-
Medical journals
- Career
Occurrence of acute retrobulbar hemorrhage during birth
Authors: K. Hurt 1; A. Krajcová 2; M. Zikán 1
Authors‘ workplace: Department of Gynecology and Obstetrics, First Medical Faculty, Charles University and Teaching Hospital Bulovka, Prague 1; Epilaser, Department of Plastic Surgery, Prague 2
Published in: Ceska Gynekol 2024; 89(1): 30-33
Category: Case Report
doi: https://doi.org/10.48095/cccg202430Overview
Objective: Presentation of acute retrobulbar subperiostal hemorrhage (hematoma) in the course of delivery. The occurrence, possible threats and recommended methods of treatment are described. Introduction: Acute retrobulbar hemorrhage is always a serious condition. Even if not connected with other ocular trauma, it could cause permanent blindness. The reason is based on constriction of the eye, decreasing of the blood supply and thus disruption of the oxygen supply to sensitive retinal tissues. After a short time, these tissues start to deteriorate and lose their natural function. This event is often connected with exophthalmia and diplopia. The primary diagnostic procedure is to measure intraocular pressure (IOP). Even if the ideal diagnostic tools are not accessible, performing a lateral canthotomy (event. with inferior cantholysis) is recommended to relieve IOP in acute situations. Normal intraocular pressure is considered to be 8–21 mmHg. Case report: Our 29-year-old female patient was in the second stage of delivery and suddenly got retrobulbar hemorrhage, resulting in exophthalmia and diplopia. Her baby was delivered shortly after the event. The following delivery course was normal, including her perineum repair and puerperium. Our patient was fortunate because her visual acuity and IOP were normal. Therefore, we chose an observational treatment strategy. After 5 weeks, we noted successful disintegration of the hematoma and decreased exophthalmia and diplopia without other consequences. Conclusion: We described retrobulbar subperiostal bleeding in our patient in the course of delivery. We depicted possible threats that could result in blindness and described recommended methods of treatment. Even if such a situation is extremely rarely, we believe that knowledge of these guidelines could help medical professionals broaden their treatment options. This particularly occurs when a trained eye surgeon is not available.
Keywords:
intraocular pressure – diplopia – retrobulbar hemorrhage – orbital compartment syndrome – lateral canthotomy – cantholysis
Introduction
Acute retrobulbar hemorrhage (ARH – non-traumatic origin) is an extremely rare emergency during delivery [1–3]. These ARHs could be anatomically divided into the following groups:
- subperiosteal;
- diffuse;
- localized in peribulbar muscles and often associated with orbital floor implants.
It persists until complete resorption and recovery. The longest resorption of subperiosteal hemorrhages often persists for over a month. Orbital space comprises of three compartments: subperiosteal, intraconal and extraconal. If hemorrhage occurs in one of these compartments, a forward protrusion of the globe and proptosis appear [4–6]. Diplopia is practically present in all cases if there is no full amblyopia. Even a minor increase in volume could rapidly lead to a rise in intraocular pressure (IOP; normal IOP is 8–21 mmHg). The lack of compartment volume could cause a rapid increase in IOP, leading to orbital compartment syndrome (OCS) followed by progressive vision loss. If not treated properly, it could lead to permanent blindness. The lids and orbit in the front constrain the eye. Thus, a rise in IOP could rapidly compress the optic nerve and its vascular supply.
The posterior ciliary artery is affected more than the central retinal artery (CRA). CRA is better protected because the optic nerve covers it. Higher systolic pressure is also one mechanism protecting the CRA. There is no similar protection in other blood vessels inside the body’s muscle cone system. Complete visual loss could be due to CRA occlusion and anterior ischemic optic neuropathy.
Non-traumatic ARH is mainly caused by vascular malformation, increased venous pressure from various origins, or both. The orbital venous system is unique in its anatomy. Contrary to other venous systems in the body, orbital veins do not have any valves. Therefore, increased pressure in other body veins directly leads to increased pressure in subperiosteal orbital veins, which could cause rupture and bleeding.
