-
Medical journals
- Career
Ranibizumab in macular oedema secondary to branch retinal vein occlusion – 24 months of treatment
Authors: M. Středová; A. Stepanov; J. Studnička; J. Nekolová; N. Jirásková
Authors‘ workplace: Oční klinika Fakultní nemocnice Hradec Králové, Sokolská 581, Hradec Králové, 500 05 přednostka: prof. MUDr. Naďa Jirásková, Ph. D., FEBO
Published in: Čes. a slov. Oftal., 75, 2019, No. 4, p. 190-198
Category: Original Article
doi: https://doi.org/10.31348/2019/4/3Overview
Purpose: To retrospectively evaluate the efficacy and safety of ranibizumab treatment for macular edema (ME) secondary to branch retina vein occlusion (BRVO) after 24 months.
Materials and Methods: This study included 39 eyes of 39 patients with ME associated with BRVO treated at the Ophthalmology Department of Faculty Hospital in Hradec Kralove. The average age of included patiens was 69,3 years, the mean duration of symptoms before treament was 5,4 months, the mean baseline visual acuity (VA) was 54,6 ETDRS (Early Treatment Diabetic Retinopathy Study) letters, the mean baseline central retinal thickness (CRT) was 544,9 µm. At 64,1% patients a retinal laserphotocoagulation was performed before intravitreal ranibizumab. After one year, the study was discontinued by 17 patiens, the remaining 22 patients were observed for 24 months. Initially, there were 3 doses of intravitreal ranibizumab administered in monthly intervals, further injections were applied according to PRN (pro re nata) regiment. Patients were examined at baseline and then at 3, 6, 9, 12 and 24 months from initiation of the treatment. In this study, the effect of ranibizumab on functional and morphological parameters of the affected eye was monitored, the safety of this treatment was also evaluated.
During the follow-up, a statistically significant improvement in VA was achieved in every visit in comparison to baseline parameters, the mean VA gain at the 3 month visit was 12,1 ETDRS letters (p < 0,001), at 6 months 12,5 letters (p < 0,001), at 9 months 10,5 letters (p < 0,001), at 12 months 12,5 (p < 0,001), at 24 months 8,6 letters (p < 0,05). There was a statistically significant decrease in CRT as well in the 3, 6, 9, 12 and 24 months visits, namely 249,0 µm (p < 0,001), 185,2 µm (p < 0,001), 187,0 µm (p < 0,001), 214,8 µm (p < 0,001) and 205,2 µm (p < 0,001). The average number of doses administered to a patient was 4,9 within 12 months and 7,1 within 24 months. The treatment had greater effect in younger patients with shorter duration of symptoms and baseline VA of less than 55 ETDRS letters (6/24 or worse. Nor serious, neighter long-term adverse events occured, only occasional intraocular pressure elevation after intravitreal application was found.
Conclusion: Our results from common clinical practice are consistent with the results of large clinial trials, we confirmed particularly good treatment efficacy in younger patients with shorter duration of macular edema and poorer baseline visual acuity. The safety of ranibizumab treatment was confirmed.
Keywords:
ranibizumab – anti-VEGF – branch retinal vein occlusion – BRVO
INTRODUCTION
Retinal vein occlusions (RVO) are vascular pathologies of the retina, causing severe loss of visual acuity (VA) due to macular edema (ME) (9, 10, 36). The incidence of RVO is stated at 180 000 per year in the United States of America (7). According to the size of the zone of capillary non-perfusion, RVO is divided into ischemic and non-ischemic forms, and according to the localisation of obstruction into central retinal vein occlusion (CRVO), branch (BRVO) and hemiretinal (7, 36).
There are various therapeutic modalities in the treatment of RVO focused on the individual pathogenic mechanisms of origin of thrombosis, on accelerating the resolution of the thrombus, on reducing the degree of ME or on the prevention of neovascularisation. Of the individual modalities we can list the following: sheathotomy with vitrectomy in the area of arteriovenous crossing, anti-aggregation therapy with fibrinolysis, isovolemic hemodilution, application of steroids intravitreally or periocularly, and laser treatment – GRID macular laser photocoagulation (LPC), LPC of the peripheral regions of the retina or arteriolar constriction (14, 26, 27). Since the publication of the results of the BVOSG (Branch Vein Occlusion Study Group), GRID LPC has become the standard in the treatment of BRVO. After laser treatment, improvement of visual functions takes place very slowly (7). The pharmaceutical of choice in the solution of ME secondary to BRVO is now VEGF (vascular endothelial growth factor) inhibitors, which target the molecular basis of its origin (8, 26, 27). The higher effectiveness of anti-VEGF treatment in comparison with laser treatment of the retina has been demonstrated in numerous clinical trials (24). This data is confirmed also by the recently published randomised trial BRIGHTER, focusing on the long-term effectiveness of treatment and the safety profile of ranibizumab within a broad population of patients with BRVO, including patients with retinal ischemia (32, 35). The influence of occlusion leads to an overproduction of VEGF (1, 5, 21) and interleukin 6 (IL6) (22), which support a leakage of fluid from the capillaries into the tissue by breaching the blood-retinal barrier, and due to higher vascular permeability upon damage to the intercellular