-
Medical journals
- Career
Smrteľná otrava metadonom u 11-mesačného dieťaťa mužského pohlavia
: J. Šidlo; J. Valuch; P. Očko; J. Bauerová
: Institute of Forensic Medicine, School of Medicine, Comenius University and Health Care Surveillance Authority, Bratislava, Slovakia
: Soud Lék., 54, 2009, No. 2, p. 23-25
Úvod:
Počet prípadov smrteľných otráv metadonom u dospelých sa zvyšuje priamo úmerne s jeho využívaním v substitučnej liečbe závislostí od opiátov. Intoxikácia metadonom v detskom veku je zriedkavá. Možnosti jej diagnostiky na základe klinického nálezu sú často obmedzené. Cieľom práce je demonštrovať prípad 11-mesačného dieťaťa mužského pohlavia, ktoré zomrelo náhle, bez údajov predchádzajúceho ochorenia.Metódy:
Rutinnými metódami bola vykonaná kompletná morfologická analýza prípadu. Chemicko-toxikologické vyšetrenie bolo zamerané na zistenie prítomnosti etanolu, psychoaktívnych a ďalších forenzne významných látok v dostupných biologických materiáloch.Výsledky:
Morfologické nálezy boli nešpecifické. Chemicko-toxikologickým vyšetrením biologických materiálov nebola zistená prítomnosť etanolu v telesných tekutinách. V analyzovaných materiáloch bola zistená prítomnosť metadonu v nasledovných koncentráciách: v krvnom sére 1,3 μg/mL, (po prepočte 0,7 μg/mL v plnej krvi), v pečeni 5,0 μg/g, v obličke 2,6 μg/g a v moči 3,2 μg/mL.Záver:
Príčina smrti 11-mesačného dieťaťa mužského pohlavia, ktoré bolo odoslané na pitvu s diagnózou syndrómu náhleho úmrtia dieťaťa, bola stanovená ako smrteľná intoxikácia metadonom. Na základe zistených výsledkov chemicko-toxikologického vyšetrenia okrem stanovenia diagnózy otravy nie je možné sa vyjadriť k otázke opakovaného podania metadonu. Je vysoko pravdepodobné, že metadon bol dieťaťu podaný inou osobou. Matka ani jej druh, ktorý nebol otcom dieťaťa, nie sú evidovaní v centre pre liečbu drogových závislostí, a tak pôvod a zdroj metadonu ostáva aj naďalej neznámy.Kľúčové slová:
metadon – dieťa – smrteľná intoxikácia – toxikologické vyšetrenieIntroduction
Methadone is a synthetic opioid narcotic analgesic prescribed for the relief of moderate-to-severe pain. It is also used in the detoxication treatment of opiate dependence, and for maintenance in heroin and narcotic addiction. Recreationally, methadone is abused for its sedative and analgesic effects (2). Due to its chemical composition it is fully a synthetic substance – diphenylpropylamine opioid. Although it is chemically different from morphine, it has clinically similar actions and analgesic effects. It is characterised by its effects on the central nervous system where performing as a long-acting μ opioid receptor agonist. Methadone is primarily administered orally, it is well absorbed from the gastrointestinal tract and 30 minutes after ingestion of therapeutic dose measurable amounts are present in plasma. Peak plasma concentrations after therapeutic doses occur within 2–4 hours. In comparison with opioids it has typically a long half life of 10–18 hours, but it can be as much as 25 hours or longer, Couper et al. (2) state a half life even up to 60 hours. Clinical effects can last up to 72 hours in some subjects after a single oral dose. Because of the long half life methadone can be prescribed just once daily. Methadone does not produce the instant euphoria of heroin (7). In Slovakia methadone is available as a solution. It is characterised by the sedative effects on the body; it evokes drowsiness, dysphoria and altered sensory perception. The adverse effects include respiratory depression, exacerbation of present asthma, hypotension, nausea, vomiting, constipation and miosis. Some of the above mentioned adverse effects can grow into tolerance. Overdosing is characterised by respiratory depression, extreme somnolence progressing into stupor or coma, maximum constriction of the pupils, skeletal muscle flaccidity, clammy skin, sometimes with present bradycardia, hypotension. Serious overdosing can be accompanied by apnoea, circulatory collapse, cardiac arrest and death (6). While in adults methadone is used for therapeutic purposes, in infants it acts as a poison even in relatively small doses. In general, methadone intoxication in child age occurs rarely and its diagnostic possibilities are often limited on the basis of clinical findings. The number of intoxication cases in infants is increasing in parallel with the increase of methadone usage in opiate withdrawal therapy in adults (8).
