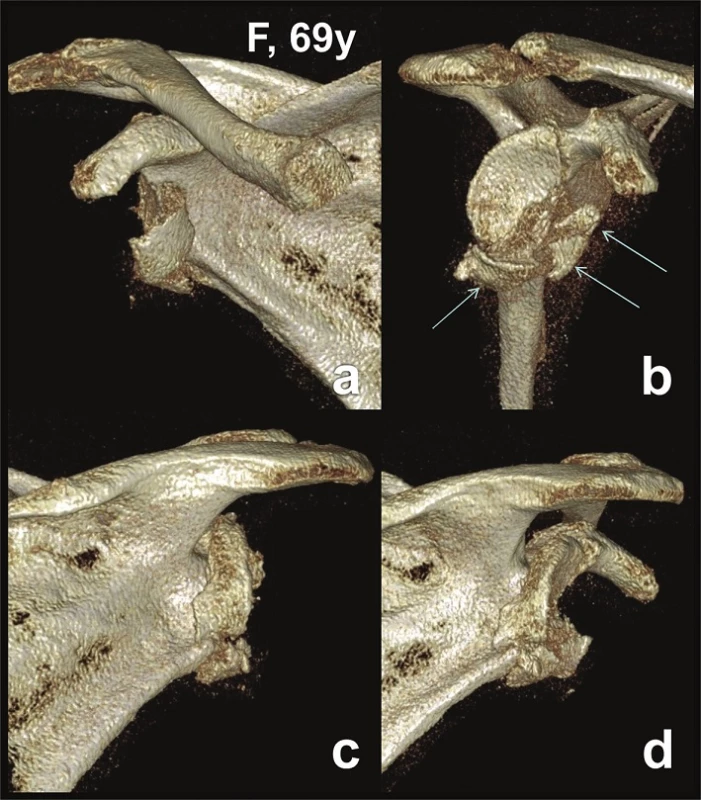
a – anterior view; b – lateral view; c – posterior view; d – posterolateral view. In the second group, comprised of 4 fractures (Pts 6−9), the separation line of the fragments of the glenoid fossa ran through the coracoid process or surgical neck of the scapula (Fig. 2−4). The superior fragment of the glenoid fossa carried the whole coracoid process or its part. In 1 case (Pt 8), the glenoid fossa fracture was associated with a fracture of the lateral border (pillar) of the scapular body and a transverse acromion fracture, in 1 case with a transverse infraspinous fracture of the scapular body (Pt 9) and in 1 case with a transverse acromion fracture (Pt 6). The mean age of the patients was 29 years.
