-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaIn-hospital therapeutic hypothermia in cardiac arrest survivors: Growing implementation in the Czech Republic (PRE-COOL 2: Hospital Survey 2008)
Nemocniční používání terapeutické mírné hypotermie u pacientů přežívajících po srdeční zástavě – nárůst v České republice (PRE-COOL 2: Hospital Survey 2008)
Cíl studie:
Analyzovat vývoj používání terapeutické mírné hypotermie (TH) v České republice, posoudit vliv aktuálních doporučení pro kardiopulmonální resuscitaci (KPR) na implementaci metody a analyzovat případné příčiny jejího nedostatečného používání.Typ studie:
Dotazníkový národní průzkum.Typ pracoviště:
Územní středisko záchranné služby, Klinika anesteziologie, resuscitace a intenzivní medicíny.Materiál a metoda:
Po kompletaci seznamu všech nechirurgických jednotek intenzivní péče (JIP) v České republice byli jejich vedoucí lékaři nebo přednostové příslušného oddělení v prosinci 2006 (S2006) a v říjnu 2008 (S2008) obesláni strukturovaným dotazníkem.Výsledky:
Srovnatelný počet JIP byl zařazen do studie v obou průzkumech (S2006: n = 468, S2008: n = 487). Návratnost dotazníků byla srovnatelná (S2006 : 39,7%, S2008 : 41,5%, p=0,617). Na pracovištích poskytujících časnou poresuscitační péči byl zjištěn nárůst počtu oddělení používajících TH (S2006 : 50,7%, S2008 : 63,8%, p = 0,037). Podíl nemocných léčených TH ze všech hospitalizovaných pacientů po KPR na jednotlivých JIP se nezměnil (S2006 : 53,3 ± 33,5 %, S2008 : 57,3 ± 33,2 %, p = 0,317). Nejsilnějším prediktorem používání TH bylo ošetřování > 10 nemocných po KPR ročně (OR 11,66, 95% CI 3,9–39,5, p < 0,001). Nejčastější příčinou nepoužívání TH v roce 2008 byl nedostatek finančních prostředků (54,9 %). Největší přírůstek JIP nově používajících metodu nastal v roce 2007, převážně na základě doporučení European Resuscitation Council pro KPR 2005.Závěr:
V nemocnicích České republiky došlo k nárůstu implementace TH u nemocných po náhlé zástavě oběhu mezi roky 2006 a 2008. Nárůst byl motivován zejména platnými doporučeními pro KPR.Klíčová slova:
terapeutická mírná hypotermie – implementace – náhlá zástava oběhu – kardiopulmonální resuscitace – intenzivní medicína
Authors: Škulec Roman Ihash2 1,4 2,4; Šeblová Jana 3; Knor Jiří 3; Dostál Pavel 4; Černý Vladimír 4
Authors place of work: Územní středisko záchranné služby Středočeského kraje, Beroun 1; Letecká záchranná služba, Hradec Králové 2; Územní středisko záchranné služby Středočeského kraje, Kladno 3; KARIM, LF UK a FN Hradec Králové 4
Published in the journal: Anest. intenziv. Med., 21, 2010, č. 6, s. 317-323
Category: Resuscitace - Původní práce
Summary
Objective:
To compare the extent of therapeutic mild hypothermia (TH) usage in cardiac arrest survivors in the Czech Republic during the last years, to assess the impact of the guidelines on TH usage and to analyze the reasons of its non-use.Design:
National questionnaire survey.Setting:
Emergency Medical Service, Department of Anaesthesiology and Intensive Care Medicine.Materials and methods:
After completing a list of all non-surgical intensive care units (ICU) in the Czech Republic, their lead physicians were sent a structured questionnaire in December 2006 (S2006) and October 2008 (S2008).Results:
Total 39.7% and 41.5% (p = 0.617) ICUs out of a comparable number of ICUs surveyed (S2006: n = 468, S2008: n = 487) responded. We detected an increase in TH usage among the ICUs in the Czech Republic that provide post-cardiac arrest care from 50.7% in S2006 to 63.8% in S2008 (p = 0.037). The proportion of patients treated with TH out of all admitted cardiac arrest patients was similar (S2006 : 53.3 ± 33.5%, S2008 : 57.3 ± 33.2%, p = 0.317). The most powerful predictor of TH implementation in an ICU was having more than ten admitted cardiac arrest patients per year (OR 11.66, 95% CI 3.9–39.5, p < 0.001). The most frequent reason for TH non-use as identified in S2008 was lack of funds (54.9%). A maximum incremental increase of the number of ICUs using TH occurred in 2007, predominantly on the basis of the 2005 European Resuscitation Council Guidelines.Conclusion:
A significant increase of in-hospital TH implementation in cardiac arrest survivors in the Czech Republic was observed during the last years. It was especially promoted by the recent guidelines for cardiopulmonary resuscitation.Keywords:
therapeutic mild hypothermia – implementation – cardiac arrest – cardiopulmonary resuscitation – intensive careIntroduction
Recently, therapeutic mild hypothermia (TH) has become a routine part of early post-cardiac arrest care in comatose cardiac arrest survivors [1–3]. Throughout the world, in-hospital TH utilisation has varied from 8 to 95% in different countries from 2003 until now [4, 5]. In the Czech Republic, it was used by 47% of the intensive care units (ICU) that cared for cardiac arrest patients at the end of 2006 [6]. Since this time, there has been a lot of other evidence published about the effectivness of this procedure. Therefore, we decided to reassess the position of TH in the Czech Republic, to analyze the extent of TH usage in cardiac arrest survivors, to assess the reasons for non-use, to evaluate the compliance to guidelines and to compare the recent data with the results of the last survey.
Material and methods
Selection of participants, study design, questionnaire
The evaluation was realized as the second project of working group PRE-COOL (Pre-hospital Cooling in Cardiac Arrest Patients) and termed by an acronym PRE-COOL 2: Hospital Survey 2008. It was performed in accordance with the Helsinki declaration. No patients data has been collected. Therefore an ethical committee agreement was not required. In December 2006, we constructed the directory of all intensive care units (ICUs) in the Czech republic irrespective of its type by means of the hospital register in the Czech Republic, public internet sources and telephone contacts. The structured questionnaire was addressed to the head physician of every ICU. A total of 600 ICUs were summonsed by the questionnaire during the period of 3 months by regular mail (The 1st survey 2006, S2006). Responses were returned via post-mail, email or fax. In 2008, the ICU directory was updated and the questionnaire was extended. After exclusion of the ICUs specialized in general surgery, obstetrics and gynecology and orthopedy, a total of 487 ICUs were summonsed in October 2008 by the same pattern as in the previous survey (The 2nd Survey 2008, S2008). Both surveys were performed anonymously. Responses were collected and statistically processed. The subject of the analysis were the providers of early post-cardiac arrest care. To enable comparison of the surveys, the results of S2006 were retrospectively reclassified into the same spectrum of summonsed ICUs as in S2008.
Questionnaire
The S2006 questionnaire was composed of 23 and S2008 of 44 structured items, respectively. The items were of dichotomous and polytomous closed type and of semi-closed type of the questiones. The first part of the questionnaire was focused on the demographic variables (type of a hospital and ICU, number of beds in ICU, instrumentation available for organ support, access to cathetrization laboratory). This was followed by items regarding the use of TH, frequency of its usage and impact of guidelines on local method implementation. The third part particularly analyzed the methodology of the cooling process and reasons of TH non-use.
Statistical analysis
Mean values ± standard deviation (SD) or percentages were calculated for all variables. Statistical significancy was assessed by χ2 test, Students t-test or Fischer exact test, with reference to the type of parameters. Independent predictors were evaluated by multivariate logistic regression analysis. Data was analyzed using JMP 3.2 statistical software (SAS Institute, Cary, NC, USA). A p value of < 0.05 was considered statistically significant.
