-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Clostridium difficile – a dangerous pathogenfor older patients
Clostridium difficile – nebezpečný patogén pro starší pacienty
Infekce způsobená Clostridium difficile (CDI) se stává závažným problémem zejména u geriatrických pacientů, kteří jsou významnou rizikovou skupinou. Cílem této práce je zhodnotit výskyt rizikových faktorů u seniorů, které vedou k onemocnění CDI.
Zkoumaný soubor tvořilo 235 seniorů ve věkové kategorie nad 65 let s potvrzenou diagnózou CDI. Pro diagnózu CDI byl rozhodující nález toxinu A a B ve stolici pacientů, či autopticky potvrzená CDI. Soubor geriatrických pacientů s klostridiovou infekcí tvořilo 148 žen (62,98 %) a 87 mužů (37,02 %). Rizikovým faktorem bylo cévní onemocnění mozku, demence, přítomnost dekubitů a imobilita. V práci se potvrdil jako statisticky významný faktor při MMSE test, ADL test, MNA-SF test a Charlsonův index komorbidity.Klíčová slova:
Clostridium difficile – geriatrický pacient – antibiotická terapie – pseudomembranózni kolitida
Authors: K. Bielaková; H. Matějovská-Kubešová; P. Weber; D. Weberová
Authors place of work: Masaryk University ; Clinic of Geriatric Medicine and General Medicine, The University hospital Brno
Published in the journal: Geriatrie a Gerontologie 2014, 3, č. 4: 171-174
Category: Původní práce/studie
Summary
Clostridium difficile infection (CDI) is becoming a serious problem predominantly in geriatric patients who are a significant risk group. The goal of this study is to evaluate the occurrence of risk factors in seniors which lead to the CDI. The examined group consisted of 235 patients at age over 65 with confirmed diagnosis of CDI. For the diagnosis of CDI finding of toxins A and B in the stool of patients or autopsy confirmation were crucial. The group of geriatric patients with CDI consisted of 148 women (62,98 %) and 87 men (37,02 %). The risk factors comprised the cerebrovascular disease, dementia, presence of pressure ulcers and immobility. The study proved the MMSE test, ADL test, MNA-SF test and Charlson comorbidity index as a statistically important factor.
Key words:
Clostridium difficile – geriatric patient – antibiotic therapy – psedomebranous colitisIntroduction
The disease caused by the bacterium Clostridium difficile (Clostridium difficile infection, CDI) is becoming a serious problem predominantly in geriatric patients who are a significant risk group (1, 2). In recent years there have been epidemics of Clostridium difficile infection with severe course with increasing mortality, wherein its cause is the spread of a new, highly virulent strain of ribotype 027 /NAP1/ B1 which is characterized in a higher production of toxins and greater resistance to antibiotics(3). The goal of this study is to evaluate the occurrence of risk factors in seniors which lead to the CDI disease and to achieve mortality reduction.
Methods
Our retrospective study were realised in patients with clostridium difficile infection, hospitalized at the Clinic of Internal Medicine, Geriatrics and Practical Medicine, Masaryk University, Faculty of Medicine and Brno Faculty Hospital, from January 1, 2008 to December 31, 2013. Within the 6 years of monitoring were diagnosed altogether 258 patients with confirmed CDI, in the age group ranging from 45 to 105 years of age. The group of subjects excluded patients under the age of 65 (altogether 23 patients) and the risk factors were evaluated in the population older than 65 years, so the subsequently examined group of subjects consisted of 235 patients.
Finding of toxin A and B in faeces of patients was crucial for the diagnosis; in one female patient the finding of CDI was confirmed only after the autopsy by the finding of pseudomembranous colitis, and was subsequently confirmed by histological evidence.
In the first two years of the monitored period, to establish the CDI diagnosis in our group of patients, we used the proof of toxin A/B in the faeces by the diagnostic test on the principle of imunochromatography (Xpect, Remel, US), and in the year 2010 by establishing the A/B toxin on the principle of ELFA – “Enzyme Linked Fluorescent Assay” (miniVidas analyser, BioMérieux, France). Afterwards we proceeded to proving the glutamate dehydrogenase (GDH) and C. difficile toxins by immunochromatography (Techlab, US).