2. Glenoid fossa fractures (two fragments) with separation through the coracoid process − CT 3D reconstructions (Pt − 7) 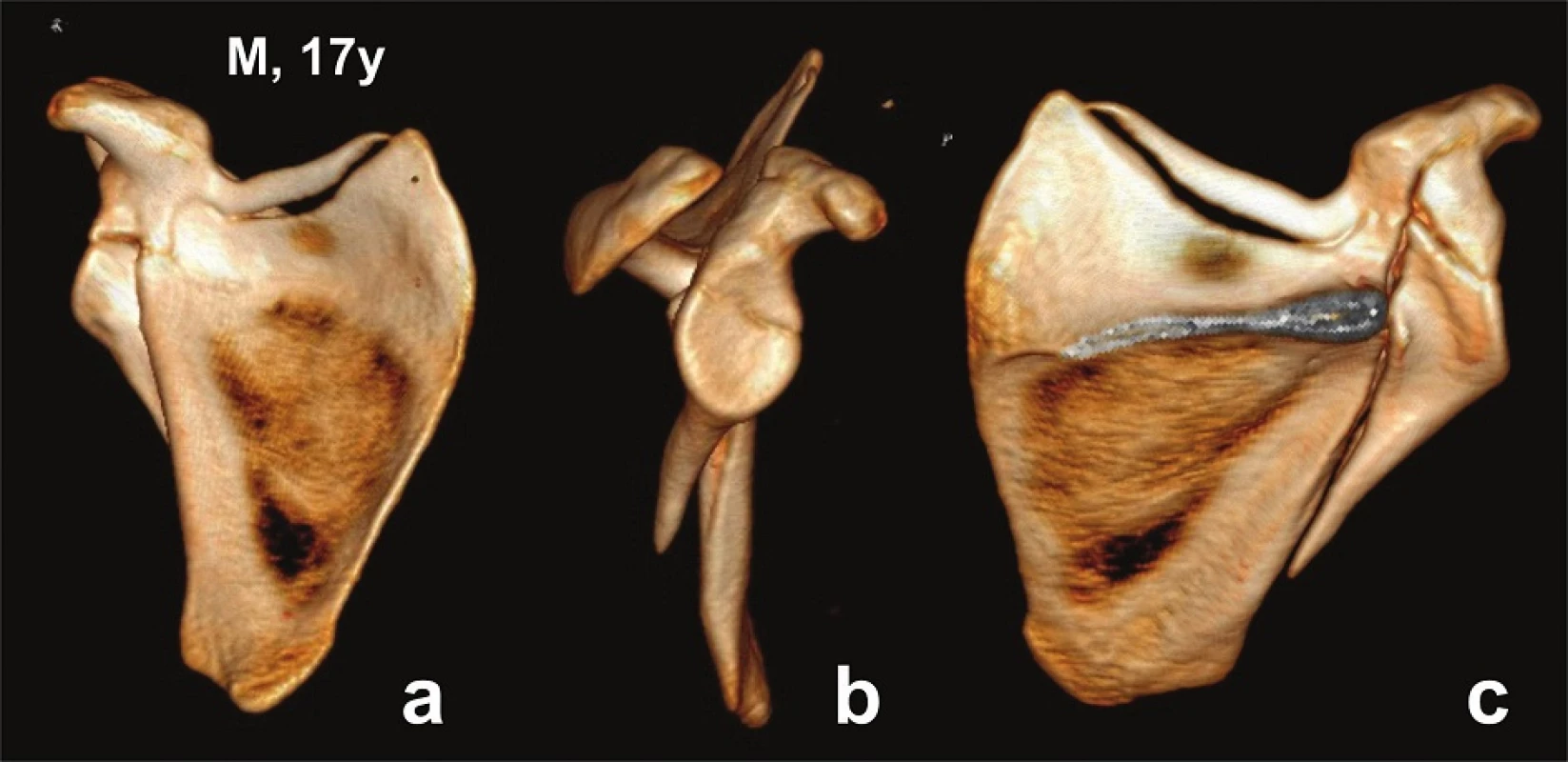
a – anterior view; b – lateral view; c – posterior view. 3. Glenoid fossa fractures (two fragments) with separation through the coracoid process and acromion fracture − CT 3D reconstructions (Pt − 6) 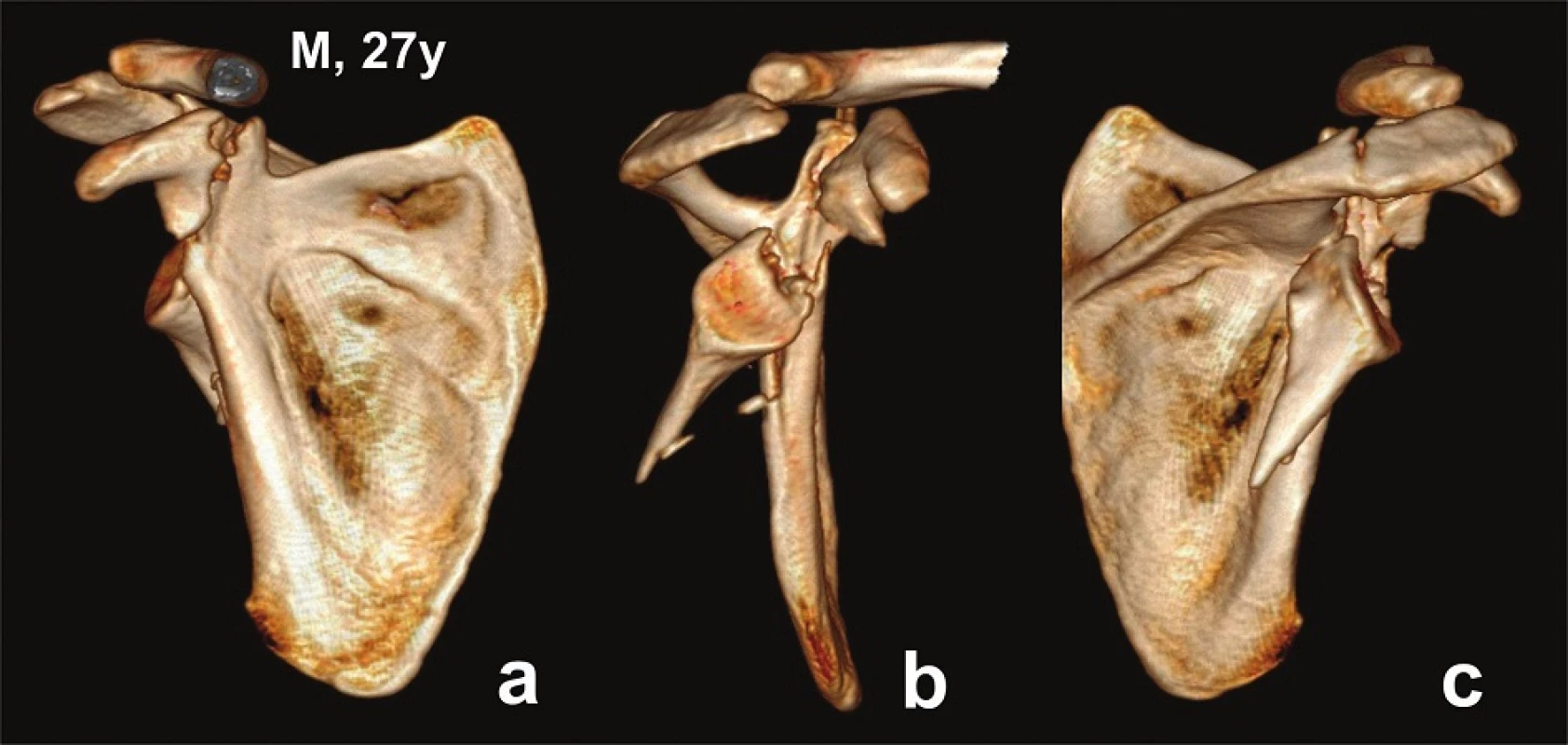
a – anterior view; b – lateral view; c – posterior view. 4. Glenoid fossa fractures (four fragments) with separation in the surgical neck − CT 3D reconstructions (Pt − 9) 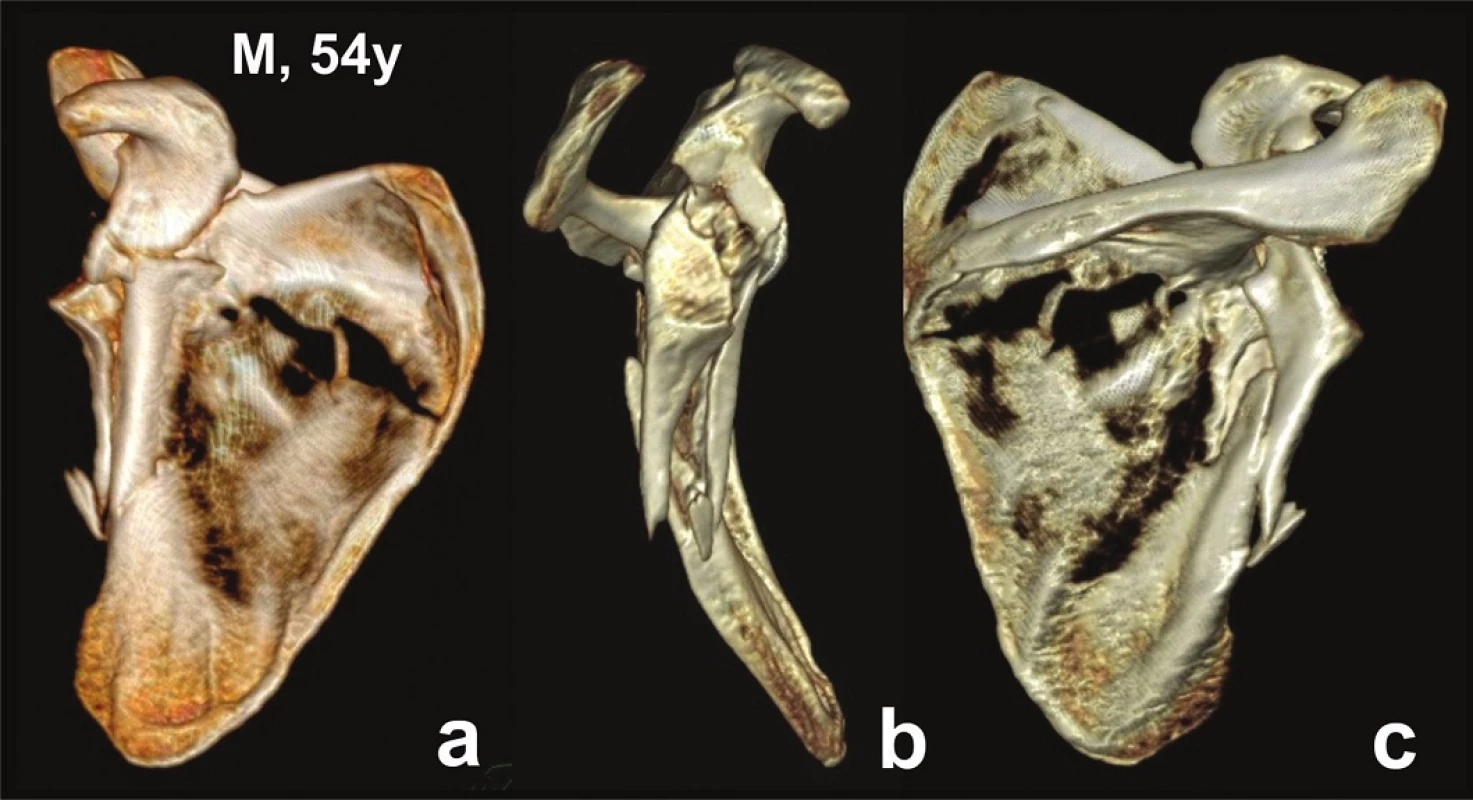
a – anterior view; b – lateral view; c – posterior view. The third group included 3 patients (Pts 10−12) with 4 fractures, always caused by high-energy trauma. The entire scapular body, i.e., both its supra - and infraspinous parts, was fractured (Fig. 5). The glenoid fossa was always split into two parts. The superior fragment was formed by a bone block carrying in 3 cases the coracoid process and the fracture line ran through the scapular notch (Pts 10, 11, 12 – left scapula). In 1 case, the fracture line passed through the spine of the scapula and the superior fragment carried in addition to the coracoid process also the lateral part of the spine of the scapula (Pt 12 − right scapula). In all 4 cases, the inferior part of the glenoid fossa was part of a large fragment formed by the entire lateral border of the scapular body. The mean age of these polytraumatized patients was 27 years.
