-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Enhanced recovery after colorectal surgery in elderly patients
ERAS v kolorektální chirurgii u geriatrických pacientů
Úvod:
Moderní perioperační péče typu ERAS (Enhanced Recovery After Surgery) vede ke snížení frekvence pooperačních komplikací a zkrácení délky hospitalizace. K dosažení těchto výsledků je nezbytná dostatečná adherence k ERAS protokolu. Míra adherence k protokolu, jeho účinnost a bezpečnost není u geriatrických pacientů známa. Cílem studie je zhodnotit adherenci k ERAS protokolu a jeho bezpečnost u geriatrických pacientů indikovaných k plánované střevní resekci.Metoda:
Formou unicentrické prospektivní nerandomizované studie byla hodnocena konsekutivní sestava 111 pacientů, kteří podstoupili plánovaný resekční výkon v oblasti kolorekta bez ohledu na operační přístup (laparoskopicky, konvenčně). Perioperační péče byla u všech pacientů vedena dle ERAS protokolu. K hodnocení byli pacienti rozděleni do dvou věkových skupin (<65 let – 51 pacientů a ≥65 let – 60 pacientů). V každé skupině byla sledována adherence k protokolu, pooperační morbidita a mortalita, parametry perioperační péče, délka hospitalizace a 30denní rehospitalizace.Výsledky:
Celková adherence k protokolu byla 81,5 % u mladších pacientů a 77,5 % u starších pacientů (p=0,03). V ostatních sledovaných parametrech nebyl mezi oběma skupinami prokázán žádný statisticky významný rozdíl. Nikdo nezemřel. Incidence závažných komplikací (stupeň IIIa–IIIb) byla u mladších pacientů 7,8 %, u starších pacientů 6,7 %. Medián pooperační délky hospitalizace byl 9 dní u mladších pacientů a 8 dní u starších pacientů. Frekvence rehospitalizace byla 8 % u mladších pacientů a 3,4 % u starších pacientů.Závěr:
U geriatrických pacientů v elektivní kolorektální chirurgii lze dosáhnout dostatečné adherence k ERAS protokolu bez zvýšení rizika pooperačních komplikací a počtu rehospitalizací ve srovnání s mladšími pacienty. Implementace ERAS protokolu je i u geriatrických pacientů možná.Klíčová slova:
akcelerovaná pooperační rehabilitace − kolorektální chirurgie − perioperační péče − geriatrie
Authors: P. Kocian 1; P. Prikryl 2; M. Bockova 1; J. Hoch 1
Authors place of work: Department of surgery, nd Faculty of medicine Charles University, Motol University Hospital, Prague 1; Department of anaesthesiology and ICM, 2nd Faculty of medicine Charles University, Motol University Hospital, Prague 2
Published in the journal: Rozhl. Chir., 2018, roč. 97, č. 1, s. 27-33.
Category: Původní práce
Summary
Introduction:
The enhanced recovery after surgery (ERAS) protocol decreases postoperative complications and reduces the length of hospital stay. To achieve these results, high adherence to the protocol is necessary. The level of adherence to the protocol, its efficacy and safety are unknown in geriatric patients. The goal of this study was to assess adherence to the ERAS protocol and its safety in elderly patients undergoing elective colorectal surgery.Method:
This was a single-centre, prospective, non-randomized study. One hundred and eleven patients undergoing elective colorectal resections were included in the study, irrespective of the type of surgery (laparoscopic or conventional). Perioperative care followed the ERAS protocol in all patients. The patients were divided into two age groups (<65 years − 51 patients and ≥65 years − 60 patients). Protocol adherence, postoperative morbidity and mortality, perioperative care parameters, length of hospital stay and readmission within 30 days were monitored in each group.Results:
Overall protocol adherence was 81.5% in the younger patients and 77.5% in the elderly patients (p = 0.03). No statistically significant difference was found between the two groups in any of the other parameters analysed. No fatalities occurred in the entire study group. The incidence of serious complications (grade IIIa−IIIb) was 7.8% in the younger patients and 6.7% in the elderly. Median postoperative length of hospital stay was 9 days in the younger patients and 8 days in the elderly patients. Readmission rates were 8% in the younger patients and 3.4% in the elderly patients.Conclusion:
Sufficient adherence to the ERAS protocol can be achieved in geriatric patients undergoing elective colorectal surgery without increasing the risk of postoperative complications and readmissions compared to younger patients. Implementation of the ERAS protocol is feasible in geriatric patients.Key words:
enhanced recovery after surgery − colorectal surgery − perioperative care − geriatricsINTRODUCTION
Modern perioperative care based on the ERAS protocol was introduced to clinical practice of elective colorectal surgery in the nineties of the previous century [1]. The protocol comprises a complex of procedures aimed at reducing perioperative stress, accelerating postoperative recovery and rapid restoration of physiological functions of the body. Adherence to these procedures is associated with reduced postoperative morbidity, shorter length of hospital stay and reduced treatment costs [2,3]. Individual recommendations in the ERAS protocol are supported by a high level of evidence and are guaranteed by the European Society for Enhanced Recovery after Surgery (ERAS Society) and the European Society for Parenteral and Enteral Nutrition (ESPEN) [4,5].