Management of diagnostics in patients with ARH involves several steps. First, the reaction to light must be evaluated. This reaction is of major importance regarding optical nerve function. Pupil dilation and fundus examination could be postponed after responses to the light. When one eye is exposed to light, bilateral pupil constriction is present, meaning an afferent signal to the brain and an efferent signal from the brain work properly. When the reaction is abnormal, both pupils stay dilated. The constriction of both pupils indicates that the optic nerve in the exposed eye is not damaged.
The main indication of OCR is intense pressure in the affected eye. It should be measured directly or at least tentatively via palpation methods. It is believed that lowering the pressure is necessary to restore and recover the affected eye. More than 2 hod of pressure may cause irreparable harm to vision [7]. There are operative procedures (e. g., lateral canthotomy) which could be extended with cantholysis (LCC) that can free the bulb of the eye, reduce the pressure exerted on the orbit by the eyelids, and decrease IOP (Fig. 1) [8]. Ideally, a trained ophthalmologist should perform this procedure. However, such help is usually unavailable in such a short time. Therefore, trained surgeons could resolve this issue and save the patient’s vision. Lateral canthotomy and inferior cantholysis could soon be performed under local anesthesia as emergency surgery [9–11].
Medical treatment can be used before or after surgical treatment of ARH. Such treatment mainly focuses on using osmotic agents, including mannitol, b-blockers, and the anti-inflammatory effects of corticosteroids.
After all these approaches, we have to point out that if the IOP follows normal values, even when ARH is confirmed and diplopia is present, we prefer to start with an observational approach over operative techniques.
1. Lateral canthotomy and cantholysis. // Laterální kantotomie a kantolýza. 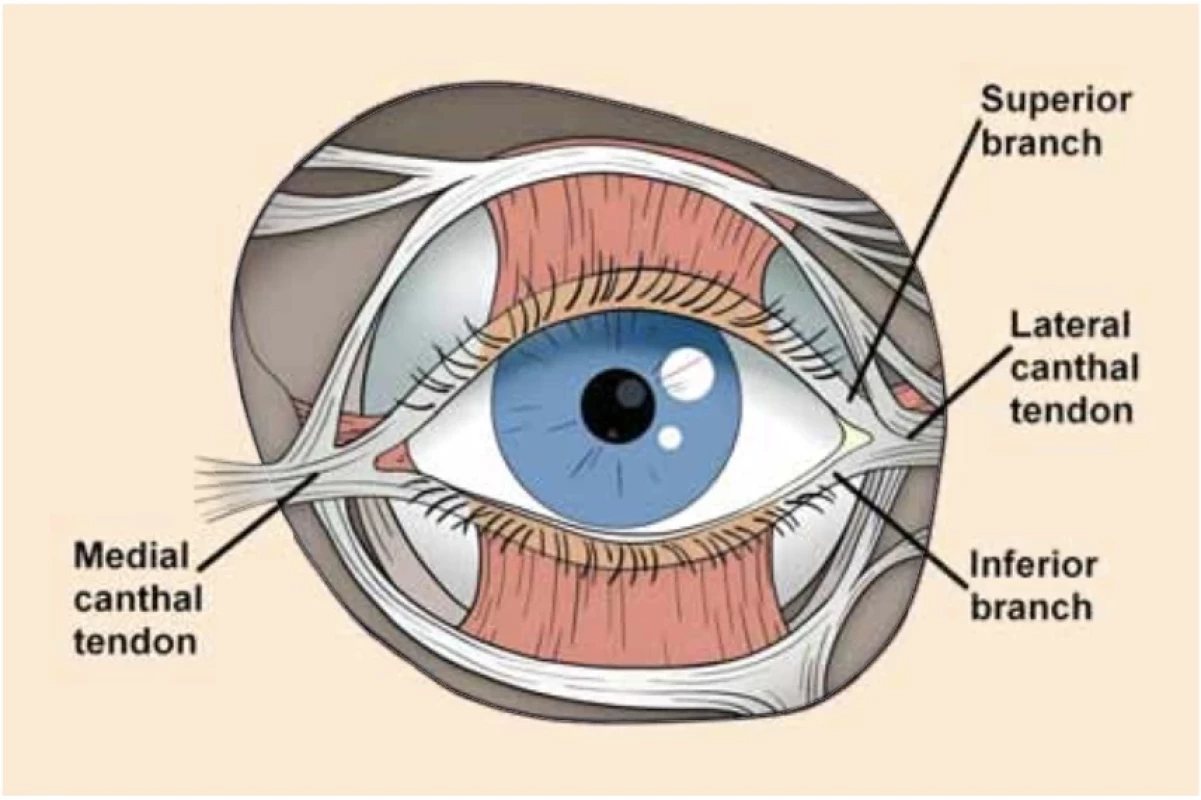
Case Report
