-
Medical journals
- Career
Late postoperative opacification of a hydrophobic acrylic intraocular lens AcryNovaTMPC 610Y
Authors: M. Otrošinová 1; J. Novák 1; J. Kvasnička 2; O. Žídek 2
Authors‘ workplace: Nemocnice Pardubického kraje a. s., Pardubická nemocnice, Oční oddělení 1; Contipro a. s. Dolní DobroučPrimář očního oddělení doc. MUDr. Jan Novák, CSc., FEBO 2
Published in: Čes. a slov. Oftal., 75, 2019, No. 4, p. 172-179
Category: Original Article
doi: https://doi.org/10.31348/2019/4/1Overview
Purpose: To report late postoperative opacification of a hydrophobic acrylic intraocular lens (IOL) AcryNovaTMPC 610Y as well as the clinical consequences in patients 10 years after uncomplicated cataract surgery.
Materials and Methods: Medical records were reviewed of 23 patients (26 eyes) with AcryNovaTMPC 610Y implantated between years 2005 and 2007. Next clinical examination was performed 10 years after surgery. We assessed best corrected distance visual acuity (BCDVA), contrast sensitivity (CSV-1000E) and relative opacity of IOL material, (OCULUS Pentacam HR). Results of BCDVA and Pentacam were analysed statistically. One explanted IOL was analysed using anterior segment OCT in vitro and spectroscopic method EDX (Energy-dispersive X-ray spectroscopy).
Results: Opacification led to a statistically significant reduction in the best corrected distance visual acuity (BCDVA) = (0,95 ± 0,10) versus (0,87 ± 0,20) and to increase of IOL opacity only in some lenses but statistically significant in the average (6,37 ± 2,16)% versus value of (14,22 ± 5,87)%. In the explanted IOL we have documented structural changes of primarily hydrophobic raw material leading to property of hydrophilic one.
Conclusion: Some batches of AcryNovaTMPC 610Y were produced from raw material of poor quality which is the cause of its structural changes and its progressive opacification.
Keywords:
intraocular lens AcryNovaTMPC 610Y – material opacification – hydrophobic intraocular lens – posterior capsule opacification – Pentacam
INTRODUCTION
The three-piece monofocal spherical intraocular lens AcryNovaTMPC 610Y was produced from hydrophobic acrylate.
At our centre the AcryNovaTMPC 610Y lens was implanted in 171 patients, comprising 61 men and 96 women, between the years 2005 and 2007. In this report we present the development of opacity of the hydrophobic lens 10 years after its implantation, and the influence of opacity of the material on visual functions. The aim of this study was to determine the frequency of increased opacity of the IOL, concerning whether opacity is an obligatory of facultative phenomenon, and the influence it has on visual functions.
Cohort and method
Included in the study were 23 patients (26 eyes) with senile cataract, who were operated on at the Department of Ophthalmology at the Pardubice Hospital in the period from 2005 to 2007, in whom an AcryNovaTMPC 610Y hydrophobic lens was implanted, with measurement of the opacity of the lens material performed immediately after surgery. The surgeries throughout the entire cohort were performed by means of an identical surgical technique: subconjunctival anaesthesia, incision of conjunctiva, posterior limbal incision with a size of 2.5 mm, 2x lateral service 1 mm incision, anterior continual capsulorhexis, hydrodissection, phacoemulsification of the nucleus of the lens, bimanual irrigation and aspiration of the cortex, aspiration of the lens cells of the anterior capsule and polishing of the posterior capsule and equator, extension of the tunnel to 3.5 mm and implantation of a folded intraocular lens AcryNovaTMPC 610Y by forceps into the lens capsule. There followed rinsing of the viscoelastic material and hydration of the paracenteses with toning of the eyeball.
The patients were examined one week after surgery. At this follow-up examination we evaluated BCVA, the percentage of IOL opacity with the aid of a Scheimpflug camera Pentacam (OCULUS Pentacam HR). Measurement of relative opacity (in percentages) was conducted symmetrically to the central axis in two fields in the IOL material of both of the two performed cross-sections (0°-180° and 90°-270°). The values in the central axis cannot be used for the incidence of optic artefacts. The isoline was set as opacity in an optically empty anterior chamber above the anterior surface of the IOL (Fig. 1).
