-
Medical journals
- Career
Evaluation of intern doctor knowledgeability of transfusion medicine in Turkey
Authors: F. T. Kupesiz 1; S. Ocak 2; B. S. Koc 3; M. S. Evim 4; O. Tufekci 5; G. T. Kintrup 6; U. Aygunes 7; I. Eker 8; B. U. Koluman 9; G. Ilhan 10; N. Andic 11; E. Toret 12; A. B. Akinci 13; B. T. Gunes 14; F. Yilmaz 15; D. G. Gokcebay 16; T. B. Ozer 17; M. Isik 16; Y. Oymak 18; B. Atesagaoglu 19; I. E. Ozunal 20; M. Duran 21; D. O. Erkan 22; E. Gurpinar 23; Y. Aydinok 24
Authors‘ workplace: Department of Paediatrics, Division of Haematology and Oncology, University of Health Sciences Antalya Training and Research Hospital, Antalya, Turkey 1; Department of Paediatrics, Division of Haematology and Oncology, Istanbul University Istanbul Faculty of Medicine, Istanbul, Turkey 2; Department of Paediatrics, Division of Haematology and Oncology, Istanbul University Cerrahpasa Faculty of Medicine, Istanbul, Turkey 3; Department of Paediatrics, Division of Haematology and Oncology, Uludag University, Bursa, Turkey 4; Department of Paediatrics, Division of Haematology and Oncology, Dokuz Eylul University, İzmir, Turkey 5; Department of Paediatrics, Division of Haematology and Oncology, Akdeniz University, Antalya, Turkey 6; Department of Paediatrics, Division of Haematology and Oncology, University of Health Sciences Konya Training and Research Hospital, Konya, Turkey 7; Department of Paediatrics, Division of Haematology and Oncology, University of Health Sciences Afyonkarahisar, Afyonkarahisar, Turkey 8; Department of Internal Medicine, Division of Haematology, Pamukkale University, Denizli, Turkey 9; Department of Internal Medicine, Division of Haematology, Mustafa Kemal University, Hatay, Turkey 10; Department of Internal Medicine, Division of Haematology, Osmangazi University, Eskisehir, Turkey 11; Department of Paediatrics, Division of Haematology and Oncology, Osmangazi University, Eskisehir, Turkey 12; Department of Paediatrics, Division of Haematology and Oncology, 18 Mart University, Canakkale, Turkey 13; Department of Paediatrics, Division of Haematology and Oncology, University of Health Sciences Tepecik Training and Research Hospital, Izmir, Turkey 14; Department of Internal Medicine, Division of Haematology, Marmara University Pendik Training and Research Hospital, Istanbul, Turkey 15; Department of Paediatrics, Division of Haematology and Oncology, University of Health Sciences Ankara City Hospital, Ankara, Turkey 16; Department of Paediatrics, Division of Haematology and Oncology, Medeniyet University Goztepe Training and Research Hospital, Istanbul, Turkey 17; Department of Paediatrics, Division of Haematology and Oncology, University Of Health Sciences Dr. Behcet Uz Children’s Training and Research Hospital, Izmir, Turkey 18; Department of Internal Medicine, Division of Haematology, Balıkesir State Hospital, Balıkesir, Turkey 19; Department of Internal Medicine, Division of Haematology, Medeniyet University Goztepe Training and Research Hospital, Istanbul, Turkey 20; Department of Internal Medicine, Division of Haematology, University of Health Sciences, Konya Training and Research Hospital, Konya, Turkey 21; Statistics Consulting Unit, Akdeniz University, Antalya, Turkey 22; Medical Education Department, Akdeniz University Faculty of Medicine, Antalya, Turkey 24Department of Paediatrics, Division of Haematology and Oncology, Ege University, İzmir, Turkey 23
Published in: Transfuze Hematol. dnes,26, 2020, No. 3, p. 201-211.
Category: Original Papers
Overview
Úvod: Správné klinické použití krve a krevních přípravků vyžaduje kompetentní teoretickou a praktickou znalost transfuzního lékařství. Výuka medicíny v Turecku je definována v Národním vzdělávacím programu kurikula lékařských fakult (National Core Education Program on the Curriculum of Medical Faculties – NCEP). Cíle: Cílem této studie bylo vyhodnotit úroveň znalostí transfuzního lékařství a dosažení cílů vzdělávání u tureckých studentů medicíny v posledním roce studia a identifikovat faktory ovlivňující vzdělávání v transfuzním lékařství.
Materiál a metody: Tato multicentrická studie byla provedena u studentů medicíny v jejich posledním roce praxe před promocí. Otázky průzkumu byly připraveny na základě základních informací o cílech vzdělávání v transfuzním lékařství podle NCEP. Dotazník sestával ze sebehodnocení kompetencí podle Linkertovy škály a teoretických otázek. Zkoumaná skupina byla vytvořena stratifikovaným výběrem. Průzkum byl prováděn formou osobních pohovorů. Ke statistické analýze byl použit program IBM SPSS v.25. Chí-kvadrát test byl použit pro parametrická a U testy Mann-Whitney pro neparametrická data. Hladina P < 0,05 byla přijata jako statisticky významná.
