-
Medical journals
- Career
SIMULTANEOUS BILATERAL ACUTE ANGLE-CLOSURE GLAUCOMA IN MILLER FISHER SYNDROME
Authors: J. Štěpánková 1; L. Kinštová 2; I. Gažová 2; M. Kodetová 1; J. Cendelín 1,3; N. Ondrová 1; D. Dotřelová 1
Authors‘ workplace: Oční klinika dětí a dospělých 2. LF UK a FN Motol, přednosta prof. MUDr. Dagmar Dotřelová, CSc., FEBO 1; Neurologická klinika 2. LF UK a FN Motol, přednosta prof. MUDr. Petr Marusič, Ph. D. 2; Oční centrum OFTA, Plzeň, primář MUDr. Jiří Cendelín, CSc. 3
Published in: Čes. a slov. Oftal., 75, 2019, No. 4, p. 210-218
Category: Case Report
doi: https://doi.org/10.31348/2019/4/5Overview
Purpose: To report a case of patient with Miller Fisher syndrome, complicated by simultaneous bilateral acute angle-closure glaucoma in her slightly (+1.5) hyperopic eyes.
Methods: We present a case report of a 71-year-old female patient presenting with total ophthalmoplegia, areflexia, ataxia and bilateral acute angle-closure glaucoma.
Results: The initial ocular examination revealed hand motion in the both eyes and oedematic corneas. Initial intraocular pressure was immeasurable high (measurment by Tonopen Avia). Measurement was possible after intravenous Mannitol 20 % infusion on both eyes as 54 and 56 mm Hg, respectively. Local medical therapy of pilocarpine, timolol, dorsolamide and dexamethasone improve intraocular pressure into normal limits within several hours. Prophylactic peripheral Nd-YAG laser iridotomy was performed on a both eyes two days later. Systemic treatment involved plasma exchange and rehabilitation program. Subsequent cataract surgery on both eyes with posterior capsule lens implantation improve the best corrected visual acuity on right eye from 0.5 to 1.0 and the left eye from 0.5 to 0.8, respectively. Intraocular pressure is within normal limits without any glaucoma therapy. Follow up period is three years.
Conclusions: This is the second reported case of patient with Miller Fisher syndrome and simultaneous bilateral acute angle-closure glaucoma and the fifth reported case of Miller Fisher syndrome and acute angle-closure glaucoma. Treatment for both conditions made a very good recovery.
Keywords:
Miller Fisher syndrome – bilateral acute angle-closure glaucoma – acute angle-closure glaucoma
INTRODUCTION
Simultaneous bilateral acute angle-closure glaucoma ranks among rare findings. Miller Fisher syndrome (MFS) is described as a rare variant of Guillain-Barré syndrome (GBS). MFS is an acute post-infection immunity mediated polyradiculoneuropathy, characterised by ophthalmoplegia, ataxia and areflexia, which was first described by Fisher in 1956 (40). It is estimated that in Europe and the USA it represents 1-5% of cases of GBS, although in South-East Asia higher percentages have been published (2). MFS is different from other forms of GBS in its characteristic rapid onset of ophthalmoplegia, occurrence of anti-glycolipid antibodies (Anti-GQ1b antibodies) with an affinity for the oculomotor nerves and peripheral nervous system, and in its clinically good prognosis, with correction within a number of weeks to maximally months, regardless of the selected treatment. The described treatment may be symptomatic, intravenously administered immunoglobulins or plasmapheresis. If in rare cases MFS progresses to a mixed form with GBS, thus a form also with affliction of the respiratory muscles, it is designated as GBS with ophthalmoplegia (2). Ophthalmoplegia may be both total (extraocular muscles and simultaneously intraocular muscles), or extraocular muscles only. Ptosis is present in approximately only one third of cases. Similarly as in other forms of GBS, MFS is preceded by approximately two weeks mostly by respiratory or less commonly gastrointestinal infection, most often with serological occurrence of Campylobacter jejuni. Lesions also of other cranial nerves may be present, most commonly the facial nerve and the caudal bulbar nerves.
CASE REPORT
The described patient was a woman aged 71 years, being treated for hypertension (bisoprolol), hyperlipidemia (rosuvastatin) and gastroesophageal reflux (pantoprazol), under general anamnesis. Six years before this pathology she had suffered from herpes zoster in the neck and shoulder region.
Two weeks before the acute onset of the complaints in May 2015 she had suffered an illness accompanied by a cough, purulent inflammation of the conjunctivas and headache, which was considered to be sinusitis, but did not respond to the administered antibiotics (amoxicillin with conjugated linoleic acid). Headaches, strongest in the occipital lobe, did not subside, vertigo progressively appeared, with vomiting and blurred vision, and impaired ability of articulation. At an initial examination in June 2015, bilateral acute angle-closure glaucoma was diagnosed, together with total ophthalmoplegia, areflexia and ataxia. Also described in the neurological finding were bulbar syndrome, upper meningeal syndrome and neocerebellar and paleocerebellar syndrome. Predominant in the ocular finding was bilateral deterioration of vision to fingers in front of the eye, certa, with edema of both corneas and medium areactive mydriasis of both pupils. Initial intraocular pressure was immeasurably high (measurement by Tono-pen Avia). After intravenous one-off administration of 100 ml 20% Mannitol, intraocular pressure in the right eye was 54 mmHg and in the left eye 56 mmHg. Local treatment with pilocarpine, timolol, dorsolamide and dexamethasone improved intraocular pressure to the level of physiological values within the course of a few hours. Prophylactic peripheral Nd-YAG laser iridotomy (LI) was performed on both eyes two days later.
Systemic therapy covered 5 times performance of plasmapheresis, re-treatment with antibiotics, symptomatic treatment and a rehabilitation programme. Examination of spinal fluid demonstrated positivity of the antibodies GQ1b (Ig G) and GT 1a (IgG). CT angio, concordant with later performed MRI, demonstrated sinusitis on the right side, in addition MRI also showed multiple deposits of gliosis in supratentorial white matter bilaterally, attributed to vascular etiology.
Subsequent cataract surgery (in October 2015 in right eye and March 2016 in left eye, with implantation of a posterior chamber intraocular lens, improved best corrected visual acuity in the right eye from 0.5 to 1.0 and in the left eye from 0.5 to 0.8 (Fig. 1 – pseudophakia natively and in artificial mydriasis). Intraocular pressure is physiological without the need for treatment. General and local therapy led to normalisation of the neurological finding and adjustment of the ocular finding (Fig. 2 – physiological motility of eyes). The observation period is three years.
