-
Medical journals
- Career
Intrapericardial teratoma as a cause of fetal death – a case report
Authors: H. Skálová; C. Povýšil
Authors‘ workplace: Czech Republic ; Institute of Pathology, 1st Faculty of Medicine, Charles University and General University Hospital in Prague
Published in: Čes.-slov. Patol., 47, 2011, No. 4, p. 189-191
Category: Original Article
Overview
Intrapericardial teratoma is a rare congenital tumor that without treatment leads to cardiac failure in either the prenatal or postnatal period. Early diagnosis and recent surgical advances can, in some cases, delay development of intrauterine symptoms and allow final treatment through a tumor resection. However, a large number of intrapericardial tumors go undetected during prenatal diagnostics, until they are found as a cause of intrauterine death or postnatal cardiorespiratory insufficiency, as in our case report. An abortion was induced in the 23rd gestational week because there was no cardiac activity detected during a routine ultrasound scan in a 35-year old woman. The tumor was found during the postmortem of the fetus.
Keywords:
teratoma – heart neoplasm – fetal deathIntrapericardial teratoma is a rare congenital tumor, which without treatment leads to cardiac failure in either the prenatal or postnatal period. Less than 100 cases have been described since the first case in 1890 (1). Prenatal diagnosis is based on routine ultrasound investigations, that usually reveal the tumor either coincidentally or as a cause of fetal hydrops. The most frequent symptom is a pericardial effusion, which results from an obstruction of cardiac and pericardial lymphatic veins and/or a ruptured cystic tumor. Rapidly increasing amounts of intrapericardial liquid put the fetus at increased risk of cardiac tamponade. In addition to fluid compression, the heart can also be compressed by the tumor itself. The second most common symptom, and a sign of intrauterine circulation failure, is fetalis hydrops, which must also be seen as a very unfavorable prognostic indicator. Early diagnosis together with recent surgical advances can, in some cases, compensate for the intrauterine situation, prevent complications or at least decelerate their development and facilitate a definitive therapy through a postnatal tumor resection. However, a high percentage of pericardial tumors still go undiagnosed during prenatal examinations and are revealed as a cause of either intrauterine death at autopsy, as it was in our case, or postnatal cardiorespiratory failure.
CASE REPORT
A 35-year-old woman, 3-gravida underwent a routine ultrasound examination during the 23rd gestational week. It showed an absence of cardiac activity and severe oligohydramnion. No further pathological findings were found. An abortion, for fetus mortuus, was then induced.
During the autopsy, a male fetus was found with an extensive intrapericardial tumor, extending from the pericardium and expelling the heart into the dorsolateral part of the left hemithorax and the the left lung into the dorsal part of the left hemithorax. The right atrium was most affected by compression. The pericardial cavity and both hemithoraxes were filled with a sanguineous effusion, additionally, there was less marked ascites and diffuse subcutaneous swelling.
A soft hemorrhagic tumor (3.5 x 3 x 3 cm) was bounded on the ventral side by the right and left cardiac ventricles and, particularly, by the right atrium. It occupied approximately two thirds of the pericardial cavity (Fig. 1). It was fixed by a white stalk to the aortic stem, otherwise it moved freely (Fig. 2). Microscopically, the tumor was a partially hemorrhagic mature teratoma composed predominantly of mature mesoblastic structures, namely lung, glandular and cartilage tissue, along with hepatic, brain, and smooth muscle tissue and vessels (Fig. 3). The tumor did not invade the aortic wall.
1. Intrapericardial teratoma. The tumor is localized anterior to the heart, which together with the left lung, are displaced posteriorly and partly covered by the tumor. Scale in cm. 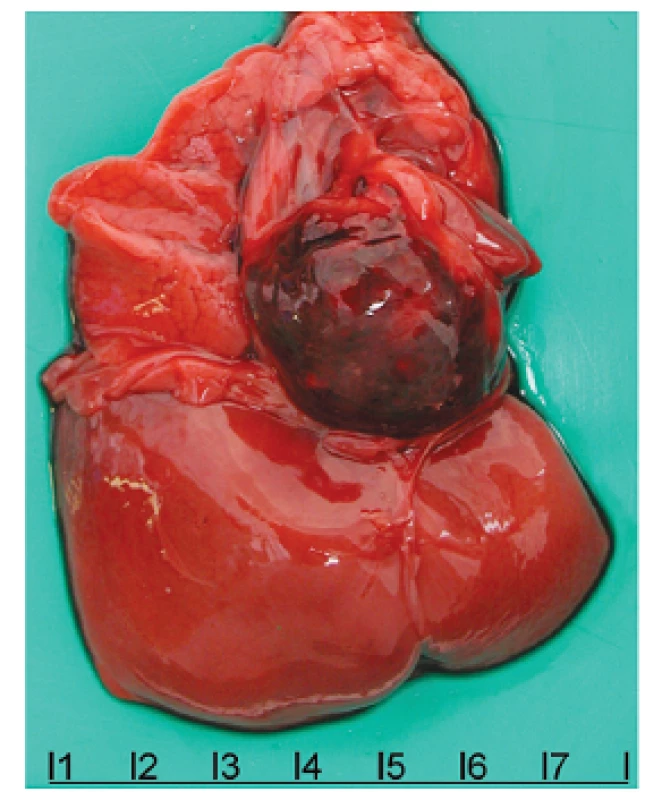
2. Intrapericardial teratoma. The tumor is fixed by a fibrous stalk to the aortic stem, otherwise it moves freely. Slightly displaced and compressed heart and left lung. 