Výsledky: Studie se zúčastnilo 727 (24 %) z 3 009 studentů posledního ročníku studia ze 13 lékařských fakult. V sebehodnocení kompetence 65 % studentů považovalo výuku transfuzního lékařství za nedostatečnou, pouze 14 % studentů se považovalo za schopných rozlišit transfuzní komplikace a podat léčbu první linie. Podání a monitorování průběhu transfuze by pod dohledem zvládlo 41 % respondentů a 7 % potvrdilo, že k tomu absolvovalo dostatečnou praxi, zatímco zbylých 52 % považovalo své znalosti v této oblasti za úplně nedostatečné. Deset otázek hodnotících základní znalosti a dosažení edukačních cílů mělo 53 možných odpovědí (26 správných a 27 nesprávných). Průměrný počet správně vybraných správných odpovědí byl 3 ± 3,5 z 26, zatímco průměrný počet nesprávných odpovědí vybraných jako správné byl 8 ± 3,1 z 27. To ukázalo, že studenti medicíny před promocí nebyly schopni určit 50 % ze správných a 30 % nesprávných údajů o základech transfuzní praxe.
Diskuse: Naše výsledky potvrzují, že velká část studentů medicíny před promocí nemá v transfuzním lékařství dostatečné teoretické znalosti nebo praktické dovednosti. Věříme, že rozšíření a standardizace kurikula transfuzního lékařství na lékařských fakultách pomůže u mladých lékařů zlepšit jejich znalosti v této oblasti.
Keywords:
transfusion medicine – Education – medical students – self-assessment questionnaire
INTRODUCTION
Transfusion is an indispensable procedure in all medical and surgical specialties. While transfusion of blood and its components may be life-saving, inappropriate clinical use may result in serious morbidity and even death. Studies regarding transfusion medicine have focused on the appropriate use of blood [1–4]. Blood and blood products are commonly used in the hospital setting and it is imperative that physicians possess at least basic theoretical and practical knowledge of transfusion medicine to ensure their proper application [5–9].
Although physicians follow developments in other medical fields and current information on diagnostics and treatment practices more closely, they show less interest in improvements in appropriate use of blood products [10–12]. Knowledge of transfusion medicine is usually based on clinical training and conventional education [5–8].
It is clear that transfusion training should be given properly in order to improve transfusion practices [11]. Studies evaluating transfusion medicine education in both developed and developing countries have revealed a lack of standardization between countries and even within faculties in the same country, at both the undergraduate and postgraduate levels [4, 13–15]. In response, several countries have scrutinized their own education systems and proposed means of improving transfusion medicine education [4, 5, 12, 13, 16].
Medical schools in Turkey use the discipline-based model. In order to improve the education and training provided in medical faculties and raise them to international standards, the National Core Education Program (NCEP) for medical school curricula was updated and all medical schools were asked to implement the 2014 NCEP. In addition, medical schools inside Turkey accredited by the Association for Evaluation and Accreditation of Medical Education Programs (TEPDAD) under the World Medical Education Federation establish their educational curricula in accordance with the 2014 NCEP.
Few studies have investigated the quality and nature of transfusion medicine education [4, 17, 18]. The purpose of our study was to evaluate the knowledge and perceptions of competence regarding transfusion medicine among intern doctors in Turkey. Determining the efficiency of transfusion medicine education at the undergraduate level in Turkish medical schools may help to understand the capability of newly graduated doctors who may be residents in medical fields where appropriate patient blood management will be lifesaving.
MATERIALS AND METHODS
This study was planned as a multicentre survey study of final-year medical students in their last internship before graduation from medical school. Sample size and distribution were determined using a stratified sampling method to represent 13 medical schools in direct proportion to the number of students enrolled in each faculty of medicine.
Survey questions were prepared by expert faculty members and included basic information that should be known given the NCEP ‘Blood Banking and Transfusion Medicine’ educational targets. The survey form is presented in the supplementary material.
The survey consisted of two parts. In the first, students rated their perceived competence in transfusion medicine and blood banking. The second part included 10 multiple-choice theoretical questions with a total of 53 options. Each of the options contained either correct or incorrect information and the students were asked to mark all of the choices they believed to be correct. Each of the options was evaluated as a separate data point. Current information about the medical schools participating in the survey was recorded (Table 1).
1. Information in faculties about education and blood banking 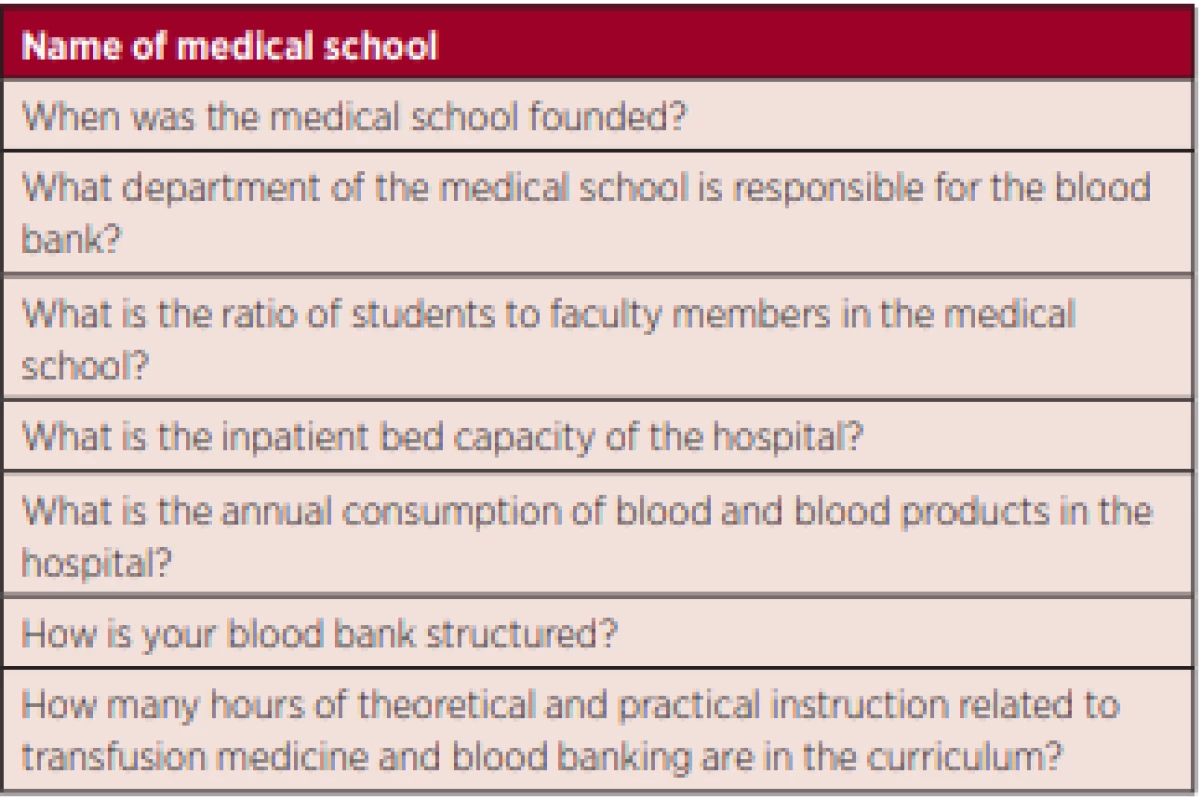
The survey questions were assessed in terms of suitability for measurement and evaluation by faculty members in the Department of Medical Education and in the Faculty of Education, Division of Measurement and Evaluation. After testing the comprehensibility of the survey using a pilot study, it was applied through one-on-one interviews with each of the students in the study group.
