-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Critical complications of intestinal tuberculosis − a case report
Kritické komplikace specifického střevního zánětu − kazuistika
Tuberkulózní postižení střev je v rozvinutých zemích vzácné onemocnění, které postihuje zejména imigranty a imunokompromitované pacienty. Klinický obraz může imitovat nitrobřišní infekce, nádorová onemocnění či Crohnovu chorobu. Diferenciální diagnostika Crohnovy choroby a břišní tuberkulózy může být pro klinika a patologa svízelná, v obou případech se jedná o chronický granulomatózní zánět s podobnou symptomatologií. Prezentujeme případ 53letého pacienta s perforační peritonitidou při tuberkulóze střeva, u kterého byla původně mylně diagnostikována Crohnova choroba. Průběh choroby, rozsah a povaha nálezu byly v každé fázi léčby příčinou kritických komplikací. S touto zkušeností předáváme i doporučení: břišní tuberkulózu zvažovat v diferenciálně diagnostické rozvaze každého chronického střevního onemocnění.
Klíčová slova:
střevní tuberkulóza − Crohnova choroba − kritické komplikace
Authors: P. Bavor; P. Kocian; J. Hoch
Authors place of work: Department of Surgery, 2nd Faculty of Medicine, Charles University Prague and Motol University Hospital, Prague, Department Head: prof. J. Hoch, MD, PhD.
Published in the journal: Rozhl. Chir., 2015, roč. 94, č. 7, s. 293-296.
Category: Kazuistika
Summary
Intestinal tuberculosis is a rare disease in developed countries, affecting mainly immigrants and immunocompromised patients. Clinical presentation may mimic many other abdominal diseases such as intra-abdominal infections, tumors, and Crohn´s disease. Differential diagnosis of Crohn´s disease and intestinal tuberculosis poses a dilemma to clinicians and pathologists as both are chronic granulomatous disorders with similar clinical features. We report the case of a 53 year-old man presenting with perforated intestinal tuberculosis in which the initial diagnostic work-up suggested Crohn´s disease. The severity of the findings resulted in critical complications during the course of treatment. This case points out the need for awareness of intestinal tuberculosis in the differential diagnosis of chronic intestinal disease.
Key words:
intestine tuberculosis − Crohn´s disease − critical complicationsINTRODUCTION
Tuberculosis is a specific infectious disease with an incidence that has been documented since ancient Greece, as well as in the Roman Empire.
The etiological agent which causes tuberculosis is the Mycobacterium tuberculosis complex of the Mycobacterium species. Strains causing TB in humans include M. tuberculosis – the most frequent etiological agent, M. bovis, and M. africanum. Positive cultures for mycobacteria confirm the diagnosis of TB. The histological findings are typical, characterized by the presence of granulomas with central caseous necrosis. Worldwide, TB is the leading deathly infectious disease - one-third of the world is infected with TB, annually approximately 20 million people are infected and 3 million people die from this disease [1]. Despite hope that tuberculosis will be eradicated in developed countries, the incidence in the last two decades is rising and is considered a global threat by the World Health Organization. TB remains a health and social problem in developing countries; however, due to worldwide migration, population aging, alcoholism and coincidence with AIDS, it is gaining significance even in developed countries [2−4].
Besides dominating pulmonary manifestation, other organs and systems may be affected - pleura, lymph nodes, joints, bones, eyes, meninges, gastrointestinal and urogenital tracts [1]. TB of abdominal organs is much more common in developing countries. The source of infection is usually contaminated food, especially milk. A postprimary form also exists, which develops due to hematogenous dissemination during pulmonary TB [5−7]. Symptoms of patients with intestinal tuberculosis are similar to those with other forms of TB - fever, sweating, weight loss, loss of appetite, as well as gastrointestinal symptoms - abdominal pain, diarrhoea, bowel obstruction.