The impact of comorbidity was in patients evaluated by the index of comorbidity (Charlson Comorbidity Index, CCI), the impact of malnutrition by the scale for nutritional status assessment – by the shortened version (Mini Nutritional Assessment short-form test, MNA-SF), the effect of cognitive functions by the short scale of mental status (Mini Mental state examination, MMSE), the impact of patients’ functional fitness by the test activities of daily living by Barthel (Activities of Daily Living, ADL).
The results were processed using the statistical software Minitab 16 and were statistically processed on the 95 % confidence level.
Results
The group of geriatric patients with clostridium difficile infection consisted of 148 women (62,98 %) and 87 men (37,02 %), at the age between 65 and 105, of the average age 81,86 ± 7,24. In relation to mortality (p = 0,921), sex was not a statistically significant factor. It was found, that the incidence of the disease increased over the monitored period up to five times. The overall incidence in seniors in the age group of 65-84 years increased six times, and if we compare these two age groups, the increase in incidence in the age group under 65 was only double the initial results (graph 1, 2).
Graph 1. The incidence of Clostridium difficile infection in seniors older than 65 years between January 1, 2008 and December 31, 2013 
Graph 2. The incidence of Clostridium difficile infection in seniors older than 65 years between January 1, 2008 and December 31, 2013, divided by sex and age 
Polymorbidity of seniors in our group was high; each patient over the age of 65 suffered from 13,51±4,34 diseases on average. The proportion of each disease was then statistically considered in relation to morality of CDI affected seniors. There proved to be a significant difference between patients with cerebrovascular disease (p = 0,019) and patients with dementia. The impact of malignant diseases affected the mortality rate marginally (p = 0,057). Up to 64 patients (27,23 %) suffered from pressure ulcers and specifically this factor proved to be statistically important (p = 0,001).
Antibiotic therapy in anamnesis is considered the most significant risk factor. It was found that, from the overall number of 235 seniors over the age of 65 in our group, only 4,68 % did not use any antibiotics and the remaining 95,32 % used one or more antibiotics (graph 3). The difference between the group of the survivor and the deceased based on the number of risk antibiotics was statistically evaluated and it was found that the highest risk comes if seniors use altogether three risk ATBs (p = 0,02). The use of tetracycline (p = 0,001) and third generation cephalosporin (p = 0,02) has proved to be a risk ATB. Further was evaluated the effect of other risk medication, such as the proton pump inhibitors, corticosteroids and cytostatics. However, neither of the groups proved a statistically significant difference: PPI(p = 0,109), corticosteroids (p = 0,329), cytostatics (p = 0,566).
Graph 3. Number of antibiotics used in the anamnesis in one patient over the age of 65 years 
A statistically significant difference was found between the group of the survivor and the deceased when comparing the leukocyte levels in the course of CDI (p = 0,005). While assessing other biochemical and haematological parameters, calcium levels, urea levels and CRP with respect to mortality measured within the course of CDI came out to be significant.
The study proved the MMSE test (p = 0,006), ADL test (p = 0,00),MNA-SF test (p = 0,010) and Charlson comorbidity index(p = 0,043) as a statistically important factor.
The examined group of patients experienced also the development of complications of CDI. Ileus was confirmed in 13 patients, peritonitis developed in 2 patients, and toxic megacolon was recorded in 2 patients. Pseudomebranous colitis was present in 12 patients, 4 of these cases were confirmed by autopsy. Out of 235 seniors over the age of 65 years, 207 patients (88,09 %) experienced their first episode of CDI a 28 patients (11,91 %) were experiencing recurrence of the disease. The most serious complication, the death caused by CDI appeared in 65 cases (27,66 %).