1. Pseudophakia – natively (A, B) and in artificial mydriasis (C, D) 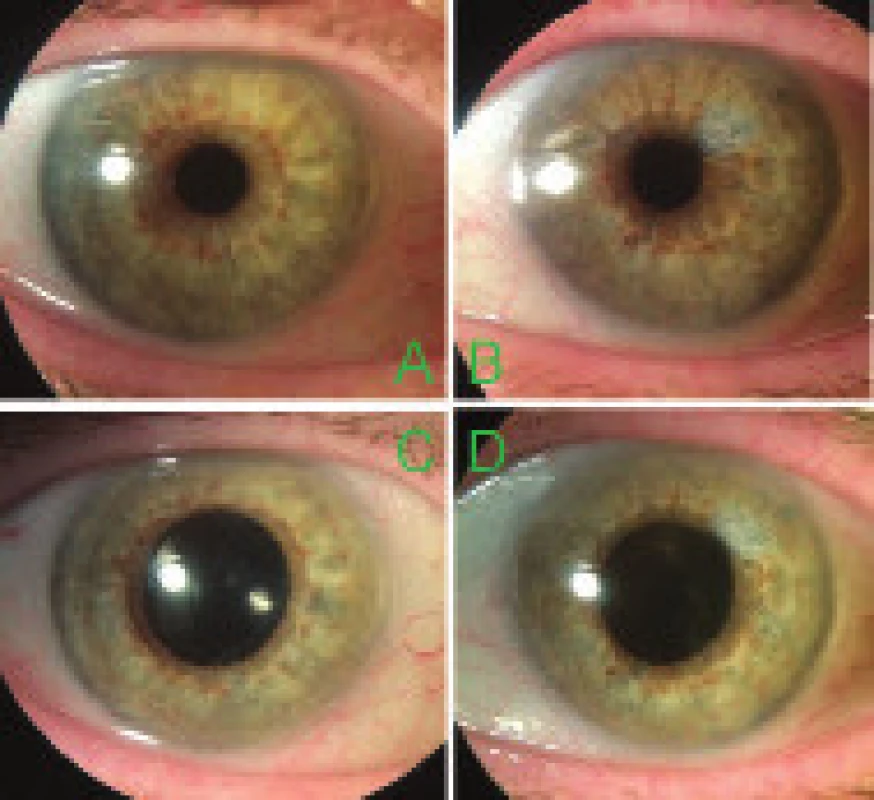
2. Adjustment of ophthalmoplegia 
METHOD
The finding on the patient was monitored continuously by means of a regular clinical examination making use of examination on a slit lamp (Nidek SL-250, Japan), biomicroscopic examination (non-contact VOLK Super Field NC lens, VOLK Optical, Ohio, USA), measurement of intraocular pressure by contact method (Tono-pen Avia), examination by indirect ophthalmoscopy (Sigma 150, Heine Optotechnik, Germany) with + 28 D lens (Ocular Instruments, Washington, USA) and photographically (retina camera Kowa VX-10α, Japan), biometric data Tomey (Tomey Corporation OA-2000 IOL cal. OPT).
In the PubMed database we used the key words Miller Fisher syndrome and glaucoma to search for references to studies on the issue in question published in journals indexed in MEDLINE.
Using the same method, in the PubMed database we used the key words acute angle-closure glaucoma and bilateral to search for references to studies describing simultaneous bilateral occurrence of acute angle-closure glaucoma.
DISCUSSION
The appearance of acute angle-closure glaucoma in MFS requires not only the occurrence of total ophthalmoplegia with bilateral mydriasis, but also predisposition of the patient in the form of age and hypermetropia. In the literature we found only four references describing acute angle-closure glaucoma in combination with MFS. Only Baxter et al. (11) in 2010 described acute angle-closure glaucoma as a bilateral ocular affliction in a 55-year-old man. Other authors described acute angle-closure glaucoma in MFS as unilateral – Brittain and Lake in 2005 in the left eye of a 64-year-old man, Ryu et al. in 2015 in the right eye of a 75-year-old man, and Han et al. in 2017 in the left eye of a 78-year-old woman (18, 120, 51). Our 71-year-old patient was also within the band of hypermetropia, axial length of the right eye was 22.38 mm, left eye 22.26 mm. According to our information, this case report is to date the second described case of a patient with simultaneous bilateral acute angle-closure glaucoma upon a background of MFS and to date the fifth described case with acute angle-closure glaucoma in this syndrome whatsoever.
Because ophthalmoplegia is an easily detected and determining symptom in MFS, from the perspective of MFS as such we could conclude the discussion here.
However, a surprisingly important factor is the issue of the very bilateral nature of acute angle-closure glaucoma, because this significantly influences both the diagnosis and the actual treatment.
If we encounter simultaneous bilateral acute angle-closure glaucoma, according to the published information there is a significant probability that this will not concern a case of primary acute angle-closure glaucoma, thus glaucoma incorporating pupillary block, as in the case in MFS, and therefore with a prompt response to the usual systemic and local anti-glaucomatous therapy covering intravenous mannitol (or peroral glycerol) and local pilocarpine, but secondary angle-closure glaucoma caused by a different mechanism, in which the usual treatment of primary angle-closure glaucoma is proving not only to be ineffective, but in many cases even worsens the condition.
In the case of this mechanism, it is possible to find swelling of the ciliary body, change of position of the lens-iris diaphragm, anterior rotation of the tips of the ciliary body, acute myopisation of the eyes, peripheral bulging of the iris and shallowing of the anterior chamber. Uveal effusion detectable by ultrasound biomicroscopy (UBM) has been described here, sometimes with signs of uveal irritation. Breach of the blood-brain barrier has also been described here (Viet Tran) (141). This finding may appear both in a systemically proceeding pathology, and also – far more frequently from the perspective of the literature – as pharmacologically iatrogenically induced. It is assumed that LI is not effective because pupillary block does not take place as such. Causal treatment is to influence the triggering causes, thus in the case of secondary effect of administered pharmaceutical its discontinuation, supporting therapy is to induce cycloplegia and local steroid treatment. With regard to the fact that pharmacologically induced bilateral acute angle-closure glaucoma has been described also in children in the case of topiramate (87, 24, 113), it is necessary to emphasise that in this mechanism, inducing cycloplegia does not directly influence myopisation (54). In terms of anterior rotation of the tips of the ciliary body and the effectiveness of local therapy with cycloplegic drugs and steroids, this mechanism is consistent with malignant glaucoma.
It is therefore necessary to divide pharmacological induction of bilateral acute angle-closure glaucoma into induction of primary acute angle-closure glaucoma (with pupillary block), thus after the administration of a pharmaceutical with a parasympatholytic or sympathomimetic effect and subsequent widening of the pupil in a predisposed individual (hypermetropia, age, prone head position), and induction of secondary acute angle-closure glaucoma following the administration of a pharmaceutical with an idiosyncratic effect, in which neither age nor original refraction of the eye play an important role.
Pharmacologically boosted or directly induced bilateral primary acute angle-closure glaucoma may occur in predisposed individuals (hypermetropia, age), most often in connection with general anaesthesia (e.g. Ates, Gayat) (7, 43), sometimes reinforced by the prone position of the head during spinal surgery (e.g. Singer) (125). It has also been described after blepharoplasty (e.g. Haverals) (53). It has further been described after local use of nasal drops (Fenox) containing phenylephrine and naphazoline (Khan) (68), or upon excessive use of cold remedies, the chief active substance of which was deadly nightshade (atropa belladonna) (Rudkin) (118), upon use of the anticholinergic drug oxybutynin (spasmolytic agent) in a predisposed individual (Haddad) (49), or ipratropium bromide either alone or in combination with salbutamol (Kola, Hall) (70, 50).
Simultaneous bilateral primary acute angle-closure glaucoma is not described often, furthermore the first authors to describe it are usually not ophthalmologists.