CASE REPORT
A 53-year-old male of Arabic ethnicity with Crohn’s disease affecting the terminal ileum and ascending colon diagnosed at another workplace was admitted to the Department of Internal Medicine for acute disease exacerbation. He was treated with mesalazine, corticosteroids, parenteral antibiotics and nutrition was ensured by nasojejunal tube. Inflammatory parameters decreased and his condition subjectively and objectively improved significantly. Due to a previous allergic reaction to contrast medium, an MR enteroclysis was planned instead of an abdominal CT. However, the improved condition was only temporary. The patient begun vomiting after almost every meal, suffered from loss of appetite, lost 5 kg in the last month. He had frequent watery stools without the presence of blood or mucous, non-specific abdominal pain in the epigastrium and hypogastrium and regular fevers exceeding 38 degrees Celsius, especially in the morning hours, chills and sweating. He was therefore readmitted to the Department of Internal Medicine. Elevation of inflammatory parameters, reactive thrombocytosis, microcytic anemia, hypochloremia, hyponatremia, elevation of cholestatic enzymes were confirmed. Due to the assumed acute exacerbation of Crohn’s disease, parenteral antibiotics and corticosteroids were administered along with parenteral nutrition. On the 5th day of this hospitalization, the abdominal pain worsened with signs of peritonitis. This was confirmed on native abdominal CT where findings of an inflammatory infiltrate in the right hypogastrium with pneumoperitoneum were described. After short preparation the patient underwent surgical revision. The cause of four-quadrant purulent peritonitis were multiple perforations of the small intestine. The oral portion of the first 50 cm of jejunum was intact, followed by a segment from 50 to 80 cm with three pin-point perforations in a terrain of bowl-like ulcerations (Fig. 1). Several other ulcerations had an intact serosa. From 110 cm the jejunum was part of an infiltrate located in the lower left quadrant. During bowel manipulation, two loops, which were connected by a wide fistula, fell apart. A similar situation was seen in the lower right quadrant, where the terminal ileum was growing into the abdominal wall and connected by fistulas. Because previous findings had confirmed Crohn’s disease, the procedure was aimed at preserving as much intestine as possible. A wedge resection with suture of the oral perforation and short resection of the jejunum containing the two distal perforations was performed along with excision and suture of the perforated bowel loops in the lower left quadrant and careful lavage and drainage of the abdominal cavity. Intensive care ensued, medication was adjusted after consultation with gastroenterologist.
Fig. 1. Operation findings during the first operation – “bowllike” ulcers in the jejunum with pin-point perforations 
On the third postoperative day, the patient’s condition rapidly worsened again. Due to circulatory and respiratory insufficiency and clinical findings on the abdomen, the patient was operated for the second time. Diffuse small bowel peritonitis was discovered with multiple perforations in the ulcerated regions extending throughout almost the entire small bowel with the exception of 50 cm of the oral portion (Fig. 2). The stigmata discovered during the first operation were now disintegrated together with a wide portion of the small intestine. A subtotal resection of the small intestine was performed along with a terminal jejunostomy orally and a caecostomy as a mucous fistula aborally. Due to the severe septic condition of the patient, he was transferred to the Department of Anesthesiology and Resuscitation postoperatively.