The numbers of geriatric patients have been rising in all fields of surgery due to population ageing. This trend is important particularly in colorectal surgery where the median age of patients with colorectal cancer is 69 years in the Czech Republic, and that of patients in Western Europe is even higher [6,7]. Generally, these patients have a higher perioperative risk due to comorbidities and decreased functional reserve. Multi-stage surgeries, repeated surgeries for complications or inadequate perioperative care may have fatal consequences in these patients. Studies published within the last 5 years have provided evidence that the implementation of the ERAS protocol may improve short-term results of surgical therapy in such patients [8–12]. The level of adherence to the protocol, its efficacy and safety are unknown in geriatric patients.
The purpose of our study was to evaluate adherence to the ERAS protocol and its safety in geriatric patients indicated for elective colorectal resection.
METHOD
This was a single-centre, prospective non-randomized study. All patients who underwent elective colorectal resections between April 2016 and April 2017 were consecutively enrolled in the ERAS protocol pathway. Patients who underwent multivisceral resection or transanal resection and patients who received postoperative care in the department of anaesthesiology were excluded from the study. Of the 147 patients screened, a total of 111 patients met study criteria and were enrolled in the ERAS protocol pathway (Scheme 1). These patients were divided in two age groups (<65 years – 51 patients and ≥65 years – 60 patients). Adherence to the protocol, postoperative morbidity and mortality, perioperative care parameters, length of hospital stay and the 30-day readmission rate were followed in each group. Postoperative complications were assessed using the Clavien-Dindo classification. Postoperative ileus was defined according to the diagnostic criteria outlined in Table 1. Postoperative ileus was classified as being primary in the absence of other intraabdominal complications and secondary if other intraabdominal complications were present.
Scheme 1: Flow chart of patient selection 
Tab. 1. Diagnostic criteria for postoperative ileus 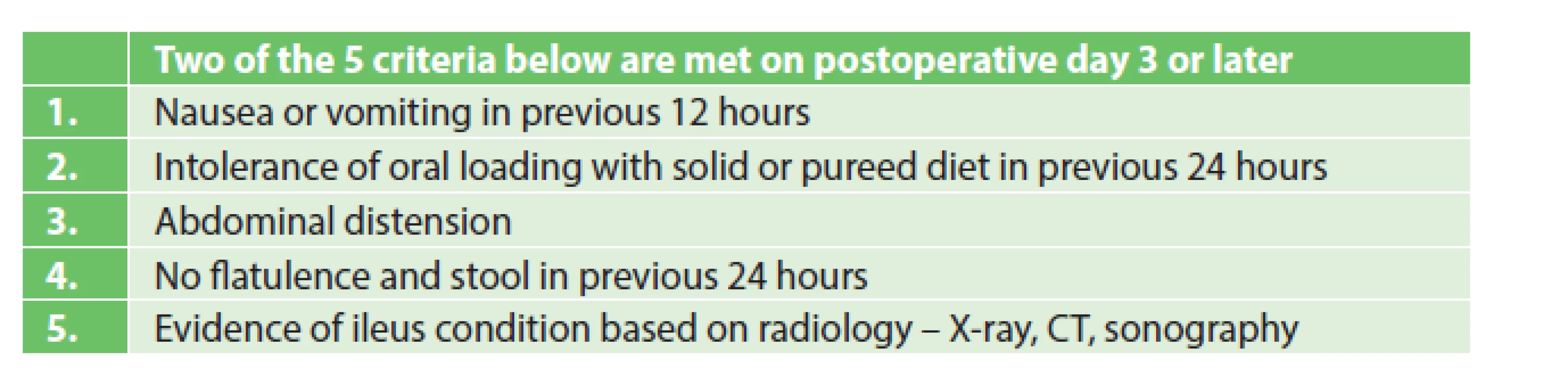
Patient characteristics
In total, 111 patients were evaluated. Men predominated in the entire group (55.9%). The median age of patients at the time of surgery was 65 years, median BMI was 26 kg/m2, and mean ASA score was 2.36. The ratio of laparoscopic and open procedures was 9 : 91%. Colon surgeries were more common than rectal procedures (63.1%). Median procedure duration was 105 minutes and median blood loss was 50 ml.
Patients assigned to the group of ≥65 years had significantly more comorbidities. Significantly more abdominoperineal resections were done in patients aged <65 years (17.7% vs 1.7%), while significantly more right hemicolectomies were done in patients aged ≥65 years (36.6% vs 17.7%). An overview of the patient group and procedures is presented in Table. 2.