1. Scheimpflug photograph. Measurement of relative opacity (in %) in two fields in the IOL material in crosssection (90° to 270°) at first follow-up. The isoline was set as opacity in an optically empty anterior chamber above the anterior surface of the IOL 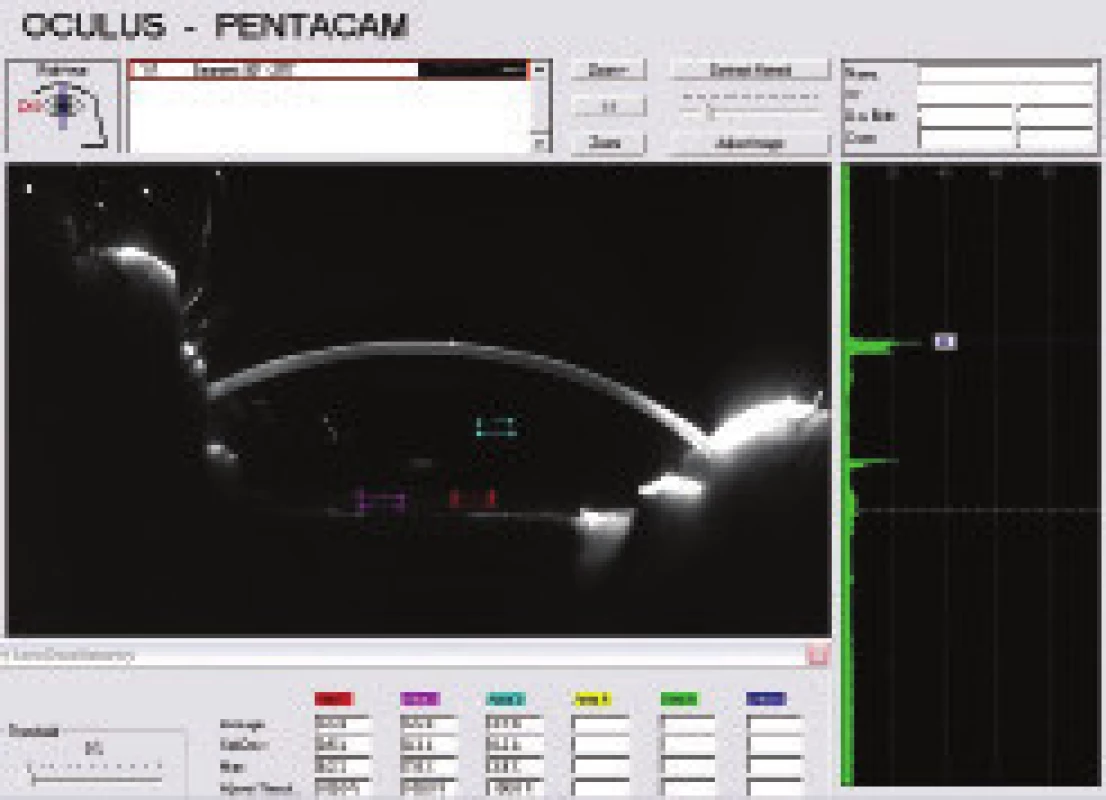
At a follow-up examination of the cohort after 10 years we evaluated BCVA, we examined contrast sensitivity under mesopic conditions on CSV-1000E tables, the percentage of opacity of the IOL with the aid of a Scheimpflug camera (OCULUS Pentacam HR), using an identical method in all 4 quadrants (Fig. 2). In each patient we performed an OCT examination in order to exclude retinal pathology, which could have influenced the resulting BCVA. We also evaluated the incidence of posterior capsule opacification (PCO).
2. Scheimpflug photograph. Measurement of relative opacity (in %) in two fields in the IOL material in cross-section (0° to 180°) at second follow-up after ten years. The isoline was set as opacity in an optically empty anterior chamber above the anterior surface of the IOL 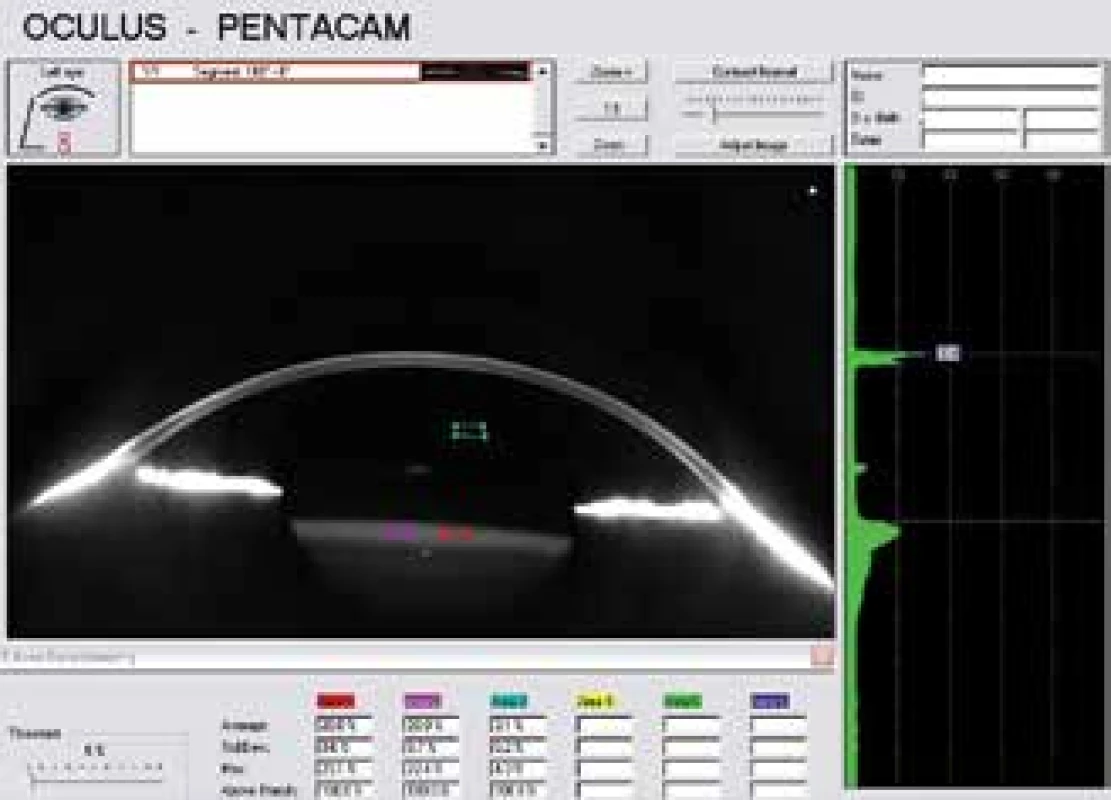
A Kolmogorov-Smirnov normality test was used for the statistical analysis. Because none of the observed values had a normal probability distribution, a non-parametric Wilcoxon test was used in the following analysis for a comparison of the parameters between the postoperative follow-up examinations one week and 10 years after surgery. A value of p = 0.05 or less was considered statistically significant.