Fig. 2. Operation findings 3 days later – multiple extensive perforations with intestine disintegration 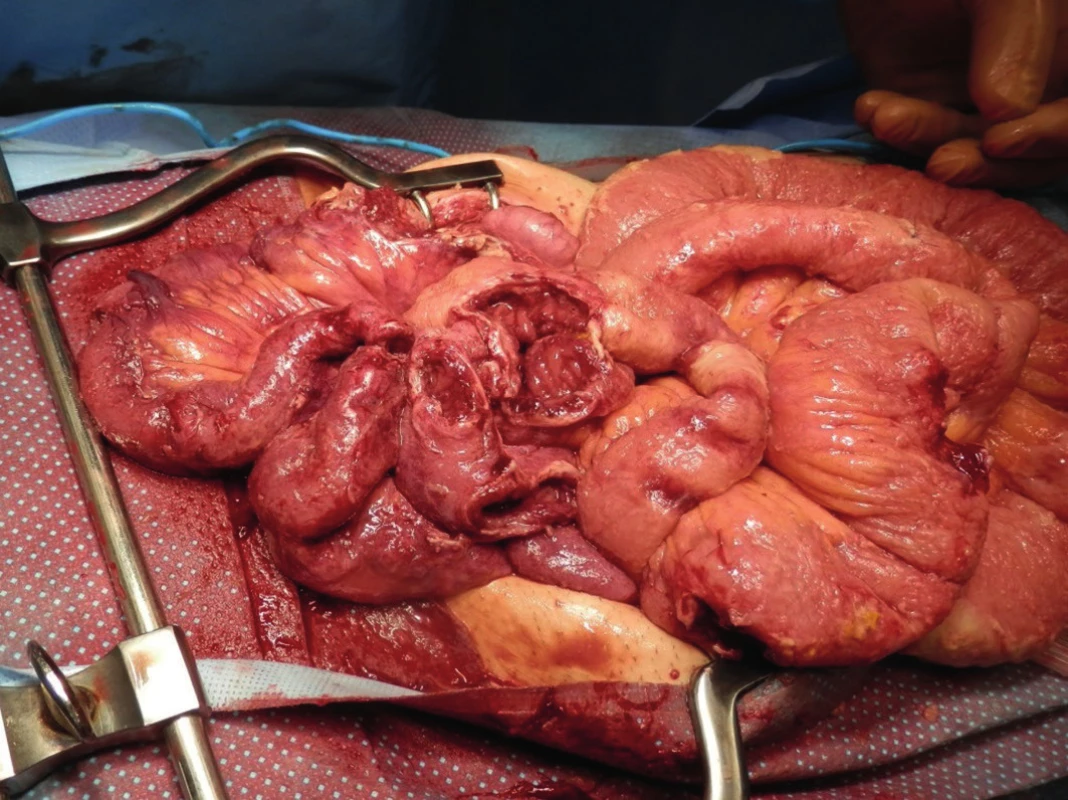
For the first time, findings on the small intestine and the rapid progression led us to consider that these changes may be caused by tuberculosis. This suspicion guided our subsequent actions. Histopathological findings confirmed granulomatous necrotizing tuberculous enteritis, cultivation samples revealed acid-resistant rods from the abdominal puncture, along with MRSA positive Staphylococcus aureus (Fig. 4,5). The originally negative findings on chest X-ray performed immediately prior to the first operation were amended to tuberculous infection (Fig. 3). The primary diagnosis of Crohn’s disease was amended to combined pulmonary and intestinal tuberculosis. After a pneumology consultation, intravenous antituberculosis therapy was initiated (Rifampin, Ciprofloxacin + Amikacin). Four days after the second operation, the patient was reoperated again due to a finding of hemoperitoneum, caused by arrosive bleeding from a branch of the mesenteric vein. Surgical intervention was successful and after stabilization, the patient was transferred from the Anesthesiology and Resuscitation Department to the Department of Infectious Diseases.