Results
Response-rate, demography
All returned questionnaires were evaluated. Out of the comparable number of the summonsed ICUs (S2006: n = 468, S2008: n = 487) responded 39.7% (n = 186) and 41.5% (n = 202), respectively (p = 0.617). From the responding ICUs, 73.1% in S2006 (n = 136) and 69,8% in S2008 (n = 141) provided early post-cardiac arrest care (p = 0.291). Those ICUs were the subject of further evaluation. From the group of post resuscitation care providers, the majority of the responding ICUs were from non-university hospitals (S2006 : 67.6%, S2008 : 72.3%, p = 0.470), the rest were the university facilities. The average number of beds per ICU was 8.3 ± 3.7 in S2006 and 7.9 ± 4.2 in S2008 (p = 0.402). More than 20 cardiac arrest patients a year admitted 25.7% in S2006 and 31.2% in S2008 (p = 0.378) and ≤ 10 patients a year 46.3 % and 41.1%, respectively (p = 0.452). While more than 11 cardiac arrest patients a year admitted as much as 85.5% of Departments of Anaesthesiology and Intensive Care and 82.3% of Coronary Care Units in S2008, this rate reached only 23.1% of Internal Medicine ICUs (p < 0.001).
Usage of therapeutic mild hypothermia
In the group of all providers of early post-cardiac arrest care, TH was used by 50,7% (n = 68) in S2006 and by 63.8% (n = 90) of them at the time of S2008 (p = 0.037). Distribution of TH implementation depending on the type of ICU and its changes in time is shown in table 1. While significant increase was observed in the Depts. of Anaesthesiology and Intensive Care, implementation in the Coronary care units was unchanged and in the Internal Medicine ICUs TH acceptance remained low. Due to the small number of the responders, it was not possible to reliably compare TH usage in the other types of ICU, like pediatric, neurologic etc.
Tab. 1. Comparison of TH usage in different types of ICUs in 2006 and 2008 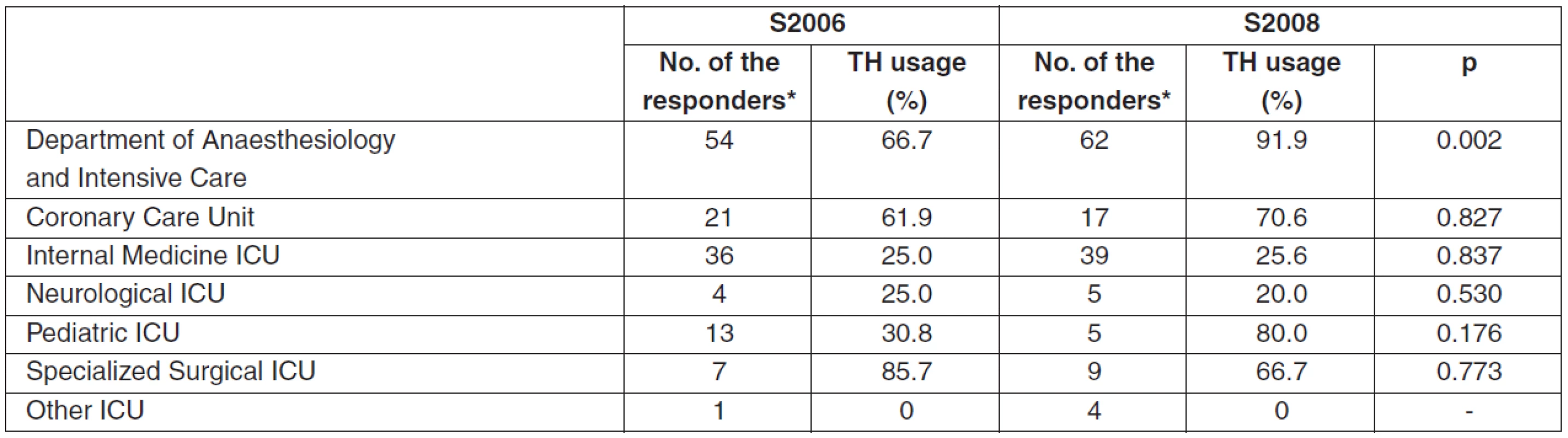
TH – therapeutic mild hypothermia, ICU – intensive care unit *Number of the responding providers of early postresuscitation intensive care. The most powerfull demographic independent positive predictor of TH usage was a fact of having more than ten admitted cardiac arrest patients per year (OR 11.66, 95% CI 3.9–39.5, p < 0.001). The other significant predictors were Dept. of Anaesthesiology and Intensive Care as the type of the ICU (OR 14.0, 95% CI 3.5–66.2, p < 0.001), and university hospital facility (OR 5.43, 95% CI 1.1–31.4, p = 0.045).