5. Glenoid fossa fractures (two fragments) with separation in the scapular body − CT 3D reconstructions (Pt − 10) 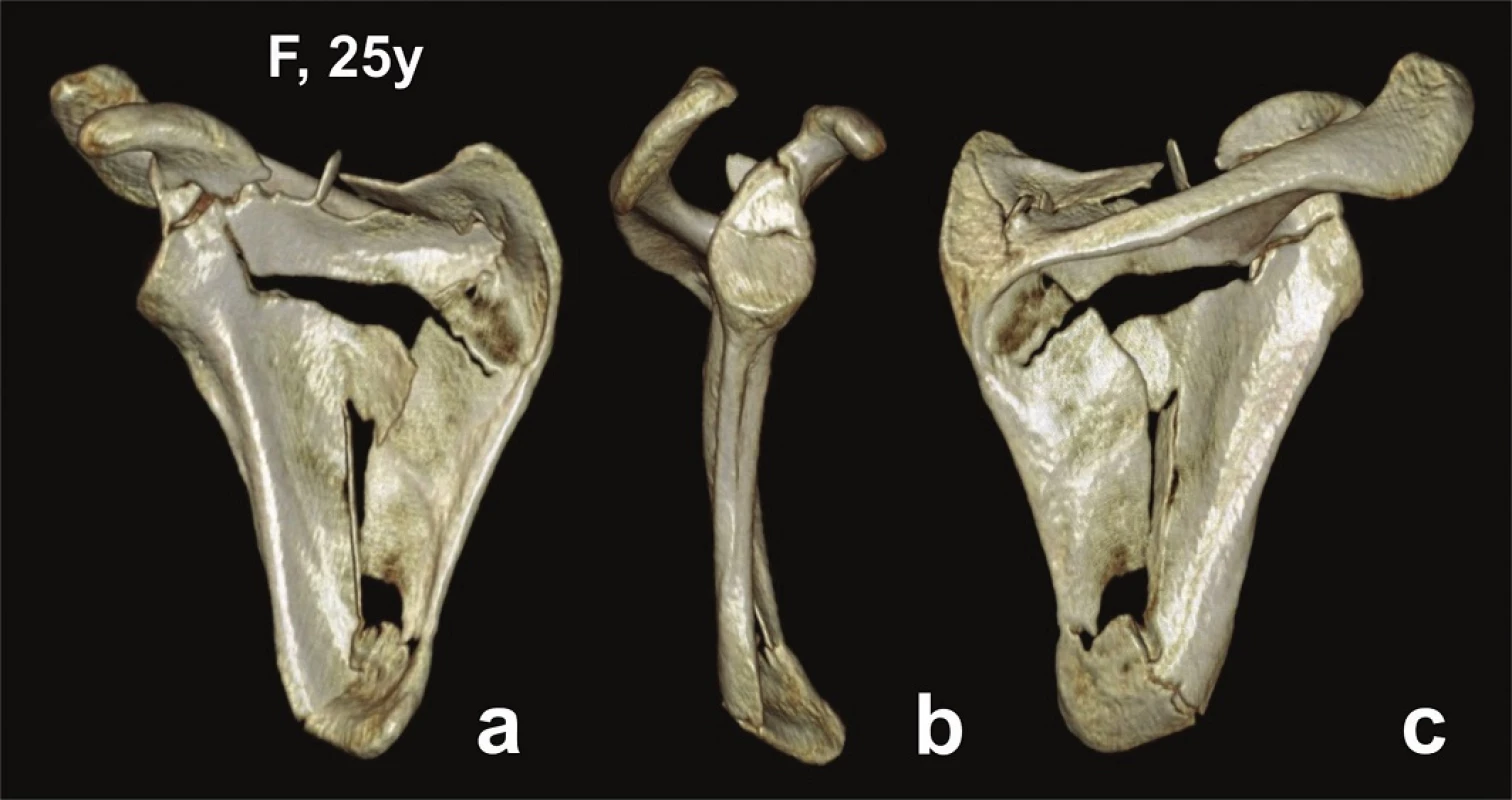
a – anterior view; b – lateral view; c – posterior view. Number of fragments of the glenoid fossa: In 7 fractures, i.e., 6 patients, the glenoid fossa was split into two parts. In 5 of these 7 cases the fracture line ran horizontally, dividing in 3 cases the superior and middle thirds, and in 2 cases the middle and inferior thirds of the glenoid fossa. In 2 cases, the fracture line passed obliquely, splitting the glenoid fossa in 1 case into two equal and in 1 case two unequal parts. The mean age of these 5 patients was 28.8 years (17−44).
In another 5 cases, the glenoid fossa was fractured into three to four fragments, the size of which varied. The mean age of the patients was 57.6 years (range, 38−71).
In 1 case of a 17-year old female patient hit in her shoulder by railway carriage step (Pt 8), one fragment carried the upper half of the glenoid fossa. The inferior half of the articular surface was smashed into small pieces.
Associated injuries of the shoulder girdle and humerus: These injuries were seen in 3 patients, including one case of a humeral shaft fracture and brachial plexus injury (Pt 8), one case (Pt 7) of a humeral shaft fracture and sternoclavicular (SC) dislocation and one case (Pt 9) of AC dislocation. Humeral shaft fractures were treated with intramedullary fixation (ESIN). AC dislocation was managed after internal fixation of the scapula with wire cerclage from the extended Judet approach. SC dislocation was treated non-operatively.
Radiological and functional evaluation: All 11 fractures radiologically healed within 3 months, without secondary displacement of fragments.
Non-operatively treated patients: Non-operative treatment was used in 5 patients with 6 fractures, but patient N 12 with a bilateral fracture was lost to follow-up.
In 2 patients (Pts 7, 10), indicated primarily for non-operative treatment due to minimal dislocation of glenoid fossa fragments, the fractures healed almost in an anatomical position, except for a minor angulation of the inferior angle of the scapula in the female patient N 10. Both patients had almost a full range of motion (ROM) in the shoulder.
Both glenoid fracture-dislocations (Pts 1, 11) healed in a non-anatomical position resulting in glenoid fossa incongruence. In the patient with an open fracture of the scapula (Pt 11), the fracture of the scapular body healed in severe displacement, fortunately without infectious complications, but with extensive heterotopic ossifications. ROM in the shoulder was painful and considerably limited in both patients.