Statistical analyses were performed using IBM SPSS v.23 statistical software with support from the Akdeniz University Statistical Consulting Unit. The chi-square test was used for parametric testing and the Mann - -Whitney test was used for nonparametric testing, with p < 0.05 accepted as significant.
After obtaining local ethics committee approval (UHS-2018-135), the study was performed via one-on - -one interviews with the students by the selected haematologist from each medical school participating in the study.
RESULTS
This multicentre study included 727 out of a total of 3009 intern doctors at 13 medical faculties. Proportional representation of each faculty was ensured as follows: 112 of 470 interns in Istanbul University, Istanbul Faculty of Medicine (23.8%), 101 of 430 in Istanbul University, Cerrahpasa Faculty of Medicine (23.4%), 81 of 343 in Ege University (23.6%), 71 of 300 in Uludağ University (23.6%), 70 of 282 in Dokuz Eylül University (24.8%), 55 of 226 in Akdeniz University (24.3%), 47 of 200 in Cumhuriyet University (23.5%), 45 of 184 in Osmangazi University (24.4%), 35 of 143 in Mustafa Kemal University (24.4%), 35 of 138 in Afyon Kocatepe University (25.3%), 30 of 119 in Pamukkale University (25.2%), 25 of 94 in Katip Çelebi University (26.5%) and 20 of 80 in Onsekiz Mart University (25%).
Within the study group, 15.4% of the interns were from Istanbul University, Istanbul Faculty of Medicine, 13.9% from Istanbul University, Cerrahpasa Faculty of Medicine, 11.1% from Ege University, 9.8% from Uludag University, 9.6% from Dokuz Eylül University, 7.6% from Akdeniz University, 4.8% from Afyon Kocatepe University, 4.1% from Pamukkale University, 3.4% from Katip Celebi University and 2.8% from Onsekiz Mart University.
Self-reported competence