A 29-year-old primipara was admitted to our obstetrical department in her first stage of delivery. All examinations were normal. The fetus was in a flexed occipito-posterior position. All other examinations, including ultrasound and CTG, did not divert from the norm. The patient’s history was also without noticeable deviations. Our patient insisted on a non-medicinal course of delivery.
2. Protrusion of the right eye. // Protruze pravého oka. 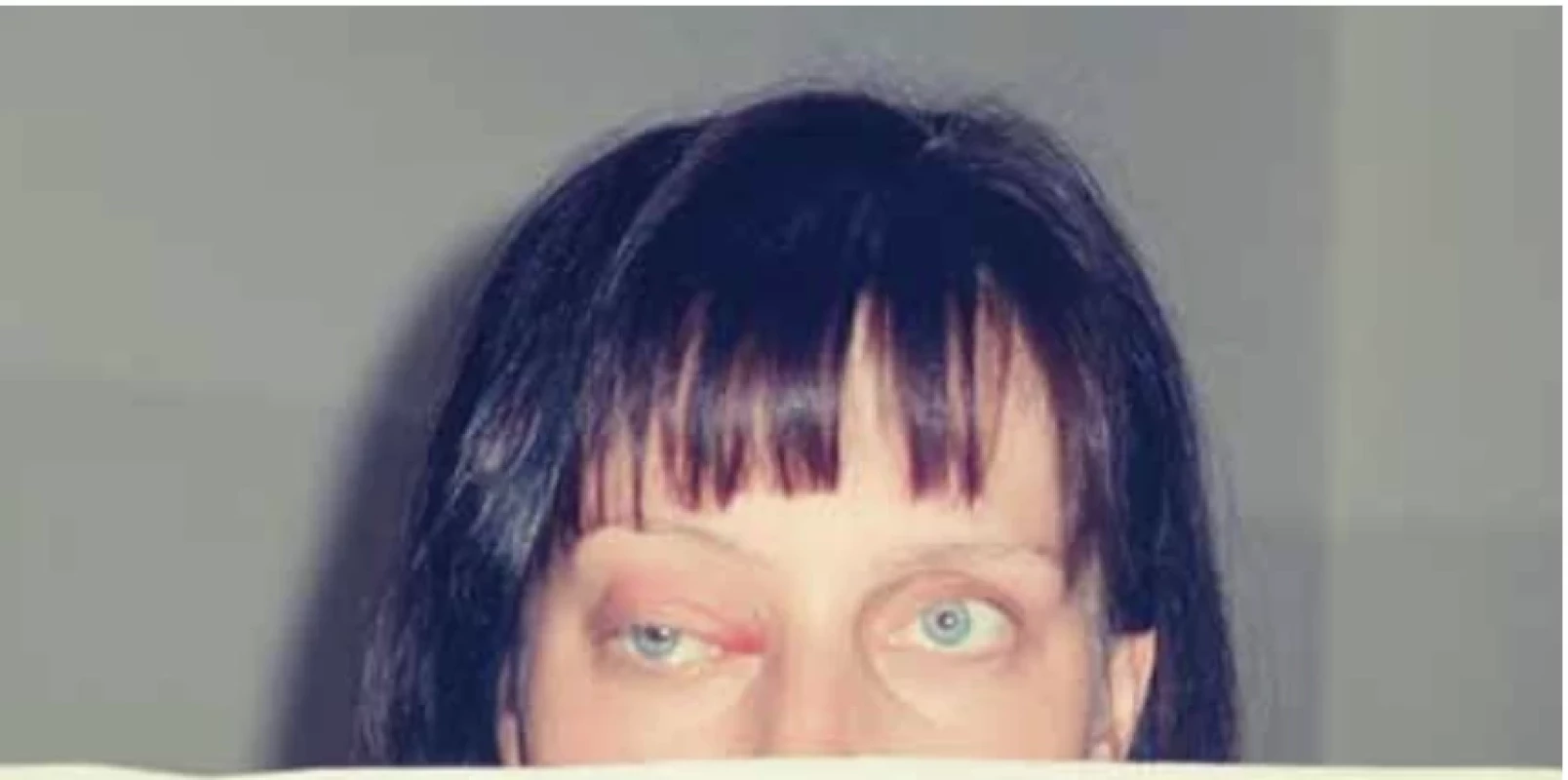
3. Retrobulbar subperiosteal hematoma. // Retrobulbární subperiostální krvácení. 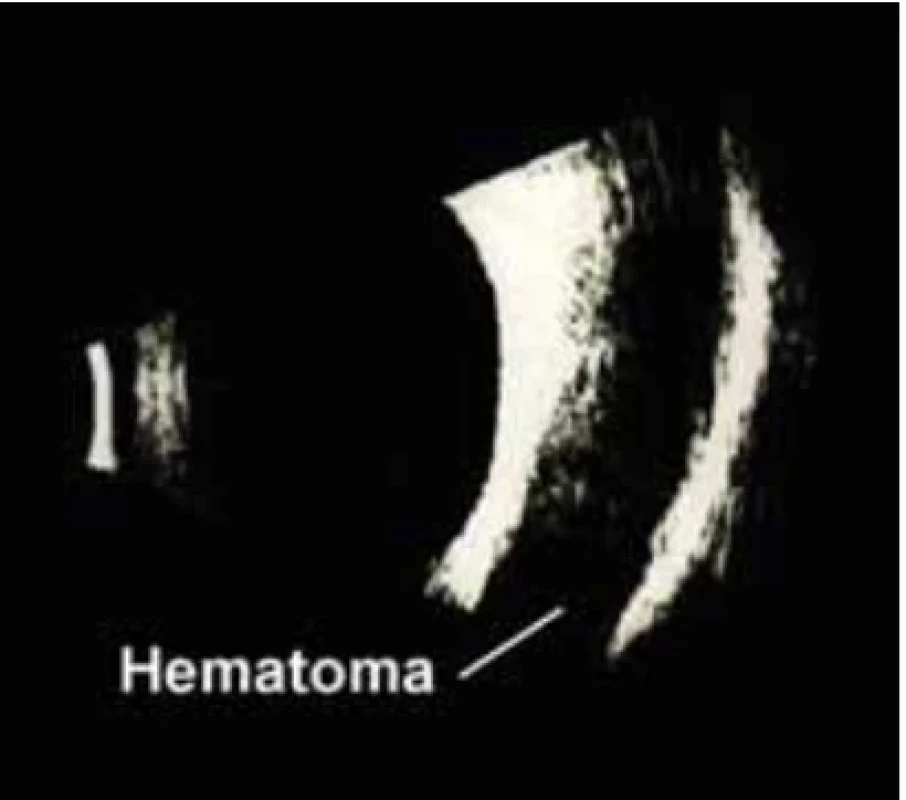
The first stage lasted 3.5 hod and the second lasted 15 min. Half a minute before fetal delivery, the patient reported a sudden pain in her right eye. An episiotomy was performed, and the fetus was delivered without complications. The normality of birth continued uneventfully in her third stage (5 min) and during perineal repair. A fetus (weight 3,200 g, length 50 cm, Apgar 10-10-10) was utterly free of pathologies.