Operatively treated patients: In 6 patients, the surgical wound healed uneventfully, 1 patient (Pt 3) developed postoperative early deep infection, requiring repeated revisions.
In 6 patients, glenoid fractures healed in anatomical position, confirmed in 4 cases by postoperative CT examination (Pts 3, 4, 6, 9). All patients but one were subjectively satisfied with the function of the joint. In 2 patients (Pts 4, 6), the ROM was fully restored (Fig. 6, 7), in 3 patients the ROM was slightly limited (Pts 2, 5, 9), (Fig. 4,8). The patient (Pt 3) with infectious complications had a limited ROM in the joint by one third (Fig. 9, 10). In a female patient (Pt 8), with comminution of the inferior part of the glenoid fossa and brachial plexus injury, the operation was performed prior to a planned neurosurgical procedure, as the neurosurgeon required a stable glenohumeral joint. Radiograph showed remodelling of bone fragments and restoration of the joint line. Unfortunately, the neurosurgeon changed his mind and the originally planned neurosurgical operation was not performed in the end. The limb, however, remained plegic.
6. Reconstruction of glenoid fossa (Pt – 4) 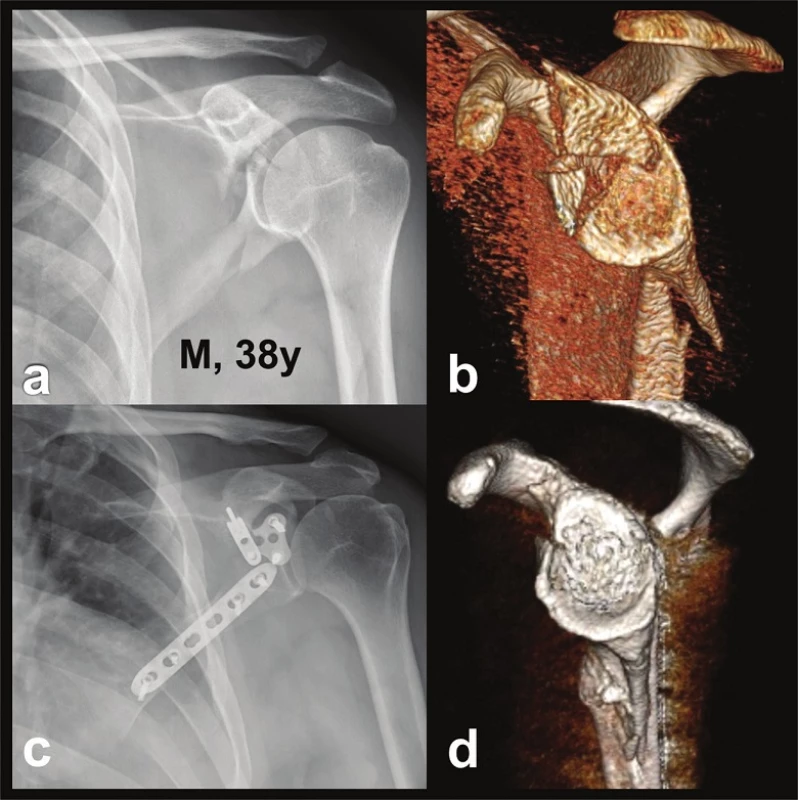
a – post-injury radiograph; b – CT 3D reconstruction in lateral view demonstrating separation in the anatomical neck; c – postoperative radiograph; d – postoperative CT 3D reconstruction in lateral view demonstrating an anatomical reconstruction of the glenoid fossa. 7. Functional result (Pt 4) in three-part glenoid fossa fracture with separation in the anatomical neck 
8. Functional and radiological result (Pt – 9) in fourpart glenoid fossa fracture with separation in the surgical neck, fracture of scapular body and AC dislocation 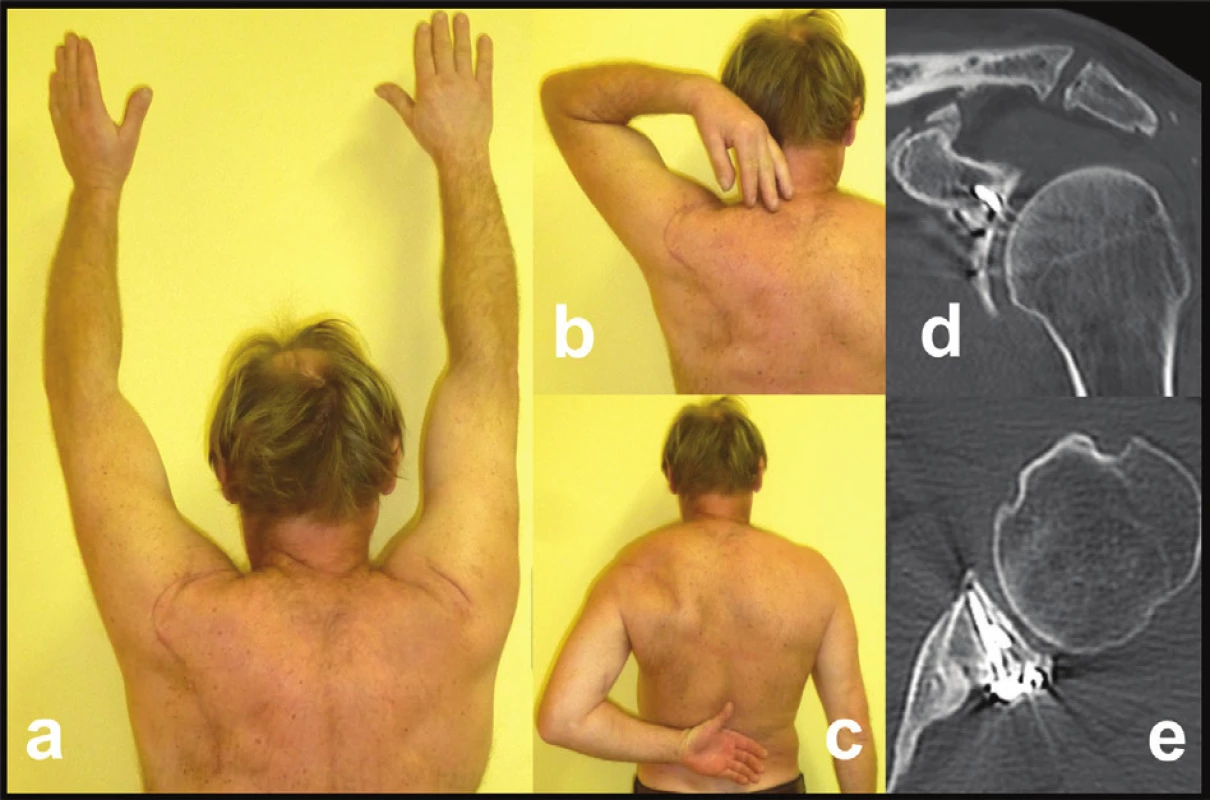
a, b, c – functional result (note a scar after extended Judet approach); d+e – postoperative CT scans demonstrating anatomic reduction of glenoid fossa and AC joint; post-injury CT see figure 4. 9. Glenoid fossa fractures (four fragments) with separation in the anatomical neck and fracture of infraspinous part of the scapular body (Pt − 3) 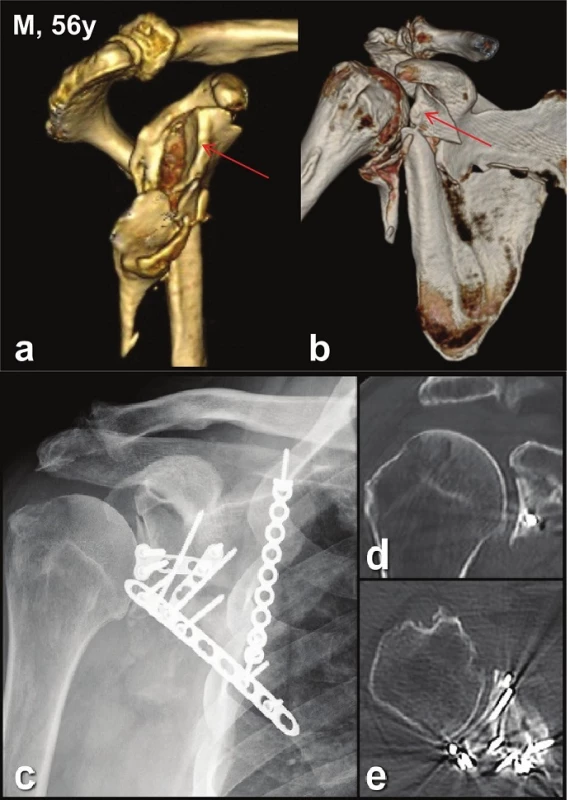
a – CT 3D reconstructions - lateral view; b – CT 3D reconstructions - anterior view; c – postoperative radiograph, d – postoperative frontal CT scan; e – postoperative transversal CT scan. 10. Functional result (Pt 3) in four-part glenoid fossa fracture with separation in the anatomical neck and fracture of the scapular body 