Tab. 1. Test results in patients based on age and sex 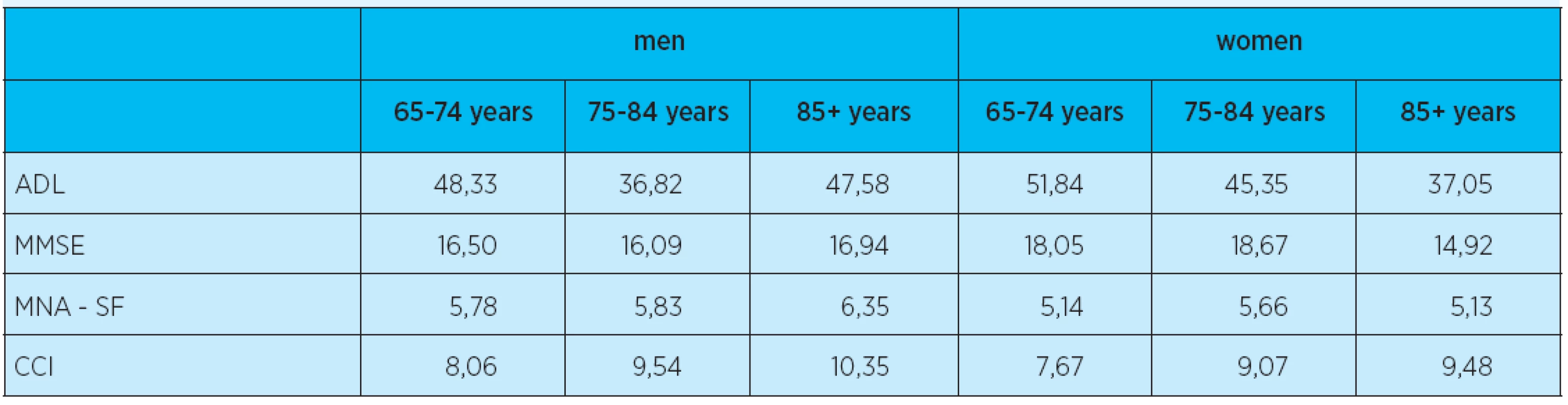
Discussion
Clostridium difficile infection is a serious disease complicating the antibiotic treatment in hospital environments. At the beginning of the 21.century, it is becoming a real threat for patients of predominantly senior age(4). Its incidence has a rising trend. Rising incidence is confirmed by Zilberberg, who in a retrospective study evaluated the occurrence of clostridial infections between the years 2000 and 2005 based on the national register in the United States and found a 117 % increase within the 5year period. The largest proportion of incidence was in the group of the diseased older than 85 years. Within the group 18–44 let was this trend smaller(5).
Our work also suggests an increasing incidence of the disease, wherein most endangered is the group of geriatric patients between 65 and 84 years of age, incidence in this age group increased six times. Statistically was found a significant difference between patients younger than 65 years of age and seniors over the age of 65 (p = 0,024), wherein there was no difference between individual seniors in the age group 65-84 let and over 85 years of age
(p = 0,193). With respect to mortality, sex was not a statistically significant factor (p = 0,921).
Also Miller in his study, which was conducted in Canada in 2005, confirms a more severe course of the infection in geriatric patients. This age predisposes the infected to a twofold increased mortality risk(6).
Cober studied risk factors in seniors over the age of 80. It was a retrospective study conducted in Michigan in 2006 and leucocytosis and ischemic heart disease were detected as independent therapeutic failure factors(7).
Also Raveh in his work confirms antibiotic medication in anamnesis as a significant risk factor (p<0,001), also the use of diuretics is assessed as risk (p <0.005). The average age of his patients was 68 ± 25 years (54 % of which were women)(8).
Out of diseases, a statistically significant difference was confirmed in the vascular disease of the brain and dementia. Other monitored diseases did not have any statistically significant effect on mortality of our group (arterial hypertension (p = 0,261), chronic renal insufficiency(p = 0,062), coronary heart disease (p = 0,257), diabetes mellitus(p = 0,439), chronic heart failures (p = 0,089)).
It was interesting that no statistically significant difference was noted even in the group of seniors with intestinal disease.
In the study, MMSE test, ADL test, MNA-SF test and Charlson comorbidity index were proved to be statistically significant factors. This confirms the appropriateness of testing the geriatric population and underlines the significance of these tests.
Our examined group experienced also the development of CDI complications. The difference between the groups of survivor and deceased patients with the formation of pseudomembranous colitis (p = 0,001) was statistically confirmed, yet the difference was not confirmed in patients with developing ileus (p = 0, 74). Cober in his study of 70 seniors over the age of 80 from the year 2006 confirmed toxic megacolon in3 patients(7). Pépin in his group confirms the development of CDI complications in u 40 % of patients(9).
Mortality of the group was 27, 66. Vaishnavi states 25 % mortality in debilitated geriatric patients(10). Also Zilberberg in his group of 278 critically ill patients confirms the differences in mortality between younger and geriatric patients. In his work he states that the 30day mortality in geriatric patients is by 68 % higher than in the younger group(11).