junctions of the endothelial cells (31). ME is closely linked with retinal hypoxia, and above all with various degrees of hypoxia in the macula (27). If pronounced hypoxia persists in the macular region, this leads to irreversible structural changes and permanent worsening of VA (27). The anti-VEGF preparations currently used in the treatment of ME secondary to RVO include ranibizumab (Lucentis) and aflibercept (Eylea). Ranibizumab, which we shall focus on in this study, is a Fab (antigen-binding fragment) of a humanised antibody acting against VEGF, with the capacity to neutralise all isoforms of VEGF-A and their biologically active degradation products (4, 28). Its application is contraindicated in patients with suspected or active periocular or intraocular inflammation, and in the case of hypersensitivity to the pharmaceutical substance (38). The effectiveness, safety and long-term results of application of ranibizumab have been confirmed by randomised trials, of which I primarily name the consecutively linked trials BRAVO (33), HORIZON (13) and RETAIN (8). The BRAVO (33) trial demonstrated that intraocular injections of ranibizumab every month for a period of 6 months lead to a marked reduction of ME and an improvement of VA. These benefits were sustained throughout the period of the following 6 months, in which patients were observed on a monthly basis and injections were applied only in the case of recurrence or persistence of ME (2, 3, 6, 7). The HORIZON trial demonstrated that many patients continued to require injections of ranibizumab 2 years after the commencement of treatment, and that less frequent observation during the course of the second year led to a worsening of edema and a reduction of VA (13). In the RETAIN trial a further, subsequent observation of the patients who had completed the HORIZON trial was conducted. With an average observation period of 50.2 months, 50% of patients with BRVO recorded regression of edema, defined as the absence of intraretinal fluid without the need for an injection of ranibizumab over a period of at least 6 months. These patients had an excellent visual result, with final VA of 6/12 or better in approximately 80% of cases. The other 50% of patients required an average of 3 injections of ranibizumab over the course of the last year of observation, but 80% of them had a resulting VA of 6/12 or better. In one half of the patients with BRVO, good resulting VA was achieved without the necessity of reapplication, but in the other half of the patients the final result remains uncertain, the majority of patients retains good visual potential, requiring only infrequent reapplications for the solution of recurrent ME (8).
It is generally known that the prognosis of BRVO is relatively good even without any therapeutic intervention, in which 50-60% of eyes spontaneously attain VA of 6/12 or better (11, 12, 19, 20). The prognostically unfavourable factors of BRVO include: baseline VA of 6/24 or worse and advanced age (age over 60-70 years according to individual authors (16, 25, 27).
METHOD
The cohort includes patients who were treated at the Department of Ophthalmology at the University Hospital in Hradec Králové for ME secondary to BRVO, by means of intravitreally applied ranibizumab over the period from October 2014 to the beginning of 2017. The total number of patients meeting the above-stated parameters was 82, out of whom we were unable to include 43 patients in the study for the following reasons: 9 patients underwent another therapeutic modality before or during treatment with ranibizumab, specifically 6 patients received intravitreal application of dexamethasone (Ozurdex), 1 intravitreal application of aflibercept (Eylea), 1 intravitreal bevacizumab (Avastin) and for 1 patient pars plana vitrectomy was indicated due to cystoid ME; 26 patients did not complete at least one year of the observation period. After the initial three injections the patients were observed further by a local ophthalmologist (1 patient upon her own wishes, in the case of the remaining 25 patients no further intravitreal anti-VEGF treatment was indicated – in 1 patient due to the risks outweighing the benefits of treatment, in 3 patients due to no improvement or even worsening of VA after the three initial injections, in 21 patients we achieved a complete absorption of ME with CRT of 250 µm and less after the initial injections), 8 patients did not report for further treatment without stating the reason, and as a result were not observed for a sufficiently long period.
Our study thus included 39 eyes of 39 patients, of whom women represented 64.1% and men 35.9%. The average age of the patients was 69.3 years ± 10.4 (within the range of 42 to 88 years). The average length of duration of the complaints before the commencement of treatment was 5.4 months, average baseline VA was 54.6 ± 11.2 letters of ETDRS (Early Treatment Diabetic Retinopathy Study) chart, average baseline central retinal thickness (CRT) was 544.9 ± 155.8 µm. Before the commencement of treatment with ranibizumab, 25 patients (64.1%) had undergone laser treatment of the macula. The demographic data of the patients is presented in Table 1, the characteristics of the cohort according to baseline VA by Graph 1. One-year observation was completed by 17 patients, the remaining 22 patients were observed over a period of 24 months.
