-
Medical journals
- Career
Primárny B-bunkový non-Hodgkinov lymfóm Burkittovského typu: popis prípadu s typickými klinickými prejavy
: Kozáková D.macháleková K.brtko P. 1 *,2 *,1; P. Szépe 2; P. Vaňuga 1; M. Pura 1
: Department of Endocrinology, the National Institute of Endocrinology and Diabetology, Ľubochňa, Slovakia 1; Institute of Pathology, Jessenius Faculty of Medicine, Comenius University, Martin, Slovakia 2
: Čas. Lék. čes. 2008; 147: 569-573
: Case Report
Primárne lymfómy CNS (PCNSL) tvoria 3 % všetkých intrakraniálnych nádorov. Z týchto predstavujú mimoriadne vzácnu a významnú klinickú jednotku primárne lymfómy hypofýzy (PPL). Prakticky všetky PCNSL sú non-Hodgkinove difúzne veľkobunkové B-bunkové lymfómy. Prezentujeme prípad 60‑ročnej pacientky s pravostrannou obrnou tretieho hlavového nervu, bitemporálnou poruchou perimetra mierneho stupňa, silnou cefaleou a polyúriou-polydipsiou. Vyšetrenia potvrdili hypopituitarizmus s hyperprolaktinémiou, pri morfologickom vyšetrení mozgu sa zobrazila expanzia hypofýzy s priemerom 16 mm a suprasellárnou propagáciou. Predbežne stanovenou diagnózou bol adenóm hypofýzy. Pacientka podstúpila neurochirurgický výkon. Histopatologické vyšetrenie a imunofenotypizácia (cytokeratín–, CD45⁺, CD79⁺, bcl-2⁻) ozrejmili vysoko malígny B-bunkový non-Hodgkinov lymfóm Burkittovho typu. Komplexnými vyšetreniami sa nepreukázali žiadne ďalšie ložiská lymfómu, HIV status pacientky bol negatívny, status infekcie vírusom Epstein-Barrovej sa nevyšetroval. Aj keď PPL môžu byť pri zobrazovacom vyšetrení neodlíšiteľné od adenómov hypofýzy, o lymfóme treba uvažovať v prípade nálezu invazívnej sellárnej expanzie, ktorá je pri vyšetrení magnetickou rezonanciou izo - až hypointenzná v T2-váženom obraze, najmä pokiaľ ide o imunokompromitovaného pacienta alebo pacienta vysokého veku, a pokiaľ sú popri očakávanom hypopituitarizme prítomné aj diabetes insipidus, obrna hlavového nervu a horúčka nejasného pôvodu.
Kľúčové slová:
primárny lymfóm hypofýzy, B-bunkový lymfóm s vysokým stupňom malignity, Burkittov lymfóm, hypopituitarizmus, diabetes insipidus, obrna hlavového nervu, horúčka nejasného pôvodu, magnetická rezonancia. Ko.Tumors of the central nervous system (CNS) with their prevalence 3.8–5.1 per 100,000 constitute the fourth cause of death in males aged 35–54 yr. In Europe, those tumors account for only 2% of all deaths due to cancer (1). Pituitary adenomas, having an annual incidence in the general population of about 25 per million (2), are the most common cause of a mass in the sella, accounting for up to 10–15% of CNS tumors (3). Primary CNS lymphomas (PCNSLs), defined as lymphomas limited to the cranial-spinal axis without systemic disease, are now thought to constitute 3% of all intracranial neoplasms (4, 5). From these, primary pituitary lymphomas (PPLs) represent an emerging clinical entity with an increasing numbers in a large series of pituitary masses (6) as well as in number of isolated reports in the last decade. These have been excellently reviewed by Giustina et al. (7).
Burkitt lymphoma is a childhood tumor that commonly affects abdominal organs. Involvement of the CNS is usually secondary and a manifestation of advanced systemic disease. Few cases of immunocompetent patients with the Burkitt type of PCNSL are reported in the literature (8–11), to the best of our knowledge, there is no report on Burkitt type of PCNSL presented as pituitary tumor. Here we report on the adult patient with PLL of the Burkitt type presenting with typical endocrinological and neurological symptomatology.