Tab. 2. Characteristics of patients and types of surgery 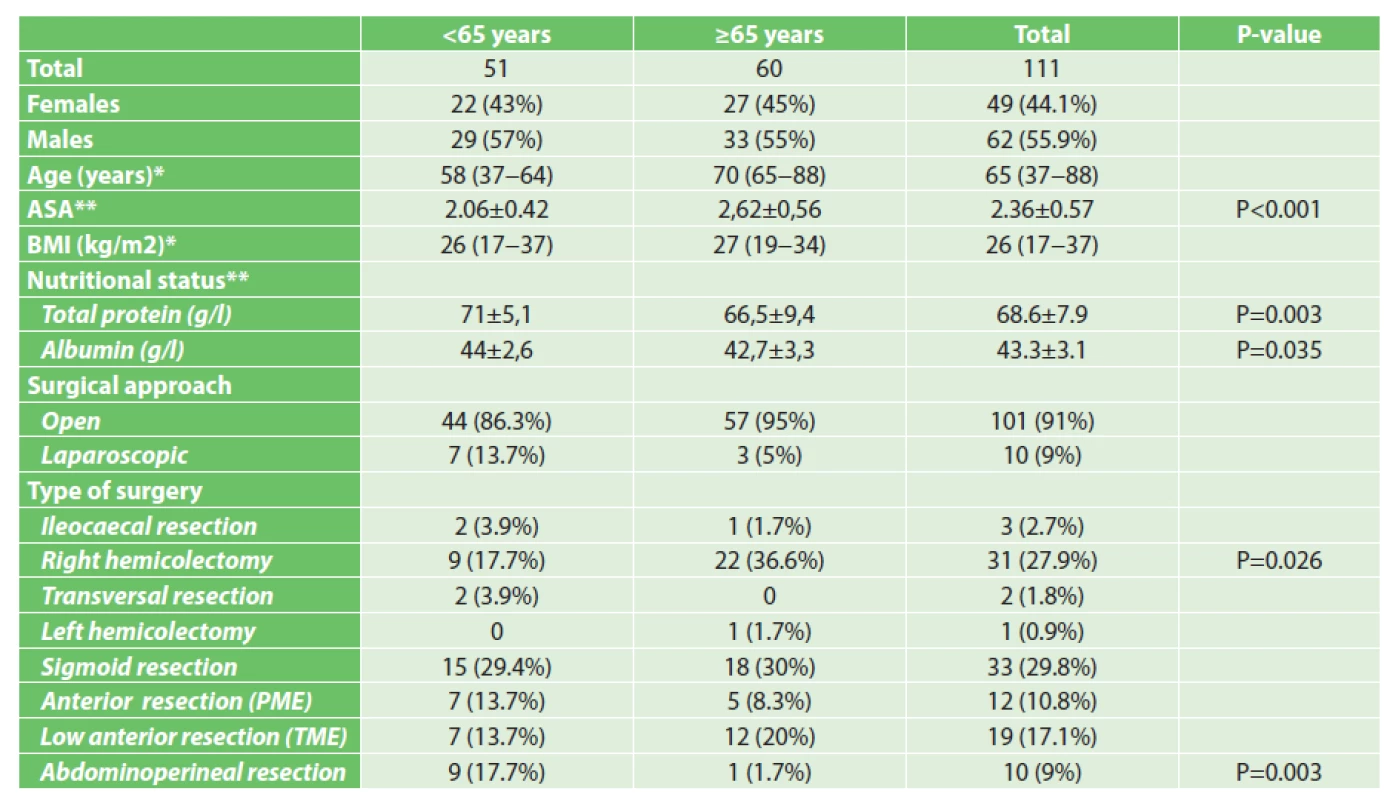
Notes: *Median (range),**Mean (standard deviation), P-value reported only for statistically significant results. ERAS protocol
Implementation of the ERAS protocol included a coordinated approach of all persons involved in perioperative care – the anaesthesiologist, surgeon, the intensive care physician, the nursing personnel and the physiotherapist. We developed and used a clinical protocol that respects the guidelines of European societies (ERAS Society, ESPEN). This protocol included 17 points (Table 3). Overall adherence to the protocol was assessed in each patient according to the number of points achieved. Adherence to the individual points of the protocol was assessed in the entire patient cohort. Nutritional status was assessed by the indicating surgeon based on nutritional screening or was included in preoperative assessments. BMI, information about weight loss and about limited oral intake, as well as laboratory assessments of total proteins and albumin were included in the screening assessments. If a malnutrition risk was identified, a detailed examination of its severity was indicated with subsequent intervention. Mechanical bowel preparation was done in all patients indicated for resection in the area of the rectum, of the left colon, and also if perioperative colonoscopy was indicated.