Fig. 3. X – Ray finding: TB infiltrates in both pulmonary fields 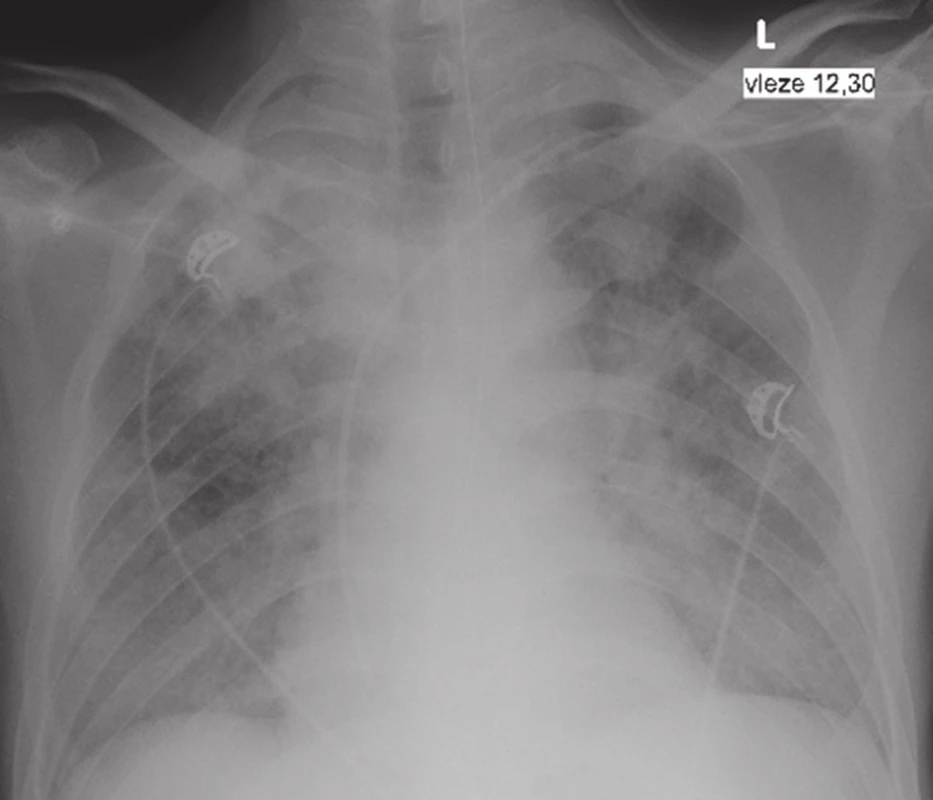
Fig. 4. Histological finding of intestinal TB – granuloma with central caseous necrosis. HE, magnified 200x 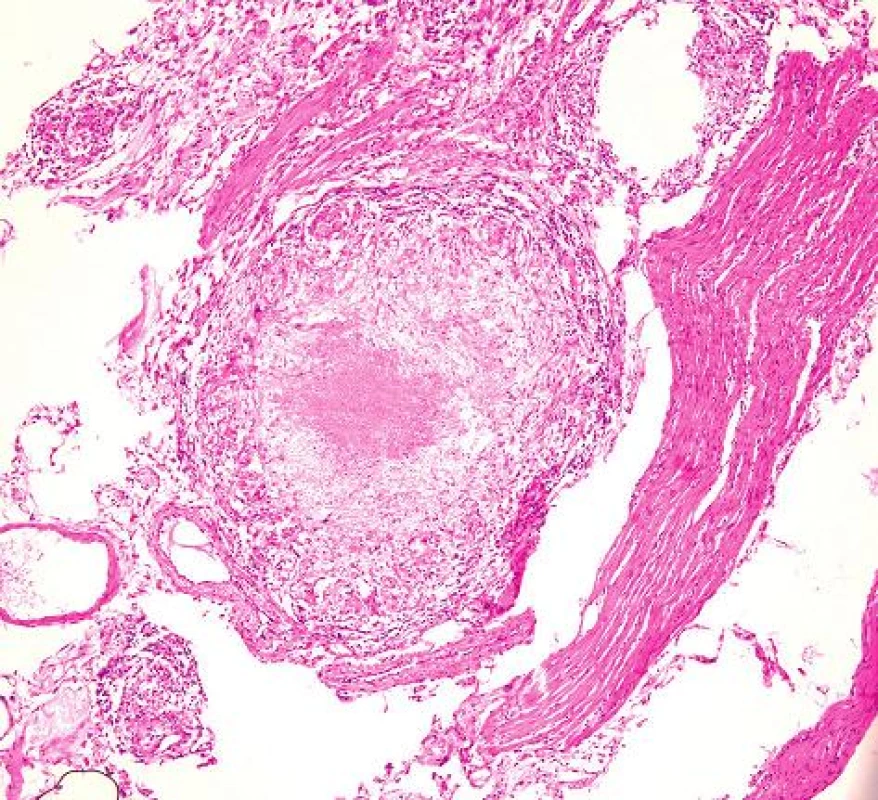
Fig. 5. TB bacterium in histological finding. HE, magnified 400x 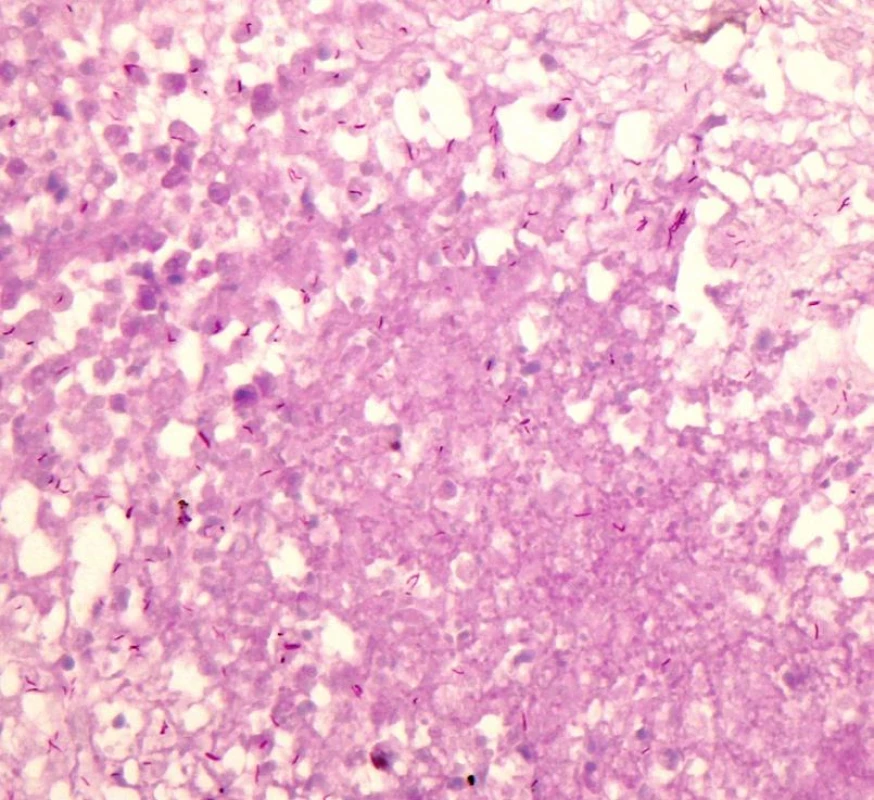
Resuscitation care continued in an isolated regime, antibiotic therapy was changed to Zyvoxid + Ciprofloxacin, antitubercolitics to Rifampin + Izoniazid i.v. and Streptomycin i.m. Ventilation support was gradually decreased and after 25 days the patient was extubated. The abdominal drains were removed, passage through the gastrointestinal tract was renewed and oral intake was begun. The only surgical complication was a seroma in the laparotomy. High output from the jejunostomy and malnutrition required continuing parenteral nutrition. Due to complications with antituberculosis therapy – elevation of obstruction enzymes and bilirubin - Rifampin + Izoniazid therapy was extended. Due to a possibly toxic effect of Streptomycin – vertigo development - this drug was terminated. After GI passage renewal, oral antituberculotics Sural and Pyrazinamide were added. Short bowel syndrome with malabsorption necessitated monitoring serum concentrations of therapeutic doses. After two months of treatment, the patient had repeatedly negative microscopic and culture findings. Isolation was terminated and antituberculotics were administered according to continuation phase guidelines. Due to the dominating short-bowel syndrome, the patient was transferred to the metabolic intensive care unit of our hospital to ensure proper realimentation.