The aim of the work is to demonstrate a case of an 11-month-old male infant who unexpectedly died without a previous disease history.
According to the investigated circumstances a mother placed the child into a crib at 09 : 15 a.m. where he fell asleep. At approximately 10 : 00 while sleeping he moved. At 10 : 45 the mother found the child lying on the abdomen without showing vital signs. The child was resuscitated in a layman’s way and the emergency service was called immediately. On arrival of emergency services the child was found unresponsive, did not breathe, the pulse was nonpalpable. Immediately the extended complex resuscitation was initiated despite which the child was pronounced dead. A physician called in established the diagnosis of sudden infant death syndrome (SIDS) and ordered to perform an autopsy.
Methods
In the period of 23 hours after the death a standard autopsy of the body of an 11–month-old male infant was performed. At autopsy the specimens of brain, salivary gland, thyroid gland, thymus, heart, lungs, liver, pancreas, spleen, adrenal gland, kidney, small and large intestine and lymph nodes were taken for histopathologic examination. The specimens were processed by standard methods and examined by a method of light microscopy. The specimens of blood, urine, liver and kidney were taken for toxicological analysis. Blood and urine specimens underwent an alcohol analysis for ethanol and other volatile substances by gas chromatography. Urine specimen underwent a screen for drugs of abuse and several prescription drug classes using a method of group immunochromatographic semi-quantitative screening focused on the following substances: amphetamines, barbiturates, benzodiazepines, cannabinoids, cocaine, methamphetamines, methadone, opiates, phencyclidine and tricyclic antidepressants. Blood, urine, liver and kidney specimens were examined by a method of high performance thin layer chromatography (HPTLC) with the follow-up densitometry both having been preceded by the isolation of possible medicaments using the Faragó’s method followed by fractionated ether extraction and by gas chromatography-mass spectrometry (GC-MS). Positive findings were confirmed using GC-MS.
Results
At autopsywithin the external examination only the signs of resuscitation were detected (cannula in the mouth, scanning electrodes on the chest, intravenousline in the left elbow fossa and multiple traces of injection insertions in the left groin region). Within the internal examination the brain oedema and enlargement of spleen, lymph nodes and thymus gland were detected. The microscopic histopathologic examination revealed the brain oedema, acute pulmonary emphysema, acute venostasis in the spleen and dilatation of proximal tubules together with medulla congestion in the kidney. In the toxicological analysis no presence of ethanol or other volatile substances was detected. Methadone was detected in specimens of all investigated post-mortem fluids and tissues in the concentrations shown in Table 1.
1. Methadone concentration in the post-mortem fluids and tissues of a 11-month-old male infant 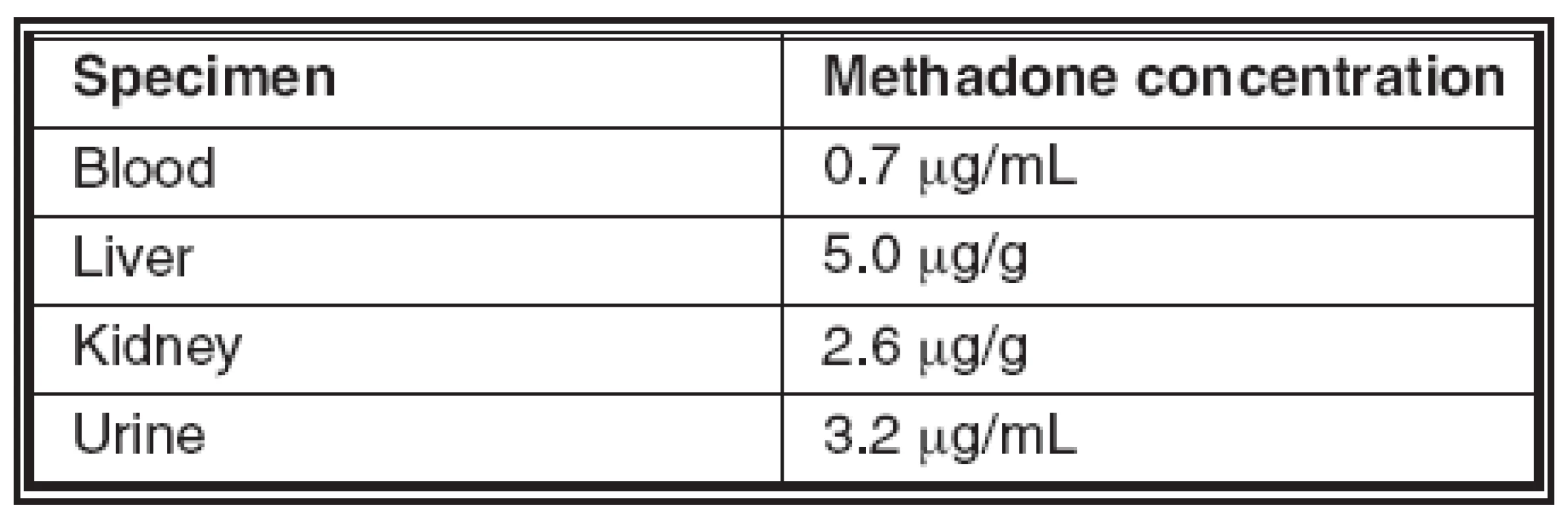
Discussion and conclusion
On the basis of results obtained at autopsy and the follow-up laboratory examinations the cause of death in an 11-month-old male infant was determined to be methadone intoxication.