1. Demographic data of patients 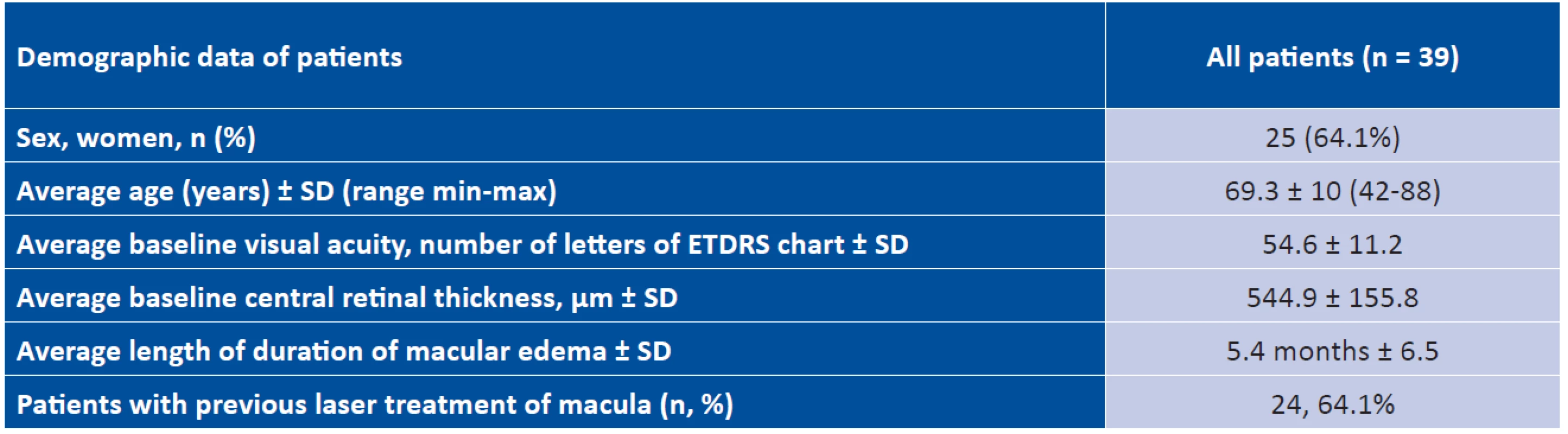
SD (standard deviation), ETDRS (Early Treatment Diabetic Retinopathy Study) 1. Characteristics of cohort according to baseline visual acuity (number of patients) 
This concerns a retrospective study. The condition for inclusion for treatment was the fulfilment of all indication limitations for payment of treatment set by the State Institute for Drug Control, which are as follows: changes in the macula are not of an irreversible character, and at the same time are refractory to laser treatment or it is not possible to perform laser treatment (extensive retinal haemorrhage, macrocystic changes in the macula). The period of duration of ME must not exceed 12 months, the patients must be compensated regarding internal aspects; exclusion criteria are myocardial infarction or stroke within an interval of less than three months previously. VA of the patient must be within the range of 6/12-6/120, CRT 250 µm or more (37).
At each examination, VA was determined with the aid of an ETDRS chart, the patients’ intraocular pressure was measured, the anterior and posterior segment of the eye were examined on a slit lamp. CRT was determined with the aid of OCT examination (optical coherence tomography, Cirrus Zeiss HD-4000). First of all 3 impregnating intravitreal doses of ranibizumab were applied to all patients, with a time interval of one month, and further injections were applied according to a PRN (pro re nata) treatment regimen, in which treatment was continued in the case of change of VA and/or signs of ME on OCT. Intravitreal application took place under aseptic conditions, following irrigation of the conjunctival sac with 5% Betadine solution. The patients were observed before the commencement of treatment and subsequently at intervals of 3, 6, 9, 12 and 24 months from the commencement of therapy, follow-up examinations were performed at regular 3-monthly intervals.
In the study we evaluated the influence of treatment with ranibizumab on the functional and morphological parameters of the afflicted eye. We also observed the safety profile of the preparation.
The quantitative data is expressed by average and range. Changes of VA and CRT were evaluated with the aid of a paired Student t-test. Statistical significance was defined as p < 0.05.
RESULTS
Average baseline VA was 54.6 ± 11.2 of ETDRS chart, at a follow-up examination 3 months after the commencement of treatment we recorded an average gain of 12.1 letters (p < 0.001) in comparison with the baseline values, after 6 months the gain was 12.5 letters (p < 0.001), after 9 months an improvement by 10.5 letters (p < 0.001), after 12 months by 12.5 (p < 0.001) and after 24 months by 8.6 letters (p < 0.05).
Improvement of VA to a resulting value of 6/12 or better within a period of 1 year was achieved in 46.2% of eyes (n = 39), and within a period of 2 years in 45.5% (n = 22). VA of 6/60 or worse did not occur in any patient within a period of one year, and in one patient within a period of two years.
Average baseline CRT on OCT was 544.9 ± 155.8 µm, in comparison with the baseline data we recorded an average reduction by 249.0 µm (p < 0.001) after 3 months, after 6 months the reduction was by 185.2 µm (p < 0.001), after 9 months 187.0 µm (p < 0.001), after 12 months 214.8 µm (p < 0.001) and after 24 months 205.2 µm (p < 0.001).
Values of CRT of < 250 µm were attained within a period of 1 year by 20.5% of patients (n = 39) and in a period of 2 years by 18.2% (n = 22).
During the observation we achieved a statistically significant improvement of VA and CRT in comparison with the baseline data at all follow-up examinations, in comparison with previous examinations a statistically significant improvement of VA was recorded only at the examination after 3 months (p < 0.001), other changes of VA in comparison with the previous follow-ups were not statistically significant. A statistically significant reduction of CRT in comparison with the previous examination was achieved at the visit after 3 months (p < 0.001) and 6 months (p < 0.05). The development of average VA is illustrated in Graph 2, the development of average CRT in Graph 3.
2. Development of best corrected visual acuity over observation period 
3. Development of average central retinal thickness in comparison with average baseline value 
In 28% of patients there was a stabilisation of the finding (complete absorption of ME without the necessity of reapplication of anti-VEGF) after the 3 initial doses of ranibizumab, in which we have data available about these patients also from the second year in 36% of cases. All of these patients were cured (i.e. no reapplication was necessary during the following year of observation), in 64% of patients we have no data from the second year and it is not possible to state whether this concerned temporary or permanent absorption of ME.
The average number of doses of ranibizumab was 4.9 over the course of 12 months, over the full two-year observation period 7.1.