DISCUSSION
Diagnosis and treatment of this relatively rare disease in our environment was accompanied by a number of critical complications. The patient was first hospitalized at the Department of Internal Medicine for activation of Crohn’s disease diagnosed at an ambulatory workplace and treated with corticosteroids and mesalazine based on the diagnosis established two months prior.
Complicating moments were as follows:
- Colonoscopy findings of the mucosa were evaluated as Crohn’s disease with ileocecal manifestation, but without bioptic verification. For an assumed complication of nonspecific bowel disease, the patient was treated with i.v. antibiotics and corticosteroids; parenteral and enteral nutrition was provided via jejunal tube. The patient’s improved condition was only temporary, no abdominal imaging examination was performed. Gastrointestinal symptomatology was probably so convincing, that not even periodic fevers, chills and sweating led to the search of an alternate etiology, including pulmonary, and a chest X-ray, which may have contributed to the diagnosis, was not performed. A complicating moment was the administration of corticosteroids during florid pulmonary and abdominal tuberculosis, which probably contributed to the progression of tuberculosis.
- Even a chest X-ray performed immediately prior to the surgical revision did not raise suspicion of pulmonary tuberculosis and described only infiltrative changes paracardially and in the right upper lung field.
- Diffuse purulent perforation peritonitis is in itself a critical abdominal catastrophe. The assumed diagnosis of Crohn’s disease led to a surgery aimed at preserving maximum bowel length with an anticipated regression of the infiltrates and ulcerations by intensifying drug therapy, including biological therapy.
- Intestinal TB was not suspected until the second operation, where multiple small bowel perforations and bowel disintegration were discovered. It was then that the chest X-ray was re-evaluated and pulmonary TB was described. Until this time, the patient was endangered by continued administration of corticosteroids, and the health care staff and everyone in the vicinity was at risk of infection.
- Treatment of such a critical patient with severe sepsis under controlled ventilation with a jejunostomy did not allow for adequate oral antituberculosis treatment.
- Toxic effects of the administered antituberculotics necessitated a change in medication, which resulted in an additional narrowing of the spectrum of suitable drugs.
- Loss of bowel with preservation of only a short segment of jejunum is an abdominal catastrophe and critical complication, which if survived, carries severe nutritional and metabolic consequences.
During the course of treatment, all of the above-mentioned moments and their combination presented a critical complication for the patient, and a risk for everyone around him in the period leading up to the correct diagnosis. Once tuberculosis was confirmed, it was extremely important to take into consideration how successful resuscitation of this patient with such serious intraabdominal findings may be and what is his prognosis. Due to these considerations and excellent interdisciplinary cooperation, the patient survived, tuberculosis was cured, and the patient was planned for restorative bowel surgery.
Great attention is currently being given to non-specific bowel diseases in both surgical and gastroenterological practices. Diagnostic procedures, conservative therapy and a surgical manual for the treatment of complications have been developed and elaborated. Specific bowel diseases are rare in our country, although their incidence has been rising in the past decades. Their incidence is often forgotten. Clinical presentation of non-specific inflammatory bowel disease and intestinal tuberculosis may be very similar [8−11]. If these diseases result in a surgical complication, the findings on imaging examinations as well as peroperative findings may be practically identical. The surgical treatment of specific and non-specific inflammatory bowel diseases may be very complicated. Despite attempts at preserving as much bowel as possible, resections may result in considerable loss of small or large intestine, sometimes requiring a terminal jejunostomy. The severity of the sepsis resulting from perforation peritonitis was increased due to the TB infection.
CONCLUSION
Not only the migration-related increasing incidence of TB, but also mistaking cases of abdominal manifestation with non-specific inflammatory bowel disease, should lead to the inclusion of this disease in the differential diagnosis of any suspected non-specific bowel disease.