Shortly after delivery, the patient experienced exophthalmia in her right eye, which left her with diplopic vision. Her blood pressure was 124 over 77, and her pulse was 88.
An ophthalmologist was consulted. A protrusion of the right eye with diplopia was confirmed (Fig. 2). Reaction to light and a fundus examination were normal. IOP was measured and found to be normal (20 mmHg).
Signs of retrobulbar subperiosteal hematoma were revealed based on ultrasonography (Fig. 3) and nuclear magnetic resonance imaging.
Because of the examinations mentioned above, especially IOP, it was decided not to perform LCC on her right eye. This decision was made because the pressure was normal, so we continued conservative treatment (i.e., observational therapy). The only medication on the first day was an infusion with mannitol (500 ml) to ensure a conservative approach. The patient was examined daily for IOP, which is believed to be a crucial decision-procedure. Based on the patient’s request, she was released from the department after two weeks of observational treatment and checked daily at an outpatient clinic. The patient was informed that the department must evaluate every adverse event immediately. Five weeks after delivery, the hematoma was fully resorbed, and even the exophthalmia with diplopiadisappeared.
Discussion
Acute retrobulbar bleeding resulting in hematoma is generally hazardous, resulting in vision loss in a few hours. High IOP can decrease the oxygen supply of the retina through its low blood perfusion. When diagnosed, it must be immediately treated with LCC. In rare cases IOP persists normal, perfusion is not impacted and surgery is not required. Our case was such a rare case. In our patient all examinations were normal, including coagulation tests. We hypothesize that there was bleeding into the subperiosteal space due to vascular malformation combined with increased venous pressure caused by strenuous pushing in the second delivery stage [1,12–14].
Conclusion
This paper describes a course of retrobulbar subperiostal bleeding and simple guidelines for saving the patient’s sight. The patient was in the second stage of delivery when the event started. We depicted our experience in this field of an extremely rare event of ARH where, thankfully, surgery was unnecessary. Even if such a situation comes extremely rarely, we think that knowledge of these guidelines could help medical professionals to broaden their treatment approach. This particularly occurs when a trained eye surgeon is not available.
Submitted/Doručeno: 5. 9. 2023
Accepted/Přijato: 18. 9. 2023Karel Hurt, MD, PhD, DrSc
Department of Gynecology and Obstetrics
First Medical Faculty
Charles University
Teaching Hospital Bulovka, Prague
Budínova 2
180 00 Prague
karel.hurt@lf1.cuni.cz
Sources
1. Jacobson DM, Itani K, Digre KB et al. Maternal orbital hematoma associated with labor. Am J Ophthalmol 1988; 105 (5): 547–553. doi: 10.1016/0002-9394 (88) 90249-8.
2. Bach CA, Coquille F, Toussain G et al. Subperiostal orbital hemorrhage induced by effort for vomiting. Rev Stomatol Chir Maxillofac 2010; 111 (4): 225–227. doi: 10.1016/j.stomax.2009.05.007.
3. McNab AA. Nontraumatic orbital hemorrhage. Surv Ophthalmol 2014; 59 (2): 166–184. doi: 10.1016/j.survophthal.2013.07.002.
4. Chan HH, Hardy TG, McNab AA. Spontaneous orbital hemorrhage related to the extraocular muscles. Ophthalmic Plast Reconstr Surg 2019; 35 (3): 256–261. doi: 10.1097/IOP.000 0000000001223.