Case report
A 60-year-old woman had a history of arterial hypertension, bilateral coxarthrosis, recurrent deep vein thrombosis, functional gastric dyspepsia and non-alcoholic liver steatosis; presented with brainstem ischemic stroke, right-sided third cranial nerve palsy, mild bitemporal visual field deficit, hemiparesis of the left upper extremity, weakness, severe cephalea, nausea, vomiting, right-sided purulent otitis media with fever up to 40.0 °C and polyuria-polydipsia (up to 4.5 litres per day). The patient was admitted for presumed hypopituitarism, which was confirmed with the following abnormally low laboratory findings: plasma morning cortisol level (62 nmol/L; normal, > 300 nmol/L), follicle stimulating hormone level (1.62 U/L; normal in postmenopausal women, 20-138 U/L), luteinizing hormone level (0.07 U/L; normal in postmenopausal women, 15–62 U/L), thyroid stimulating hormone level (0.288 mIU/L; normal, 0.35–4.94 mIU/L), free thyroxine (7.4 pmol/L; normal, 9.0–19.0 pmol/L). Prolactin level was increased (1219 mU/L; normal in postmenopausal women, < 470 mU/L).
Brain computer tomography imaging revealed a 16 mm-diameter sellar mass with suprasellar extension, without significant perifocal edema, centro-medial structures without deviation from the middle line, obstruction of the circulation of the liquor or skull bone destruction. A presumptive diagnosis of pituitary adenoma was made. The patient underwent a neurosurgical intervention, intraoperatively also the sphenoidal extension of the tumor was recorded. Histology revealed a mitotically high active tumor with blastic-like neoplastic lymphoid cells with clumped chromatin and small nucleoli and large pale macrophages forming the “stars” in the “starry sky”. Immunophenotyping (cytokeratin–, CD45+, CD79+, bcl-2–) verified high-grade B cell non-Hodgkin lymphoma of the Burkitt type (Fig. 1). HIV status of the patient was negative, Epstein-Barr virus (EBV) status was not disclosed, systemic work-up including bone marrow aspiration were obtained and excluded systemic lymphoma (Fig. 2).
1. Photomicrographs of a histological section showing a population of B-cell lymphoma of the Burkitt type arising in the pituitary gland – neoplastic lymphoid cells with pale macrophages forming the typical “starry sky” pattern (immunohistochemical stains not shown) A) H & E stain, original magnification x 20, B) H & E stain, original magnification x 40, C) Giemsa stain, original magnification x 20, D) Giemsa stain, original magnification x 40 
2. Photomicrographs of a histological section from bone marrow core biopsy showing normocellular marrow without intrasinusoidal infiltration of lymphoma A) H & E stain, original magnification x 4, B) H & E stain, original magnification x 10 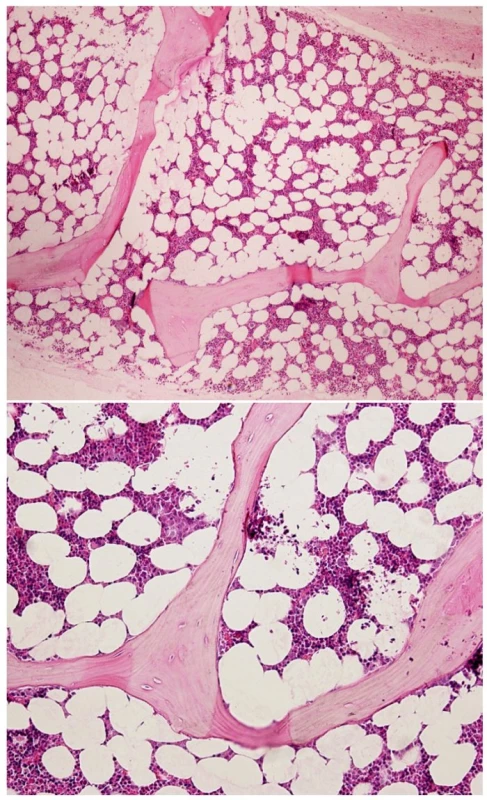
Discussion
Non-Hodgkin lymphomas may involve the CNS either as a primary tumor or after spreading from an established systemic lymphoma. This occurs in 5–29% of patients with systemic lymphoma (12). This frequency has largely increased because of the increasing number of patients with congenital and iatrogenic immunosuppression and acquired immunodeficiency syndrome (AIDS) (13). Although recent data show an increase in the incidence of PCNSLs in immunocompetent individuals (4), thus representing approximately 3% of intracranial neoplasms (4, 5), reports of primary pituitary lymphoma have been exceedingly rare. In 2001 Giustina et al. summarized the cases of PPLs reported in some detail in the literature, specifically 14 cases of apparently PPLs and 10 cases of secondary localization or infiltration of the sella turcica (7). After this review few new cases of PPLs have been published (14–18).