Tab. 3. ERAS protocol – investigated parameters 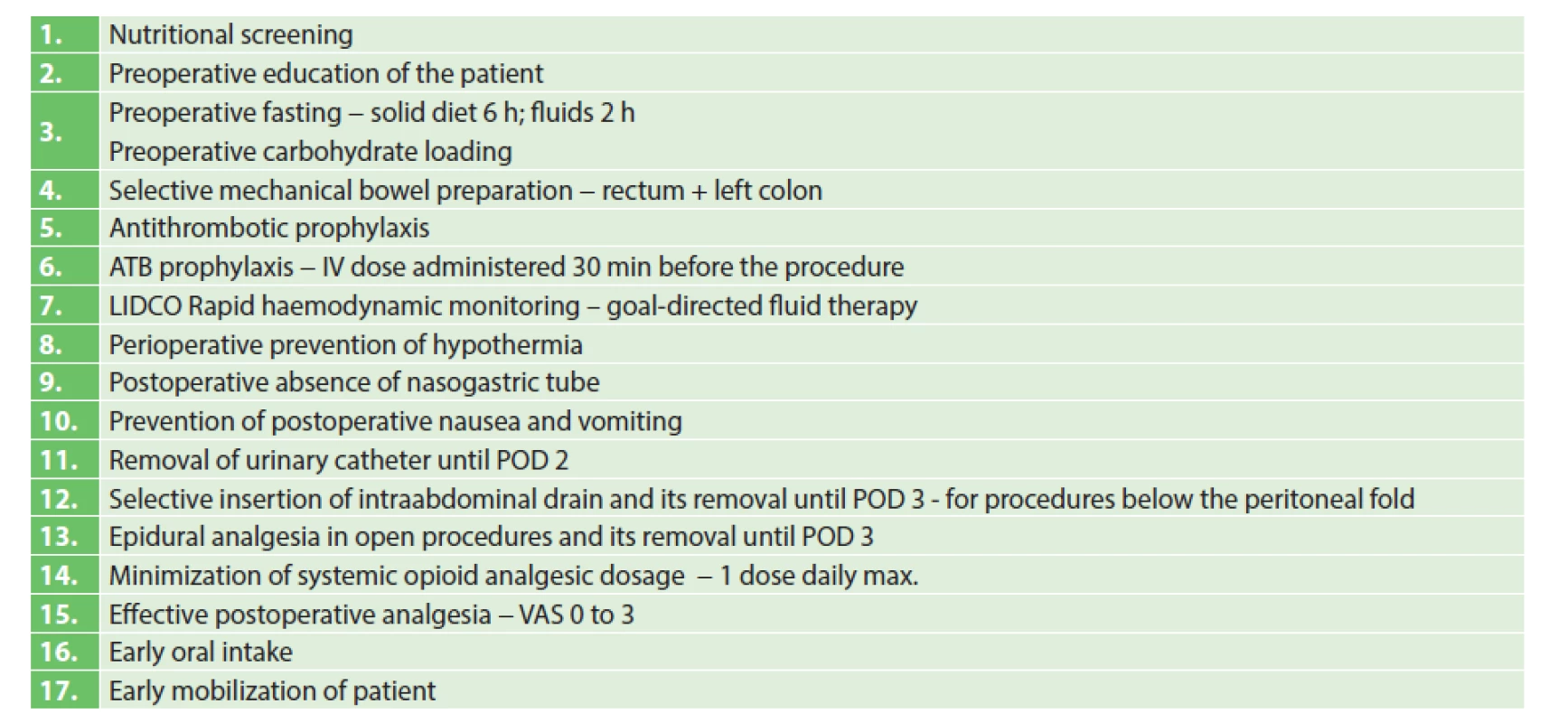
Statistical analysis
Data was analyzed using Statistica 10.0. Contingency tables and the Pearson’s chi-squared test were used for categorical variables. Continuous variables were analysed using the t-test; given a high variability of the variance, blood loss differences were assessed using the Mann-Whitney U test. A difference at the p-level <0.05 was considered as statistically significant.
RESULTS
Adherence to the protocol
The level of adherence to individual ERAS protocol points was comparable in both age groups. A significant difference was found only for preoperative education, administration of carbohydrates and LIDCO Rapid haemodynamic monitoring. The lowest adherence was found for early removal of invasive devices – the permanent urinary catheter, intraabdominal drain, epidural catheter – and for early postoperative realimentation. These points of the protocol were not followed equally in both age categories. Overall mean adherence to the ERAS protocol was 81.5% in patients below 65 years of age, 77.5% in those over 65 years of age, and 79.3% in the entire set. A detailed analysis is presented in Table 4. A risk of malnutrition was found in two geriatric patients based on nutritional screening and nutritional support by sipping was indicated. The sipping was initiated 10 days before surgery in both cases. Mechanical bowel preparation was done in 75.7% of patients in the entire cohort.
Tab. 4. Adherence to the ERAS protocol 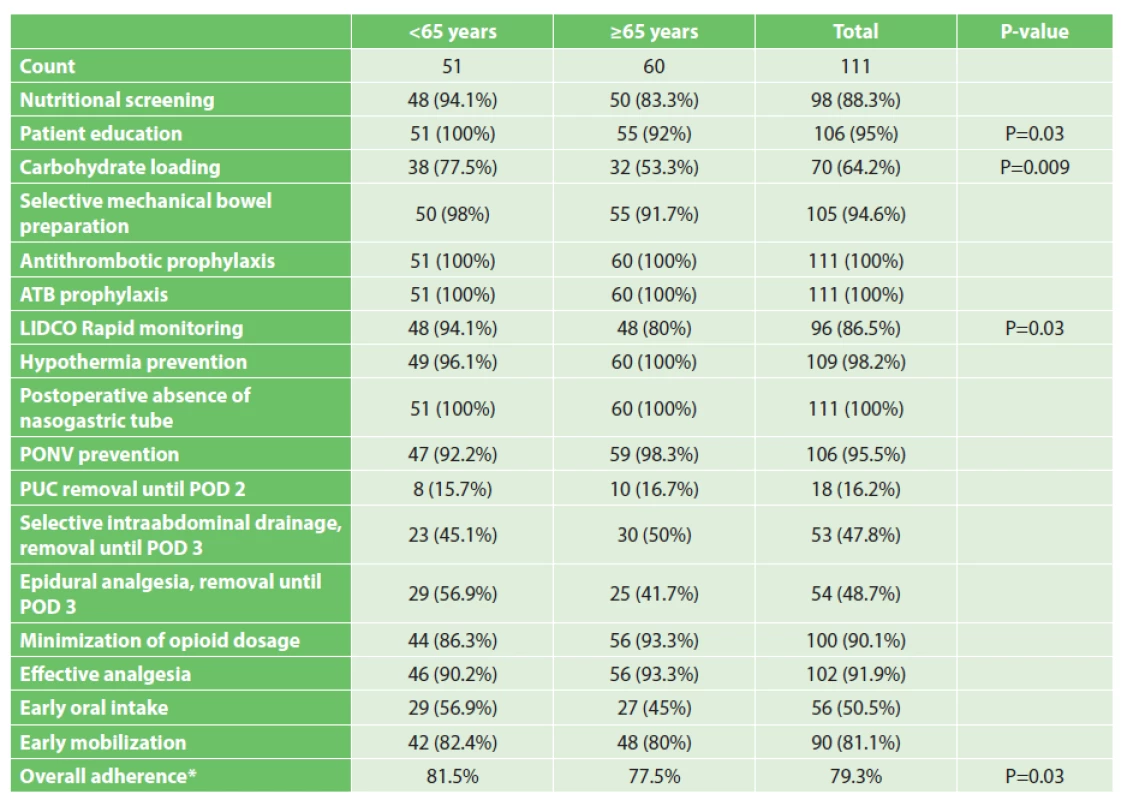
Notes: *Mean, P-value reported only for statistically significant differences. Perioperative care parameters