The median age of the patients included in our study was 69 years. In patients aged 69 years and younger we recorded an average gain of 14.7 letters of ETDRS chart (p < 0.001) 12 months after the commencement of treatment, and an average reduction of CRT by 235 µm (p < 0.001), after 24 months the total average gain of letters was 10.1 (p < 0.05) and the average reduction of CRT by 188 µm (p < 0.05). VA of 6/12 or better was attained by 70% of patients within a period of 1 year, and by 50% of patients within a period of 2 years.
In the group of patients aged 70 years and over, the average gain 12 months after the commencement of treatment was 9.93 letters of ETDRS chart (p < 0.001), and the average reduction of CRT was by 194 µm (p < 0.001), after 24 months the total average gain of letters was 7.08 (p = 0.08) and the average reduction of CRT by 218 µm (p < 0.001). VA of 6/12 or better was achieved in 21% of patients within a period of 1 year, and in 42% of patients within a period of 2 years.
The group of patients was divided into two halves according to the length of duration of ME, in the first half the duration of complaints was 4 months or less, in the second half longer than 4 months. In both groups we achieved identical average changes of CRT after 12 months of therapy – a reduction of 216 µm, and after 24 months the average reduction in the group with the shorter duration of complaints was 205 µm, in the group with complaints persisting longer than 4 months 194 µm. Patients with the shorter duration attained CRT of 250 µm or less in 24% of cases (n = 21) within a period of 1 year, and within a period of 2 years in 14% (n = 14). Patients with a duration of complaints of more than 4 months before the commencement of treatment had CRT of 250 µm or less in 11% of cases (n = 18) within a period of 1 year, and within a period of 2 years in 25% (n = 8). The resulting average gain of VA in patients from the first group was 17.1 letters of ETDRS chart after 12 months and 15.6 letters after 24 months. In the group with the longer duration of ME, the average gain after 12 months was 6.77 letters of ETDRS chart, after 24 months there was an average loss of 5.4 letters in comparison with the baseline data. Upon a mutual comparison of data within a period of one year this concerns a statistically significant difference in the case of both VA and CRT (p = 0.01); within a period of 2 years this was not statistically significant in either case.
Patients with baseline VA of 55 letters of ETDRS chart (6/24) or better attained an average gain of 7.42 letters (p < 0.05) after one year of treatment with ranibizumab, after 2 years the average gain was by 1.33 letters (p = 0.39) in comparison with baseline VA. Patients in whom baseline VA was 54 letters of ETDRS chart or worse attained an average gain of 17 letters of ETDRS chart (p < 0.001) after one year of treatment, after 2 years the average gain of VA was by 13.6 letters (p < 0.05).
Patients who had not undergone LPC of the centre of the retina before the commencement of anti-VEGF therapy had an average baseline VA of 47.4 ± 10.0 letters of ETDRS chart, at the follow-up examination 3 months after the commencement of treatment we recorded an average gain of 16.6 letters in comparison with the baseline values, after 6 months the gain was 17.3 letters, after 9 months the improvement was by 15.2 letters, after 12 months 18.1 and after 24 months 14.1 letters (p = 0.004). VA of 6/12 or better was achieved in 36% of patients within a period of 1 year, and within a period of 2 years in 40% of patients. Average baseline CRT on OCT was 612.6 ± 167.5 µm, at the follow-up examination after 3 months we recorded an average reduction by 321.1 µm in comparison with the baseline data, after 6 months the reduction was by 294.7 µm, after 9 months 287.1 µm, after 12 months 294.7 µm and after 24 months 296.6 µm (p < 0.001). CRT of 250 µm or less was achieved within a period of 1 year in 29% of patients, within a period of 2 years in 20% of patients. The average number of doses of ranibizumab was 5.2 within 12 months, 7.5 within 24 months.
Patients who had undergone LPC of the retina before intravitreal application of ranibizumab had an average baseline VA of 57.9 ± 10.1 letters of ETDRS chart, at the follow-up examination 3 months after the commencement of treatment we recorded an average gain of 9.6 letters in comparison with the baseline values, after 6 months 10.0 letters, after 9 months 8.0 letters, after 12 months 9.4 and after 24 months 4.0 letters (p = 0.18). VA of 6/12 or better was achieved within a period of 1 year in 52% of patients, within a period of 2 years in 50% of patients. Average baseline CRT on OCT was 507.0 ± 134.8 µm, at the follow-up examination after 3 months we recorded an average reduction by 208.8 µm in comparison with the baseline values, after 6 months the reduction was 120.8 µm, after 9 months 128.2 µm, after 12 months 168.7 µm and after 24 months 130.6 µm (p < 0.05). CRT of 250 µm or less was achieved within a period of 1 year in 16% of patients, within a period of 2 years in 17% of patients. The average number of doses of ranibizumab was 4.8 within 12 months, 7.25 within 24 months.
During the observation period, besides complications in connection with intravitreal application of ranibizumab we recorded only transitory elevation of intraocular pressure, which was resolved conservatively by means of application of topical anti-glaucomatous agents or peroral acetozalamide. Elevation of intraocular pressure above 23 mmHg occurred in 13 patients, of whom 6 patients experienced elevation above 25 mmHg. The maximum measured value of intraocular tension after application was 27 mmHg. No subsequent complications were observed in connection with intravitreal application of ranibizumab, for example severe intraocular inflammation, hemophthalmos or development of glaucoma.