Complications in operated patients: No intraoperative complications were recorded. One patient (Pt 3) developed the above mentioned postoperative infection, requiring removal of the infraspinatus muscle. This complication was caused by the patient´s general condition (smoking and alcoholic hepatopathy). The function of the joint, however, was surprisingly very good. In 4 patients, we recorded a mild atrophy of the infraspinatus, but without any impact on the functional outcome. The female patient with brachial plexus injury (Pt 8) was already mentioned before. One patient (Pt 9) developed asymptomatic heterotopic ossification along the lateral border of the scapular body, most probably due to traumatic muscle damage.
Discussion
Total articular fractures of the glenoid, when all fragments of the articular surface lose contact with the scapular neck or body, accounted for 11% of all intraarticular injuries to the scapula in our statistics [11]. In the literature, fractures of the entire glenoid fossa are most often described as comminuted, multifragmentary or total articular glenoid fractures [7−10]. Schematic drawings in individual classifications show the fragments of comminuted glenoid fossa separated from the scapula in the line of the anatomical neck [7]. Goss classification [3,4] specifies them as type VI, Euler-Rüedi classification [5]as type D2b and OTA [7] classification as types 14C2 and 14C3 (in combination with transverse infraspinous fracture of the scapular body). These types correlate with our first group of glenoid fractures. This group included patients with a higher mean age (55 years) and, as a result, with worse bone quality. In 4 of 5 cases, low - or medium-energy violence caused breaking of the glenoid fossa into three to four fragments in the anatomical neck line. Splitting of the articular surface and separation of both fragments from the surgical neck of the body of the scapula is specified in the Goss classification as type Va or type Vc [3,4]. In these cases, the superior fragment is formed by a block carrying also the coracoid process and the inferior fragment carries the proximal part of the lateral borer of the scapular body. These types of injuries are similar to certain fractures from our second and third groups. Goss classification, however, does not take into account variability of the shape of the inferior articular fragment or involvement of the scapular body.