The followed parameters are presented in Table 5. Goal-directed fluid therapy using non-invasive LIDCO Rapid monitoring during the procedure and in the early postoperative period was implemented in the total of 86.5% of patients. Median intravenous fluid intake on the day of surgery was 3200 ml in patients below 65 years of age, 2950 ml in patients over 65 years of age, and 2960 ml in the entire cohort. Multimodal postoperative analgesia resulted in a reduction of the overall consumption of opioids. Almost 60% of patients did not need their systemic application throughout the postoperative period. More than 80% of patients including seniors were successfully verticalized on the first postoperative day. The frequency of postoperative nausea and vomiting (PONV) was 3.6% in the entire cohort. However, PONV was monitored only in 49.5% of the patients, and its actual frequency can thus be expected to be higher. The tolerance of dietary loading, tolerating normal per oral intake of solids foods by fourth postoperative day, was about 50% in both age groups. No statistically significant difference was observed between the groups for any of the followed parameters.
Tab. 5. Parameters of perioperative care 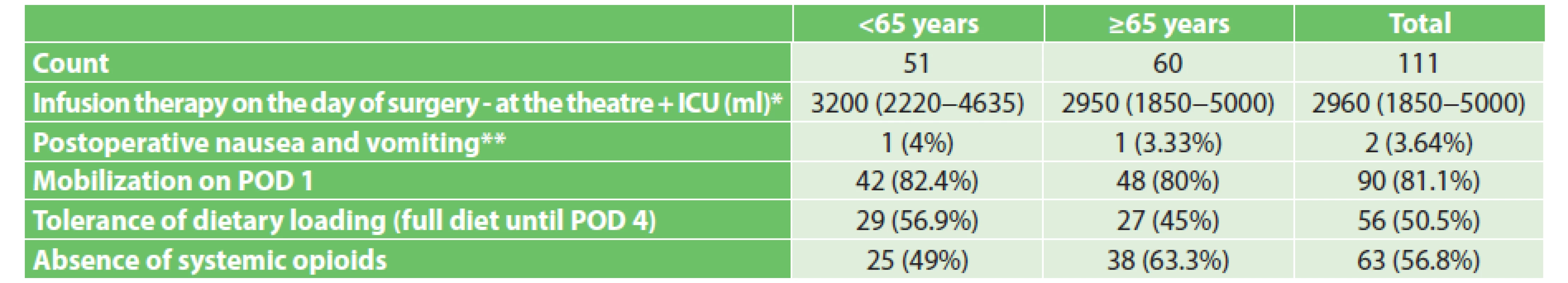
Notes: *Median (range), **Monitored in the total of 55 patients, no statistically significant difference was shown – P-value not reported. Postoperative morbidity and mortality
No patients died. No statistically significant differences were found for the incidence and severity of postoperative complications between the groups of patients below and over 65 years of age. The incidence of serious complications – grades IIIa and IIIb – was 7.2% in the entire patient cohort. Anastomotic leak was diagnosed in 2 patients. Its incidence in the entire patient cohort (in rectal resection) was 6.4%. Surgical site complications occurred in 31.5% of patients; of these, seromas and haematomas represented 18%. A postoperative ileus occurred in 23.4% of patients; of these, 2.7% had a secondary ileus due to an intraabdominal complication. Details of the postoperative complications are presented in Table 6.