Conclusion
The increase in incidence of diseases caused by CDI often has lethal consequences for the geriatric population. It is therefor important to consider this significant disease, especially with regard to a typical patient, that is a polymorbid geriatric patient, often suffering from a number of comorbidities, such as the s cerebrovascular disease, malignancy, malnutrition, using antibiotics in the anamnesis. Prevention of the development of this infection is closely associated with the antibiotic use restriction, which should be administered only in cases of high suspicion or confirmed bacterial infection.
K. Bielaková, H. Matějovská-Kubešová,P. Weber, D. Weberová
Clinic of Geriatric Medicine and General Medicine,
The University hospital Brno
Masaryk University
MUDr. Katarína Bielaková
e-mail: bielakovak@seznam.cz
Promovala v roce 2003 na Fakultě všeobecného lékařství Univerzity v Bratislave. V roce 2009 absolvovala Interní kmen.
Druhou atestaci z geriatrie absolvovala v roce 2010. V současnosti pracuje jako asistentka na Klinice interní, geriatrie a praktického lékařství v Brně. Je studentkou postgraduálního studia na Masarykově universitě v Brně. Tématem její disertační práce je Clostridium difficile u geriatrických pacientů.
Zdroje
1. Jones MA, Kuijper EJ, Wilcox M.H. Clostridium difficile: a European perspective. J Infect. 2013; 66(2):115–28.
2. Depestel DD, Aronoff DM. Epidemiology of Clostridium difficile Infection. J Pharm Pract. 2013;26(5): 464–475.
3. Dupont HL, Garey KW. Clostridium difficile infection: an emerging epidemic with more questions than answers. Future Microbiol. 2010; 5(8):1153–6.
4. Khana S, Pardi DS. The growing incidence and severity of Clostridium difficile infection in inpatient and outpatient settings. Expert Rev Gastroenterol Hepatol. 2010; 4(4):409–16
5. Zilberberg MD, Shorr AF, Kollef MH. Increase in adult Clostridium difficile–related hospitalizations and case-fatality rate, United States, 2000–2005. Emerg Infect Dis. 2008; 14(6): 929–931.
6. Miller M, Gravel D, Mulvey M et al. Health care-associated Clostridium difficile infection in Canada: patient age and infecting strain type are highly predictive of severe outcome and mortality. Clin Infect Dis. 2010; 50(2):194–201.
7. Cober ED, Malani PN. Clostridium difficile infection in the „oldest“ old: clinical outcomes in patients aged 80 and older. J Am Geriatr Soc. 2009; 57(4):659–62.
8. Raveh D, Rabinowitz B, Breuer GS, Rudensky B, Yinnon AM. Risk factors for Clostridium difficile toxin-positive nosocomial diarrhoea. Int J Antimicrob Agents. 2006; 28(3):231–7.
9. Pépin J, Valiquette L, Alary ME et al. Clostridium difficile-associated diarrhoea in a region Quebec from 1991 to 2003: a changing pattern of disease severity. CMAJ. 2004; 171(5):466–472.
10. Vaishnavi C. Clinical spectrum & pathogenesis of Clostridium difficile associated diseases. Indian J Med Res. 2010; 31 : 487–99.
11. Zilberberg MD, Shorr AF, Micek ST, Doherty JA, Kollef MH. Clostridium difficile-associated disease and mortality among the elderly critically ill. Crit Care Med. 2009; 37(9):2583–9.
Štítky
Geriatrie a gerontologie Praktické lékařství pro dospělé Protetika
Článek vyšel v časopiseGeriatrie a Gerontologie
Nejčtenější tento týden
2014 Číslo 4- Alergie na antibiotika u žen s infekcemi močových cest − poznatky z průřezové studie z USA
- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
-
Všechny články tohoto čísla
- Editorial
- Evaluating quality of life in patients with dementia
- Quality of life of caregivers – family members of patients with severe dementia
- The reason of stress of senior living in home environment
- Clostridium difficile – a dangerous pathogenfor older patients
- Nutrition in the elderly
- Iron deficiency related anaemia and geriatric medicine
- Normocytic and macrocytic anemia in the elderly
- Dehydration in the old age
- Thyreopathy in elderly patients
- Diabetes mellitus – geriatric syndroms, aims and therapeutic options in the elderly
- Adverse effects of NSAIDs on colopathies in older age
-
Paliative care of chronic heart failure:
When is it the right time?
- Geriatrie a Gerontologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Normocytic and macrocytic anemia in the elderly
- Dehydration in the old age
- Iron deficiency related anaemia and geriatric medicine
- Nutrition in the elderly
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