With regard to the progression of opacification and the significant influencing of visual functions, in one case we were forced to perform explantation of the IOL. We examined the explanted IOL optically with the aid of AS-OCT Optovue (linear cross-sections in vitro), with the aid of a SEM (scanning electron microscope) for assessment of the homogeneity of the IOL, and with the aid of the EDX spectroscopic method (EDX-Energy Dispersive X-Ray Spectroscopy) for assessment of potential calcification of the material.
RESULTS
A total of 23 patients (26 eyes) reported for the follow-up examination 10 years after the operation, comprising 12 women and 11 men. No complications were recorded in any of them perioperatively. Table 1 presents a comparison of the observed values at the first postoperative follow-up and at the follow-up after ten years: BCVA and relative values of measured opacity of the implanted lens in the individual quadrants. Average opacity of the material immediately after implantation was 6.37%. The lowest value was 3.90% and the highest 11.3%. Average opacity of the material after 10 years was 14.22%, lowest measured value 4.40% and highest 23.15%. After ten years there was a significant decrease of BCVA (p = 0.026). In the cohort we determined markedly reduced contrast sensitivity (Table 2). Because we did not examine contrast sensitivity immediately after surgery, it is not possible to statistically evaluate the decrease in contrast sensitivity. From the measured values, after 10 years it is primarily the lenses (numbering 19), in which a very significant clouding took place, which have a significant influence on the resulting measured values (opacity of material, BCVA and contrast sensitivity). In 7 eyes (7 patients) from the cohort, opacity of the intraocular lens did not increase whatsoever or only negligibly. In these patients we did not record any decrease of visual acuity or a significant change of contrast sensitivity.