As resulting from literature data the problems of establishing the diagnosis of methadone intoxication is relatively difficult. Morphological post-mortem examination in the majority of cases fails to contribute to the final diagnosis and the only one positive finding is the methadone presence in bodily fluids and organs. However, its concentrations vary from case to case in a relatively great range, thus giving rise to the discussion on the issue of the level of lethal methadone concentration. Medical examiners and toxicologists are often criticised by clinicians for over diagnosing fatal methadone intoxications on the basis that the concentrations recommended for maintenance treatment are above those at which death is ascribed to methadone intoxication. (5). In adults a therapeutic methadone concentration in plasma serving for monitoring withdrawal symptoms ranges between 150–200 μg/L and as a maintaining level is determined to a concentration of 400 μg/L and more (7). The papers dealing with studying larger groups of lethal methadone intoxications present the following concentration ranges of methadone in cadaverous blood. Clark et. al. state the concentrations from 200 to 1863 μg/L (mean 560 μg/L) in the group of 18 cases of intoxications involving 17 adults and one 3-year-old-female child (1). Milroy and Forrest analysed 55 cases, where methadone intoxication was given as the sole cause of death. Fifty victims were adults, with five victims under 14 years of age. The mean methadone concentration in the adult deaths was 584 μg/L, range 84–2700 μg/L (7). Segal and Catherman quoted concentrations of 100–2500 μg/L (mean, 1100) for deaths after intravenous administration and 100–2600 μg/L (mean, 393) after oral administration (9). Worm and colleagues examined 59 cases of methadone deaths and they found the methadone range 60–3090 μg/L (mean, 430). They also compared 11 deaths in people in a methadone programme with 11 deaths in people not in any such programme. The blood methadone range in those on treatment was 30–1240 μg/L (mean, 470). In those not in a maintenance programme, the methadone range was 30–990 μg/L (mean, 270) (11). One of the factors affecting the variation in post-mortem concentrations is post-mortem methadone redistribution between bodily fluids and tissues. Diffusion from the stomach is possible and this might affect concentrations in heart blood. Compounding this is the problem of release of methadone from the liver, which again might affect blood concentrations. Movement of methadone from other tissues to blood and vice versa all contribute to the problems of determining an accurate concentration of methadone in relation to the cause of death. The distribution of methadone might also depend on whether methadone has been injected (9).
The data on childhood deaths are limited. The five cases seen in the study of Milroy and Forrest had methadone concentrations between 200 and 489 μg/L (7). In two deaths reported by Smialek and colleagues of a 1-year-old boy and a 3-year-old girl both had methadone concentrations of 110 μg/L (10). These findings support the opinion that only relatively small amounts of methadone are required to kill a child. Other cases of methadone intoxication in children were reported within another study done in Maryland (1992–1996) were 4 infants died. In one case a 4-year-old child died as a result of ingesting methadone, which was stolen from a methadone clinic by his grandmother who was a nurse at the clinic. Another case involved the death of a 4-month-old boy who had been given methadone by his grandmother because he was „sick and irritated“. The third case involved a 5-year-old girl who had ingested some of the methadone illegally acquired by her mother. The fourth case involved a 3-year-old boy who had reportedly drank some orange juice containing methadone that his mother, a recovering heroin addict in the methadone programme, had left in the fridge (4). Accidental contamination of amoxicillin dispensed for a 41/2-year-old boy, in a pharmacy, which was also a methadone maintenance centre has been reported (3).
It indicates several manners of ingesting a drug into the infant’s body. There have been reported cases of methadone intoxication due to its administration by another person, intoxications “in utero”, the excretion of this substance into breast milk was confirmed. However, apparently the most frequent cause in older children remains an accidental ingestion of methadone being carelessly stored, when methadone was prescribed to one of the parents or their partner or it was obtained illegally (4).