The proportion of cardiac arrest patients treated with TH of all admitted cardiac arrest patients in all centers has remained in both surveys the same (S2006 : 53.3 ± 33.5%, S2008 : 57.3 ± 33.2%, p = 0.317). Table 2 shows the proportion of cardiac arrest survivors treated with TH and the most responding types of ICU in both surveys. The fraction of centers applying TH in more than 75% of all admited cardiac arrest patients has been comparable (S2006 : 34.7%, S2008 : 31.1%, p = 0.602). In S2008, this active cooling approach was significantly more frequent in university facilities than in non-university hospitals (46.4 vs. 23.7%, p = 0.032). The responders who implemented TH in 2005 or earlier cooled higher proportion of cardiac arrest patiens than those who started with the method later (74.9 vs. 51.5%, p = 0.004).
Tab. 2. Comparison of the proportion of patients treated with TH out of all admitted cardiac arrest patients in both surveys 
Reasons of non-use
In S2008, the proportion of TH non-using responding providers of early post-cardiac arrest support was lower than in S2006 (36.5 vs. 49.3%, p = 0.044). The number of non-users who had not heard about TH treatment were comparable in both surveys (16.4 vs. 9.8%, p = 0.443). The proportion of the most frequent reasons for non-use detected in S2006 was decreased in S2008. It was a lack of information about the method (from 75.0 to 25.5%, p < 0.001), an absence of the national guidelines for TH usage (from 48.2 to 15.7%, p < 0,001) and a method technically too difficult (from 23.2 to 9.8%, p = 0.004). The complete list of the reasons of non-use in 2008 is reviewed in Figure 1.
Fig. 1. The reasons for TH non-use given by the providers of post-cardiac arrest care in 2008 TH – therapeutic mild hypothermia 
Guidelines implementation
Figure 2 shows the annual gain of new TH users every year from 2001 and the cumulative amount of TH users. The year of the maximal annual gain of the new TH users was 2007. After the publication of both documents, an ILCOR Advisory statement 2003 was considered to be the impulse for TH introduction in 25% of the responding ICUs, while the subsequent European Resuscitation Council guidelines 2005 accounted for 73% of them [1, 2].
Fig. 2. The annual gain of new TH using ICUs and the cumulative number of TH using ICUs ILCOR 2003 – therapeutic hypothermia after cardiac arrest. An advisory statement by the Advancement Life support Task Force of the International Liaison committee on Resuscitation1; ERC 2005 – European Resuscitation Council guidelines for resuscitation 20052; TH – therapeutic mild hypothermia; ICU – intensive care unit 
As much as 77.8% of the responders supported the strategy of cooling initiation of succesfully resuscitated out-of-hospital cardiac arrest patients as early as in the pre-hospital period.
Discussion
The results of our survey found that the implementation of TH after cardiac arrest in the non-surgical ICUs in the Czech Republic increased from 50.7 to 65.3% during the period from December 2006 to October 2008. The most frequent reason for non-use in 2008 was a lack of resources.