1. BCVA, relative opacity of IOL material in individual quadrants and average opacity of IOL at first follow-up one week after surgery and at follow-up after 10 years, statistical evaluation 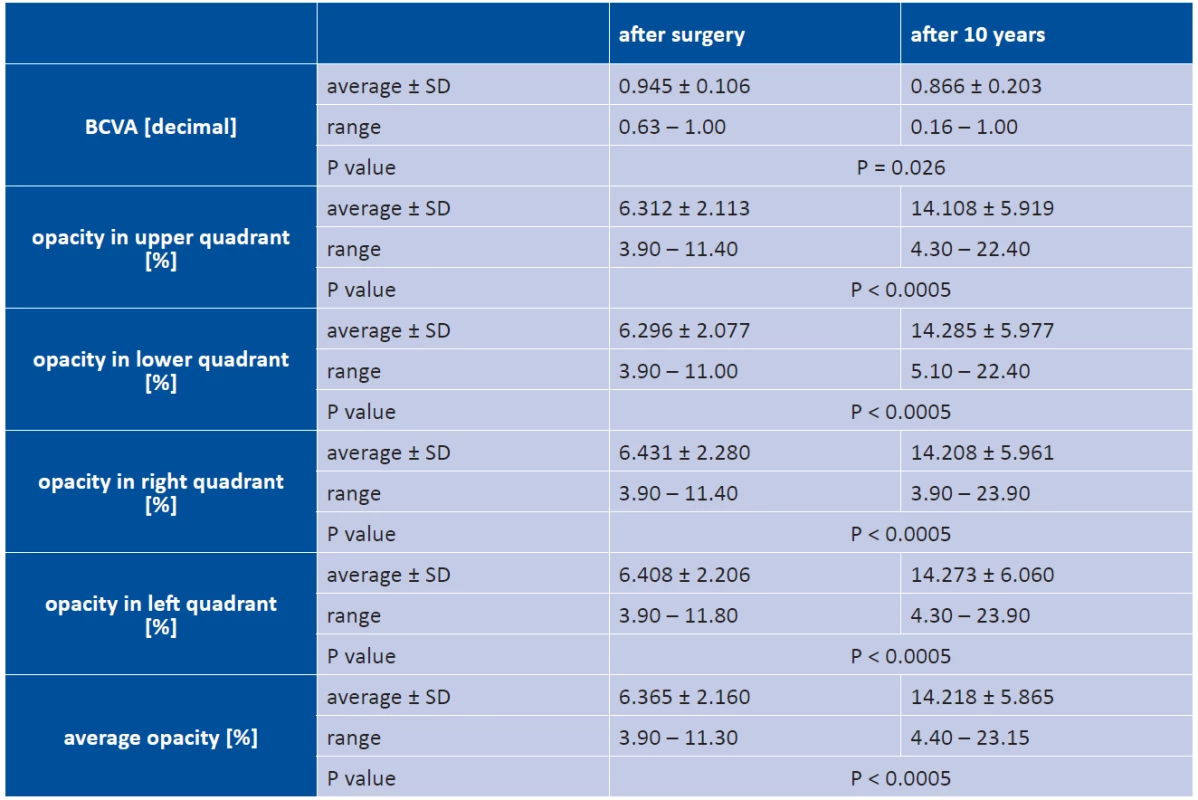
NKZO – nejlépe korigovaná zraková ostrost
SO – směrodatná odchylka2. Contrast sensitivity with the aid of CSV – 1000E at follow-up after ten years 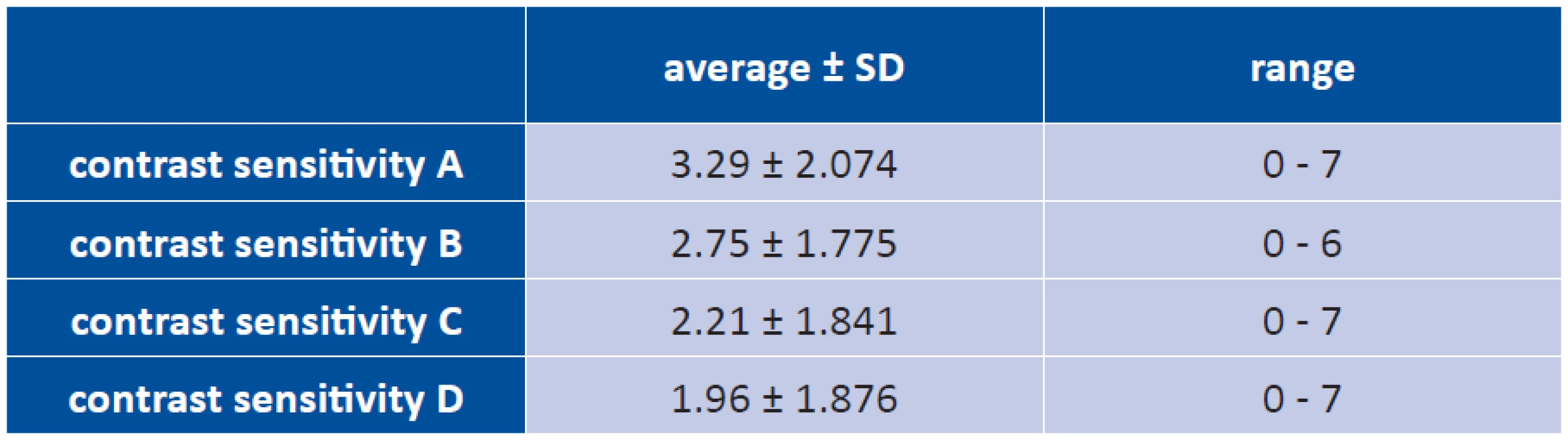
SD – standard deviation Upon an examination of the numbers of the individual production series, we succeeded in demonstrating that when the lenses from one production batch were implanted there was a similar increase of opacity of the material. In table 3 the individual batches are colour differentiated. With regard to the relatively small cohort in comparison with the quantity of production series in our cohort, it was not possible to prove the opposite –that there is no increase in opacity in certain batches, because in the cohort there were not at least two implanted lenses from a batch in which we measured a low increase in opacity. It is however possible to point to the fact that in these patients there was no decrease of visual acuity or contrast sensitivity.
3. BCVA and average opacity of IOL at first follow-up after surgery and at follow-up after 10 years in individual batches, contrast sensitivity at examination after 10 years 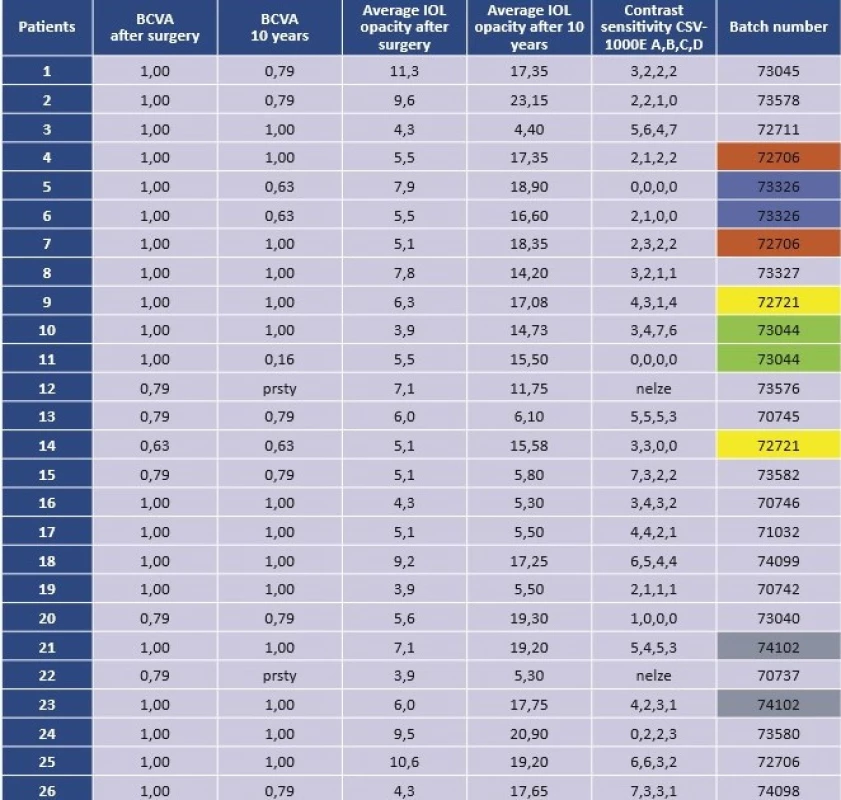
BCVA – best corrected visual acuity Lens replacement was indicated for an 82-year-old patient 9 years after bilateral implantation in 2005, in whom there was a decrease of BCVA to 0.63. At the examination zero contrast sensitivity upon glare was determined, and the opacity of the lens material was 21%. We indicated replacement in one eye only (Fig. 3, 4), on the second eye laser capsulotomy was performed at another centre on the assumption that this concerned a secondary cataract, without effect. In this eye, also with BCVA of 0.63, we did not indicate replacement of the IOL due to the higher risk.