Pharmacologically induced secondary acute angle-closure glaucoma following the administration of a pharmaceutical and its idiosyncratic effect has been most widely described to date in the case of topiramate. This drug is used for the treatment of epilepsy (third generation anti-epileptic drug), migraine and off label as an anorectic drug. It is a sulfamate derivative of fructose, chemically classified as 2.3 : 4.5-bis-O-(1-methylethylidene)-ß-D-fructopyranose sulfamate. Bilateral acute angle-closure glaucoma in the case of topiramate was first described by Banta et al. in 2001 (10). We found more than forty studies (2001 – Banta, Rhee (10, 116), 2002 – Nemet (103), 2003 – Lin, Coats (87, 24), 2004 – Craig, Fraunfelder (26, 42), 2005 – Mansoor (92), 2006 – Viet Tran, Levy, Desai (141, 84, 34), 2007 – Stangler, Izambart, Guier, Parikh, Singh (131, 59, 48, 106, 126), 2008 – Aminlari, Chalam, Zalta, Boonyaleephan (5, 20, 150, 15), 2009 – Sbeity, Cruciani (121, 30), 2010 – Tahiri Joutei Hassani, Natesh, Acharya, Senthil (132, 102, 1, 122), 2011 – van Issum, Paciuc-Beja, Willet, Tanaka (139, 105, 145, 134), 2012 – Cole, Caglar, Muniesa Royo, Rodriguez-Blanco (25, 19, 100, 117), 2013 – Quagliato, Kulkarni (112, 74), 2014 – Czyz, Kamal, Reis, Rapoport, Pikkel, Katsimpris, Mitra (31, 63, 115, 113, 110, 64, 97), 2015 – Grewal, Dhar (45, 35), 2016 – Behl, Beaudry (14, 12), 2017 – Joshi, Lan, Meijer (61, 78, 95)), including cases of described incidence in children (Lin, Coats, Rapoport) (87, 24, 113).
Another large group of pharmaceuticals, also of compounds containing sulphur, in which an idiosyncratic effect of administration of the drug and induction of bilateral secondary acute angle-closure glaucoma by this mechanism has been described, is the group of sulphonamides.
Sulphonamides constitute a broad group of pharmaceuticals, including not only drugs with an antimicrobial effect, but also antidiabetic drugs on the basis of sulphonylurea, diuretics, anti-convulsive drugs, antiviral drugs and other substances, such as the anti-glaucomatous agents used in ophthalmology brinzolamide and dorsolamide. Tamsulosin, which increases the difficulty of cataract surgery by inducing a condition designated as IFIS (intraoperative floppy iris syndrome), is also a sulphonamide derivative.
Secondary acute angle-closure glaucoma has been most frequently described in the case of sulphonamides with a diuretic effect, in the case of acetazolamide (Grigera, Mancino, Malagola, Lee GC, Parthasarathi, Senthil) (46, 91, 90, 79, 107, 122), furosemide (Bondaoui) (15), hydrochlorothiazide (Chen, Geanon, Lee GC) (22, 44, 79), methazolamide (Aref, Kwon) (6, 77), indapamide (Senthil) (122) and chlorthalidone (Durai, Singer) (36, 124). In the case of sulphonamides with an anti-inflammatory effect, it has been described in connection with sulfasalazine in combination with trimethoprim (Lee GC) (79), in sulphonamides with an antimicrobial effect in the case of sulfamethoxazole (Spadoni, Waheeb) (128, 143), in sulphonamides with an anti-convulsive effect in the case of zonisamide (Weiler) (144), and also in the anti-migraine drug sumatriptan (Hsu) (55).
In the case of drugs used as antidepressants, secondary acute angle-closure glaucoma has been described in connection with venlafaxin (serotonin and norardrenaline reuptake inhibitor, SNRI) (de Guzman, Ezra, Ng) (32, 38, 104), duloxetine (SNRI) (Shifera, Mahmut) (123, 89), trazodone (serotonin reuptake inhibitor, SRI) (Hrčková) (54), citalopram and escitalopram (selective serotonin reuptake inhibitor, SSRI) (Croos, Massaoutis, Zelefsky (28, 93, 152), paroxetine (SRI) (Kirwan, Levy) (69, 85) and bupropion (aminoketone) (Takusagawa) (133). Acute angle-closure glaucoma has also been described in the case of tramadol (SNRI), which is used as a painkilling drug (Mahmoud) (88).
Secondary acute angle-closure glaucoma has been described in the case of two different serotonin agonists, namely the anti-migraine drug zolmitriptan (Lee JTL) (80) and the anorectic drug dexfenfluramine (Denis) (33).
We present other substances linked with secondary bilateral acute angle-closure glaucoma only in alphabetical order: cabergoline (lactation suppressor) (Razmjoo) (114), cyclosporine (Braun) (17), ecstasy (3.4-methylenedioxymethamphetamine (MDMA)) (Kumar, Trittibach) (76, 137), the plant ephedra (Ma-huang) (natural source of ephedrine) in a natural compound for slimming (Ryu) (119), ephedrine and phendimetrazine (anorectic drug) (Lee W) (82), flavoxate (spasmolytic agent for urinary tract) used on a patient already using indapamide (Mohammed) (98), flucloxacillin and carbamazepine (Chan) (21), isoretinoin (acne treatment) (Park) (108), mefenamic acid (Vishwakarma) (142), olsetamivir (Tamiflu), neuraminidase inhibitor (Lee JW, Yazdani) (81, 149), methylsulfonylmethane (MSM), used as a food supplement and source of biologically bound sulphur (Hwang) (57) and a poisonous bite from a further unspecified Indian snake (Srinivasan) (130).
Bilateral secondary angle-closure glaucoma in connection with change of position of the ciliary body due to its swelling has been described also in the case of systemic tumours, inflammatory and infectious diseases.
In the case of systemic tumorous pathologies, it has been described in connection with Hodgkin’s lymphoma (Belz, Baillif) (13, 9), lymphoma (Cristol) (27), myelofibrosis (Lin) (86) and myelodysplastic syndrome (Smith) (129).
In the case of systemic inflammatory pathologies it has been described in connection with leukocytoclastic vasculitis (Guerriero) (47), systemic lupus erythematodes (Han) (52), large cell arteritis (Hunter) (56), Wegener’s granulomatosis (Mete) (96) and several times in the case of Vogt-Koyanagi-Harada syndrome (Eibschitz-Tsimhoni, Forster, Yang, Yao) (37, 41, 147, 148).
In the case of systemic infectious pathologies it has been described in connection with acute retinal necrosis (Kaushik) (66), infection by Campylobacter iejuni (Mukherji) (99) herpes zoster (al Halel) (4), HIV infection and AIDS (Fineman, Joshi, Koster, Krzystolik, Meige, Nash, Ullman, Zambarakji) (39, 62, 71, 72, 94, 101, 138, 151), in haemorrhagic fevers – Dengue fever (Joob, Levaggi, Pierre Filho Pde) (60, 83, 109), Korean haemorrhagic fever and haemorrhagic fevers caused by hantavirus (Cho, Zimmermann) (23, 153). We do not have any explanation for the fact that in the case of HIV – AIDS infection all the studies came within a relatively short time interval, from 1986 (Ullman) (138) to 1997 (Fineman) (39).