Students rated their opinion regarding whether the transfusion medicine education provided at their medical school was sufficient using a 5-point scale (1: Strongly disagree, 2: Disagree, 3: Partially agree, 4: Agree, 5: Strongly agree). The mean score was 2.22 ± 0.91 (median: 2), indicating that the interns generally considered the education to be insufficient. Only 2% of intern doctors strongly agreed that the education was sufficient, while a total of 65% disagreed or strongly disagreed (Table 2).
2. Distribution of scores in the students’ self-evaluation of competence 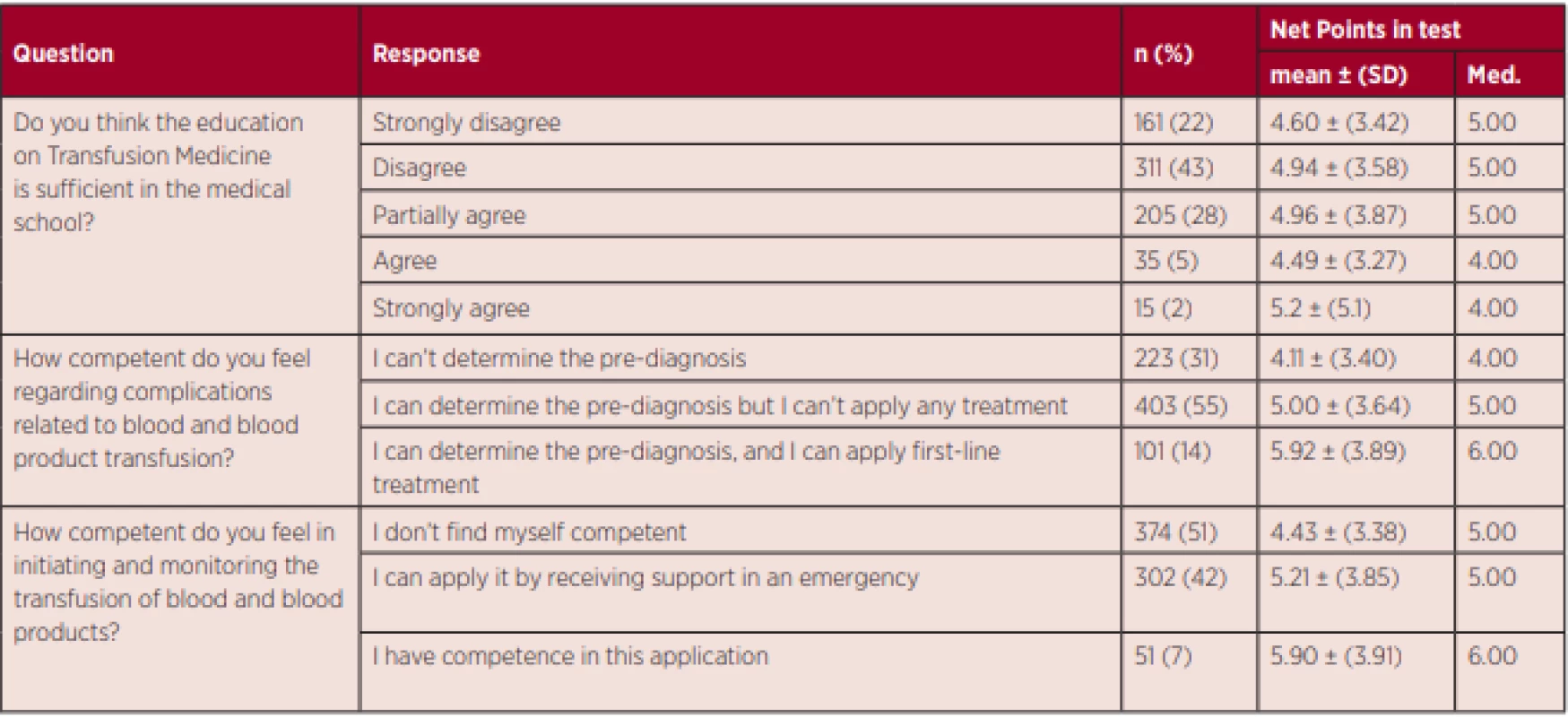
The students then evaluated their ability to recognize transfusion complications and administer first-line treatment using a 3-point scale (1: I cannot determine a pre-diagnosis, 2: I can determine a pre-diagnosis but not intervene, 3: I can determine a pre-diagnosis and administer the first-line treatment). The mean score was 1.83 ± 0.65 (median: 2), with the majority stating they could diagnose but not treat. Only 14% of the students felt competent in recognizing transfusion complications and applying first-line treatment (Table 2). Although being able to recognize transfusion complications at the pre-diagnosis level is an NCEP educational target, 30% of the students did not express confidence in the pre-diagnosis of transfusion complications.
When the students rated their perceived competence in initiating and monitoring blood transfusions on a 3-point scale (1: I do not feel competent, 2: I can do under supervision in case of emergency, 3: I am competent), the mean score was 1.56 ± 0.62 (median: 1). Only 7% of intern doctors felt completely capable, 41% said they could manage under supervision in case of emergency and the other half of (52%) felt completely unprepared to initiate and monitor blood transfusions (Table 2).