3. Anterior segment – opacified IOL AcryNovaTMPC 610Y before explantation 
4. Anterior segment OCT – opacified IOL AcryNovaTMPC 610Y before explantation 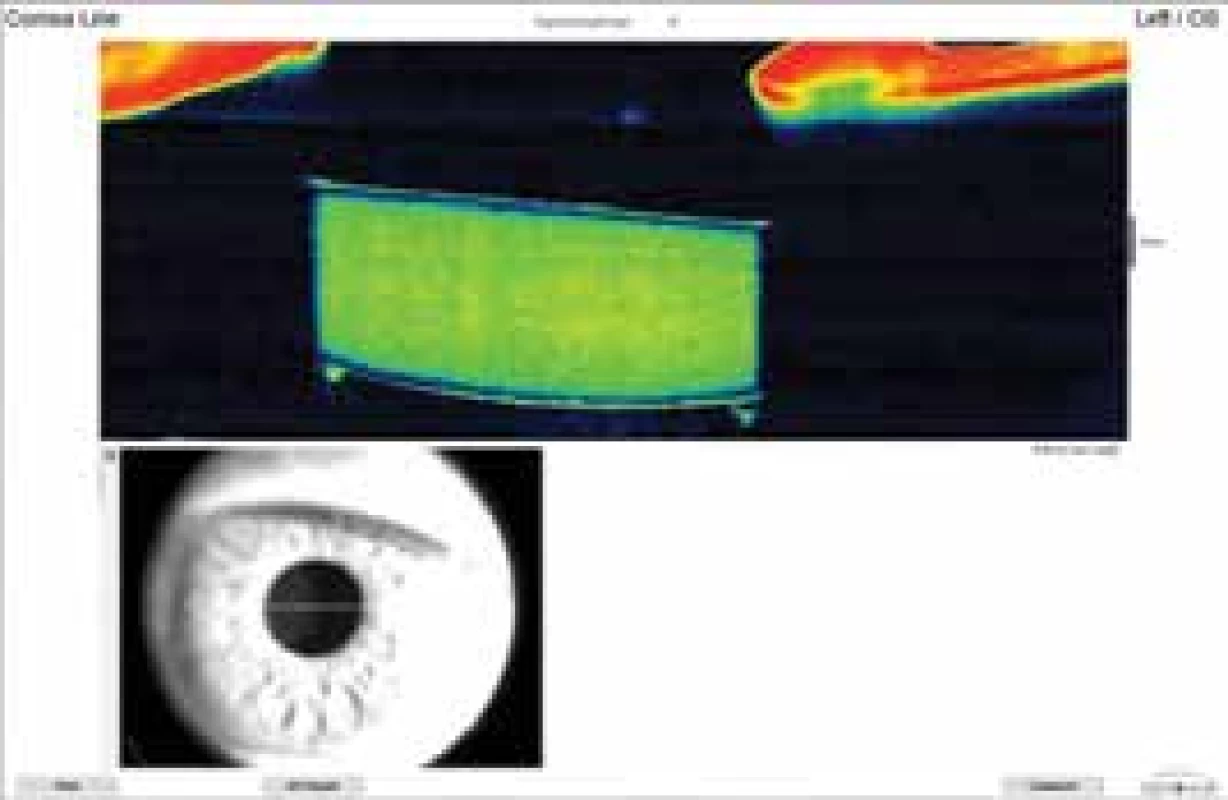
We did not find signs of non-homogeneity (i.e. micro glistening – vacuoles) in the material upon an examination of the explanted IOL and test with the aid of SEM upon 20 000x enlargement. Using the EDX method we did not record the presence of calcium or phosphorus, and we therefore excluded calcification of the material. Anterior segment OCT of AcryNova hydrophobic lenses with symptoms of opacification shows homogeneous light dispersion (scattering effect), in contrast with lenses from transparent PMMA or hydrophobic acrylate (Fig. 5).
5. Cross-sections with the aid of anterior segment OCT in vitro – a. homogeneous light dispersion (“scattering effect”) on explanted IOL, b. disappearance of light dispersion on dried IOL and c. light dispersion on rehydrated IOL, which demonstrates that this concerns hydrophilic material 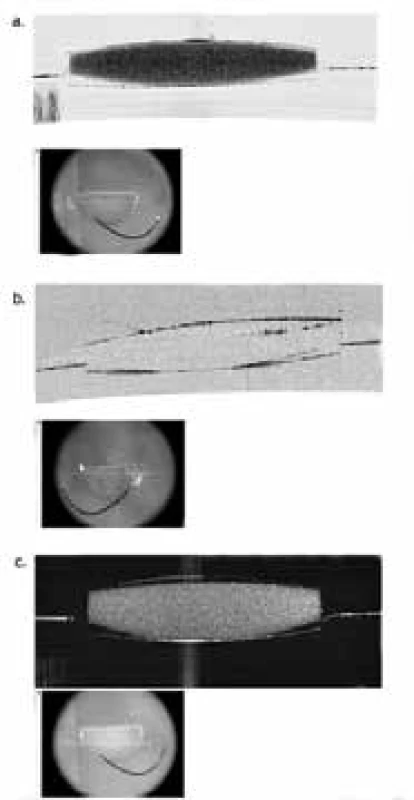
DISCUSSION
Phacoemulsification with implantation of an IOL into the lens sac has been the standard in microincision cataract surgery in the last few decades. Upon a large number of operations, material complications began to appear perioperatively and in the postoperative period (26). Reduction of the transparency of the IOL material is one of the serious complications influencing visual functions, and has been described in a range of IOLs (23), first of all in 1987 in the case of hydrogel IOLs (3). “Snowflakes” opacities were described on hard polymethylmethacrylate IOLs, as well as a change of colouring of the material in silicon IOLs, opacity caused by calcification in IOLs with hydrophilic acrylate, and the presence of micro-vacuoles (glistening) in hydrophobic IOLs (1, 36). Opacification may affect the anterior and posterior surface of the lens, deep structures of the central part, haptics or almost the entire IOL (23, 26, 33). This is the reason for constant research into materials suitable for the production of IOLs.