List of abbreviations:
KZM – department of imaging methods
TB – tuberculosis
The authors wish to thank Dr. M. Grega and Dr. R. Chmelová, Department of Pathology and Molecular Medicine 2. LF UK and FN Motol for providing histological findings.
Conflict of Interests
The authors declare that they have not conflict of interest in connection with the emergence of and that the article was not published in any other journal.
MUDr. Petr Bavor
V Úvalu 84
150 00, Praha 5
e-mail: petr.bavor@fnmotol.cz
Zdroje
1. Toth A, Fackelmann J, Pigott W, et al. Tuberculosis prevention and treatment. Can Nurse 2004;100 : 27−30.
2. Al-Hajoj S, Shoukri M, Memish Z, et al. Exploring the sociodemographic and clinical features of extrapulmonary tuberculosis in Saudi Arabia. PLoS One 2015;10:e0101667.
3. Varghese B, Supply P, Shoukri M, et al. Tuberculosis transmission among immigrants and autochthonous populations of the eastern province of Saudi Arabia. PLoS One 2013;8:e77635.
4. Pročke M. Terminální ileitida: vždy jen Crohnova nemoc? ZDN. Přil Lék listy 2012;1 : 16-18.
5. McElvanna, K, Skelly RT, O´Neill C, et al. Miliary tuberculosis causing multiple intestinal perforations in an immigrant worker. Ulster Med J 2008;77 : 206−8.
6. Rondelli F, Finocchi L, Covarelli P, et al. Multiple intestinal perforations due to tuberculosis: a case report and review of the literature. Chir Ital 2009;61 : 397−9.
7. Mert A, Bilir M, Ozaras R, et al. A rare complication of miliary tuberculosis: intestinal perforation. Acta Chir Belg 2001;101 : 42−5.
8. Chatzicostas C, Koutroubakis IE, Tzardi M, et al. Colonic tuberculosis mimicking Crohn´s disease: case report. BMC Gastroenterol 2002;2 : 10.
9. Arhan M, Köksal AS, Ozin Y, et al. Colonic tuberculosis or Crohn´disease? An important differential diagnosis. Acta Gastroenterol Belg 2013;76 : 59−61.
10. Epstein D, Watermeyer G, Kirsch R. Review article: the diagnosis and management of Crohn´disease in populations with high-risk rates for tuberculosis. Aliment Pharmacol Ther 2007;25 : 1373−88.
11. Bártů Václava. Tuberkulóza - onemocnění stále aktuální. Postgraduální medicína 2008;4 : 360−3.
Štítky
Chirurgie všeobecná Ortopedie Urgentní medicína
Článek XV. Bedrnův denČlánek Pruritus ani
Článek vyšel v časopiseRozhledy v chirurgii
Nejčtenější tento týden
2015 Číslo 7- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
-
Všechny články tohoto čísla
- Rectal cancer. More or less radiation?
- Pruritus ani
- Profesor Čapov oslavil 60. jubileum
- Current status in the treatment of rectal cancer in the Czech Republic regarding the rate of complete pathological response after neoadjuvant therapy – PATOD C20 study 2011−2012
- SentiMag – the magnetic detection system of sentinel lymph nodes in breast cancer
- Acute bleeding into the GI tract – A surgical diagnosis?
- Critical complications of intestinal tuberculosis − a case report
- Endoscopic endonasal treatment of cerebrospinal fluid leak caused by clival fracture – a case report
- Heterotopic mesenteric ossification
- XV. Bedrnův den
- Rozhledy v chirurgii
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Pruritus ani
- SentiMag – the magnetic detection system of sentinel lymph nodes in breast cancer
- Heterotopic mesenteric ossification
- Endoscopic endonasal treatment of cerebrospinal fluid leak caused by clival fracture – a case report
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