There were significant but weak correlations between total score and perceived competence in recognizing and treating transfusion complications (p < 0.001, r = 0.149) and in starting and monitoring blood transfusions (p = 0.002, r = 0.115).
Assessment of theoretical knowledge
The students were presented with 53 choices in 10 questions and asked to indicate all correct answers. The students selected a mean of 13 ± 3.5 (median: 13) of the total 26 right answers, while they incorrectly chose a mean of 8 ± 3.1 (median: 8) of the total 27 wrong answers. Their mean net score was calculated as 5 ± 3.7 (median 5). This showed that among very basic and practical transfusion information, intern doctors approaching medical school graduation were unable to recognize 50% of the correct answers and 30% of the incorrect answers. Striking examples of right and wrong answers that the students missed are presented in Tables 3 and 4 respectively, together with student percentages. Distribution of scores according to the characteristics of the students’ medical schools is presented in Table 5.
3. Correct answers not recognized as correct by the students 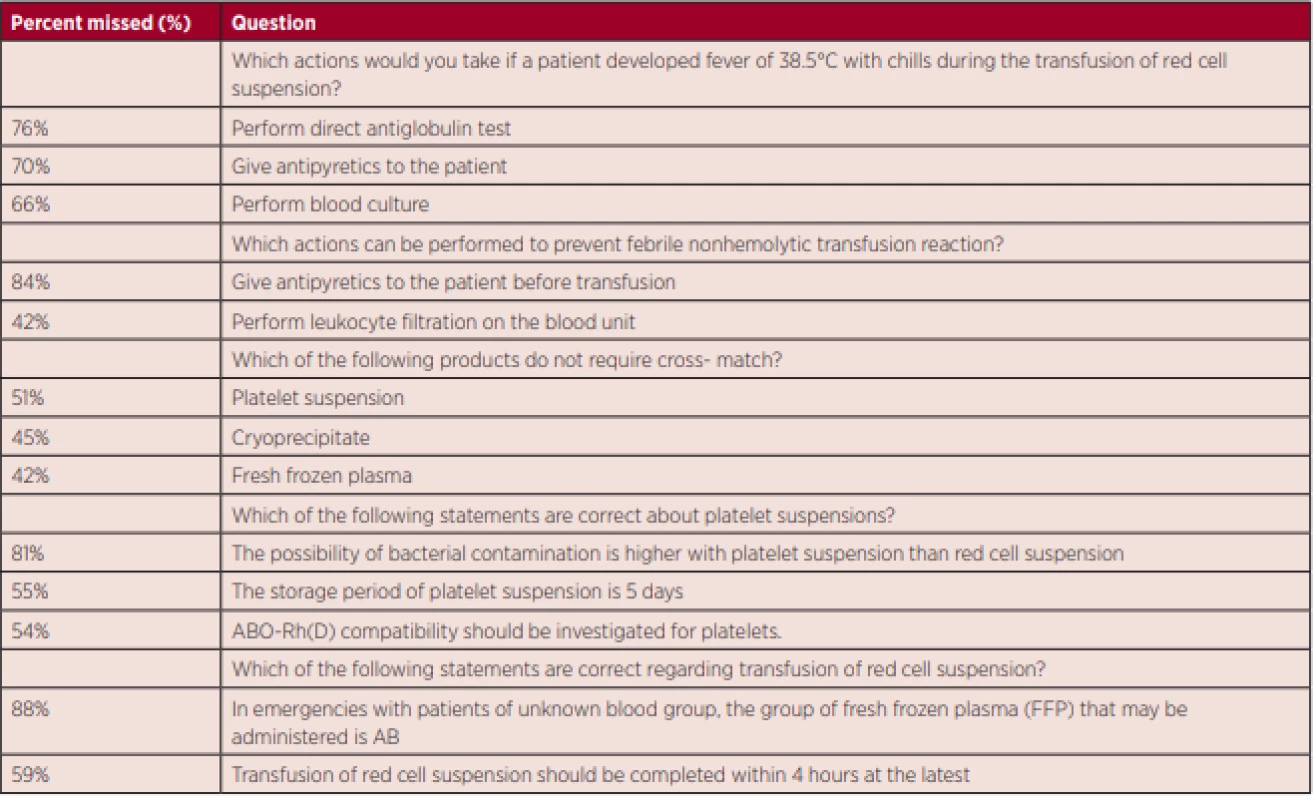
4. Incorrect answers not recognized as incorrect by the students 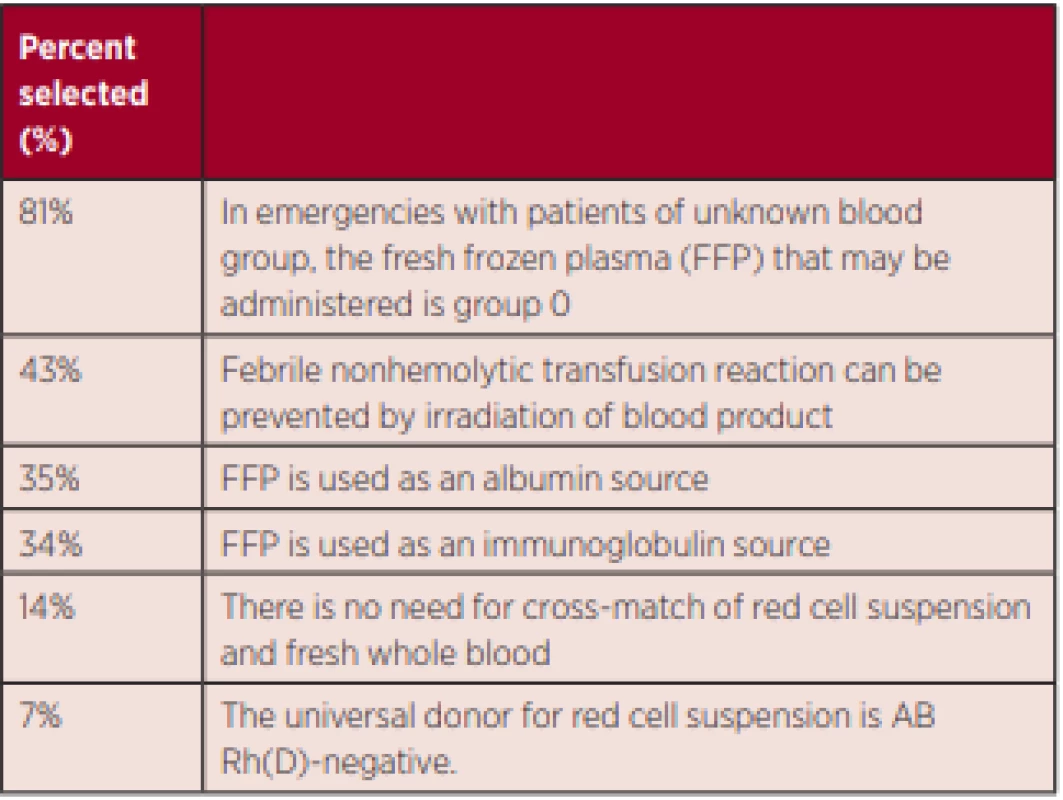
5. Distribution of the student´s scores according to the characteristics of medical schools 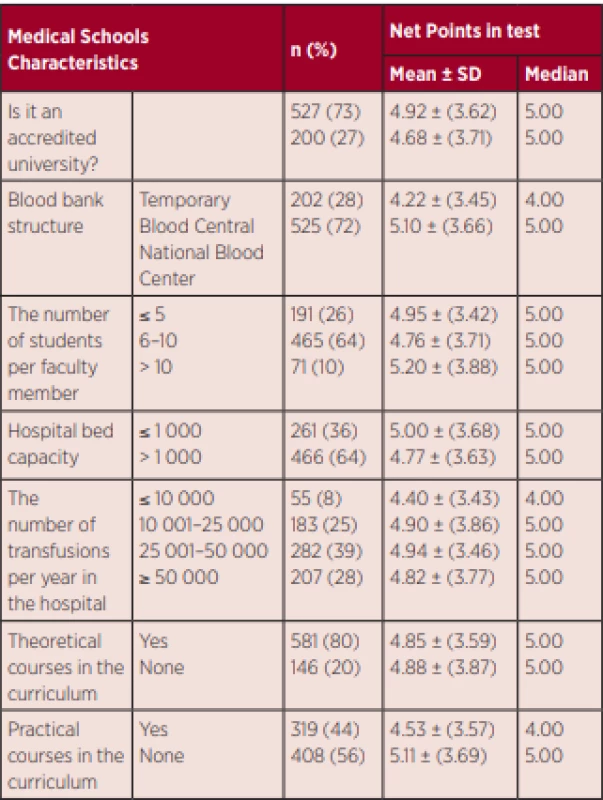
Evaluation of factors affecting education
While 10 of the 13 faculties represented in our study had theoretical courses in their curriculum, only 6 offered practical training. Although theoretical education was not associated with total scores (p = 0.873), students attending faculties with practical training had significantly lower scores (p = 0.017).