Our third group of patients represents an opposite pole to the first group. The fractures were caused by high-energy mechanism, which resulted in injury to the entire scapular body, including the glenoid fossa, which was, however, fractured only into two large fragments. Unlike Goss types Va and Vc, the inferior articular fragment included the entire border of the scapular body and the body itself was broken into several fragments. None of our 3 patients (4 fractures) was older than 30 years. This documents a different bone quality as compared to the first group of patients.
Our second group of patients, where the trauma occurred in the region of the coracoid process or surgical neck, represents a transition between the two extreme types, partially similar to types Va and Vc of Goss classification.
Our analysis shows that the anatomy of total glenoid fractures varies in view of the injury mechanism and bone quality. Certain types identified by us have not yet been described in the currently used classifications.
Opinions on treatment of comminuted glenoid fractures differ. According to Christensen et al. [17], these fractures should be treated non-operatively due to poor results of their operative treatment. On the other hand, some authors report good results of arthroscopic reconstruction of “comminuted” glenoid fossa fracture in 1 [18], and 11 patients [19]. Unfortunately, these two studies do not provide a clear picture of the anatomy of the reported glenoid fossa fractures.
In any case, the comminuted type with separation of fragments in the anatomical neck represents the most severe fractures of the glenoid fossa. Their operative treatment is highly demanding as the fragments are small and the bone quality corresponds to the patients´ age (mean, 56 years). In spite of this, in our 4 operated patients, 3 times we achieved a very good and once a good result (Tab. 1). In contrast, the result of non-operative treatment of a female patient was poor.
In the second group with separation of fragments through the coracoid process or surgical neck, a very good result was achieved in two of three operated patients. One poor result was caused by brachial plexus injury.
All three displaced fractures in the third group were treated non-operatively due to the patient´s general or local condition. But for these complications, these fractures were, in view of their size and number of articular fragments and bone quality, an ideal indication for operative treatment. Even despite the involvement of the articular surface, a good result may be expected in these fractures, similar to that which we have achieved in case of scapular body fractures combined with partial intraarticular fracture of the glenoid fossa [14].
Our experience in operative treatment of total glenoid fractures is generally positive. In 6 of 7 patients, we achieved a very good or excellent result, including the patient with an infectious complication. The only negative exception in our group of patients treated operatively was the female patient with brachial plexus injury. To achieve a good result, restoration of the shape and congruence of the inferior two thirds of the glenoid fossa, the so called circular area was of decisive importance. Another important factor was early postoperative intensive rehabilitation and motivation, particularly in elderly patients.
The weakness of our study is a small and rather heterogeneous group of patients. The problem of heterogeneity, however, exists in a number of significant studies dealing with operative treatment of displaced glenoid fractures of type II to VI of the Goss classification [18−32]. These studies report good results, but none of them includes their analysis in view of the fracture pattern. As a result, this issue remains open and requires additional research.
Conclusion
Fractures of the entire glenoid fossa are the most severe injuries to scapula. Their diagnosis requires CT examination, including 3D CT reconstruction with subtraction of the humeral head, ribs, and sometimes also subtraction of the acromion. Displaced fractures are indicated for operative treatment from the Judet approach. The aim is to primarily reconstruct the inferior two thirds of the articular surface, the so called circular area, and to firmly fix the reconstructed glenoid fossa to the scapular neck or body. An early and intensive postoperative rehabilitation is of no less importance.
The authors wish to thank Ludmila Bébarová, PhD for her assistance in the preparation of the manuscript.
Conflict of Interests
The authors declare that they have not conflict of interest in connection with the emergence of and that the article was not published in any other journal.
Prof. MUDr. Jan Bartoníček, DrSc.
Department of Orthopaedics, 1st Faculty of Medicine
of Charles University and Central Military Hospital, Prague,
U Vojenské nemocnice 1200,
169 02 Prague 6
e-mail: bartonicek.jan@seznam.cz
Sources
1. Ideberg R. Fractures of the scapula involving glenoid fossa. In: Bateeman JE, Welsh RP (eds). Surgery of the shoulder. Philadelphia, Decker 1984 : 63.
2. Ideberg R, Grevsten S, Larsson S. Epidemiology of scapula fractures. Acta Orthop Scand 1995;66 : 395−7.
3. Goss TP. Fractures of the glenoid cavity. J Bone Joint Surg Am 1992;74-A:299−305.
4. Goss TP. Fractures of the scapula. In: Rockwood CA, Matsen FA, Wirth MA, Lippitt SB (eds). The Shoulder. 3rd edition. Philadelphia; Saunders 2004 : 413−54.
5. Euler E, Rüedi T. Scapulafraktur In: Habermeyer P, Schweiber L (Hrsg.) Schulterchirurgie. München, Urban und Schwarzenberg 1996 : 261−71.
6. Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa. Clin Orthop Rel Res 1998;346 : 122−30.
7. Orthopaedic Trauma Association Fracture and dislocation compendium. Scapula fractures. J Orthop Trauma (Suppl 1) 2007;21:S68−71.
8. Jaeger M, Lambert S, Südkamp NP, et al. The AO Foundation and Orthopaedic Trauma Association (AO/OTA) scapular fracture classification system: focus on glenoid fossa involvement. J Shoulder Elbow Surg 2013;22 : 512−520.