3. Histological structure of the teratoma. Islet of cartilage in the left part, islet of hepatocytes in the right part, miscellaneous glandular structures in surrounding areas. HE, magnification 200x. 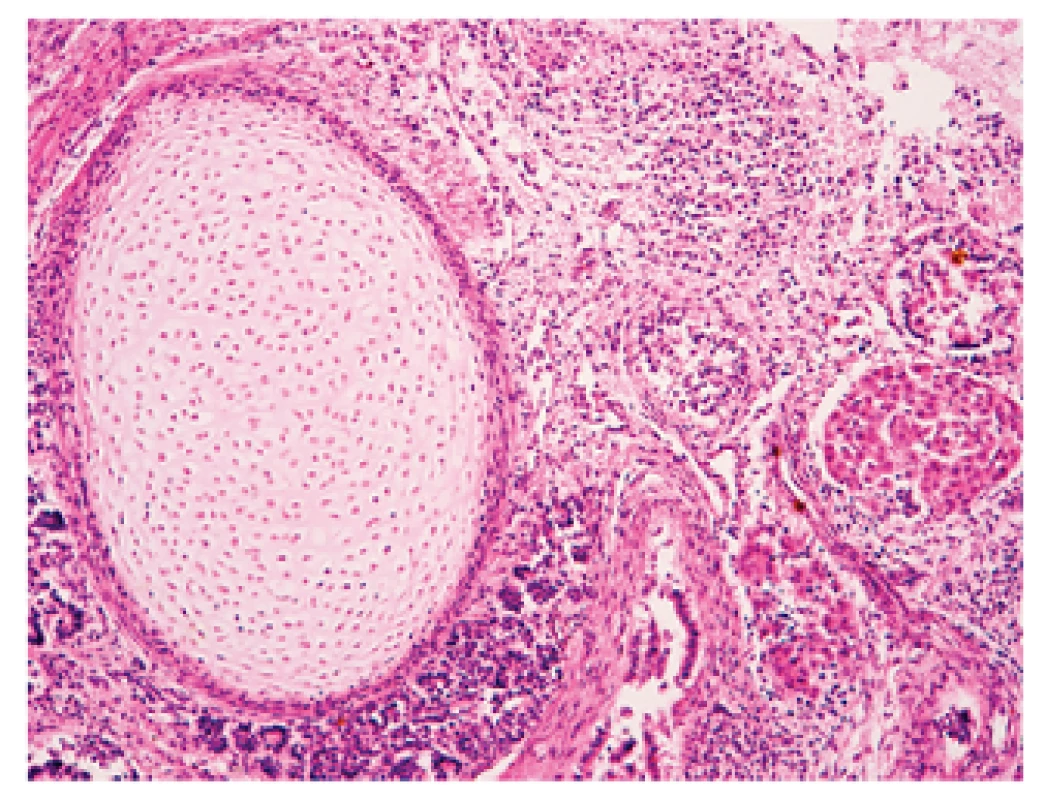
DISCUSSION
Before the first ultrasound intrauterine diagnosis was performed in 1983 (1), pericardial teratomas were identified as a cause of cardiorespiratory failure in the first neonatal hours or days. On ultrasound examination, the tumor is revealed as a well-circumscribed hyperechogenic mainly solid mass with cystic parts and sometimes focal calcifications, that is two or three times the size of a normal heart. As in our case, this mass is typically localized behind the right atrium and attached by a fibrous stalk to the aortic stem (1). Presumably because of its intrapericardial localization, it often escapes attention and is not displayed on ultrasound at all or only as a nonspecific slight pericardial extension. More frequently, the consequences of its presence in pericardium are detected as a pericardial effusion and hydrops. In contrast to our case, it is usually accompanied by polyhydramnion. The diagnosis is most often established around the 28th gestational week (1). The growing tumor is almost never found during routine scans during the first or second trimester of gravidity. Supposedly, these tumors grow and differentiate promptly between the 20th and 40th gestational week. The same was true in our case; it was not detected until the 23rd gestational week, despite early development of severe complications that led to intrauterine death.
The etiology of non-immune fetal hydrops encompasses miscellaneous cardiac anomalies, such as tumors, or more often, arrhythmias, malformations and cardiomyopathies. Pericardium teratoma is the second most common tumor, after rhabdomyoma (2). The differential diagnosis needs to consider fibromas, myxomas and hemangiomas. Non-tumourous lung lesions, e.g. cystic adenomatoid malformation and pulmonary sequestration, can imitate a heart tumor on an ultrasound.