For 72.5% (525) of students, the blood banks of their faculty hospital were operating as temporary blood centres and these students had significantly higher scores than students from hospitals that were structured as blood bank transfusion centres (p = 0.003). Higher annual amount of blood products transfused in a faculty was associated with the students’ knowledge level (p = 0,002).
When the medical schools were evaluated with regard to their faculty member to student ratio, the results ranged from 2 : 1 to 1 : 12. After grouping based on student to faculty ratio (≤ 5, 6–10, ≥ 11), no significant association with total scores was observed (p = 0.638).
In the 7 faculties that had National Medical Education Accreditation and had adopted the NCEP as their curriculum, 72% of students received education in transfusion medicine, but being an accredited university was not shown to have any effect on the students’ knowledge level (p = 0.554).
Being educated at an accredited faculty, blood bank structuring, student to faculty member ratio, incorporation of theoretical and practical courses in the curriculum and annual amount of blood transfusions were not associated with students’ perceptions of the adequacy of their transfusion medicine education or their competence in recognizing and managing transfusion complications or initiating and monitoring transfusions (p <0.05).
DISCUSSION/CONCLUSION
Basic transfusion medicine curricula should cover good clinical practice with regards to the use of blood and blood products and the principles of proper implementation of transfusion services during physicians’ specialist training.
Medical students and residents in internal and surgical specialties should have accurate and comprehensive information on the use of blood and blood products. A study by Flausino et al. revealed that young physicians in particular do not have sufficient information on the indications and complications of the use of blood products [5]. O’Brien and colleagues also evaluated the knowledgeability of 116 recently graduate physicians in transfusion medicine based on standard patient practices and written examination and emphasized the lack of sufficient information in this field [19]. Only 17% of the residents knew what “TRALI” was (transfusion-related acute lung injury), while none of the resident assistants knew that irradiating blood products could prevent graft-versus-host disease. Similarly, our study demonstrated that medical students nearing graduation generally did not feel competent in transfusion medicine and did not possess basic knowledge about blood transfusions. In our study, almost half of the medical students who were about to graduate believed that febrile nonhemolytic reactions could be prevented by irradiation and hardly any of the interns knew the universal donor group for fresh frozen plasma (FFP). The lack of basic theoretical and practical knowledge of transfusion medicine among these interns who will work in emergency departments or enter residency programs after graduation, warrants concern. Karp et al. advised awareness of this in disciplines where transfusion is frequently used during resident training and stated that new graduates should also realize that they are not well-equipped for administering transfusions. We have reached similar conclusions based on our results and we believe that providing focused education on blood banking and transfusion practices to first-year residents in departments with frequent transfusion procedures will improve patient care and safety [15].
Panzer et al. evaluated transfusion medicine curricula in 14 countries and determined that the content, training methods, duration and timing of undergraduate transfusion medicine education vary widely between medical schools [4]. In Australia, while there is theoretical training, there are no training programs available to support students’ clinical skills. The curriculum is broader in Israel and is covered in the form of mandatory courses in France. Since transfusion medicine is regarded as a separate area of expertise in Germany, it is included in a separate training module and practical transfusion training is conducted bedside. In the United States, despite the frequent use of blood components and allocation of funds for transfusion medicine training, a standardized curriculum has not been developed as yet [4].
Although there is substantial variability in transfusion medicine education globally, the coverage of transfusion medicine and blood banking in medical school curricula is typically limited and general [13, 19]. In most medical schools, transfusion medicine is covered as part of bedside clinical training [5].
Since studies revealed the inadequacy of basic and continuing education in transfusion medicine in Brazil, research has focused on the dissemination of accredited transfusion medicine training programs [13, 20].
In African countries, transfusion medicine training has assumed an important place in the fight against AIDS. However, it was observed that physician training in transfusion medicine in most African countries was limited to only 1 - or 2-hour courses. This awareness led to the creation and implementation of training programs appropriate to local conditions [13]. Our study revealed that some medical schools in Turkey still allocate only 1 or 2 teaching hours to transfusion medicine.
In their study on transfusion medicine training in developing countries, Eichbaum et al. reported that each country is trying to determine their current situation and to develop training plans to improve local transfusion medicine practices within the framework of national health policies. [13].
Our study is the most comprehensive study conducted on this topic in our country. For a physician who has graduated from a Turkish medical school, the learning outcomes of the NCEP state that “they should be aware of blood and blood product transfusion complications at the preliminary diagnosis level and should know enough to refer to the relevant specialist after performing the necessary pre-treatment.”; and “In an emergency, they should have the ability to practice blood transfusions in accordance with the guidelines.” However, the result of our study showed that only 15% of final-year students close to graduation had achieved this learning objective. Considering that transfusion complications are urgent and may require life-saving intervention, the ratio of physicians who think that the learning target has been reached is quite insufficient.
The NCEP educational outcome for blood banking states that a graduate of medical school “recognizes complications of blood and blood product transfusion at pre-diagnosis level“. In our study, one-third of medical students near graduation stated that they could not determine the pre-diagnosis. Considering the urgency of potential transfusion-related complications, it is clear that this educational target is not being adequately met.