The majority of serious cases of opacification have been described in relation to IOLs from hydrophilic acrylate, and in hydrophobic lenses it is relatively rare (28). Hydrophobic lenses are implanted ever increasingly with regard to the overall higher biocompatibility and low incidence of the onset of opacification of the posterior capsule, resistance to change of colour and the impossibility of calcification of the internal structures of the material (15, 16, 30, 32). Their more rapid spread has been hindered by the more complex and therefore more expensive production technology. Nevertheless, lenses from hydrophobic acrylate also have certain complications.
The best known optically significant phenomenon is glistening – the appearance of vacuoles or micro-vacuoles in the material. The phenomenon occurs upon distension of preformed heterogeneities in the material. Within these an expansion of gas or accumulation of fluid takes place. Hydrophobic IOLs are also permeable for water molecules. Glistenings are micro-vacuoles (11, 12, 20, 25, 35) which are visible on a slit lamp, already shortly after implantation. They are usually distributed diffusely throughout the entire optics of the IOLS (36, 37). Although the phenomenon of glistening reduces contrast sensitivity, the literary data attests to the fact that decrease of visual acuity is rare (6, 24, 35, 38).
The precise etiopathogenesis leading to opacification of IOLs still remains unclear. Numerous potential risk factors have been described, such as damage to material upon handling of the lens, breach of the blood-ocular barrier during intraocular operation, excessive postoperative inflammatory reaction (5, 7, 8, 22). The overall health condition of the patient may play a role also in the pathogenesis of calcification (26, 28). At the same time, however, studies have been published which have excluded the influence of the surgeon and patient. Cases have been described of entire batches of IOLs from certain manufacturers with a high probability of the occurrence of opacification, regardless of secondary surgical intervention or comorbidity of patients (2, 17, 31). In the case of these manufacturers it is possible to indicate as the cause admixtures of impurities in the material, faulty production or storage, as well as interaction with the packaging material. However, individual factors such as intraocular inflammations or ocular and systemic comorbidities which influence the metabolism of the eye may contribute to the process (17, 31).
Another phenomenon is transitory opacities of the IOL. This concerns a reversible phenomenon, in the literature acutely occurring perioperative opacification of an IOL from hydrophobic acrylate as a consequence of temperature changes has been described (14). This demonstrates the importance of storing lenses at the correct temperature.
The material of the IOL has a certain spatial molecular structure, filled with a larger or smaller quantity of water molecules. Breach of this schema leads to a loss of transparency (increase of opacity) of the material. The breakdown of such a structure was probably responsible for the progression of opacity of the IOLs in our cohort, without the necessity of accumulation of other substances (compounds of calcium were excluded).
Affliction of visual functions caused by opacification of IOLs is rarely directly linked to a decrease of visual acuity. Contrast sensitivity also plays an important role in the quality of an individual's vision. Our results clearly demonstrate a fundamental deterioration of this function, with a small influence on visual acuity. In our cohort there was first of all a clinical deterioration of contrast sensitivity, progressively followed by “cloudy” or “blurred” vision, and in a section of the patients finally also a decrease of visual acuity.
Contrast sensitivity depends on various factors and decreases with the age of the patient (19). Our results attest to the fundamental influence of lens opacity. From the results it clearly ensues that a decrease of contrast sensitivity is dependent upon the opacity of the IOL material (Table 3).
In the case of clinically serious opacifications of IOLs, explantation is the only possible option for treatment. However, explantations are burdened by a high risk of intraoperative and postoperative complications (4). In a series of 25 eyes with an opacified Aqua-Sense IOL (single-piece IOL made of hydrophilic acrylate copolymer with water content of 25%, Aaren Scientific, Ontario, California, USA), Dagres et al. published a value of complications (dehiscence of zonules, rupture of posterior capsule, decompensation of cornea) as high as 48% (4). Above all the strong adhesion of the IOL to the capsule makes explantation a demanding procedure, and in many cases subsequent implantation of a new IOL into the sac may be impossible. Indication for surgical explantation of an opacified IOL therefore requires thorough preoperative diagnosis, clinical deliberation, and following the decision to proceed with explantation also informed consent of the patient. It should be considered only in the case of highly engaged patients with clinically clear symptoms (especially decrease of visual acuity).
The data from the literature attests to the fact that lens epithelial cells (LECs) overgrow on the surface of the IOL and may cause PCO, decentration of the IOL and fibrous changes of tissue even up to phimosis of the capsule (10, 29). Changes are less serious on the surface of an IOL made of hydrophobic acrylate in comparison with lenses made from hydrophilic material (34). The material of intraocular lenses therefore plays a large role in the onset of secondary cataract (18, 27). Here we emphasize the advantages of thorough cleaning of the lens sac, including the equator, in our cohort the incidence of PCO was relatively low, in 50% of cases after ten years.