In our study we find a high percentage of “uncured patients”, i.e. those who require further reapplication of anti-VEGF preparations – within a period of 1 year 32 (82%) of patients (n = 39) and at the follow-up examination after 2 years 19 (86.4%) (n = 22).
1. Retina of right eye in patient with occlusion of superior temporal branch of central retinal vein – image obtained upon indication of intravitreal treatment with ranibizumab, on the retina there is a finding of spattered haemorrhages and cotton wool spots in the central region and in the upper temporal quadrant of the retina, best corrected visual acuity in the right eye at the time of indication is 6/30 
2. Image of optical coherence tomography in the same patient obtained upon indication for intravitreal treatment with ranibizumab, central retinal thickness 759 μm, macrocystic edema in the region of the upper 2/3 of the central landscape 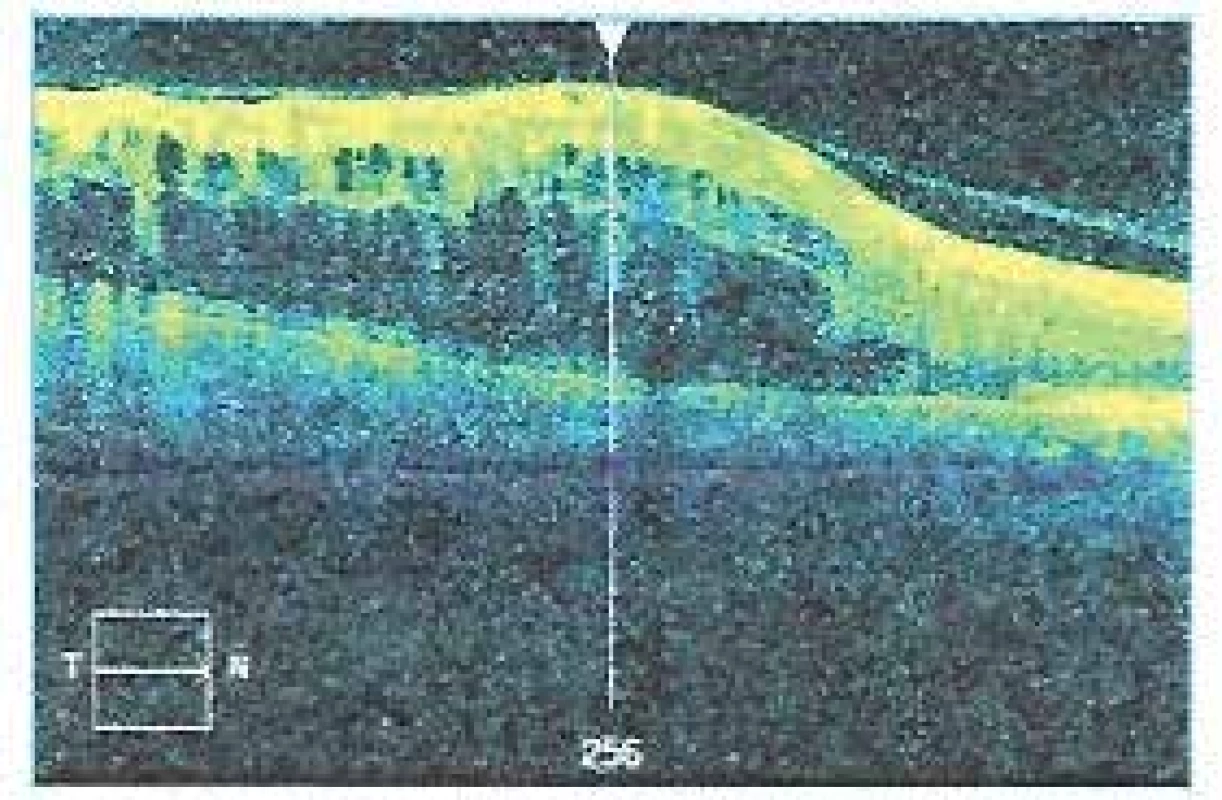
3. Image of optical coherence tomography in the same patient obtained after 3 intravitreal injections of ranibizumab, central retinal thickness 292 μm, residual edema in the upper part of the central landscape, best corrected visual acuity 6/7.5. Further injections were not indicated, the residual edema was spontaneously absorbed without the necessity of further reapplication, throughout the period of the following year the patient maintained visual acuity of 6/6 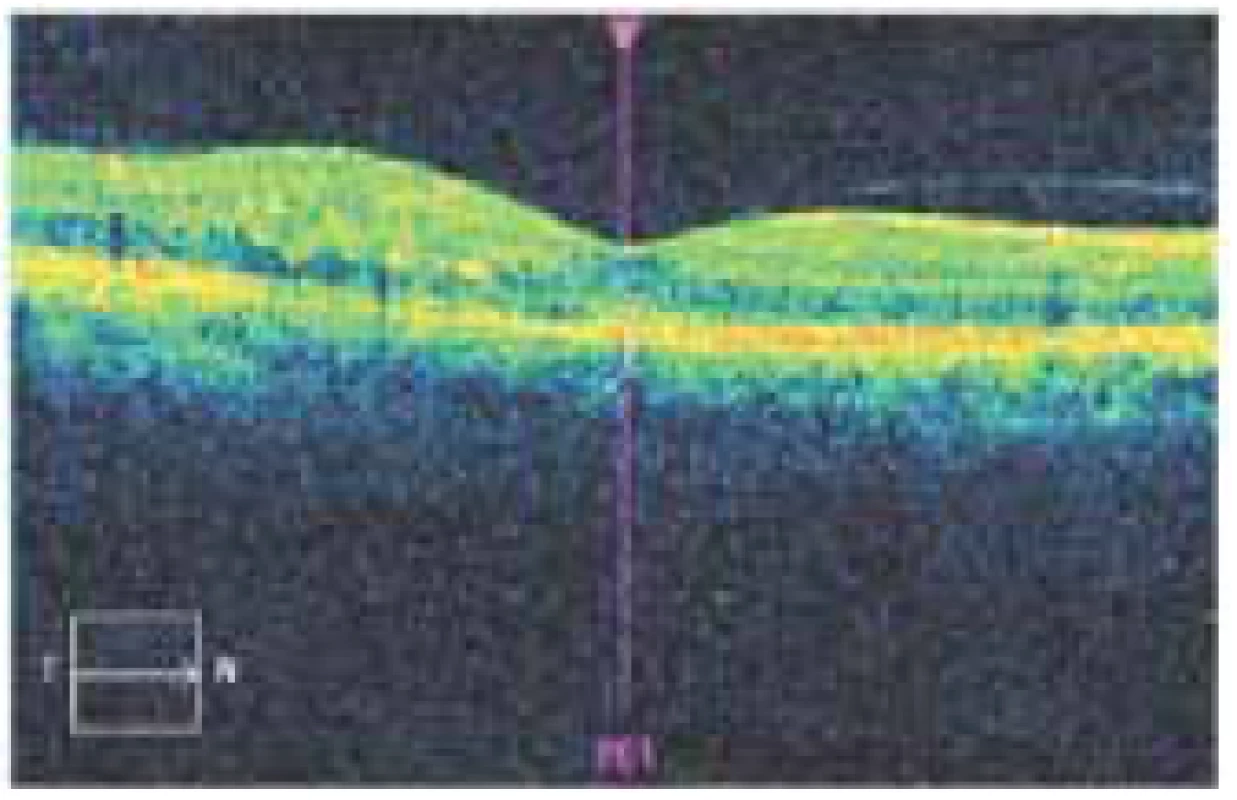
DISCUSSION
In our retrospective study, the efficacy and safety of treatment with intravitreally applied ranibizumab was evaluated in patients with ME secondary to BRVO. The patients were observed over a period of up to 24 months. During the observation a statistically significant increase of VA and reduction of ME was achieved in the patients in our cohort after 1 and 2 years of treatment.
In his study, Suner states that an increase of VA by 15 or more letters of ETDRS chart is clinically significant, with regard to the fact that this difference represents a doubling of the visual angle, and at the same time this change is considered clinically significant also by the questionnaire compiled by the National Eye Institute – Visual Functioning Questionnaire (29). In the BRAVO trial the average gain of letters after 12 months of anti-VEGF therapy was 18.3 letters. A gain of fifteen or more letters of ETDRS chart was obtained after 12 months of treatment in 56% of patients treated with 0.3 mg of ranibizumab, and in 60.3% treated with 0.5 mg of ranibizumab (33). A study conducted by Czech authors from the Department of Ophthalmology at Královské Vinohrady University Hospital on a cohort of 54 patients treated with 0.5 mg of ranibizumab according to a therapeutic schema of 3 initial doses followed by a PRN therapeutic regimen demonstrates an average increase of VA by 16.5 letters after one year of treatment. A gain of fifteen or more letters of ETDRS chart was achieved in 63% of eyes (18). In our study we attained an improvement of VA by 12.5 letters of ETDRS chart after 12 months, therefore we achieved clinically significant improvement of VA, a gain of 15 or more letters of ETDRS chart, in 43% of eyes after 1 year of treatment, and in 23% at the follow-up after two years.