To complete the list it is necessary to add that secondary bilateral angle-closure glaucoma has also been described in the case of congenital developmental defects, repeatedly in the case of bilateral and multiple occurrence of ciliary cysts (Azuara-Blanco, Tanihara, Kuchenbecker, Viestenz, Badlani, Crowston, Katsimpris) (3, 135, 73, 140, 8, 29, 65)) and sporadically in other congenital defects – Alagille syndrome (Potamitis) (111), spherophakia and Weill-Marchesani syndrome (Kaushik, Wright) (67, 146). It has also been described in iridoschisis (Iaccarino, Torricelli) (58, 136). It has also once been described in the case of phacomorphic glaucoma in the first identification of type 1 diabetes mellitus (Skrabic) (127) and as the first symptom of primary pulmonary hypertension (Kunjukunju) (75).
CONCLUSION
The Miller Fisher syndrome is a post-infection, self-limiting, immunity mediated pathology from the group of Guillain-Barré syndrome, which has a good prognosis. If total ophthalmoplegia in a patient of risk age with hypermetropia appears upon the background of Miller Fisher syndrome, this may lead to primary acute angle-closure glaucoma, either unilateral or bilateral. With regard to pupillary block, ocular treatment is standard.
If an ophthalmologist encounters simultaneous bilateral acute angle-closure glaucoma, it is necessary to evaluate the patient’s overall condition of health, the pharmaceuticals used, and in differential diagnostics not to overlook secondary acute angle-closure glaucoma.
Presented at the 26th annual congress of the Czech Ophthalmology Association, Czech Medical Association of J. E. Purkyně in Prague, 13-15 September 2018
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Supported by a project (Ministry of Health) for conceptual development of research organisation 00064203 (Motol University Hospital) and CZ.2.16/3.1.00/24022
Received: 6. 5. 2019
Accepted: 26. 7. 2019
Available on-line: 6.1.2020
MUDr. Jana Štěpánková
Oční klinika dětí a dospělých FNM
V Úvalu 84,
150 08 Praha 5 - Motol
Sources
1. Acharya, N., Nithyanandam, S., Kamat S.: Topiramate-associated bilateral anterior uveitis and angle clossure glaucoma. Indian J Ophthalmol, 58(6); 2010 : 557-559.
2. Ambler, Z., Valeš, J.: Miller Fisher Syndrome – Four Case Reports and Review of Current Concept. Cesk Slov Neurol N, 74/107(6); 2011 : 689-694.
3. Azuara-Blanco, A., Spaeth, GL., Araujo, SV. et al.: Plateau iris syndrome associated with multiple ciciary body cysts. Report of three cases. Arch Ophthalmol, 114(6); 1996 : 666-668.
4. al Halel, A., Hirsh, A., Melamed, S. et al.: Bilateral simultaneous spontaneous acute angle closure glaucoma in a herpes zoster patient. Br J Ophthalmol, 75(8); 1991 : 510.
5. Aminlari, A., East, M., Wei, W. et al.: Topiramate induced acute angle closure glaucoma. Open Ophthalmol J., 2; 2008 : 46-47.
6. Aref, AA., Sayyad, FE., Ayres, B. et al.: Acute bilateral angle closure glaucoma induced by methazolamide. Clin Ophthalmol,7; 2013 : 279-282.
7. Ates, H., Kayikçioğlu, O., Andaç, K.: Bilateral angle closure glaucoma following general anesthesia. Int Ophthalmol, 23(3), 1999 : 129-130.
8. Badlani, VK., Quinones, R., Wilensky, JT. et al: Angle-closure glaucoma in teenagers. J Glaucoma, 12(3), 2003 : 198-203.
9. Baillif, S., Cornut, PL., Girard, C. et al.: Bilateral angle-closure glaucoma and multifocal choroiditis as a first presentation in Hodgkin lymphoma. Retin Cases Brief Rep, 5(3); 2011 : 201-205.
10. Banta, JT., Hoffman, K., Budenz, DL. et al: Presumed topiramate-induced bilateral acute angle-closure glaucoma. Am J Ophthalmol, 132(1); 2001 : 112-114.
11. Baxter, JM., Alexander, P., Maharajan, VS.: Bilateral, acute angle-closure glaucoma associated with Guillain-Barre syndrome variant. BMJ Case rep, 2010 Jul 21; 2010.
12. Beaudry, Goncette, V., Collignon, N.: [Bilateral angle-closure glaucoma induced by topiramate]. Rev Med Liege, 71 (11), 2016 : 509. French.
13. Belz, Thalabard, Bretagnolles: [Hodgkin‘s disease and acute bilateral glaucoma]. Bull Soc Ophtalmol, Fr., 3; 1954 : 244-246.
14. Behl, A., Fasahtay, A.: Topiramate-induced bilateral angle closure glaucoma and myopic shift. Neurol India, 64(5); 2016 : 1040-1042.
15. Boonyaleephan, S.: Bilateral acute onset myopia and angle closure glaucoma after oral topiramate: a case report. J Med Assoc Thai, 91(12); 2008 : 1904-1907.
16. Boundaoui, ON., Woodruff, TE.: Presumed Furosemide-associated Bilateral Angle-Closure Glaucoma. J Glaucoma, 25(8); 2016 : 748-50.
17. Braun, R., Holler, E., Wolff, D. et al.: [Bilateral ciliary body oedema under treatment with ciclosporine.] Ophthalmologe, 115(1); 2018 : 55-58. German.
18. Brittain, CJ., Lake, D.: Acute angle closure glaucoma in Miller Fisher syndrome. Eye (Lond), 20(6); 2006 : 739-40.
19. Caglar, C., Yasar, T., Ceyhan, D.: Topiramate induced bilateral angle-closure glaucoma: low dosage in a short time. J Ocul Pharmacol Ther, 28(2); 2012 : 205-207.
20. Chalam, KV., Tillis, T., Syed, F. et al.: Acute bilateral simultaneous angle closure glaucoma after topiramate administration: a case report. J Med Case Rep, 2; 2008 : 1.
21. Chan, KC., Sachdev, N., Wells, AP.: Bilateral acute angle closure secondary to uveal effusions associated with flucloxacillin and carbamazepine. Br J Ophthalmol, 92(3); 2008 : 428-430.
22. Chen, SH., Karanjia, R., Chevrier, RL. et al.: Bilateral acute angle closure glaucoma associated with hydrochlorothiazide-induced hyponatraemia. BMJ Case Rep, 2014.
23. Cho, IH., Chang, JH., Choo, EJ.: Bilateral simultaneous angle-closure glaucoma associated with septic condition of Korean hemorrhagic fever (KHF). J Glaucoma, 24(1); 2015 : 81-3.
24. Coats, DK.: Bilateral angle closure glaucoma in a child receiving oral topiramate. J AAPOS, 7(4); 2003, 303.
25. Cole, KL., Wang, EE., Aronwald, RM.: Bilateral acute angle--closure glaucoma in a migraine patient receiving topiramate: a case report. J Emerg Med, 43(2); 2012: e89-91.
26. Craig, JE., Ong, TJ., Louis, DL. et al.: Mechanism of topiramate-induced acute-onset myopia and angle closure glaucoma. Am J Ophthalmol, 137(1); 2004 : 193-195.