5. Tran KD, Scawn RL, Whipple KM et al. Mastication induced retrobulbar hemorrhage. Orbit 2013; 32 (6): 387–388. doi: 10.3109/01676830. 2013.815229.
6. Vassallo S, Hartstein M, Howard D et al. Traumatic retrobulbar hemorrhage: emergent decompression by lateral canthotomy and cantholysis. J Emerg Med 2002; 22 (3): 251–256. doi: 10.1016/s0736-4679 (01) 00477-2.
7. Erickson BP, Garcia GA. Evidence-based algorithm for the management of acute traumatic retrobulbar haemorrhage. Br J Oral Maxillofac Surg 2020; 58 (9): 1091–1096. doi: 10.1016/j.bjoms.2020.05.026.
8. Hislop WS, Dutton GN, Douglas PS. Treatment of retrobulbar haemorrhage in accident and emergency departments. Br J Oral Maxillofac Surg 1996; 34 (4): 289–292. doi: 10.1016/s0266-4356 (96) 900004-2.
9. Pamukcu C, Odabaşi M. Acute retrobulbar haemorrhage: an ophthalmologic emergency for the emergency physician. Ulus Travma Acil Cerrahi Derg 2015; 21 (4): 309–314. doi: 10.5505/tjtes.2015.16768.
10. Rampat R, Gupta A, Henderson H et al. Nontraumatic orbital hemorrhage during uncomplicated labor. Ophthalmic Plast Reconstr Surg 2019; 35 (2): e54. doi: 10.1097/IOP.0000000000 001227.
11. Winterton JV, Patel K, Mizen KD. Review of management options for a retrobulbar hemorrhage. J Oral Maxillofac Surg 2007; 65 (2): 296–299. doi: 10.1016/j.joms.2005.11.089.
12. Christie B, Block L, Ma Y et al. Retrobulbar hematoma: a systematic review of factors related to outcomes. J Plast Reconstr Aesthet Surg 2018; 71 (2): 155–161. doi: 10.1016/j.bjps.2017.10.025.
13. Różańska-Walędziak A, Szewczuk O, Walędziak M et al. Spontaneous unilateral exophthalmos after a vaginal delivery. Eur J Ophthalmol 2021; 31 (3): NP57–NP59. doi: 10.1177/11 20672120914534.
14. Tan JC, Chan EW, Looi A. Bilateral orbital subperiosteal hemorrhage following labor. Ophthalmic Plast Reconstr Surg 2011; 27 (3): e59–e63. doi: 10.1097/IOP.0b013e3181e97 a7b.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicine
Article was published inCzech Gynaecology

2024 Issue 1-
All articles in this issue
- Preoperative and postoperative staging in endometrial cancer – a prospective study
- Importance of vaginal packing after laparoscopic sacrocolpopexy – retrospective study
- Discrepancies in staging and perioperative classification of pelvic endometriosis according to #Enzian 2021
- Pandemic fear and psychological resilience in pregnant women after the pandemic – a study in Turkey
- Occurrence of acute retrobulbar hemorrhage during birth
- Occult invasive cervical cancer, FIGO stage III, with a negative Pap smear test – clinical presentation and brief review of the literature
- Primary perineal endometriosis – a case report and literature review
- Ultrasound finding of endometrial polyp and factors increasing risk of malignancy
- Female orgasm, reproduction and couple relationships
- Uterovesical fistula and its treatment in Sub-Saharan Africa
- Birth plan – legal and medical aspects
- New recommendations for informing patients and gamete donors in assisted reproduction
- Diagnostika a léčba endometriózy
- Czech Gynaecology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ultrasound finding of endometrial polyp and factors increasing risk of malignancy
- Diagnostika a léčba endometriózy
- Importance of vaginal packing after laparoscopic sacrocolpopexy – retrospective study
- Female orgasm, reproduction and couple relationships
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