The clinical picture of opacification of the IOL material may be diverse. Opacities may be reminiscent of confluent cellular PCO. This causes doctors in these cases to proceed to Nd:YAG laser capsulotomy (9, 13, 21). Breach of the posterior capsule leads to difficult explantation of the IOL and increases the frequency of potential complications during the operation, with an increased risk of loss of the vitreous body (21). Nd:YAG laser capsulotomy may induce further damage to the IOL material and lead to a further reduction of optical quality of the IOL. There can be no doubt that capsulotomy is not useful in such cases.
CONCLUSION
According to our results, up to 20% opacity of the material does not cause a greater decrease of visual functions, with the exception of contrast sensitivity, and, as a result, patients do not seek medical attention. However, implantation of an IOL in younger individuals remains a problem. In our cohort, the youngest patient was aged 51 years at the time of implantation of the IOL, and the progression of opacity is approximately 1% per year. It is possible to deduce that a clinically significant decrease of visual functions may occur after 20 years, i.e. in the time of advanced age (the average life expectancy in our population is 82 years in women, 76 years in men). Therefore, it occurs at a time when the quality of life of senior citizens should not be impaired by phenomena other than those dependent on biological changes of the organism.
Hydrophobic acrylate can also be subject to degradation accompanied by a decrease in transparency. There is a spectrum of examinations (e.g. Scheimpflug camera, anterior segment OCT) which are capable of detecting degradation of materials, manifested in increased opacity of the IOL shortly after implantation. These IOLs should be quickly excluded from the implantation portfolio. Upon suspicion of a defect of material we do not recommend the performance of YAG capsulotomy, with respect to the loss of the option of safe replacement of the IOL.
We see the cause of opacities in our cohort in an error in the production procedure in certain batches of IOLs, or in the poor quality material used for these batches.
The study was presented in abbreviated form as a lecture at the annual congress of the Czech Ophthalmology Association in Hradec Králové on 18 September 2015
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 7. 6. 2019
Accepted: 3. 7. 2019
Available on-line: 6. 1. 2020
MUDr. Marianna Otrošinová
NPK a.s., Pardubická nemocnice
Kyjevská 44, 532 03 Pardubice
Sources
1. Apple, DJ., Peng, Q., Arthur, SN. et al.: Snowflake degeneration of polymethyl methacrylate posterior chamber intraocular lens optic material: A newly described clinical condition caused by unexpected late opacification of polymethyl methacrylate. Ophthalmology, 109; 2002 : 1666–1675.
2. Bompastor-Ramos, P., Povoa, J., Lobo, C. et al.: Late postoperative opacification of a hydrophilic-hydrophobic acrylic intraocular lens. J Cataract Refract Surg, 42; 2016 : 1324–1331.
3. Buchen, SY., Cunanan, CM., Gwon, A. et al.: Assessing intraocular lens calcification in an animal model. J Cataract Refract Surg, 27; 2001 : 1473-1484.
4. Dagres, E., Khan, MA., Kyle, GM. et al.: Perioperative complications of intraocular lens exchange in patients with opacified Aqua-Sense lenses. J Cataract Refract Surg, 30; 2004 : 2569–2573.
5. De Cock, R., Fajgenbaum, MA.: Calcification of Rayner hydrophilic acrylic intra-ocular lenses after Descemet‘s stripping automated endothelial keratoplasty. Eye (Lond), 28; 2014 : 1383–1384.
6. Dhaliwal, DK., Mamalis, N., Olson, RJ. et al.: Visual significance of glistenings seen in the AcrySof intraocular lens. J Cataract Refract Surg, 22; 1996 : 452–457.
7. Dhital, A., Spalton, DJ., Goyal, S. et al.: Calcification in hydrophilic intraocular lenses associated with injection of intraocular gas. Am J Ophthalmol, 153; 2012 : 1154–1160.
8. Fellman, MA., Werner, L., Liu, ET. et al.: Calcification of a hydrophilic acrylic intraocular lens after Descemet-stripping endothelial keratoplasty: Case report and laboratory analyses. J Cataract Refract Surg, 39; 2013 : 799–803.
9. Gartaganis, SP., Kanellopoulou, DG., Mela, EK. et al.: Opacification of hydrophilic acrylic intraocular lens attributable to calcification: Investigation on mechanism. Am J Ophthalmol, 146; 2008 : 395-403.
10. Gayton, JL., Apple, DJ., Peng, Q. et al.: Interlenticular opacification: clinicopathological correlation of a complication of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg, 26;2000 : 330–336.
11. Gunenc, U., Oner, FH., Tongal, S. et al.: Effects on visual function of glistenings and folding marks in AcrySof intraocular lenses. J Cataract Refract Surg, 27; 2001 : 1611–1614.
12. Hayashi, K., Hirata, A., Yoshida, M. et al: Long-term effect of surface light scattering and glistenings of intraocular lenses on visual function. Am J Ophthalmol, 154; 2012 : 240–251.
13. Haymore, J., Zaidman, G., Werner, L. et al.: Misdiagnosis of hydrophilic acrylic intraocular lens optic opacification: Report of 8 cases with the memoryLens. Ophthalmology, 114; 2007 : 1689-1695.
14. Helvacı, S.: Acute opacification of hydrophobic acrylic intraocular lens during implantation:result of temperature variation. Arq Bras Oftalmol, 78; 2015 : 267.
15. Hollick, EJ., Spalton, DJ., Ursell, PG.: Biocompatibility of poly (methyl methacrylate), silicone, and AcrySof intraocular lenses: randomized comparison of the cellular reaction on the anterior lens surface. J Cataract Refract Surg, 24; 1998 : 361–366.