27. Cristol, SM., Baumblatt, JG., Icasiano, E. et al.: Bilateral acute angle-closure associated with systemic lymphoma: a report of 2 cases. J Glaucoma, 20(2); 2011 : 115-117.
28. Croos, R., Thirumalai, S., Hassan, S. et al.: Citalopram associated with acute angle-closure glaucoma: case report. BMC Ophthalmol, 5; 2005 : 23.
29. Crowston, JG., Medeiros, FA., Mosaed, S. et al.: Argon laser iridoplasty in the treatment of plateau-like iris configuration as result of numerous ciliary body cysts. Am J Ophthalmol, 139(2); 2005 : 381-383.
30. Cruciani, F., Lorenzatti, M., Nazzarro, V. et al.: Bilateral acute angle closure glaucoma and myopia induced by topiramate. Clin Ter, 160 (3); 2009 : 215-216.
31. Czyz, CN., Clark, CM., Justice, JD. et al.: Delayed topiramate-induced bilateral angle - closure glaucoma. J Glaucoma, 23(8); 2014 : 577-578.
32. de Guzman, MH., Thiagalingam, S., Ong, PY. et al.: Bilateral acute angle closure caused by supraciliary effusions associated with venlafaxine. Med J Aust, 182(3) 2005 : 121-123.
33. Denis, P., Charpentier, D., Berros, P. et al.: Bilateral acute angle-closure glaucoma after dexfenfluramine treatment. Ophthalmologica, 209(4); 1995 : 223-224.
34. Desai, CM., Ramchandani, SJ., Bhopale, SG. et al.: Acute myopia and angle closure caused by topiramate, a drug used for prophylaxis of migraine. Indian J Ophthalmol, 54(3); 2006 : 195-197.
35. Dhar, SK., Sharma, V., Kapoor, G. et al.: Topiramate induced bilateral anterior uveitis with choroidal detachment and angle closure glaucoma. Med J Armed Forces India, 71(1); 2015 : 88-91.
36. Durai, I., Mohan Dhavalikar, M., Anand, CP. et al.: Bilateral, Simultaneous, Acute Angle Closure Glaucoma in Pseudophakia Induced by Chlorthalidone. Case Rep Ophthalmol Med, 2016.
37. Eibschitz-Tsimhoni, M., Gelfand, YA., Mezer, E. et al.: Bilateral angle closure glaucoma: an unusual presentation of Vogt-Koyanagi-Harada syndrome. Br J Ophthalmol, 81(8); 1997 : 705-706.
38. Ezra, DG., Storoni, M., Whitefield, LA.: Simultaneous bilateral acute angle closure glaucoma following venlafaxine treatment. Eye (Lond), 20(1); 2006 : 128-129.
39. Fineman, MS., Emerick, G., Dudley, D. et al.: Bilateral choroidal effusions and angle-closure glaucoma associated with human immunodeficiency virus infection. Retina, 17(5), 1997 : 455-457.
40. Fisher, M.: An unusual variant of acute idiopathic polyneuritis (syndrome of ophthalmoplegia, ataxia and areflexia), N Engl J Med, 255(2); 1956 : 57-65.
41. Foster, DJ., Rao, NA., Hill, RA. et al.: Incidence at management of glaucoma in Vogt-Koyanagi-Harada syndrome. Ophthalmology, 100(5); 1993 : 613-618.
42. Fraunfelder, FW., Fraunfelder, FT., Keates, EU.: Topiramate-associated acute, bilateral, secondary angle-closure glaucoma. Ophthalmology, 111(1); 2004 : 109-111.
43. Gayat, E., Gabison, E., Devys, JMN.: Case report: bilateral angle closure glaucoma after general anesthesia. Anesth Analg, 112(1); 2011 : 11-12.
44. Geanon, JD., Perkins, TW.: Bilateral acute angle-closure glaucoma associated with drug sensitivity to hydrochlorothiazide. Arch Ophthalmol, 113(10); 1995 : 1231-1232.
45. Grewal, DS., Goldstein, DA., Khatana, AK. et al.: Bilateral angle closure following use of a weight loss combination agent containing topiramate. J Glaucoma, 24(5); 2015: e132-6.
46. Grigera, JD., Grigera, ED.: Ultrasound biomicroscopy in acetazolamide induced myopic shift with appositional angle clossure. Arq Bras Oftalmol, 80(5); 2017 : 327-329.
47. Guerriero, S., Dammacco, R., Cimmino, A. et al.: Bilateral acute angle-closure glaucoma as the presenting feature of a systemic leukocytoclastic vasculitis. Clin Exp Ophthalmol, 39(8); 2011 : 837-839.
48. Guier, CP.: Elevated intraocular pressure and myopic shift linked to topiramate use. Optom Vis Sci, 84(12); 2007 : 1070-1073.
49. Haddad, A., Arwani, M., Sabbagh, O.: A Novel Association between Oxybutynin Use and Bilateral Acute Angle Closure Glaucoma: A Case Report and Literature Review. Cureus, 10(6); 2018: e2732.
50. Hall, SK.: Acute angle-closure glaucoma as a complication of combined beta-agonist and ipratropium bromide therapy in the emergency department. Ann Emerg Med, 23(4); 1994 : 884-887.
51. Han, J., Ji, Y., Cao, D. et al.: Miller Fisheer syndrome with acute angle closure glaucoma as the first manifestation: A case report Medicine (Baltimore), 96(50); 2017: e9201.
52. Han, YS., min Yang, C., Lee, SH. et al.: Secondary angle closure glaucoma by lupus choroidopathy as an initial presentation of systemic lupus erythematosus: a case report. BMC Ophthalmol, 15; 2015; 148.
53. Haverals, K., Augustinus, A., Hodeghem, K.: Bilateral acute angle-closure glaucoma after blefaroplasty. Bull Soc Belge ophthalmol, 316; 2010 : 59-61.
54. Hrčková, L., Mojžiš, P., Žiak, P.: Acute myopia with elevation of intraocular tension as an adverse side effect of antidepresant medication. Cesk Slov Oftalmol, 74(2); 2018 : 68-72.
55. Hsu, CR., Chen, YH., Tai, MC. et al.: Sumatriptan-induced angle-closure glaucoma: A case report. Medicine (Baltimore), 96(22); 2017: e6953.
56. Hunter, TG., Chong, GT., Asrani, S. et al.: Simultaneous bilateral angle closure glaucoma in a patient with giant cell arteritis. J Glaucoma, 19(2); 2010 : 149-50.
57. Hwang, JC., Khine, KT., Lee, JC. et al.: Methyl-sulfonyl-methane (MSM)-induced acute angle closure. J Glaucoma, 24(4); 2015: e28-30.
58. Iaccarino, G., Forte, R., Cennamo, G.: [Iridoschisis and angle-closure glaucoma: a case report]. J Fr Ophtalmol, 29(9); 2006: e26. French.
59. Izambart, C., Rocher, F., Zur, C. et al.: [Topiramate and acute myopia with angle-closure glaucoma: case report and literature review]. J Fr Ophtalmol, 30(5); 2007: e11. French.