Induction of TH in cardiac arrest survivors has been entrenched in the guidelines and should be a routine part of an armamentarium of all facilities providing post-cardiac arrest support [2, 3]. Effectivity of the method has been evaluated by randomized clinical trials [7, 8]. An excellent clinical effect of the method has been shown with a number-needed-to-treat of 6 to reach a favourable neurological outcome [9]. Nevertheless, a number of surveys published in the last five years has revealed that an implementation of TH into the routine post-resustitaion management has been unsatisfactory in different countries, fluctuating from 8 to 95 % – Figure 3 [4, 5, 10–18].
Fig. 3. TH implementation in different countries in the last years USA – United States of America; D – Germany; GB – Great Britain; AUS – Australia; FIN – Finland; CA – Canada; CZ – Czech Republic; PL – Poland; SCOT – Scotland; NL – Netherlands; TH – therapeutic mild hypothermia. 
However, these findings represent general information only. There has been a lot of methodological differences between the surveys, especially in the definition of the target group of the investigations (some surveys investigated a personal experience of the individual physicians, the other examined TH implementation in the separate ICUs), in the questionnaire design, in the number of items, in its formulation, in the way of the questionnaire delivery etc. Moreover, assessment of TH implementation was usually only qualitative, based on the question like „have you ever used TH after cardiac arrest?“. It would be more useful to analyze also a proportion of cardiac arrest patients treated with TH within all admitted cardiac arrest cases. Such analysis has been published by Oksanen et al. [5]. They performed a very sophisticated registry-based national survey in all 20 Finnish ICUs providing early post-cardiac arrest support. They found a very high TH implementation of 95%. However, the proportion of cooled patients within all the cardiac arrest cases in the country was only 28% in 2005. It is also important that in this nation-wide survey, the authors found a similar 6-months outcome of cardiac arrest patients as in published randomized studies.
Therefore, we should be aware that TH implementation in USA, Canada and in several other european countries except for Finland has been low and probably applied only to a limited group of patients. Thus, in the following surveys, it is advisable to investigate not only a simple TH implementation but also its real frequency of use and further interventions should be targeted also to this aspect.
In the Czech Republic, we observed an increase in number of the ICUs using TH while the frequency of its application has remained the same in the last two years. The second survey showed that the frequency of the TH application is associated with the length of TH implementation and a rule proceeds “the longer time method implemented, the higher frequency of use”. In the last 3 years an intensive professional discussion dealing with TH has been in progress in the community of intensivists, cardiologists and emergency medicine physicians in the Czech Republic. This can be one of the main influences of TH usage enhancement. We found exquisite implementation in the Depts. of Anaesthesiology and Intensive Care, where there has been a majority of cardiac arrest patients admitted in the Czech Republic’s history. It has reached almost 100% in the time of the survey and the frequency of use was 54%. In the Coronary Care Units, TH implementation has remained permanently high, but with the increase of frequency of use. On the contrary, unsatisfactory positions have been described in both survey and in the Internal Medicine ICUs with low implementation and frequency of use. A main reason is probably a small number of admitted cardiac arrest patients in the Internal Medicine ICUs. We can speculate that this fact can be associated with less intense effort to update a post-cardiac arrest care. The implementation of TH in other types of ICU (neurological, pediatric etc.) was not possible to assess beyond the statement of the fact that some of them use TH for a small number of the responders in our survey.
Almost all the published studies reffered also to the reasons for non-use of TH. The most common were not enough data, a lack of experiences with the method, a lack of resources, an absence of the guidelines or local protocol and informants have never thought about TH or had no reason for non-use [4, 5, 10–16].
Despite of an increasing number of published articles in the last years, one tenth of the responders providing post-cardiac arrest care indicated in S2008 that they had never heard about the method. In S2006, the most frequent reasons among the informed non-users have been the a lack of information about the method and the absence of the national guidelines for TH usage. Both have been significantly less frequent in 2008, but still present. All these reasons are related together and we hope that will be minimalized by Czech Consensual statement for the application of TH which has been released recently [19]. This document covers essential knowledge and a protocol for TH administration.