16. Cheng, JW., Wei, RL., Cai, JP. et al.: Efficacy of different intraocular lens materials and optic edge designs in preventing posterior capsular opacification: a meta-analysis. Am J Ophthalmol, 143; 2007 : 428–436.
17. Izak, AM., Werner, L., Pandey, SK. et al.: Calcification of modern foldable hydrogel intraocular lens designs. Eye (Lond), 17; 2003 : 393–406.
18. Jirásková, N., Rozsíval, P.: Metody hodnocení zkalení zadního pouzdra po operaci katarakty, Cesk Slov Oftalmol, 60; 2004 : 155–157.
19. Liutkeviciene, R., Cebatoriene, D., Liutkeviciene, G. et al.: Associations between contrast sensitivity and aging. Medicina (Kaunas), 49; 2013 : 273–277.
20. Matsushima, H., Mukai, K., Nagata, M. et al.: Analysis of surface whitening of extracted hydrophobic acrylic intraocular lenses. J Cataract Refract Surg, 35; 2009 : 1927–1934.
21. Morgan-Warren, PJ., Andreatta, W., Patel, AK.: Opacification of hydrophilic intraocular lenses after descemet stripping automated endothelial keratoplasty. Clin Ophthalmol, 9; 2015 : 277-283.
22. Neuhann, IM., Neuhann, TF., Rohrbach, JM.: Intraocular lens calcification after keratoplasty. Cornea, 32; 2013 : 6–10.
23. Neuhann, IM., Werner, L., Izak, AM. et al.: Late postoperative opacification of a hydrophilic acrylic (hydrogel) intraocular lens: A clinicopathological analysis of 106 explants. Ophthalmology, 111; 2004 : 2094–2101.
24. Ogura, Y., Ong, MD., Akinay, A. et al.: Optical performance of hydrophobic acrylic intraocular lenses with surface light scattering. J Cataract Refract Surg, 40; 2014 : 104–113.
25. Ong, MD., Callaghan, TA., Pei, R. et al.: Etiology of surface light scattering on hydrophobic acrylic intraocular lenses. J Cataract Refract Surg, 38; 2012 : 1833–1844.
26. Pandey, SK., Werner, L., Apple, DJ. et al.: Hydrophilic acrylic intraocular lens optic and haptics opacification in a diabetic patient: Bilateral case report and clinicopathologic correlation. Ophthalmology, 109; 2002 : 2042–2051.
27. Pozlerová, J., Nekolová, J., Jirásková, N. et al.: Hodnocení opacit zadního pouzdra u různých typů umělých nitroočních čoček. Cesk Slov Oftalmol, 65; 2009 : 12-15.
28. Prasad, PS., Oliver, SC., Gonzales, CR.: Midlenticular optic opacification of a hydrophobic acrylic intraocular lens in association with retained perfluorocarbon liquid following vitreoretinal surgery. Ophthalmic Surg Lasers Imaging, 9; 2010 : 1–2.
29. Schauersberger, J., Amon, M., Kruger, A. et al: Lens epithelial cell outgrowth on 3 types of intraocular lenses. J Cataract Refract Surg, 27; 2001 : 850–854.
30. Sundelin, K., Friberg-Riad, Y., Ostberg, A. et al.: Posterior capsule opacification with AcrySof and poly (methyl methacrylate) intraocular lenses. Comparative study with a 3-year follow-up. J Cataract Refract Surg, 27; 2001 : 1586–1590.
31. Tandogan, T., Khoramnia, R., Choi, CY. et al.: Optical and material analysis of opacified hydrophilic intraocular lenses after explantation: a laboratory study. BMC Ophthalmology, 15; 2015 : 170.
32. Tetz, M., Jorgensen, MR.: New hydrophobic IOL materials and understanding the science of Glistenings. Curr Eye Res, 40; 2015 : 969–981.
33. Walker, NJ., Saldanha, MJ., Sharp, JA. et al.: Calcification of hydrophilic acrylic intraocular lenses in combined phacovitrectomy surgery. J Cataract Refract Surg, 36; 2010 : 1427–1431.
34. Weinberg, T., Klein, I., Zadok, D. et al.: Lens epithelial cell growth on the anterior optic of 2 hydrophobic intraocular lens models. J Cataract Refract Surg, 42; 2016 : 296–301.
35. Werner, L.: Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg, 33; 2007 : 713–726.
36. Werner, L.: Glistenings and surface light scattering in intraocular lenses. J Cataract Refract Surg, 36; 2010 : 1398–1420.
37. Werner, L., Michelson, J., Ollerton, A. et al.: Anterior segment optical coherence tomography in the assessment of posoperative intraocular lens optic changes J Cataract Refract Surg, 36; 2012 : 1077-1085.
38. Xi, L., Liu, Y., Zhao, F. et al.: Analysis of glistenings in hydrophobic acrylic intraocular lenses on visual performance. Int J Ophthalmol, 7; 2014 : 446–451.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 4-
All articles in this issue
- Slovo vedoucího redaktora
- Výročie narodenia prof. MUDr. Milana Izáka, PhD, FEBO
- Panu docentovi s láskou...
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
- Late postoperative opacification of a hydrophobic acrylic intraocular lens AcryNovaTMPC 610Y
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Ranibizumab in macular oedema secondary to branch retinal vein occlusion – 24 months of treatment
- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- SIMULTANEOUS BILATERAL ACUTE ANGLE-CLOSURE GLAUCOMA IN MILLER FISHER SYNDROME
- Lichen planus as a possible rare cause of an ocular disease
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Lichen planus as a possible rare cause of an ocular disease
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