9. Christensen TJ, Kubiak EN. Epidemiology, clinical evaluation, imaging and classification of scapular fractures. In: Iannotti JP, Miniaci A, Williams GR, Zuckerman JD (eds) Disorders of the shoulder, Diagnosis and management: shoulder trauma. Third edition. Philadelphia, Wolter Kluwer 2014 : 153−66.
10. ter Meulen DP, Janssen SJ, Hageman MGJS, Ring DC. Quantitative three-dimensional computed tomography analysis of glenoid fracture patterns according to the AO/OTA classification. J Shoulder Elbow Surg 2016;25 : 269−75.
11. Bartoníček J, Tuček M, Klika D, et al. Pathoanatomy and CT classification of glenoid fossa fractures based on 90 patients. Int Orthop DOI 10.1007/s00264-016-3169-4. On line.
12. Chochola A, Tuček M, Bartoníček J, et al. [CT-diagnosis of scapular fractures] Czech, Rozhl Chir 2013;92 : 385−8.
13. Bartoníček J Scapular fractures. In: Court-Brown CH, Heckman AD, MqQueen M, Ricci WM, Torneta P (eds) Rockwood and Green´s fractures in adults. 8th edition. Philadelphia, Wolters Kluwer 2015 : 1475−1501.
14. Bartoníček J, Frič V. Scapular body fractures: Results of the operative treatment. Inter Orthop (SICOT) 2011;35 : 747−53.
15. Bartoníček J, Tuček M, Luňáček L [Judet posterior approach to the scapula] Czech, Acta Chir Orthop Traumatol Čechoslov 2008;75 : 429−35.
16. Constant CR, Murley AH Clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;214 : 160−64.
17. Christensen TJ, Kubiak EN. Non operative management of scapular fractures: Indications, techniques, and outcomes. In Iannotti JP, Miniaci A, Williams GR, Zuckerman JD (eds) Disorders of the shoulder, diagnosis and management: Shoulder trauma. Third edition. Philadelphia, Wolter Kluwer 2014 : 167−75.
18. Gigante A, Marinelli M, Verdeneli A, et al. Arthroscopy-assisted reduction and percutaneous fixation of a multiple glenoid fracture. Kne Surg Sports Traumatol Arthrosc 2003;11 : 112−5.
19. Qu F, Yuan B, Li Ch, et al. Arthroscopic fixation of comminuted glenoid fractures using cannulated screw and suture anchors. Medicine 2015;94/49 : 1−4.
20. Hardegger F, Simpson LA, Weber BG. The operative treatment of scapula fractures. J Bone Joint Surg Br 1984;66-B:725−31.
21. Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intra-articular fractures of the glenoid fossa. J Bone Joint Surg Am 1993;75-A:479−84.
22. Leung KS, Lam TP, Poon KM. Operative treatment of displaced intra-articular glenoid fractures. Injury 1993;24 : 324−28.
23. Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa. Clin Orthop Rel Res 1998;346 : 122−30.
24. Schandelmaier P, Blauth M, Schneider, et al. Fractures of the glenoid treated by operation. J Bone Joint Surg Br 2002;84-B:173−7.
25. Hersovici D, Roberts CS. Scapula fractures: to fix or not to fix? J Orthop Trauma 2006;20 : 227−9.
26. Zlowodski M, Bhandari M, Zelle BA, et al. Treatment of scapula fractures: systematic review of 520 fractures in 22 case series. J Orthop Trauma 2006;20 : 230−3.
27. Nork SE, Barei DP, Gardner MJ, et al. Surgical exposure and fixation of displaced type IV, V, and VI glenoid fractures. J Orthop Trauma 2008;22 : 487−93.
28. Lantry JM, Roberts CS, Giannoudis PV. Operative treatment of scapular fractures: A systematic review. Injury 2008;39 : 271−83.
29. Anavian J, Gauger EM, Schroder LK, et al. Surgical and functional outcomes after operative management of complex and displaced intra-articular glenoid fractures. J Bone Joint Surg Am 2012;94 : 645−53.
30. Lewis S, Argintar E, Jahn R, et al. Intra-articular scapular fractures: Outcomes after internal fixation. J Orthop 2013;10 : 188−92.
31. Sen KR, Sud S, Rangal S, et al. Glenoid fossa fractures: Outcome of operative and nonoperative treatment. Ind J Orthop 2014;48 : 14−9.
32. Mulder FJ, van Suchtelen M, Menedez ME, et al. A comparison of actual and theoretical treatments of glenoid fractures. Injury 2015;46 : 699−702.
Labels
Surgery Orthopaedics Trauma surgery
Article was published inPerspectives in Surgery

2016 Issue 11-
All articles in this issue
- The possibility of eliminating axillary dissection in breast cancer patients using neoadjuvant treatment
- Thyroid carcinoma, ten-years file
- Transplantation of allogeneic bone graft in the therapy of massive post-sternotomy defects – 6 years of experience with the method
- An uncommon case of purulent mesenteric lymphadenitis
- Rare malignant tumors of the appendix: surgical treatment of liver metastases − case reports
- Mechanical ileus as a result of scar tissue stenosis of the small intestine
- Total glenoid fractures
- Perspectives in Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- An uncommon case of purulent mesenteric lymphadenitis
- Rare malignant tumors of the appendix: surgical treatment of liver metastases − case reports
- Total glenoid fractures
- Transplantation of allogeneic bone graft in the therapy of massive post-sternotomy defects – 6 years of experience with the method
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