Tab. 6. Postoperative complications 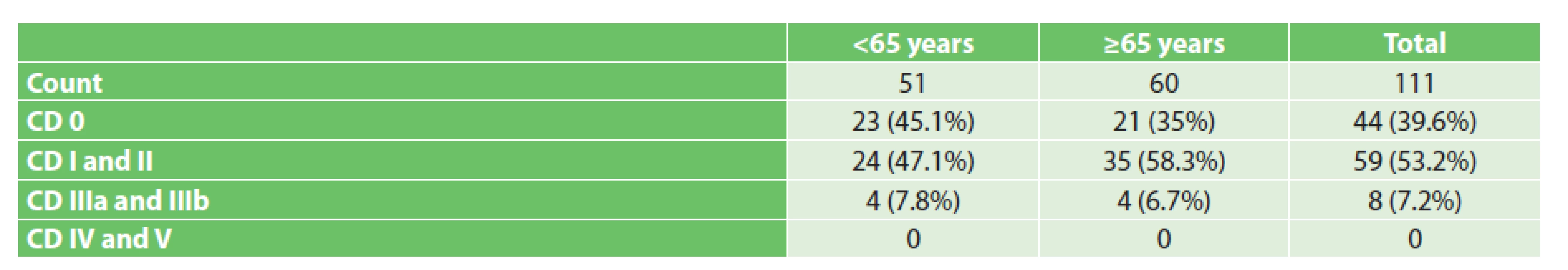
Notes: No statistically significant difference was shown – P-value not reported. Length of hospital stay
Median length of hospital stay was 9 days for patients below 65 years of age, 8 days for patients over 65 years of age, and 8 days for the entire patient cohort. Median length of stay at the ICU was 3 days in patients below 65 years of age, 4 days in patients over 65 years of age, and 4 days in the entire patient cohort. Median length of stay at the ward was 5 days for both age groups. The differences in the lengths of hospital stay were not statistically significant (Table 7). Prolonged length of hospital stay, defined as being more than 8 days, was due to grade I and II postoperative complications (63.6%), social reasons (21.8%) and grades IIIa and IIIb complications (14.6%). The reasons for prolonged hospital stay are shown in Graph 1.
Tab. 7. Postoperative length of hospital stay 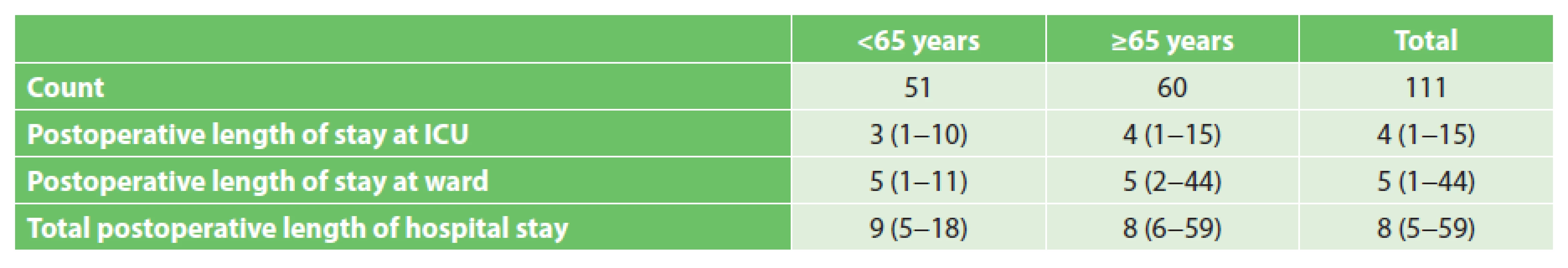
Notes: Median (range), no statistically significant difference was shown – P-value not reported. Graph 1. Reasons for delaying discharge 
Legend: ED – estimated date of discharge (corresponds to median total postoperative length of stay in the entire set; 8 days) 30-day readmission rates
Only one patient was lost for follow-up in the group of older patients. The readmission rate was evaluated for the total of 110 patients. In total, 6 patients were readmitted; of these, 4 received conservative therapy and 2 underwent surgery. The readmission rate was 8% in patients below 65 years of age, 3.4% in patients over 65 years of age, and 5.5% in the entire set. The differences were not statistically significant.
DISCUSSION
The ERAS protocol in elective colorectal procedures reduces the frequency of postoperative complications, shortens the length of hospital stay, and enhances patient comfort [2,3]. High adherence to the ERAS protocol both on part of the healthcare professionals and of the patients is necessary to achieve these results [13]. Cognitive disorders, malnutrition, insufficient continence, poor mobility, conditions of delirium or depression are associated with advanced age [14]. Given that it may be problematic to achieve high adherence in advanced age, geriatric patients were primarily not enrolled in the ERAS protocol pathway for many years. However, as indicated by recent studies, age is not a decisive factor, and adherence of the ERAS protocol by geriatric patents is comparable to that in younger patients [9,10]. It is important to assess the actual condition of the geriatric patient and his or her functional reserves as these may not always correlate with the calendar age and the presence of comorbidities. This opinion is in harmony with the results of our prospective study where an almost 80% adherence to the protocol was achieved even in geriatric patients with a higher prevalence of comorbidities. The lowest adherence was seen, equally in both age groups, in the removal of invasive devices and in early postoperative realimentation. Not the age, scope of the surgery or complications, but apparently the persisting tradition and a lack of trust in new procedures were the main reason for failing to follow these parts of the protocol. This approach reflects the situation in the Czech Republic where, based on the results of a national survey of 2013, the ERAS protocol is not followed at most departments of surgery [15].