Today a proportion of intrapericardial teratomas are diagnosed prenatally during routine ultrasound scans, which provide an opportunity to prevent complications that would otherwise develop before birth in approximately 50 % of cases. Intrauterine pericardiocentesis, which was first performed in 1992 (2), can avert imminent cardiac tamponade and development of hydrops, thus allowing a full-term birth. Because of the high risk of thoracic compression during vaginal delivery, a Caesarean operation is preferred with a tumor resection during the first postnatal days. Rarely, the surgery requires either a cardiopulmonary bypass or resection of the aortic wall. Considering the benign behavior of most teratomas, the surgery is both life saving and curative (3), which gives a significantly preferable prognosis for newborns with a intrapericardial tumor and calls into question the otherwise obvious indication for an abortion. An early prenatal diagnosis and the absence of fetal hydrops are favorable prognostic indicators.
Malignant teratomas arise in only 15 % of cases, and markedly worsen the prognosis, although an early tumor resection can possibly inhibit metastatic spread (3). However, very few cases have been described to date.
The histological structure of an intrapericardial teratoma does not differ from teratomas in other sites. Most of them grow out of pericardium and consist of endodermal (e.g. gastric, intestinal mucosa), mesodermal (e.g. bone, cartilage, fatty or fibrous tissue) and neuroectodermal structures (e.g. neuroglia) (4). To our knowledge, only one report of an intrapericardial teratoma containing pancreatic tissue with endocrine activity has been published so far (5). Malignant teratomas usually have a neuroectodermal origin.
Eventually, extremely rare cases of an intrapericardial teratoma were found in older children and even adults. The oldest patient, as far as we know, was a 51-year-old (6). Nevertheless, notwithstanding age, most of the cases described were females.
Generally, the incidence of a teratoma in the heart is rare but therefrom the intrapericardial localization is most frequent. Cases of a teratoma in a heart atrium or ventricle are very uncommon (7).
Adresa pro korespondenci:
MUDr. Helena Skálová
Ústav patologie 1. LF UK a VFN
Studničkova 2, 128 00 Praha 2
tel: +420224968711, +420605502654
fax: +420224911715
e-mail: helenaskalova1@seznam.cz
Sources
1. MacKenzie S, Loken S, Kalia N, et al. Intrapericardial teratoma in the perinatal period – Case report and review of the literature. Journal of Pediatric Surgery 2005; 40: E13–E18.
2. Pachy F, Raiffort C, Mechler C, Zilberman S, Mandelbrot L. Intrapericardial teratoma with hydrops leading to in utero demise. Prenatal Diagnosis 2007; 27 : 970–972.
3. Paw PT, Jamieson SW. Surgical Management of Intrapericardial Teratoma Diagnosed in Utero. The Annals of Thoracic Surgery 1997; 64 : 552–554.
4. Beghetti M, Prieditis M, Rebeyka IM, Mawson J. Intrapericardial teratoma. Circulation 1998; 97 : 1523–1524.
5. Ertugrul T, Dindar A., Elmaci TT, Onursal E, Kilicaslan I. An intrapericardial teratoma with endocrine function. J Cardiovasc Surg 2001; 42(6):781 – –783.
6. Gonzalez M, Krueger T, Schaefer SC, Ris HB, Perentes JY. Asymptomatic Intrapericardial Mature Teratoma. Ann Thorac Surg 2010; 89:e46–e47.
7. Gilbert-Barness E, Kapur RP, Oligny LL. Potter’s Pathology of the Fetus, Infant and Child, 2nd edition. Mosby Elsevier 2005; Vol.2 : 1061–1062.
Labels
Anatomical pathology Forensic medical examiner Toxicology
Article was published inCzecho-Slovak Pathology

2011 Issue 4-
All articles in this issue
- Gastrointestinal stromal tumor molecular diagnostics in relation to the prediction of a therapeutic response to targeted biological therapy
- Mollecular predictive markers of EGFR-targeted therapy in metastatic colorectal cancer
- Predictive diagnosis of HER2 in gastric adenocarcinoma
- Targeted therapy of melanoma: Fact or fiction ?
- News in the classification of pulmonary adenocarcinomas and potential prognostic and predictive factors in non-small lung cancer
- Clinical registers as a necessary support for personalized medicine Clinical registers as a necessary support for personalized medicine
- Giant cutaneous basal cell carcinoma of the head with intracranial propagation – a case report
- Acatholytic Variant of Squamous Carcinoma of the Breast. A Case Report and Review of Literature
- Carney complex
- Intrapericardial teratoma as a cause of fetal death – a case report
- Czecho-Slovak Pathology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Carney complex
- Predictive diagnosis of HER2 in gastric adenocarcinoma
- Giant cutaneous basal cell carcinoma of the head with intracranial propagation – a case report
- Acatholytic Variant of Squamous Carcinoma of the Breast. A Case Report and Review of Literature
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