Our results are somewhat worse than in the above-stated publications, although the available data with average baseline VA and the length of duration of the complaints are comparable. The difference in the number of applied doses is substantial in comparison with the BRAVO trial, in which an average of 3.8 injections were applied during the course of 6 months, while in the case of the team of authors from the Královské Vinohrady University Hospital the number of applied doses is almost identical as in our study – 4.8 over the course of 12 months. The results may be influenced by a further range of factors, for example the proportion of eyes with relatively good baseline VA, which therefore have less room for improvement. Further factors are the average age of the patients and the percentage of patients with a prognostically unfavourable occlusion, with regard to the fact that these factors are significant predictors of the results of therapy (16, 25, 26, 27).
In patients with a shorter duration of complaints before the commencement of therapy, we attained statistically significantly better anatomical and functional results within a period of 1 year of observation. The reason for the worse resulting parameters in the group with the longer duration of complaints is most probably the onset of irreversible changes in the region of the macula due to the influence of prolonged hypoxia (8, 25).
An interesting feature mentioned by Puche et al. is that although baseline VA indirectly proportionally correlated with baseline CRT, the resulting values of VA and CRT do not correlate, but a relationship is observed in the attained change of these parameters. A correlation is further observed between baseline and resulting VA and between baseline and resulting CRT (23). The fact that higher baseline CRT predicted a greater change of CRT at the end of observation is noted also in the study by Kim et al. (17). This trend is also confirmed by our study. This phenomenon is not surprising, with regard to the fact that a patient with higher baseline CRT has greater room for improvement. Kim also points to the fact that patients of a younger age have a higher probability of achieving CRT of less than 250 µm – he does not specify an exact age (17). In our cohort, in the younger patients (aged up to 69 years) there was a larger and statistically significant gain of letters and a more pronounced reduction of CRT after 12 months of treatment than in the group of older patients (70 years and over). This was also demonstrated in the study by the authors Řehák et al. (25).