60. Joob, B., Wiwanitkit, V.: Bilateral acute angle closure in a patient with dengue. Arq Bras Oftalmol, 81(1); 2018 : 80.
61. Joshi, AK., Pathak, AH., Patwardhan, SD. et al.: A Rare Case of Topiramate Induced Secondary Acute Angle Closure Glaucoma. J Clin Diagn Res, 11(6); 2017: ND01-ND03
62. Joshi, N., Constable, PH., Margolis, TP. et al.: Bilateral angle closure glaucoma and accelerated cataract formation in a patient with AIDS. Br J Ophthalmol, 78(8); 1994 : 656-657.
63. Kamal, S., Yadava, U., Kumar, S. et al.: Topiramate-induced angle-closure glaucoma: cross-sensitivity with other sulphonamide derivatives causing anterior uveitis. Int Ophthalmol, 34(2); 2014 : 345-349.
64. Katsimpris, JM., Katsimpris, A., Theoulakis, PE. et al.: Bilateral severe anterior uveitis and acute angle-closure glaucoma following topiramate use for migraine crisis. Klin Monbl Augenheilkd. 231(4); 2014 : 439-441.
65. Katsimpris, JM., Petropoulos, IK., Sunaric-Mégevand, G.: Ultrasound biomicroscopy evaluation of angle closure in patient with multiple and bilateral iridociliary cysts. Klin Monbl Augenheilkd, 224(4); 2007 : 324-327.
66. Kaushik, S., Lomi, N., Singh, MP. et al.: Acute retinal necrosis presenting as bilateral acute angle closure. Lancet, 384; 2014 : 636.
67. Kaushik, S., Sachdev, N., Pandav, SS. et al.: Bilateral acute angle closure glaucoma as a presentation of isolated microspherophakia in an adult: case report. BMC Ophthalmol, 6; 2006 : 29.
68. Khan, MA., Watt, LL., Hugkulstone, CE.: Bilateral acute angle-closure glaucoma after use of Fenox nasal drops. Eye (Lond), 16(5); 2002 : 662-663.
69. Kirwan, JF., Subak-Sharpe, I., Teimory, M.: Bilateral acute angle closure glaucoma after administration of paroxetine. Br J Ophthalmol, 81(3); 1997 : 252.
70. Kola, M., Hacıoğlu, D., Erdöl, H. et al.: Bilateral acute angle closure developing due to use of ipratropium bromide and salbutamol. Int Ophthalmol, 38(1); 2018 : 385-388.
71. Koster, HR., Liebmann, JM., Ritch, R. et al.: Acute angle-closure glaucoma in a patient with acquired immunodeficiency syndrome successfully treated with argon laser peripheral iridoplasty. Ophthalmic Surg, 21(7); 1990; 501-502.
72. Krzystolik, MG., Kuperwasser, M., Low, RM. et al.: Anterior-segment ultrasound biomicroscopy in a patient with AIDS and bilateral angle-closure glaucoma secondary to uveal effusions. Arch Ophtalmol, 114(7), 1996 : 878-879.
73. Kuchenbecker, J., Motschmann, M., Schmitz, K. et al.: Laser iridocystotomy for bilateral acute angle-closure glaucoma secondary to iris cysts. Am J Ophthalmol, 129(3); 2000 : 391-393.
74. Kulkarni, C., Chaudhuri, UR., Jagathesan, A.: Bilateral acute angle-closure glaucoma following treatment with topiramate for headache. Neurol Ther, 2(1-2); 2013 : 57-62.
75. Kunjukunju, N., Gonzales, CR., Rodden, WS.: Exudative retinal detachement and angle closure glaucoma as the presenting sign of primary pulmonary hypertension. Retin Cases Brief Rep, 5(2); 2011 : 108-112.
76. Kumar, RS., Grigg, J., Farinelli, AC.: Ecstasy induced acute bilateral angle closure and transient myopia. Br J Ophthalmol, 91(5); 2007 : 693-695.
77. Kwon, SJ., Park, DH., Shin, JP.: Bilateral transient myopia, angle-closure glaucoma, and choroidal detachment induced by methazolamide. Jpn J Ophthalmol, 56(5); 2012 : 515-517.
78. Lan, YW., Hsieh, JW.: Bilateral acute angle closure glaucoma and myopic shift by topiramate-induced ciliochoroidal effusion: case report and literature review. Int Ophthalmol, 38(6); 2018 : 2639-2648.
79. Lee, GC., Tam, CP., Danesh-Mexyer, HV. et al.: Bilateral angle closure glaucoma induced by sulfonamide derived medcations. Clin Exp. Ophthalmol, 35(1), 2007 : 55-58.
80. Lee, JTL., Skalicky, SE., Lin, ML.: Drug-induced Myopia and Bilateral Angle Closure Secondary to Zolmitriptan. J Glaucoma, 26(10); 2017 : 954-956.
81. Lee, JW., Lee, JE., Choi, HY.: Oseltamivir (Tamiflu)-induced bilateral acute angle closure glaucoma and transient myopia. Indian J Ophthalmol. 62(12); 2014 : 1165-1167.
82. Lee, W., Chang, JH., Roh, KH. et al.: Anorexiant-induced transient myopia after myopic laser in situ keratomileusis. J Cataract Refract Surg,33(4); 2007 : 746-749.
83. Levaggi, ND., Lucas, AN., Barletta, JAE.: Bilateral acute angle closure in a patient with dengue fever: a case report. Arq Bras Oftalmol, 80(4);2017 : 266-267.
84. Levy, J., Yagev, R., Petrova, A. et al.: Topiramate-induced bilateral angle-closure glaucoma. Can J Ophthalmol. 41(2); 2006 : 221-225.
85. Levy, J., Tessler, Z., Klemperer, I. et al.: Late bilateral acute angle-closure glaucoma after administration of paroxetine in a patient with plateau iris configuration. Can J Ophthalmol, 39(7); 2004 : 780-1.
86. Lin, AL., Burnham, JM., Pang, V. et al.: Ocular manifestations of primary myelofibrosis. Retin Cases Brief Rep, 10(4); 2016 : 364-367.
87. Lin, J., Fosnot, J., Edmond, J.: Bilateral angle closure glaucoma in a child receiving oral topiramate. J AAPOS, 7(1); 2003 : 66-68.
88. Mahmoud, A., Abid, F., Ksiaa, I. et al: Bilateral acute angle-closure glaucoma following tramadol subcutaneous administration. BMC Ophthalmol,18(1); 2018 : 50.
89. Mahmut, A., Tunc, V., Demiryurek, E. et al.: Bilateral acute angle-closure glaucoma induced by duloxetine. Ideggyogy Sz, 70(9-10); 2017 : 358-360.
90. Malagola, R., Arrico, L., Giannotti, R. et al.: Acetazolamide-induced cilio-choroidal effusion after cataract surgery: unusual posterior involvement. Drug Des Devel Ther, 7; 2013 : 33 - 62.
91. Mancino, R., Varesi, C., Cerulli, A. et al.: Acute bilateral angle-closure glaucoma and choroidal effusion associated with acetazolamide administration after cataract surgery. J Cataract Refract Surg., 37(2); 2011 : 415-417.
92. Mansoor, Q., Jain, S.: Bilateral angle-closure glaucoma following oral topiramate therapy. Acta Ophthalmol Scand, 83(5); 2005 : 627-628.