The very similar case to the one we report regarding the infant’s age, a determined methadone concentration in blood and the manner of intoxication was reported by Couper et al. It involved a 10-month-old female infant whose mother started to administer the liquid methadone semi-regularly to stop the child from „crying and fussing“. She would either add the methadone to the infant’s formula and feed the child over a period of time, or directly administer the methadone to the infant via the dropper. This occurred for several months leading up to withdrawal symptoms, which would appear to the mother as “fussing“ and irritability. This would subsequently prompt the mother to administer another dose of methadone to sedate the child. On the day of infant’s death, the mother admitted to administering approximately twice the amount of methadone she normally gave her child. The infant was found unresponsive in her crib the next morning. By post-mortem analysis of blood specimen the methadone was detected at a concentration of 670 μg/L. The cause of death was determined to be methadone intoxication, and manner of death was homicide (2).
In our case the determined methadone concentration in blood reached 700 μg/L. The above mentioned concentration, the same as in the previous case, is multiple higher than the concentrations quoted in literature data. On the basis of such matter of fact it is possible to claim that in both above mentioned cases the diagnosis of methadone intoxication is undisputed. Similarly the only possibility of entering the methadone into the child’s body in our case was its administration by another person. One of the reasons can be the effort to sedate the child. On the basis of the investigated circumstances and autopsy results together with follow-up laboratory examinations it is not possible to answer the question of repeated methadone administration as well. The subsequent police investigation failed to reveal any new facts regarding the circumstances of child’s death. It was found out that neither mother nor her partner who was not the infant’s father is registered in the Centre for Treatment of Drug Dependencies and thus the origin and source of the methadone still remains unknown. Both partners together with their 5-year-old daughter shortly after death of child moved from a town and their whereabouts is unknown.
The case is instructive also with respect to the initially made diagnosis of SIDS by a physician. It is necessary to take into consideration a possible intoxication in a differential diagnosis of SIDS and through a complex post-mortem toxicological analysis to rule it out in justified cases.
Acknowledgements
Anna Cibulková, Institute of Foreign Languages, Faculty of Medicine Comenius University Bratislava, Slovakia
Address for correspondence:
Jozef Šidlo, MD., PhD.
Institute of Forensic Medicine, School of Medicine, Comenius University and Healthcare Surveillance Authority, Antolská 11, 857 01 Bratislava, Slovakia
tel: ++421259357264, ++421268672349, ++421904819241
fax: ++42163531990
Sources
1. Clark, J.C., Milroy, C.M., Forrest, A.R.W.: Deaths from methadone use. Journal of Clinical Forensic Medicine, 2, 1995, pp. 143–144.
2. Couper, F.J., Chopra, K., Pierre-Louis, M.L.Y.: Fatal methadone intoxication in an infant. Forensic Sci. Int., 153, 2005, pp. 71–73.
3. Lalkin, A. et al.: Contamination of antibiotics resulting in severe pediatric methadone poisoning. Ann. Pharmacother., 33, 1999, pp. 314–317.
4. Li, L., Levine, B., Smialek, J.E.: Fatal methadone poisoning in children: Maryland 1992–1996. Subst. Use Misuse, 35, 2000, pp. 1141–1148.
5. Merril, J., Garvey, T., Rosson, C.: Methadone treatment: methadone concentrations taken as indicating deaths due to overdose need to be reviewed. BMJ, 313, 1996, p. 1481.
6. Methadone solution – summary of characteristic features. Available on: <http://www.sukl.sk> (in Slovak)
7. Milroy, C.M., Forrest, A.R.W.: Methadone deaths: a toxicological analysis. J. Clin. Pathol., 53, 2000, pp. 277–281.
8. Riascos, R., Kumfa, P., Rojas, R., Cuellar, H., Descartes, F.: Fatal methadone intoxication in a child. Emerg. Radiol. 15, 2008, pp. 67–70.
9. Segal, R.J., Catherman, R.L.: Methadone – a cause of death. J. Forensic Sci., 19, 1974, pp. 575–584.
10. Smialek, J.E., Monteforte, J.R., Aronow, R. et al.: Methadone deaths in childhood. JAMA, 238, 1977, pp. 2516–2517.
11. Worm, K., Steentoft, A., Krinsholm, B.: Methadone and drug addicts. Int. J. Legal Med., 106, 1993, pp. 119–123.
Labels
Anatomical pathology Forensic medical examiner Toxicology
Article was published inForensic Medicine

2009 Issue 2
Most read in this issue
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