A publication by Korean authors states that in patients with ME secondary to BRVO treated by various modalities – various intravitreally applied anti-VEGF preparations, triamcinolone or laser, or a combination thereof, there was a more pronounced improvement of VA in patients of a younger age, with worse baseline VA and a shorter duration of ME (17). This data corresponds with the results of the SCORE (Standard Care versus Corticosteroid for Retinal Vein Occlusion) study (15), whereas by contrast the BVOSG study does not state any correlation of resulting VA with age (30, 34). Puche mentions that neither the age of patients, nor the type of occlusion (ischemic, non-ischemic), nor the length of duration of symptoms had any influence on changes of anatomical relations or visual functions (23). On the basis of our results, it would be possible to consider a shorter duration of complaints, lower age and worse baseline VA to be predictive factors of the effectiveness of treatment on the resulting functional parameters. This is also confirmed by previously published studies (16, 25, 26).
The RETAIN study (8) states that due to recurrent or persistent ME, approximately 50% of patients require repeated intravitreal doses of ranimizubab. In our study this percentage is up to twice as high, although this may be distorted by the fact that “cured patients” (patients who did not require a further application of anti-VEGF) were sent for observation to local ophthalmologists, and as a result did not attend further follow-ups at our clinic and were therefore not included in this study. A role here is also played by the fact that, primarily for reasons of capacity, there is generally a relatively long period between the worsening of the patient’s complaints and the further reapplication of the pharmaceutical.
CONCLUSION
In our retrospective study, we evaluated the efficacy and safety of treatment of ME secondary to BRVO by means of intravitreal application of ranibizumab up to a period of 2 years. Our experience with the treatment correspond with the results of large clinical trials, although we were limited by the smaller scope of the cohort of patients. A further factor complicating the data gathering was the fact that the intervals between the follow-up examinations on patients cannot be ensured entirely regularly during normal operation, and frequently the interval between applications must be extended for capacity reasons. On the basis of our results, we confirm the findings from previously published studies that the effect of treatment of ME secondary to BRVO by anti-VEGF preparations is more pronounced in patients aged 69 and under, with a shorter duration of complaints and worse baseline VA. We also demonstrated the safety of treatment with ranibizumab. The precise parameters of predictive factors of the success of treatment and long-term effectiveness remain the subject of investigation.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 2. 7. 2019
Accepted: 23. 8. 2019
Available on-line: 6.1.2020
MUDr. Markéta Středová
Oční klinika Fakultní nemocnice Hradec Králové
Sokolská 581
500 05 Hradec Králové,
Sources
1. Aiello LP., Avery RL., Arrigg PG. et al.: Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med, 331; 1994 : 1480–7.
2. Brown DM., Campochiaro PA., Bhisitkul RB. et al.: Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology, 118; 2011 : 1594–602.
3. Brown DM., Campochiaro PA., Singh RP. et al.: Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point of a phase III study. Ophthalmology, 117; 2010 : 1124–33.
4. Brown DM., Kaiser PK., Michels M. et al.: Ranibizumab versus verteporfin for neovascular age related macular degeneration. N Engl J Med, 355; 2006 : 1432–44.
5. Campochiaro PA., Hafiz G., Shah SM. et al.: Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther, 16; 2008 : 791–9.
6. Campochiaro PA., Brown DM., Awh CC. et al.: Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. Ophthalmology, 118; 2011 : 2041–9.
7. Campochiaro PA., Heier JS., Feiner L. et al.: Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology, 117 (6); 2010 Jun: 1102-1112.
8. Campochiaro PA., Sophie R., Pearlman J. et al.: Long-term outcomes in patients with retinal vein occlusion treated with ranibizumab: the RETAIN study. Ophthalmology, 121 (1); 2014 : 209-219.
9. Feng XX., Li C., Shao WW. et al.: Intravitreal anti-VEGF agents, oral glucocorticoids, and laser photocoagulation combination therapy for macular edema secondary to retinal vein occlusion: preliminary report. Int J Ophthalmol, 11 (3); 2018 : 429-437.
10. Fuma S., Nishinaka A., Inoue Y. et al.: A pharmacological approach in newly established retinal vein occlusion model. Sci Rep, 7; 2017 : 1-14.
11. Gutman FA., Zegarra H., Zakov ZN.: The natural course of tempoval retinal vein occlusion. Trans Am Acad Opthalmol Otolaryngol, 78; 1974 : 178-192.
12. Hayreh SS., Rojas P., Podhajsky P. et al.: Ocular neovascularization with retinal occlusion: III. Incidence of neovascularization with retinal vascular occlusion. Ophthalmology, 90; 1983 : 488–506.
13. Heier JS., Campochiaro PA., Yau L.: Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology, 119 (4); 2012 : 802-9.
14. Ho M., Liu DT., Lam DS. et al.: Retinal vein occlusions, from basics to the latest treatment. Retina, 36 (3); 2016 : 432–448.
15. Ip MS., Oden NL., Scott IU. et al.: SCORE Study report 3: study design and baseline characteristics. Ophthalmology, 116; 2009 : 1770-7.
16. Jaissle GB., Szurman P., Feltgen N.: Predictive factors for functional improvement after intravitreal bevacizumab therapy for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol, 249 (2); 2011 : 183-92.