93. Masaoutis, P., Goh, D., Foster, PJ.: Bilateral symptomatic angle closure associated with a regular dose of citalopram, an SSRI antidepressant. Br J Ophthalmol, 91(8) 2007 : 1086-1087.
94. Meige, P., Cohen, H., Morin, B. et al.: [Acute bilateral glaucoma in an LAV-positive subject]. Bull Soc Ophtalmol Fr, 89(3); 1989 : 449-454.
95. Meijer, N., Nguyen, HT., Wolff, R.: [A woman with acute bilateral vision loss]. Ned Tijdschr Geneeskd, 161; 2017: D1255. Dutch.
96. Mete, A., Kimyon, S., Saygili, O. et al.: Bilateral acute angle-closure glaucoma as a first presentation of granulomatosis with polyangiitis (Wegener‘s). Arq Bras Oftalmol,79(5); 2016 : 336-338.
97. Mitra, A., Ramakrishnan, R., Kader, MA.: Anterior segment optical koherence tomography documentation of a case of topiramate induced acute angle closure. Indian J Ophthalmol. 62(5); 2014 : 619-622.
98. Mohammed, ZS., Simi, ZU., Tariq, SM. et al.: Bilateral acute angle closure glaucoma in a 50 year old female after oral administration of flavoxate. Br J Clin Pharmacol, 66(5); 2008 : 726-727.
99. Mukherji, S., Ramanathan, S., Tarin, S.: Uveal effusion associated with Campylobacter jejuni infection presenting as bilateral angle closure glaucoma. J Glaucoma, 20(9); 2011 : 587-588.
100. Muniesa Royo, MJ., Traveset Maeso, A., Jurjo Campo, C.: [Topiramate-induced bilateral acute angle closure glaucoma and myopia]. Med Clin (Barc), 138(8); 2012 : 368-369.
101. Nash, RW., Lindquist, TD.: Bilateral angle-closure glaucoma associated with uveal effusion: presenting sign of HIV infection. Surv Ophthalmol, 36(4); 1992 : 255-258.
102. Natesh, S., Rajashekhara, SK., Rao, AS. et al.: Topiramate-induced angle closure with acute myopia, macular striae. Oman J Ophthalmol, 3(1); 2010 : 26-28.
103. Nemet, A., Nesher, R., Almog, Y. et al.: [Bilateral acute angle closure glaucoma following topiramate treatment]. Harefuah, 141(7); 2002 : 597-599, 667. Hebrew.
104. Ng, B., Sanbrook, GM., Malouf, AJ. et al.: Venlafaxine and bilateral acute angle closure glaucoma. Med J Aust, 176(5); 2002 : 241.
105. Paciuc-Beja, M., Retchkiman-Bret, M., Velasco-Barona, CF. et al.: Secondary Bilateral Angle Closure Glaucoma due to Topiramate. Case Rep Ophthalmol Med, 2011
106. Parikh, R., Parikh, S., Das, S. et al.: Choroidal drainage in the management of acute angle closure after topiramate toxicity. J Glaucoma, 16(8); 2007 : 691-693.
107. Parthasarathi, S., Myint, K., Singh, G. et al.: Bilateral acetazolamide-induced choroidal effusion following cataract surgery. Eye (Lond), 21(6), 2007 : 870-872.
108. Park, YM., Lee, TE.: Isoretinoin induced angle closure and myopic shift. J Glaucoma, 26(11); 2017: e252-e254.
109. Pierre Filho Pde, T., Carvalho Filho, JP., Pierre, ET.: Bilateral acute angle closure glaucoma in a patient with dengue fever: case report. Arq Bras Oftalmol, 71(2); 2008 : 265-268.
110. Pikkel, YY.: Acute bilateral glaucoma and panuveitis as a side effect of topiramate for weight loss treatment. BMJ Case Rep., 2014.
111. Potamitis, T., Fielder, AR.: Angle closure glaucoma in Alagille syndrome. A case report. Ophthalmic Paediatr Genet, 14(2); 1993; 101-104.
112. Quagliato, LB., Barella, K., Abreu Neto, JM. et al.: Topiramate-associated acute, bilateral, angle-closure glaucoma: case report. Arq Bras Oftalmol, 76 (1); 2013 : 48-49.
113. Rapoport, Y., Benegas, N., Kuchtey, RW. et al.: Acute myopia and angle closure glaucoma from topiramate in a seven-year-old: a case report and review of the literature. BMC Pediatr, 2014.
114. Razmjoo, H., Rezaei, L., Dehghani, A. et al.: Bilateral angle-closure glaucoma in a young female receiving cabergoline: a case report. Case Rep Ophthalmol, 2(1); 2011 : 30-33.
115. Reis, GM., Lau, OC., Samarawickrama, C. et al.: Utility of ultrasound biomicroscopy in the diagnosis of topiramate-associated ciliochoroidal effusions causing bilateral acute angle closure. Clin Exp Ophthalmol, 42(5); 2014 : 500-501.
116. Rhee, DJ., Goldberg, MJ., Parrish, RK.: Bilateral angle-closure glaucoma and ciliary body swelling from topiramate. Arch Ophthalmol, 119(11); 2001 : 1721-1723.
117. Rodríguez-Blanco, M., Piñeiro, A., Bande, M. et al.: [Angle-closure glaucoma secondary to topiramate use]. Arch Soc Esp Oftalmol, 87(4); 2012 : 122-124.
118. Rudkin, AK., Gray, TL., Awadalla, M. et al.: Bilateral simultaneous acute angle closure glaucoma precipitated by non-prescription cold and flu medication. Emerg Med Australas, 22 (5); 2010 : 477-479.
119. Ryu, SJ., Shin, YU., Kang, MH. et al.: Bilateral acute myopia and angle closure glaucoma induced by Ma-huang (Ephedra): A case report. Medicine (Baltimore), 96(50); 2017: e9257.
120. Ryu, WY., Kim, JK., Jin, SW. et al.: Acute angle-clossure glacoma in a patient with Miller Fisher syndrome without pupillary dysfunction, J Glaucoma, 24 (2); 2015: e5-6.
121. Sbeity, Z., Gvozdyuk, N., Amde, W. et al.: Argon laser peripheral iridoplasty for topiramate-induced bilateral acute angle closure. J Glaucoma, 18(4); 2009 : 269-271.
122. Senthil, S., Garudadri, C., Rao, HB. et al.: Bilateral simultaneous acute angle closure caused by sulphonamide derivatives: a case series. Indian J Ophthalmol, 58(3); 2010 : 248-252.
123. Shifera, AS., Leoncavallo, A., Sherwood, M.: Probable Association of an Attack of Bilateral Acute Angle-Closure Glaucoma With Duloxetine. Ann Pharmacother, 48(7); 2014 : 936-939.
124. Singer, JR., Pearce, ZD., Westhouse, SJ. et al.: Uveal effusion as a mechanism of bilateral angle-closure glaucoma induced by chlorthalidone. J Glaucoma, 24(1); 2015 : 84-86.
125. Singer, MS., Salim, S.: Bilateral acute angle-closure glaucoma as a complication of facedown spine surgery. Spine, 10(9), 2010: e7-e9.