In S2008, the most frequent recent reason for non--use has been referred a lack of financial resources. It is true that sophisticated device-based cooling techniques are associated with considerable initial and operating costs. However, rapid administration of cold crystaloids and simple surface cooling via ice packs is a very cheap and efficient method. Although this approach is burdened by a considerable risk of overcooling, it has been evaluated as effective in randomized studies [7, 8, 20, 21]. Therefore, conventional simple methods are still an acceptable way of cooling and are applicable especially as a starting implementation technique with minimal costs. Thus, a lack of resources should not be a fundamental reason for non--use of TH.
We appreciate that more than one third of non-using ICUs reported that they are ready for use and waiting for the first patient. This indicates ongoing increment of TH implementation.
We also assessed whether and how intensively the implementation of TH in the Czech Republic has been influenced by the published ILCOR Advisory statement of 2003 and The European Resuscitation Council guidelines for resuscitation 2005 [1, 2]. The latter was the impulse for the TH acceptance in the majority of the responders. The maximum annual gain of new TH users was observed 2 years after the guidelines were released, indicating a common period neccessary to complete the process for a major acceptance of guidelines.
It is noteworthy that three quarters of the TH using responders supported pre-hospital initiation of cooling in the resuscitated out-of-hospital cardiac arrest patients. This is in agreement with the standpoint of The Czech Society for Emergency and Disaster Medicine. It is with the close cooperation of in-hospital facilities that makes it an effort to augment pre-hospital post-cardiac arrest support including TH.
Even though increasing implementation of TH induction in cardiac arrest patients is obvious in the Czech Republic, there are a lot of challenges and room for improvement. Firstly, one stream of effort dealing with TH in cardiac arrest survivors should be targeted to extend general TH acceptance and implementation in the Internal Medicine ICUs. This would be with the cooperation with the Czech Society of Internal Medicine. Secondly, effort should be focused on enhancing the frequency of TH application in all ICUs. Thirdly, with an understanding of the advantages of device-based cooling techniques, its unavailability should not be a barrier for TH implementation. We hope that the release of a national consensual statement will help to widen the acceptance of the effective and safe practice of TH in cardiac arrest survivors. Anyway, we are aware of the fact that guidelines, however evidence-based, are only a single contributor to the definite clinicians acceptance of a new method. Soreide et al. and Brooks et al. reviewed specific barriers for the implementation of TH and outlined the specific interventions having potentional to improve TH uptake [22, 23]. These increase the visibility of TH guidelines within the guideline, the addition of a cooling protocol to the guidelines, the usage of clinically embedded reminders, the optimalization of organizational factors to facilitate TH delivery, the encouragement of interprofessional involvement to promote guideline implementation, the dissemination of research findings through courses, mailing and journals and the adoption of periodic audit and feedback. The continuing process of guideline implementation must be stepwise, following the awareness-agreement-adoption-adherence model [24]. Generally, we consider that further TH surveys should be constructed as ICU clinical practice targeted rather than an analysis of experiences of separate physicians. The most benefitial would be to assess a particular proportion of treated patients of all admitted cardiac arrest patients rather than evaluation of simple use or non-use only.
We will continue monitoring the practice of TH and we plan to perform a subsequent survey in 2011.
Acknowledgements: The study was supported by a grant IGA MH CZ NS10383-2/2009 and by a research project MZO 00179906.
Došlo dne 7. 5. 2010.
Přijato dne 21. 9. 2010.
Adresa pro korespondenci:
MUDr. Roman Škulec
Územní středisko záchranné služby Středočeského kraje
Prof. Veselého 461
266 01 Beroun
e-mail: skulec@email.cz
Zdroje
1. Nolan, J. P., Morley, P. T., Hoek, T. L., Hickey, R. W. Advancement Life support Task Force of the International Liaison committee on Resuscitation. Therapeutic hypothermia after cardiac arrest. An advisory statement by the Advancement Life support Task Force of the International Liaison committee on Resuscitation. Resuscitation, 2003, 57, p. 231–235.
2. Nolan, J. P., Deakin, C. D., Soar, J., Böttiger, B. W., Smith, G. European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2005. Section 4. Adult advanced life support. Resuscitation, 2005, 67, Suppl 1, p. S39–S86.