17. Kim SJ., Yoon YH., Kim HK. et al.: Baseline predictors of visual acuity and retinal thickness in patients with retinal vein occlusion. J Korean Med Sci, 30 (4); 2015 : 475-82.
18. Lalinska L., Krasny J., Studeny P. et al.: Results of the first 12 months treatment of macular edema complicating BRVO in patients treated with ranibizumab. Cesk Slov Oftalmol, 74 (2); 2018 : 62-67.
19. Magargal LE., Sanborn GE., Kimmel AS. et al.: Tempoval branch retinal vein obstruction: A review. Ophthal Surg, 17; 1986 : 240–246.
20. Michels RG., Gass JDM.: Natural course of temporal retinal branch occlusion. Trans Am Acad Ophthalmol Otolaryngol, 78; 1974 : 166–177.
21. Noma H., Funatsu H., Yamasaki M. et al.: Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and interleukin-6. Am J Oph-thalmol, 140; 2005 : 256–61.
22. Noma H., Minamoto A., Funatsu H. et al.: Intravitreal levels of vascular endothelial growth factor and interleukin-6 are correlated with macular edema in branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol, 244; 2006 : 309–315.
23. Puche N., Glacet A., Mimoun G. et al.: Intravitreal ranibizumab for macular oedema secondary to retinal vein occlusion: a retrospective study of 34 eyes. Acta Ophthalmol, 90 (4); 2012 Jun: 357-61.
24. Regnier SA., Larsen M., Bezlyak V. et al.: Comparative efficacy and safety of approved treatments for macular oedema secondary to branch retinal vein occlusion: a network meta-analysis. BMJ Open, 5 (6); 2015 Jun: e007527.
25. Rehak J., Dusek L., Chrapek O. et al.: Initial visual acuity is an important prognostic factor in patients with branch retinal vein occlusion. Ophthalmic Res, 45(4); 2011 : 204-9.
26. Rehak J., Dusek L., Sin M. et al.: Long term visual outcome after arteriolar constriction in patients with branch retinal vein occlusion. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 158 (4); 2014 : 577-82.
27. Rehak J., Rehak M.: Branch retinal vein occlusion: pathogenesis, visual prognosis, and treatment modalities. Curr Eye Res, 33 (2); 2008 : 111-31.
28. Rosenfeld PJ., Brown DM., Heier JS. et al.: Ranibizumab for neovascular age-related macular degeneration. N Engl J Med, 355; 2006 : 1419–31.
29. Suner IJ., Kokame GT., Yu E. et al.: Responsiveness of NEI VFQ-25 to changes in visual acuity in neovascular AMD: validation studies from two phase 3 clinical trials. Invest Ophthalmol Vis Sci, 50; 2009 : 3629-35.
30. Scott IU., VanVeldhuisen PC., Oden NL. at al.: Baseline Predictors of Visual Acuity and Retinal Thickness Outcomes in Patients with Retinal Vein Occlusion. SCORE Study Report 10. Ophthalmology, 118 (2); 2011 Feb: 345–352.
31. Silva RM., Faria de Abreu JR., Cunha-Vaz JG.: Blood-retina barrier in acute retinal branch vein occlusion. Graefes Arch Clin Exp Ophthalmol, 233; 1995 : 721–726.
32. Tadayoni R., Waldstein SM., Boscia F. et al.: Sustained Benefits of Ranibizumab with or without Laser in Branch Retinal Vein Occlusion: 24-Month Results of the BRIGHTER Study. Ophthalmology, 124 (12); 2017 Dec: 1778-1787.
33. Thach AB., Yau L., Hoang C. et al.: Time to clinically significant visual acuity gains after ranibizumab treatment for retinal vein occlusion: BRAVO and CRUISE trials. Ophthalmology, 121 (5); 2014 May: 1059-66.
34. The Branch Vein Occlusion Study Group: Argon laser photocoagulation for macular edema in branch vein occlusion, Am J Ophthalmol, 98 (3); 1984 : 271-82.
35. Varma R., Bressler NM., Suñer I. et al.: Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: results from the BRAVO and CRUISE trials. Ophthalmology, 119 (10); 2012 : 2108–2118.
36. Doporučené postupy pro léčbu RVO, dostupné z URL: http://www.cvrs.cz/dokumenty/RVO-guidelines.pdf
37. Indikační omezení úhrady léčby Lucentisem pojišťovnou dostupné z URL: www.cvrs.cz/indikacni-omezeni-uhrady-lucentis
38. SPC (souhrn údajů o léčivém přípravku) Lucentis, dostupné z URL: http://www.ema.europa.eu/docs/cs_CZ/document_library/EPAR_-_Product_Information/human/000715/WC500043546.pdf
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 4-
All articles in this issue
- Slovo vedoucího redaktora
- Výročie narodenia prof. MUDr. Milana Izáka, PhD, FEBO
- Panu docentovi s láskou...
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
- Late postoperative opacification of a hydrophobic acrylic intraocular lens AcryNovaTMPC 610Y
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Ranibizumab in macular oedema secondary to branch retinal vein occlusion – 24 months of treatment
- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- SIMULTANEOUS BILATERAL ACUTE ANGLE-CLOSURE GLAUCOMA IN MILLER FISHER SYNDROME
- Lichen planus as a possible rare cause of an ocular disease
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Lichen planus as a possible rare cause of an ocular disease
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