Similar studies helped identify deficits in transfusion medicine education in Iran [12, 21]. These suggested that 80% of Iranian medical schools did not provide effective theoretical and practical transfusion medicine training. In addition, they pointed out the lack of basic education in transfusion medicine, which is needed not only by medical students and general practitioners but also by medical staff. Taking the example of training programs around the world and targeting different levels of education, a training program was adapted to conditions in Iran and was reported to have played a vital role in improving patient safety and reducing the high cost of treatment with blood products [12, 21]
The students participating in the present study evaluated the education at their medical schools as insufficient. The 6-year medical curricula include a total of 0–4 hours of theoretical courses about blood banking and transfusion medicine, with no standardization in terms of which department is responsible for giving the course or the number of course hours. We have argued that 1 to 4 hours of theoretical training during 6 years of education is grossly insufficient for meeting the educational needs in blood banking and transfusion medicine and has essentially no educational value. Our findings support this, as there was no significant relationship between receiving theoretical education and the students’ knowledge level or self-perceived competence.
If the current approach provides no educational benefit, the methods, contents, and objectives of training should be re-evaluated and the programs revised accordingly. For example, centralized education was not effective in China, whereas extremely successful outcomes were obtained with locally structured education [13, 22].
An interesting finding in our study was that students receiving practical training scored lower in questions assessing theoretical knowledge. Assuming that the training they received is mostly based on bedside clinical training and mentor-apprentice relationships, this paradoxical result may be attributable to the transfer of inaccurate information and practice. Evaluating the content and delivery methods of these schools’ programs and interviewing lecturers may help identify failures in practical applications. Holding focus group discussions with the students in these schools may also help identify the problem by analysing it in its natural environment.
In faculties with temporary blood banks, blood centres procuring their own blood products will provide more encounters with blood banking, apheresis procedures and donors during student education. This can positively contribute towards education in blood banking and transfusion medicine.
One of the most common practices physicians encounter during their career is the use of blood products. However, we have demonstrated that medical students nearing graduation do not possess even very basic information about the properties of blood products. Lack of such information can lead to medical mistakes that may result in serious complications. Therefore, we believe that medical school curricula must be revised in terms of blood banking and the objectives and content of medical education.
Lack of transfusion medicine knowledgeability among physicians is common in both underdeveloped areas such as Africa, where there are fewer than 100 physicians trained in transfusion medicine per country, and in developed nations such as the USA, which has some of the most advanced transfusion medicine training in the world [23]. This clearly demonstrates the need to improve and disseminate transfusion medicine training globally [13].
The best way to reduce adverse events associated with blood transfusions is to decrease the number of unnecessary and noncompliant transfusions. The current curriculum is somewhat limited in terms of the rational use of blood and its components. Establishing regulations targeting the appropriate use of blood products as well as theoretical and practical training will create better equipped physicians and prevent many complications and unnecessary transfusions.
The results of our study suggest that medical schools are not producing physicians who are sufficiently knowledgeable and competent in transfusion medicine. At least, final-year medical students did not feel sufficiently competent in this field. More current and extensive knowledge of transfusion medicine can be provided to physicians in training through the re-evaluation of transfusion medicine practices and educational targets by a commission consisting of competent academicians; standardization of educational approaches and curricula, and clearer delegation of this educational responsibility. The results of our study were evaluated at a meeting of TEPDAD and the contents of the transfusion part of medical education curriculum in Turkish medical schools were changed.
Study Limitations
It is not entirely correct to deem transfusion medicine education insufficient based on results obtained from a limited number of theoretical questions presented to students. However, these questions covered very basic information about the properties of blood products and transfusion indications and complications and the expert consensus was that physicians without this minimal level of knowledge could pose a serious threat to patient safety. Therefore, the inadequate transfer of such basic information indicates a shortcoming in the medical education system that should be taken seriously.
ABBREVIATIONS
NCEP – National Core Education Program (of Turkey)
TEPDAD – Association for Evaluation and Accreditation of Medical Education Programs
AIDS – Acquired immunodeficiency syndrome
Author contributions
All authors contributed to the conception or design of the study or acquisition of data. Y. Aynidok, F. Kupesiz, and D. Ozel, performed data analysis and interpretation. Y. Aydinok, F. Kupesiz, and N. Andac prepared the manuscript and provided final approval of the published version.
Disclosure statement
The authors have no conflicts of interest to declare.
Statement of ethics
Ethics committee approval (2018-135) was received for the study by the Health Sciences University Education and Research Hospital.
Funding sources
The technical and political support of the ‘Turkish Society of Haematology’. This study was conducted as a project of the Turkish Society of Haematology ‘Transfusion Medicine and Apheresis Master Class’.
Acknowledgement
The authors thank Assistant Professor Hakan Kogar of Akdeniz University, Faculty of Education, Department of Measurement and Evaluation (Antalya) for assessing the suitability of survey questions in terms of measurement and evaluation.
Manuscript submitted on March 16, 2020.
Manuscript accepted after review on May 26, 2020.
Funda Tayfun Kupesiz, M.D.
Department of Paediatrics,
Division of Haematology and Oncology
University of Health Sciences Antalya Training and Research Hospital
Kazim Karabekir
Street Antalya, 07050,
Turkey
e-mail: fundatyfn@gmail.com
Sources
1. Tinmouth A. Reducing the amount of blood transfused by changing clinicians’ transfusion practices. Transfusion. 2007;47(2 Suppl):132S–136S; discussion 55S–56S.
2. Tinmouth A, Macdougall L, Fergusson D, et al. Reducing the amount of blood transfused: a systematic review of behavioral interventions to change physicians’ transfusion practices. Arch Intern Med. 2005;165(8):845–852.