3. Castrén, M., Silfvast, T., Rubertsson, S. et al. Task Force on Scandinavian Therapeutic Hypothermia Guidelines, Clinical Practice Committee Scandinavian Society of Anaesthesiology and Intensive care Medicine. Scandinavian clinical practice guidelines for therapeutic hypothermia and post-resuscitation care after cardiac arrest. Acta Anaesthesiol. Scand., 2009, 53, p. 280–288.
4. Krawczyk, P., Fraczek, B., Drab, E. Use of therapeutic hypothermia in Polish intensive care units. Resuscitation, 2008, 79, p. 339.
5. Oksanen, T., Pettilä, V., Hynynen, M., Varpula, T. Intensium Consortium study group. Therapeutic hypothermia after cardiac arrest: implementation and outcome in Finnish intensive care units. Acta Anaesthesiol. Scand., 2007, 51, p. 866–871.
6. Skulec, R., Dostalova, G., Kovarnik, T., Linhart, A., Seblova, J. Therapeutic hypothermia in cardiac arrest survivors: a survey of practice in the Czech Republic. Resuscitation, 2008, 77, p. 419–420.
7. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N. Engl. J. Med., 2002, 346, p. 549–556.
8. Bernard, S. A., Gray, T. W., Buist, M. D. et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N. Engl. J. Med., 2002, 346, p. 557–563.
9. Holzer, M., Bernard, S. A., Hachimi-Idrissi, S., Roine, R. O., Sterz, F., Müllner, M. Collaborative Group on Induced Hypothermia for Neuroprotection After Cardiac Arrest. Hypothermia for neuroprotection after cardiac arrest: systematic review and individual patient data meta-analysis. Crit. Care Med., 2005, 33, p. 414–418.
10. Abella, B. S., Rhee, J. W., Huang, K. N., Vanden Hoek, T. L., Becker, L. B. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation, 2005, 64, p. 181–186.
11. Wolfrum, S., Radke, P. W., Pischon, T., Willich, S. N., Schunkert, H., Kurowski, V. Mild therapeutic hypothermia after cardiac arrest – a nationwide survey on the implementation of the ILCOR guidelines in German intensive care units. Resuscitation, 2007, 72, p. 207–213.
12. Laver, S. R., Padkin, A., Atalla, A., Nolan, J. P. Therapeutic hypothermia after cardiac arrest: a survey of practice in intensive care units in the United Kingdom. Anaesthesia, 2006, 61, p. 873–877.
13. Kennedy, J., Green, R. S., Stenstrom, R. CAEP Critical Care Committee. The use of induced hypothermia after cardiac arrest: a survey of Canadian emergency physicians. CJEM, 2008, 10, p. 125–130.
14. Bianchin, A., Pellizzato, N., Martano, L., Castioni, C. A. Therapeutic hypothermia in Italian intensive care units: a national survey. Minerva Anestesiol., 2009, 75, p. 357–362.
15. Sim, M., Dean, P., Booth, M., Kinsella, J. Uptake of therapeutic hypothermia following out-of-hospital cardiac arrest in Scottish Intensive Care Units. Anaesthesia, 2008, 63, p. 886–887.
16. Merchant, R. M., Soar, J., Skrifvars, M. B. et al. Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest. Crit. Care Med., 2006, 34, p. 1935–1940.
17. Bouwes, A., Kuiper, M. A., Hijdra, A., Horn, J. Induced hypothermia and determination of neurological outcome after CPR in ICUs in the Netherlands: results of a survey. Resuscitation, 2010, 81, p. 393–397.
18. Binks, A. C., Murphy, R. E., Prout, R. E. et al. Therapeutic hypothermia after cardiac arrest - implementation in UK intensive care units. Anaesthesia, 2010, 65, p. 260–265.