Besides the established common risk factors for PCNSLs – AIDS, organ transplantation, autoimmune or inflammatory disease requiring continual pharmacological immune suppression, and hereditary immunodeficiency syndromes (19), pituitary adenomas and lymphocytic hypophysitis have been implicated as hypothetical specific risk factors for PPLs (7, 19). A case of mucosa-associated lymphoid tissue lymphoma of the pituitary gland presenting as a homogeneously enhancing solid mass in the sellar region and in both parasellar regions was also reported (20). In immunocompetent patients, the median age at diagnosis of PCNSLs is 60 years, with a male/female ratio of 1.2. The highest risk group appears to be those of 60 years of age or older, as in present case. Among patients with AIDS, the typical age at presentation is younger; the mean age is 31 to 36 years. Consistent with the population at highest risk for AIDS in the past, the published male/female ratio for AIDS-associated PCNSLs in adults is 7.4 to 1.8 (7, 19).
Similarly to the large majority of PPLs recorded, also in our patient a preoperative misdiagnosis of pituitary adenoma had been made. In the series of patients with PPLs examined by Giustina et al., only in one case was the presumptive diagnosis lymphoma of the brain (7). Recently Kosák et al. reported a new case of primary B-cell lymphoma of the hypothalamo-pituitary area, in which correct presumptive diagnosis of lymphoma had been made, based on the patient’s presentation, radiologic findings and cytologic analysis of the cerebrospinal fluid (21).
On imaging the differential diagnosis between PPL and a pituitary adenoma is not easy, but one should consider lymphoma when evaluating an invasive sellar mass that is iso - to hypointense on T1 - and T2-weighted magnetic resonance (MR) images (14, 22). The lack of T2 hyperintensivity can be explained by dense cellularity and high nucleus-to-cytoplasm ratio of these tumours. This MRI feature can be useful in differential diagnosis of these tumours. On the other hand PCNSLs are significantly hyperintense after contrast administration in MRI (14, 22).