3. Rothschild JM, McGurk S, Honour M, et al. Assessment of education and computerized decision support interventions for improving transfusion practice. Transfusion. 2007;47(2):228–239.
4. Panzer S, Engelbrecht S, Cole-Sinclair MF, et al. Education in transfusion medicine for medical students and doctors. Vox Sang. 2013;104(3):250–272.
5. Flausino Gde F, Nunes FF, Cioffi JG, Proietti AB. Teaching transfusion medicine: current situation and proposals for proper medical training. Rev Brasil Hematol Hemoter. 2015;37(1):58–62.
6. Graham J, Grant-Casey J, Alston R, Baker P, Pendry K. Assessing transfusion competency in junior doctors: a retrospective cohort study. Transfusion. 2014;54(1):128–136.
7. Graham JE. Transfusion e-learning for junior doctors: the educational role of ‘LearnBloodTransfusion’. Transfus Med. 2015;25(3):144 – 150.
8. Graham JE, Narayan S, Pendry K. Improving transfusion education for junior doctors; exploring UK experiences. Transfus Med. 2017;27(2):96–104.
9. Rahav Koren R, Suriu C, Yakir O, et al. Physicians’ lack of knowledge – a possible reason for red blood cell transfusion overuse? Israel J Health Policy Res. 2017;6(1):49.
10. Lin Y, Tinmouth A, Mallick R, Haspel RL, Investigators B-T. BESTTEST2: assessment of hematology trainee knowledge of transfusion medicine. Transfusion. 2016;56(2):304–310.
11. Haspel RL, Lin Y, Mallick R, Tinmouth A, Cid J, Eichler H, et al. Internal medicine resident knowledge of transfusion medicine: results from the BEST-TEST international education needs assessment. Transfusion. 2015;55(6):1355–1361.
12. Javadzadeh Shahshahani H. Status of transfusion medicine education in Iran. Arch Iran Med. 2016;19(6):439–445.
13. Eichbaum Q, Shan H, Goncalez TT, et al. Global health and transfusion medicine: education and training in developing countries. Transfusion. 2014;54(7):1893–1898.
14. Kumarage S, Fernando R, Gunasekara L. A survey of knowledge and practices of transfusion medicine among post intern doctors in specialized hospital in Sri Lanka. Lab Med. 2017;48(1):46–50.
15. Karp JK, Weston CM, King KE. Transfusion medicine in American undergraduate medical education. Transfusion. 2011;51(11):2470 – 2479.
16. Zeller MP, Sherbino J, Whitman L, et al. Design and implementation of a competency-based transfusion medicine training program in Canada. Transfus Med Rev. 2016;30(1):30–36.
17. Rock G, Berger R, Pinkerton P, Fernandes B. A pilot study to assess physician knowledge in transfusion medicine. Transfus Med. 2002;12(2):125–128.
18. Arinsburg SA, Skerrett DL, Friedman MT, Cushing MM. A survey to assess transfusion medicine education needs for clinicians. Transfus Med. 2012;22(1):44–49; quiz 49–51.
19. O’Brien KL, Champeaux AL, Sundell ZE, et al. Transfusion medicine knowledge in postgraduate year 1 residents. Transfusion. 2010;50(8):1649–1653.
20. Maiolino A, Spector N. Challenges for medical residency in hematology and transfusion medicine in Brazil. Rev Brasil Hematol Hemoter. 2012;34(5):321–322.
21. Gharehbaghian A, Javadzadeh Shahshahani H, Attar M, et al. Assessment of physicians knowledge in transfusion medicine, Iran, 2007. Transfus Med. 2009;19(3):132–138.
22. Li T, Wang W, Zhang L, et al. Designing and implementing a 5-year transfusion medicine diploma program in China. Transfus Med Rev. 2017;31(2):126–131.
23. Makani J, Lyimo M, Magesa P, Roberts DJ. Strengthening medical education in haematology and blood transfusion: postgraduate programmes in Tanzania. Br J Haematol. 2017;177(6):838–845.
Labels
Haematology Internal medicine Clinical oncology
Article was published inTransfusion and Haematology Today

2020 Issue 3-
All articles in this issue
- COVID-19 a transfuzní služba v ČR
- Regenerating haematopoiesis resembles embryonic stem cell-independent haematopoiesis
- Symptoms and manifestations of Erdheim-Chester disease
- Current treatment approaches in patients with newly diagnosed peripheral T-cell lymphoma and novel therapies-focusing on brentuximab vedotin
- Treatment of the multicentric and unicentric forms of Castleman disease
- Addressing the issues of complex care from the perspective of people with haemophilia
- Characteristics and results of treatment of younger patients less than 60 years old with AML: analysis of real data from the Czech DATOOL-AML database
- Rare dermatological entities associated with monoclonal gammopathy: sclerodema, scleromyxedema and IgA pemphigus – overview of 5 cases and therapeutic modalities
- Doporučený postup pro použití rekonvalescentní plazmy v léčbě dospělých pacientů s COVID-19
- Doporučený postup při řešení a vyšetřování potransfuzních reakcí
- Consensual guidelines of the Czech National Haemophilia Programme (CNHP) for replacement treatment of patients with haemophilia during invasive procedures and surgery, 2nd edition, year 2020
- Evaluation of intern doctor knowledgeability of transfusion medicine in Turkey
- Transfusion and Haematology Today
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Symptoms and manifestations of Erdheim-Chester disease
- Doporučený postup při řešení a vyšetřování potransfuzních reakcí
- Characteristics and results of treatment of younger patients less than 60 years old with AML: analysis of real data from the Czech DATOOL-AML database
- Current treatment approaches in patients with newly diagnosed peripheral T-cell lymphoma and novel therapies-focusing on brentuximab vedotin
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