19. Cvachovec, K., Černý, V., Dostál, P, et al. Czech Society of Anaesthesiology and Intensive Care Medicine CLS JEP, Czech Society of Intensive Medicine CLS JEP, Czech Society for Emergency and Disaster Medicine CLS JEP. Consensual statement for the application of therapeutic hypothermia. Anest. Intenziv. Med., 2009, 20, p. 221–224.
20. Merchant, R. M., Abella, B. S., Peberdy, M. A. et al. Therapeutic hypothermia after cardiac arrest: Unintentional overcooling is common using ice packs and conventional cooling blankets. Crit. Care Med., 2006, 34, 12 Suppl., p. S490–S494.
21. Škulec, R., Kovárník, T., Bělohlávek, J. et al. Nadměrné ochlazení během mírné hypotermie po srdeční zástavě – fenomén zasluhující pozornost. Vnitr. Lek., 2008, 54, p. 609–614.
22. Brooks, S. C., Morrison, L. J. Implementation of therapeutic hypothermia guidelines for post-cardiac arrest syndrome at a glacial pace: seeking guidance from the knowledge translation literature. Resuscitation, 2008, 77, p. 286–292.
23. Søreide, E., Sunde, K. Therapeutic hypothermia after out-of hospital cardiac arrest: how to secure worldwide implementation. Curr. Opin. Anaesthesiol., 2008, 21, p. 209–215.
24. Pathman, D. E., Konrad, T. R., Freed, G. L., Freeman, V. A., Koch, G. G. The awareness-to-adherence model of the steps to clinical guideline compliance. The case of pediatric vaccine recommendations. Med. Care, 1996, 34, p. 873–889.
Štítky
Anesteziologie a resuscitace Intenzivní medicína
Článek Zápis z jednání výboru ČSIMČlánek JMENNÝ REJSTŘÍKČlánek VĚCNÝ REJSTŘÍKČlánek Chladná hlava nad zlatoČlánek Dynamics of the neurofilament pNF-H as a predictor of mortality in children with brain injuryČlánek Thrombocytes in sepsisČlánek Výborová schůze ČSARIM
Článek vyšel v časopiseAnesteziologie a intenzivní medicína
Nejčtenější tento týden
2010 Číslo 6- Jak souvisí postcovidový syndrom s poškozením mozku?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Neodolpasse je bezpečný přípravek v krátkodobé léčbě bolesti
- Léčba akutní pooperační bolesti z pohledu ortopeda
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
-
Všechny články tohoto čísla
- Chladná hlava nad zlato
- Comparison of patient satisfaction after general and regional anaesthesia in total hip and knee replacement surgery
- In-hospital therapeutic hypothermia in cardiac arrest survivors: Growing implementation in the Czech Republic (PRE-COOL 2: Hospital Survey 2008)
- High frequency jet ventilation applied via a catheter for Fantoni’s tracheostomy
- Dynamics of the neurofilament pNF-H as a predictor of mortality in children with brain injury
- Septic shock in fatal pneumonia caused by Staphylococcus aureus: The significance of producing Pantone-Valentine leukocidine – case report
- Thrombocytes in sepsis
- 6. CELOSTÁTNÍ KONFERENCE UMĚLÁ PLICNÍ VENTILACE 2010
- In memoriam doc. MUDr. Václav Trávníček, CSc. (1924–2010)
- Statistika oboru anesteziologie a resuscitace
- Výborová schůze ČSARIM
- Seznam akcí pořádaných v roce 2010 společností ČSARIM nebo pod její záštitou
- Zápis z jednání výboru ČSIM
- Česká resuscitační rada – nová organizace založena s podporou ČSARIM a ČSIM
- JMENNÝ REJSTŘÍK
- VĚCNÝ REJSTŘÍK
- Anesteziologie a intenzivní medicína
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Septic shock in fatal pneumonia caused by Staphylococcus aureus: The significance of producing Pantone-Valentine leukocidine – case report
- Comparison of patient satisfaction after general and regional anaesthesia in total hip and knee replacement surgery
- Thrombocytes in sepsis
- High frequency jet ventilation applied via a catheter for Fantoni’s tracheostomy
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



