-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Migraine and risk of cardiovascular disease in women: prospective cohort study
Objective:
To evaluate the association between migraine and incident cardiovascular disease and cardiovascular mortality in women.Design:
Prospective cohort study among Nurses’ Health Study II participants, with follow-up from 1989 and through June 2011.Setting:
Cohort of female nurses in United States.Participants:
115 541 women aged 25-42 years at baseline and free of angina and cardiovascular disease. Cumulative follow-up rates were more than 90%.Main outcome measures:
The primary outcome of the study was major cardiovascular disease, a combined endpoint of myocardial infarction, stroke, or fatal cardiovascular disease. Secondary outcome measures included individual endpoints of myocardial infarction, stroke, angina/coronary revascularization procedures, and cardiovascular mortality.Results:
17 531 (15.2%) women reported a physician’s diagnosis of migraine. Over 20 years of follow-up, 1329 major cardiovascular disease events occurred and 223 women died from cardiovascular disease. After adjustment for potential confounding factors, migraine was associated with an increased risk for major cardiovascular disease (hazard ratio 1.50, 95% confidence interval 1.33 to 1.69), myocardial infarction (1.39, 1.18 to 1.64), stroke (1.62, 1.37 to 1.92), and angina/coronary revascularization procedures (1.73, 1.29 to 2.32), compared with women without migraine. Furthermore, migraine was associated with a significantly increased risk for cardiovascular disease mortality (hazard ratio 1.37, 1.02 to 1.83). Associations were similar across subgroups of women, including by age (<50/≥50), smoking status (current/past/never), hypertension (yes/no), postmenopausal hormone therapy (current/not current), and oral contraceptive use (current/not current).Conclusions:
Results of this large, prospective cohort study in women with more than 20 years of follow-up indicate a consistent link between migraine and cardiovascular disease events, including cardiovascular mortality. Women with migraine should be evaluated for their vascular risk. Future targeted research is warranted to identify preventive strategies to reduce the risk of future cardiovascular disease among patients with migraine.
Authors: Tobias Kurth 1,2,3; Anke C Winter 4; A. Heather Eliassen 3,5; Rimma Dushkes 1; Kenneth J Mukamal; Eric B Rimm 3,5,6; Walter C Willett 3,6; Joann E Manson 1,3,5; Kathryn M Rexrode 1
Authors place of work: Institute of Public Health, Charité - Universitätsmedizin, D-10117 Berlin, Germany 1; Division of Preventive Medicine, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA 2; Department of Epidemiology, Harvard T. H. Chan School of Public Health, Boston, MA, USA 3; Division of Public Health Sciences, Department of Surgery, Washington University School of Medicine, Saint Louis, MO, USA 4; Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA 5; Department of Nutrition, Harvard T. H. Chan School of Public Health, Boston, MA, USA 6
Published in the journal: BMJ 2016, 353:i2610
Category: Research
doi: https://doi.org/10.1136/bmj.i2610© 2016 BMJ Publishing Group Ltd
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.Summary
Objective:
To evaluate the association between migraine and incident cardiovascular disease and cardiovascular mortality in women.Design:
Prospective cohort study among Nurses’ Health Study II participants, with follow-up from 1989 and through June 2011.Setting:
Cohort of female nurses in United States.Participants:
115 541 women aged 25-42 years at baseline and free of angina and cardiovascular disease. Cumulative follow-up rates were more than 90%.Main outcome measures:
The primary outcome of the study was major cardiovascular disease, a combined endpoint of myocardial infarction, stroke, or fatal cardiovascular disease. Secondary outcome measures included individual endpoints of myocardial infarction, stroke, angina/coronary revascularization procedures, and cardiovascular mortality.Results:
17 531 (15.2%) women reported a physician’s diagnosis of migraine. Over 20 years of follow-up, 1329 major cardiovascular disease events occurred and 223 women died from cardiovascular disease. After adjustment for potential confounding factors, migraine was associated with an increased risk for major cardiovascular disease (hazard ratio 1.50, 95% confidence interval 1.33 to 1.69), myocardial infarction (1.39, 1.18 to 1.64), stroke (1.62, 1.37 to 1.92), and angina/coronary revascularization procedures (1.73, 1.29 to 2.32), compared with women without migraine. Furthermore, migraine was associated with a significantly increased risk for cardiovascular disease mortality (hazard ratio 1.37, 1.02 to 1.83). Associations were similar across subgroups of women, including by age (<50/≥50), smoking status (current/past/never), hypertension (yes/no), postmenopausal hormone therapy (current/not current), and oral contraceptive use (current/not current).Conclusions:
Results of this large, prospective cohort study in women with more than 20 years of follow-up indicate a consistent link between migraine and cardiovascular disease events, including cardiovascular mortality. Women with migraine should be evaluated for their vascular risk. Future targeted research is warranted to identify preventive strategies to reduce the risk of future cardiovascular disease among patients with migraine.Introduction
Migraine is a primary headache disorder that affects approximately one fifth of the general US population for at least part of their lives, and women are affected three to four times more often than men.1 2 3 Migraine, specifically migraine with aura, has been consistently associated with increased risk of stroke, including both ischemic and hemorrhagic subtypes.4 5 Although the pathophysiology of migraine has close links to the vascular system, the mechanisms by which migraine increases risk of stroke remain unclear.6 7 Potential mechanisms for an association between migraine and stroke include endovascular dysfunction,8 9 increased thrombogenic susceptibility,10increased prevalence of vascular risk factors,11 shared genetic markers,12 13 cortical spreading depolarization,14 15and inflammation.16 17
As most of these mechanisms also increase the risk of other cardiovascular disease events, migraine may be viewed as a marker of increased risk for any vascular disease event. However, as the one year prevalence of migraine peaks in midlife whereas the incidence of cardiovascular events increases exponentially with age, links between migraine and any cardiovascular disease are not easily identifiable. Long follow-up, particularly of younger populations, is needed to study this association. Few prospective studies have reported an association between migraine and any cardiovascular disease events,18 19 20 21 including ischemic heart disease and cardiovascular death.18 20 21
Because of the high prevalence of migraine, any association between migraine and cardiovascular disease would have a substantial effect on public health. We thus aimed to evaluate the association of migraine with total and specific cardiovascular disease events as well as cardiovascular disease specific mortality in the Nurses’ Health Study II, one of the largest prospective cohort studies on health in younger women, aged 25 to 42 at baseline.
Methods
Study population
Established in 1989, the Nurses’ Health Study II is an ongoing prospective cohort study of 116 430 female registered nurses in the United States who were 25-42 years old at baseline. Information on reproductive factors, lifestyle factors, and medical history was collected through a self administered questionnaire at baseline and has been updated every two years through follow-up questionnaires. The cumulative response rate based on person time is more than 90%. For the purpose of this analysis, we included follow-up from baseline through June 2011. We excluded 889 women who reported cardiovascular disease at baseline (angina, a coronary revascularization procedure, myocardial infarction, or stroke) from our analyses, leaving 115 541 women free of angina or any symptomatic cardiovascular disease for our analyses.
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of the study. No patients were asked to advise on interpretation or writing up of results. Results of the study will be disseminated to patients’ organizations and via the webpage of the Nurses’ Health Study (http://www.nurseshealthstudy.org).
Assessment of migraine
On the baseline (1989) and two follow-up questionnaires (1993 and 1995), women were asked to indicate whether a physician had diagnosed them as having migraine. Person time status for having a migraine started whenever migraine was first reported. Agreement between self reported migraine and 2004 International Headache Society criteria was high in another comparable cohort of female health professionals.22 Information on migraine aura, migraine frequency, or migraine specific drugs was not available.