Optimization of perioperative fluid intake is one of important aspects of the ERAS protocol. As shown by the results of a Danish multicentre randomized study, perioperative volume restriction in elective colorectal surgery leads to reduced postoperative morbidity [16]. Restrictive regimens are in full synergy with the other procedures used in ERAS. Patients are not dehydrated before surgery as their oral fluid intake is not restricted, and most patients do not complete mechanical bowel preparation. It still needs to be answered what amount of intravenous fluids on the day of surgery is optimal for the patients. The authors of a Scandinavian study report median intravenous fluid intake on the day of surgery as 3800 ml in patients below 65 years of age, 3900 ml in patients aged 66–79 years, and 4800 ml in patients over 80 years of age [9]. The group of authors of a Polish study support a rather more restrictive regimen, reporting mean intravenous fluid intake on the day of surgery as 2500 ml [11]. Before ERAS implementation, retrospective analysis was done at our department to evaluate the effect of perioperative volume restriction on reduced postoperative morbidity in patients undergoing rectal resection. Median intravenous fluid intake on the day of surgery was 4450 ml in the restrictive group, 5400 ml in the liberal group, and 5000 ml in the entire group. Fluid restriction was demonstrated to be associated with lower postoperative morbidity [17]. In the current prospective study goal-directed fluid therapy resulted in a significant reduction of intravenous fluid intake; median intravenous fluid intake on the day of surgery of 3200 ml in patients below 65 years of age, and 2950 ml in patients over 65 years of age.
Major indicators of successful ERAS implementation include postoperative morbidity and mortality, the length of hospital stay, and readmission frequency. No statistically significant difference was shown upon evaluation of these parameters in our prospective study.
No patient died in the entire patient cohort. The incidence of serious complications was 7.8% in patients below 65 years of age and 6.7% in those over 65 years of age. This finding agrees with the cited studies [9−11]. The frequency of other than serious complications in geriatric patients has been reported as 24.5–42.1% in the literature [9, 10]. The higher incidence of these complications in our paitents seems to follow from our very careful evaluation. Any deviation from the normal postoperative course was identified as a complication – e.g. even ionic dysbalance based on laboratory assessments.
Length of hospital stay was comparable in both age groups (9 days vs 8 days). The shorter length of hospital stay in older patients with a higher prevalence of comorbidities was probably due to the difference in the number and severity of the surgery between both groups. Significantly more abdominoperineal resections were performed in the younger patients (17.7% vs 1.7%), while the older patients had significantly more right hemicolectomies (36.6% vs 17.7%). These conclusions are in agreement with the results of recently published studies that did show any significant difference in the length of hospital stay between older and younger patients [9,11,18−23]. The postoperative length of hospital stay in elective colorectal procedures following the ERAS protocol has been reported between 4 and 8 days in geriatric patients based on the literature [9−11,19,21]. The higher length of hospital stay in our prospective study is conditioned by a number of factors. In particular, they include the inclusion criteria for patient enrolment in the ERAS protocol. Compared to the above-cited studies, patients with ASA score 4, patients requiring repeated surgery within 72 hours from their procedure and patients undergoing palliative intestinal resection were not excluded from the ERAS protocol. The relative high rate of rectal procedures (almost 40%) and a lower rate of laparoscopic procedures (9%) are additional factors. The prolonged length of hospital stay was also due to social reasons (Graph 1). Despite having complied with the discharge criteria, in many cases elderly patients are not able to sufficiently manage their situation alone at home and depend on cooperation of the family or home care after their discharge. Also, our results are influenced by the fact that compared to the situation in other countries, the pressure on reducing bed-days is lower in the Czech Republic.
The 30-day readmission rate was comparable in both age groups. A readmission rate of 6.4–25% in geriatric patients enrolled in the ERAS protocol pathway has been reported by recent studies [9,10,21]. The readmission rate of patients over 65 years of age was 3.4% in our patient cohort.
We are aware that our study is limited by its non-randomized design, the relatively small sample of enrolled patients and by the absence of a non-ERAS control group.
CONCLUSION
High adherence to ERAS can be achieved in geriatric patients undergoing elective colorectal surgery without any increased risk of postoperative complications or the readmission rate compared to younger patients. Calendar age is not a decisive factor for high adherence. It is important to assess the actual condition of the senior and his or her functional reserves that need not always correlate with the calendar age and the presence of comorbidities. Close cooperation of all healthcare professionals involved in perioperative care is necessary, while nursing staff plays a major role. ERAS implementation is feasible in geriatric patients.
Abbreviations
- ASA – American Society of Anesthesiologists
- BMI – Body mass index
- CD – Clavien-Dindo
- ERAS – Enhanced Recovery After Surgery
- ERAS Society – Enhanced Recovery After Surgery Society
- ESPEN – European Society for Parenteral and Enteral Nutrition
- ICU – Intensive care unit
- LIDCO – Lithium dilution cardiac output
- PME – Partial mesorectal excision
- PUC – Permanent urinary catheter
- POD – Postoperative day
- PONV – Postoperative nausea and vomiting
- TME – Total mesorectal excision
- TEM – Transanal endoscopic microsurgery
- VAS – Visual analogue scale
Conflict of interests
The authors declare no conflict of interest in connection with this article; the authors also declare that this paper has not been published in any other journal.
MUDr. Petr Kocián, Ph.D.