Imaging studies performed were not suggestive of lymphoma in our case, however, there were some clinical symptoms, that pointed to non-pituitary lesion in our patient. These were severe headache, ocular motor nerve palsy, diabetes insipidus, and fever. Severe headache without growth hormone hypersecretion and coexisting signs of hypopituitarism with diabetes insipidus and/or cranial nerve involvement should prompt the clinical suspect of a nonpituitary etiology of sellar mass. From these, clinical diabetes insipidus at presentation is highly suggestive of a nonpituitary etiology of a sellar or parasellar mass (6). Interestingly, even in a clinicopathological examination of brain tissue taken postmortem from patients with PCNSLs carried out to determine the topographic involvement of the CNS, particularly the posterior but not anterior lobe of the pituitary gland was involved (23). As many as 25% of patients with nonpituitary sellar or parasellar masses have impairment of cranial nerves II, III, IV, and VI (6). Cranial nerve involvements due to the pituitary lymphoma have been reported in 7 out of 17 of the patients (7, 16, 18, 21). These findings may also have a more insidious onset, with variable presentations ranging from diminished abduction of the ipsilateral eye due to sixth nerve involvement to diplopia associated with ocular motor nerve compression, or facial pain if the first and second branches of the trigeminal nerve are affected (7). Neurological symptoms of PPLs strictly reflect tumour location. Intra - and suprasellar location is associated mainly with hypopituitarism and visual disturbances. Infiltration of hypothalamus is associated with water imbalance syndromes. Less common symptoms are altered sexual behavior and eating disorders (hyperphagia) (24). One should keep in mind, that pituitary tumors are rarely associated with fever (6); on the other side lymphomas, both Hodgkin and non-Hodgkin types are the most common neoplasms causing fever of unkown origin (FUO) (25), via the production of pyrogenic cytokines (26). Cases of PPL presenting as FUO have been recorded (16, 27), however in our case fever was thought to be associated with otitis media.
The vast majority (approximately 90-95%) of PCNSLs are non-Hodgkin diffuse large B-cell lymphomas (28). The remaining cases comprise even more rare pathological entities such as low-grade PCNSLs, T-cell lymphomas, and Burkitt lymphomas (5, 28), as in present case. Histological picture of neoplastic lymphoid cells with pale macrophages forming the “starry sky” is typical of but not unique to Burkitt lymphoma (29). Few cases of immunocompetent patients with the Burkitt type of PCNSL are reported in the literature (8–11). Spath-Schwalbe et al., reported a case of a highly malignant B-cell lymphoma of the Burkitt type that responded partially to methotrexate (10), Toren et al. (11) described the case of a 6-year-old immunocompetent girl whose clinical diagnosis was Guillain–Barré syndrome but whose immunological, cytological, and molecular CSF studies were diagnostic for primary CNS Burkitt lymphoma. Hochberg et al. (30) reported on an immunocompetent patient with PCNSL and serological evidence of recent primary infection with the EBV, suggesting that the lymphoma would have been induced by the virus. Finally, Monabati et al. (8) reported another case of an immunocompetent patient, in whom testing for the EBV produced negative results, who had a PCNSL in which histopathological studies revealed a high-grade non-Hodgkin lymphoma of the small, noncleaved, Burkitt type. In our HIV-negative patient the EBV status was not disclosed, however PPLs in association with EBV occur in a young, immunodeficient persons. In older persons there is no association with EBV (28).
In conclusion, PPL is an extremely rare cause of hypopituitarism. Although it can be undistinguishable from pituitary adenoma at imaging, one should consider lymphoma when evaluating an invasive sellar mass that is iso - to hypointense on T2-weighted MR images, particularly when the patient is immunocompromised or old and presents with diabetes insipidus, cranial nerve palsy and FUO in addition to the expected finding of hypopituitarism.
Abbreviations
AIDS – acquired immunodeficiency syndrome
CNS – central nervous system
EBV – Epstein-Barr virus
FUO – fever of unknown origin
MRI – magnetic resonance imaging
PCNSL, PCNSLs – primary central nervous system lymphoma(s)
PPL, PPLs – primary pituitary lymphoma(s)
Dr. Alexander Kreze Jr. is thank fully acknowledged for valuable suggestions during preparation of the manuscript.
*these authors contributed equally to the study
Mikuláš Pura, M.D.
Department of Endocrinology, the National Institute of Endocrinology and Diabetology,
034 91 Ľubochňa, Slovakia
fax: +421 444 306 322, e-mail: mikulas.pura@nedu.sk
Sources
1. Flowers, A.: Brain tumors in the older person. Cancer Causes Control., 2000, 7, s. 523–538.
2. Clayton, R. N.: Sporadic pituitary tumours: from epidemiology to use of database. Baillieres Clin. Endocrinol. Metab., 1999, 13, s. 451-460.