126. Singh, SK., Thapa, SS., Badhu, BP.: Topiramate induced bilateral angle-closure glaucoma. Kathmandu Univ Med J (KUMJ), 5(2); 2007 : 234-236.
127. Skrabic, V., Ivanisevic, M., Stanic, R. et al.: Acute bilateral cataract with phacomorphic glaucoma in a girl with newly diagnosed type 1 diabetes mellitus. J Pediatr Ophthalmol Strabismus, 47; 2010: e1-3.
128. Spadoni, VS., Pizzol, MM., Muniz, CH. et al.: [Bilateral angle-closure glaucoma induced by trimethoprim and sulfamethoxazole combination: case report]. Arq Bras Oftalmol, 70(3); 2007 : 517-520. Portuguese.
129. Smith, DL., Skuta, GL., Trobe, JD. et al.: Angle-closure glaucoma as initial presentation of myelodysplastic syndrome. Can J Ophthalmol, 25(6); 1990 : 306-308.
130. Srinivasan, R., Kaliaperumal, S., Dutta, TK.: Bilateral angle closure glaucoma following snake bite. J Assoc Physicians India, 532; 2005 : 46-48.
131. Stangler, F., Prietsch, RF., Fortes Filho, JB.: [Bilateral acute angle closure glaucoma in a young patient receiving oral topiramate: case report]. Arq Bras Oftalmol, 70(1); 2007 : 133-136. Portuguese.
132. Tahiri Joutei Hassani, R., Dupont Monod, S., Oukacha, G. et al.: [Acute bilateral angle-closure glaucoma induced by topiramate: contribution of Visante OCT]. J Fr Ophtalmol, 33(5); 2010 : 307-311. French.
133. Takusagawa, HL., Hunter, RS., Jue, A. et al.: Bilateral uveal effusion and angle-closure glaucoma associated with bupropion use. Arch Ophthalmol, 130(1); 2012 : 120-122.
134. Tanaka, S., Chuman, Y., Akaike, K. et al.: [A case of topiramate-induced angle closure glaucoma]. Nihon Shinkei Seishin Yakurigaku Zasshi, 31(3); 2011 : 131-133. Japanese.
135. Tanihara, H., Akita, J., Honjo, M. et al.: Angle closure caused by multiple, bilateral iridociliary cysts. Acta Ophthalmol Scand, 75(2); 1997 : 216-217.
136. Torricelli, A., Reis, AS., Abucham, JZ. et al.: Bilateral nonarteritic anterior ischemic neuropathy following acute angle-closure glaucoma in a patient with iridoschisis: case report. Arq Bras Oftalmol, 74(1); 2011 : 61-63.
137. Trittibach, P., Frueh, BE., Goldblum, D.: Bilateral angle--closure glaucoma after combined consumption of “ecstasy“ and marijuana. Am J. Emerg Med, 23(6); 2005 : 813-814.
138. Ullman, S., Wilson, RP., Schwartz, L.: Bilateral angle-closure glaucoma in association with the acquired immune deficiency syndrome. Am J Ophthalmol, 101(4); 1986; 419-424.
139. van Issum, C., Mavrakanas, N., Schutz, JS. et al.: Topiramate-induced acute bilateral angle closure and myopia: pathophysiology and treatment controversies. Eur J Ophthalmol, 21(4); 2011 : 404-409.
140. Viestenz, A., Bergua, A., Mardin, CY. et al.: [Acute bilateral angle-closure glaucoma secondary to ciliary body epithelial cysts of the pars plicata correlation with the ultrasound biomicroscope]. Klin Monbl Augenheilkd, 217(2); 2000 : 127-129. German.
141. Viet Tran, H., Ravinet, E., Schnyder, C. et al.: Blood-brain barrier disruption associated with topiramate-induced angle-closure glaucoma of acute onset. Klin Monbl Augenheilkd, 223(5); 2006 : 425-427.
142. Vishwakarma, P., Raman, GV., Sathyan, P.: Mefenamic acid-induced bilateral transient myopia, secondary angle closure glaucoma and choroidal detachment. Indian J Ophthalmol, 57(5); 2009 : 398-400.
143. Waheeb, S., Feldman, F., Velos, P. et al.: Ultrasound biomicroscopic analyse of drug-induced bilateral angle-closure glaucoma assocciated with supraciliary choroidal effusion. Can J Ophthalmol, 38(4); 2003 : 299-302.
144. Weiler, DL.: Zonisamide-induced angle closure and myopic shift. Optom Vis Sci, 92(5); 2015: e46-51.
145. Willett, MC., Edward, DP.: Refractory topiramate-induced angle-closure glaucoma in a man: a case report. J Med Case Rep, 5; 2011 : 33.
146. Wright, KW., Chrousos, GA.: Weill-Marchesani syndrome with bilateral angle-closure glaucoma. J Pediatr Ophthalmol Strabismus, 22(4); 1985 : 129-132.
147. Yang, P., Liu, X., Zhou, H. et al.: Vogt-Koyanagi-Harada disease presenting as acute angle closure glaucoma at onset. Clin Exp Ophthalmol, 39(7); 2011 : 639-647
148. Yao, J., Chen, Y., Shao, T. et al.: Bilateral acute angle closure glaucoma as a presentation of Vogt-Koyanagi-Harada syndrome in four chinese patients: a small case series. Ocul Immunol Inflamm, 21(4); 2013 : 286-291.
149. Yazdani, S., Esfandiari, H., Safi, S. et al.: Oseltamivir (Tamiflu)-induced Bilateral Ciliochoroidal Effusion and Angle Closure Glaucoma: What Type of Idiosyncratic Reaction? J Ophthalmic Vis Res, 12(4); 2017; 434-436.
150. Zalta, AH., Smith, RT.: Peripheral iridoplasty efficacy in refraktory topiramate-associated bilateral acute angle-closure glaucoma. Arch Ophthalmol, 126(11); 2008 : 1603-1605.
151. Zambarakji, HJ., Simcock, PR.: Bilateral angle closure glaucoma in HIV infection. J R Soc. Med, 89(10); 1996 : 581-582.
152. Zelefsky, JR., Fine, HF., Rubinstein, VJ. et al.: Escitalopram-induced uveal effusions and bilateral angle closure glaucoma. Am J Ophthalmol, 141(6); 2006 : 1144-1147.
153. Zimmermann, A., Lorenz, B., Schmidt, W.: [Bilateral acute angle-closure glaucoma due to an infection with Hantavirus]. Ophthalmologe, 107(11); 2010 : 1072-1076. German.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 4-
All articles in this issue
- Slovo vedoucího redaktora
- Výročie narodenia prof. MUDr. Milana Izáka, PhD, FEBO
- Panu docentovi s láskou...
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
- Late postoperative opacification of a hydrophobic acrylic intraocular lens AcryNovaTMPC 610Y
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Ranibizumab in macular oedema secondary to branch retinal vein occlusion – 24 months of treatment
- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- SIMULTANEOUS BILATERAL ACUTE ANGLE-CLOSURE GLAUCOMA IN MILLER FISHER SYNDROME
- Lichen planus as a possible rare cause of an ocular disease
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Lichen planus as a possible rare cause of an ocular disease
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