Ascertainment of cardiovascular disease events
Every two years, women reported any incident cardiovascular disease event on the follow-up questionnaires and then completed a supplemental questionnaire confirming the event. Self reported information on cardiovascular disease was confirmed through review of medical record or supporting information by a physician who was blinded to the exposure status and the specific research question under study. Deaths were identified by reports from next of kin, from postal authorities, or by searching the National Death Index. At least 98% of deaths among the Nurses’ Health Study II participants were identified using these approaches.23 Causes of death were confirmed by review of autopsy reports, medical records, and death certificates.
The occurrence of non-fatal myocardial infarction was confirmed if symptoms met World Health Organization criteria, which require typical symptoms plus either diagnostic electrocardiographic findings or elevated cardiac enzyme concentrations.24 If medical records were unavailable, we considered myocardial infarctions probable when additional confirmatory information was provided by the participant. Information on angina and coronary revascularization procedures (percutaneous transluminal coronary angioplasty or coronary artery bypass grafting surgery) was self reported, and we included only events that occurred before a manifest cardiovascular disease event.
A non-fatal stroke diagnosis was confirmed, according to National Survey of Stroke criteria, if the participant had a new focal neurologic deficit with sudden or rapid onset that persisted for more than 24 hours.25 We excluded cerebrovascular pathology due to infection, trauma, or malignancy, as well as “silent” strokes discovered only by radiologic imaging. Radiology reports of brain imaging (computed tomography or magnetic resonance imaging) were available in 89% of those with medical records. We classified strokes as ischemic stroke (thrombotic or embolic occlusion of a cerebral artery), hemorrhagic stroke (subarachnoid and intraparenchymal hemorrhage), or stroke of probable/unknown subtype (a stroke was documented but the subtype could not be ascertained owing to medical records being unobtainable).
Fatal cardiovascular disease was defined as fatal coronary heart disease, fatal stroke, or fatal cardiovascular disease. Fatal coronary heart disease was defined as ICD-9 (international classification of diseases, ninth revision) codes 410-412 and was considered confirmed if fatal coronary heart disease was confirmed via medical records or autopsy reports or if coronary heart disease was listed as the cause of death on the death certificate and there was prior evidence of coronary heart disease in the medical records. We designated as probable those cases in which coronary heart disease was the underlying cause on the death certificates but no prior knowledge of coronary heart disease was indicated and medical records concerning the death were unavailable. Similarly, we used ICD-9 codes 430-434 to define fatal stroke and followed the same procedures to classify cases of confirmed or probable fatal stroke. Lastly, fatal cardiovascular disease was defined by ICD-9 codes 390-458.
Our primary outcome measure was major cardiovascular disease, a combined endpoint of myocardial infarction, stroke, or fatal cardiovascular disease (fatal stroke, fatal myocardial infarction, and fatal coronary heart disease). We chose this composite outcome as it has been used as outcome in previous studies,18 26 and it follows guidelines on prevention of all cardiovascular disease to capture the full impact of risk factors and cardiovascular health.27 We further assessed the following secondary outcome measures: total myocardial infarction, which was defined as fatal or non-fatal myocardial infarction; total stroke, which included all fatal and non-fatal stroke cases (ischemic, hemorrhagic, and undetermined subtypes); angina/coronary revascularization procedure; and cardiovascular disease mortality.
Statistical analyses
We calculated person time from the return date of the 1989 questionnaire until the date of diagnosis of cardiovascular disease, date of death, or end of follow-up (June 2011), whichever occurred first. We used Cox proportional hazards models with age and two year follow-up cycle as timescale to evaluate the association between migraine and the various outcomes. We calculated age adjusted and multivariable adjusted hazard ratios and corresponding 95% confidence intervals. The multivariable adjusted models controlled for age (continuous), elevated cholesterol (yes/no), diabetes (yes/no), hypertension (yes/no), body mass index (<25, 25-<30, ≥30), smoking status (never, past, current), alcohol consumption (0, 0-14.9, ≥15 g/day), physical activity (metabolic equivalent of tasks (METs) in fifths) (continuous), postmenopausal hormone use (never, past, current), menopausal status (premenopausal, postmenopausal, dubious), ever used oral contraceptive (never, past, current), aspirin use (<2 days/week, ≥2 days/week), acetaminophen (paracetamol) use (<2 days/week, ≥2 days/week), non-steroidal anti-inflammatory drug use (<2 days/week, ≥2 days/week), and family history of myocardial infarction before the age of 60 (yes/no). We adjusted for all the covariates in the models in a time varying fashion on the basis of information available on each of the biennial questionnaires (1991 to 2009).