Department of surgery
2nd Faculty of medicine Charles University
Motol University Hospital
V Úvalu 84
150 06 Praha 5
e-mail: petr.kocian@fnmotol.cz
Zdroje
1. Kehlet H. Organizing postoperative accelerated recovery programs. Reg Anesth 1996;21 : 149−51.
2. Adamina M, Kehlet H, Tomlinson GA, et al. Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery 2011;149 : 830−40.
3. Varadhan KK, Neal KR, Dejong CH, et al. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr 2010;29 : 434−40.
4. Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 2012;31 : 783−800.
5. Nygren J, Thacker J, Carli F, et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Clin Nutr 2012;31 : 80−16.
6. Hoch J, Blaha M, Maluskova D. [Colorectal cancer in the elderly] Czech, Rozhl Chir 2016;95 : 13−8.
7. Soreide K, Wijnhoven BP. Surgery for an ageing population. Br J Surg 2016;103 : 7−9.
8. Bagnall NM, Malietzis G, Kennedy RH, et al. A systematic review of enhanced recovery care after colorectal surgery in elderly patients. Colorectal Dis 2014;16 : 947−56.
9. Forsmo HM, Erichsen C, Rasdal A, et al. Enhanced recovery after colorectal surgery (ERAS) in elderly patients is feasible and achieves similar results as in younger patients. Gerontol Geriatr Med 2017;3 : 1−8.
10. Gonzalez-Ayora S, Pastor C, Guadalajara H, et al. Enhanced recovery care after colorectal surgery in elderly patients. Compliance and outcomes of a multicenter study from the Spanish working group on ERAS. Int J Colorectal Dis 2016;31 : 1625−31.
11. Kisialeuski M, Pedziwiatr M, Matlok M, et al. Enhanced recovery after colorectal surgery in elderly patients. Wideochir Inne Tech Maloinwazyjne 2015;10 : 30−6.
12. Pirrera B, Lucchi A, Gabbianelli C, et al. E.R.A.S. pathway in colorectal surgery in elderly: Our experience. Int J Surg 2017;43 : 101−6.
13. Gustafsson UO, Hausel J, Thorell A, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 2011;146 : 571–7.
14. Audisio RA. Tailoring surgery to elderly patients with cancer. Br J Surg 2016;103 : 10–1.
15. Ryska O, Serclova Z, Antos F. [Compliance with the procedures of modern perioperative care (Enhanced Recovery After Surgery) at surgery departments in the Czech Republic – results of a national survey] Czech, Rozhl Chir 2013;92 : 435−42.
16. Brandstrup B, Tonnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 2003;238 : 641−8.
17. Kocian P, Neumann J, Majtan P, et al. [Fluid therapy and surgical outcomes after low anterior resection] Czech, Rozhl Chir 2014;93 : 463−7.
18. Baek SJ, Kim SH, Kim SY, et al. The safety of a fast-track program after laparoscopic colorectal surgery is comparable in older patients as in younger patients. Surg Endosc 2013;27 : 1225−32.
19. Kahokehr AA, Sammour T, Sahakian V, et al. Influences on length of stay in an enhanced recovery programme after colonic surgery. Colorectal Dis 2011;13 : 594−9.
20. Keller DS, Lawrence JK, Nobel T, et al. Optimizing cost and short-term outcomes for elderly patients in laparoscopic colonic surgery. Surg Endosc 2013;27 : 4463−8.
21. Pawa N, Cathcart PL, Arulampalam TH, et al. Enhanced recovery program following colorectal resection in the elderly patient. World J Surg 2012;36 : 415−23.
22. Verheijen PM, Vd Ven AW, Davids PH, et al. Feasibility of enhanced recovery programme in various patient groups. Int J Colorectal Dis 2012;27 : 507−11.
23. Walter CJ, Watson JT, Pullan RD, et al. Enhanced recovery in major colorectal surgery: safety and efficacy in an unselected surgical population at a UK district general hospital. Surgeon 2011;9 : 259−64.
Štítky
Chirurgie všeobecná Ortopedie Urgentní medicína
Článek Zemřel docent Zdeněk SlezákČlánek Chirurgie ve vyšším věku
Článek vyšel v časopiseRozhledy v chirurgii
Nejčtenější tento týden
2018 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
-
Všechny články tohoto čísla
- Breast cancer in elderly patients over 70 years of age
- Plicní lobektomie pro bronchogenní karcinom u osmdesátiletých pacientů
- Zemřel docent Zdeněk Slezák
- Je laparoskopická kolorektální chirurgie bezpečná i u starších pacientů?
- ERAS v kolorektální chirurgii u geriatrických pacientů
- Chirurgie ve vyšším věku
- Pankreatoduodenektomie pro karcinom pankreatu u seniorů – zkušenosti jednoho centra
- Tyreoidektomie u seniorů - má specifika, limity, kontraindikace?
- Atlas vaskulárnych aneuryziem
- Vývoj názorů na léčení pankreatické nekrózy v posledních 50 letech
- Rozhledy v chirurgii na prahu 98. ročníku – tři novinky
- Sympozium 3. Střešovické videokazuistiky z laparoskopie
- Plastická chirurgie pokročilého věku
- Rozhledy v chirurgii
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Breast cancer in elderly patients over 70 years of age
- ERAS v kolorektální chirurgii u geriatrických pacientů
- Pankreatoduodenektomie pro karcinom pankreatu u seniorů – zkušenosti jednoho centra
- Chirurgie ve vyšším věku
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