3. Gsponer, J., De Tribolet, N., Déruaz, J. P. et al.: Diagnosis, treatment, and outcome of pituitary tumors and other abnormal intrasellar masses. Retrospective analysis of 353 patients. Medicine, 1999, 78, s. 236–269.
4. Eby, N. L., Grufferman, S., Flannelly, C. M., Schold Jr., S., C., Vogel, F. S., Burger, P. C.: Increasing incidence of primary brain lymphoma in the US. Cancer, 1988, 62, s. 2461–2465.
5. Da Silva, A. N., Lopes, M. B., Schiff, D.: Rare pathological variants and presentations of primary central nervous system lymphomas. Neurosurg. Focus, 2006, 21, s. E7, [online]. American Association of Neurological Surgeons, 2006 [cit. 2008-01-04]. Dostupné na: <http://thejns.org/doi/pdfplus/ 10.3171/foc.2006.21.5.8>.
6. Freda, P. U., Post, K. D.: Differential diagnosis of sellar masses. Endocrinol. Metab. Clin. North. Am., 1999, 28, s. 81–117.
7. Giustina, A., Gola, M., Doga, M., Rosei, E. A.: Clinical review 136: Primary lymphoma of the pituitary: An emerging clinical entity. J. Clin. Endocrinol. Metab., 2001, 86, s. 4567–4575.
8. Monabati, A., Rakei, S. M., Kumar, P. V. et al.: Primary Burkitt lymphoma of the brain in an immunocompetent patient. Case report. J. Neurosurg., 2002, 96, s. 1127–1129.
9. Shehu, B. B.: Primary central nervous system Burkitt’s lymphoma presenting with proptosis. Ann. Trop. Paediatr., 2003, 23, s. 319–320.
10. Spath-Schwalbe, E., Genvresse, I., Stein, H. et al.: Primary cerebral highly-malignant B-cell lymphoma of the Burkitt type. Dtsch. Med. Wochenschr., 1999, 124, s. 451–455.
11. Toren, A., Mandel, M., Shahar, E., et al.: Primary central nervous system Burkitt’s lymphoma presenting as Guillain-Barre syndrome. Med. Pediatr. Oncol., 1994, 23, s. 372–375.
12. Fine, H. A., Mayer, R. J.: Primary central nervous system lymphoma. Ann. Intern. Med., 1993, 119, s. 1093–1104.
13. Snider, W. D., Simpson, D. M., Aronyk, K. E., Nielsen, S. L.: Primary lymphoma of the central nervous system associated with acquired immune-deficiency syndrome (Letter)., N. Engl. J. Med., 1983, 308, s. 45.
14. Kaufmann, T. J., Lopes, M. B., Laws Jr. et al.: Primary sellar lymphoma: radiologic and pathologic findings in two patients. AJNR Am. J. Neuroradiol., 2002, 23, s. 364–367.
15. Stephens, J. W., Morganstein, D. L., McLaughlin, J. E. et al.: Isolated B-cell lymphoma of the pituitary region: a rare clinical entity. Hosp. Med., 2002, 63, s. 306–307.
16. Huang, Y. Y., Lin, S. F., Dunn, P. et al.: Primary pituitary lymphoma presenting as hypophysitis. Endocr. J., 2005, 52, s. 543–549.
17. Rudnik, A., Larysz, D., Blamek, S. et al.: Primary pituitary lymphoma. Folia Neuropathol., 2007, 45, s. 144–148.
18. Wolfe, S. Q., Hood, B., Barker, J., Benveniste, R. J.: Primary central nervous system lymphoma mimicking pituitary apoplexy: case report. Pituitary, 2008, doi: 10.1007/s11102-008-0084-8.
19. Eichler, A. F., Batchelor, T. T.: Primary central nervous system lymphoma: presentation, diagnosis, and staging. Neurosurg. Focus 2006, 21, s. E16 [online]. American Association of Neurological Surgeons, 2006 [cit. 2008-01-04]. Dostupné na: <http://thejns.org/doi/pdfplus/10.3171/foc.2006. 21.5.16>.
20. Lee, J. H., Lee, H. K., Choi, C. T., Huh, J.: Mucosa-associated lymphoid tissue lymphoma of the pituitary gland: MR imaging features. AJNR Am. J. Neuroradiol., 2002, 23, s. 838–840.
21. Kosák, M., Obenberger, J., Campr, V. et al.: Clinical case seminar: Correct evaluation of the clinical course and radiologic findings leading to the exact presumptive diagnosis of primary hypothalamo-pituitary lymphoma. J. Clin. Endocrinol. Metab. 2008, submitted.
22. Erdag, N., Bhorade, R. M., Alberico, R. A. et al.: Primary lymphoma of the central nervous system: typical and atypical CT and MR imaging appearances. AJR Am. J. Roentgenol., 2001, 176, s. 1319–1326.
23. Onda, K., Wakabayashi, K., Tanaka, R., Takahashi, H.: Intracranial malignant lymphomas: clinicopathological study of 26 autopsy cases. Brain Tumor Pathol., 1999, 16, s. 29–35.
24. Baehring, J. M., Hochberg, F. H.: Central nervous system lymphoma in AIDS and non-AIDS patients. In: Black, P. M., Loeffler, J. S. (eds.). Cancer of the nervous system. Lippincott Williams and Wilkins, 2005, s. 589–603.
25. Hirschmann, J. V.: Fever of unknown origin in adults. Clin. Infect. Dis., 1997, 24, s. 291–300.
26. Dinarello, C. A., Bunn Jr, P. A.: Fever. Semin. Oncol., 1997, 24, s. 288–298.
27. Landman, R. E., Wardlaw, S. L., Connell, R. J. et al.: Pituitary lymphoma presenting as fever of unknown origin. J. Clin. Endocrinol. Metab., 2001, 86, s. 1470–1476.
28. Commins, D. L.: Pathology of primary central nervous system lymphoma. Neurosurg. Focus 2006, 21, s. E2 [online]. American Association of Neurological Surgeons, 2006 [cit. 2008-01-05]. Dostupné na: <http://thejns.org/doi/pdfplus/ 10.3171/foc.2006.21.5.3>.
29. Jaffe, E. S., Harris, N. L., Stein, H., Vardiman, J., W.: Pathology and genetics. Tumours of haematopoietic and and lymphoid tissues. Lyon: WHO classification of tumours, International Agency for Research on Cancer, 2001.
30. Hochberg, F. H., Miller, G., Schooley, R. T. et al.: Central-nervous-system lymphoma related to Epstein-Barr virus. N. Engl. J. Med., 1983, 309, s. 745–748.
Labels
Addictology Allergology and clinical immunology Angiology Audiology Clinical biochemistry Dermatology & STDs Paediatric gastroenterology Paediatric surgery Paediatric cardiology Paediatric neurology Paediatric ENT Paediatric psychiatry Paediatric rheumatology Diabetology Pharmacy Vascular surgery Pain management Dental Hygienist
Article was published inJournal of Czech Physicians

-
All articles in this issue
- Galectins in Squamous Cell Carcinomas of the Head and Neck Cancers
- Hiatal hernia and Barrett’s oesophagus Impact on symptoms occurrence and complications
- Primary B-cell pituitary lymphoma of the Burkitt type: case report of the rare clinic entity with typical clinical presentation
- Pathogenetically Complicated Case of Osteoporosis in a Young Man
- Rationality and Irrationality in the Medicine and in the Life
- Journal of Czech Physicians
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Galectins in Squamous Cell Carcinomas of the Head and Neck Cancers
- Rationality and Irrationality in the Medicine and in the Life
- Hiatal hernia and Barrett’s oesophagus Impact on symptoms occurrence and complications
- Primary B-cell pituitary lymphoma of the Burkitt type: case report of the rare clinic entity with typical clinical presentation
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