We evaluated effect modification by age (<50/≥50), smoking status (current/past/never), hypertension (yes/no), postmenopausal hormone therapy (current/not current), and oral contraceptive use (current/not current). We tested effect modification by including an interaction term for migraine and the potential effect modifier in the outcome models.
We tested the proportional hazards assumption by including an interaction term for migraine status and the logarithm of follow-up time for the primary outcomes in age adjusted models. We found no statistically significant violation. In sensitivity analyses, we repeated the analyses on the basis of migraine information provided at baseline only.
We had 3.1% missing information on all covariates and used a missing variable indicator to account for this lack of information in our multivariable models. In sensitivity analyses, we used multiple imputation (proc mi) to account for missing information and also ran a model excluding all missing information.
We used SAS 9.3 for all analyses. All P values were two sided, and we considered a P value of less than 0.05 to be statistically significant.
Results
Of the 115 541 women in this study, 17 531 (15.2%) reported a physician’s diagnosis of migraine at baseline in 1989. An additional 6389 women newly reported a physician’s diagnosis on subsequent questionnaires and were classified having migraine during follow-up. Women with migraine were more likely to have an unfavorable cardiovascular risk factor profile, including hypertension, hypercholesterolemia, family history of myocardial infarction, body mass index of 30 or above, and current smoking status. They were also more likely to use aspirin, acetaminophen, and non-steroidal anti-inflammatory drugs (table 1).
Tab. 1. Age standardized baseline characteristics (1989) according to migraine status in Nurses’ Health Study II (n=115 541). Values are percentages unless stated otherwise 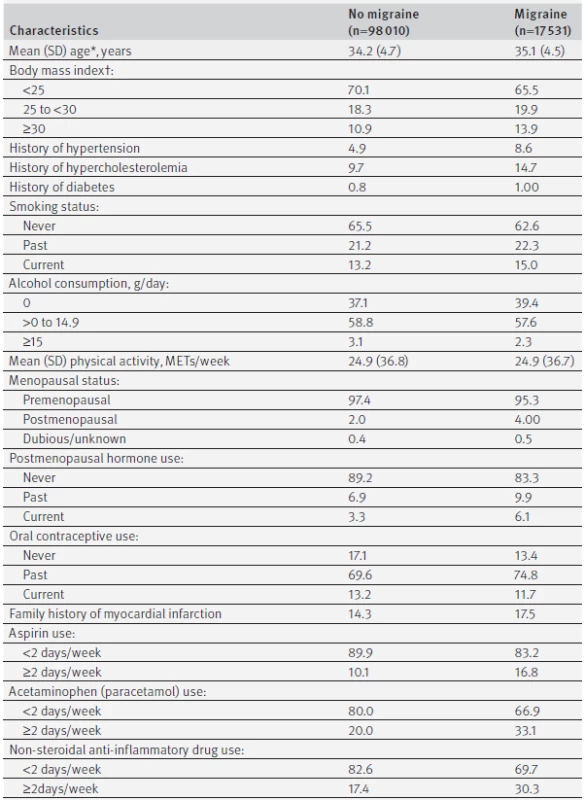
Percentages may not add to a 100% because of rounding or missing values. MET=metabolic equivalent. *Value is not age adjusted. †Calculated as weight in kilograms divided by height in meters squared. Table 2 summarizes the associations between migraine and various cardiovascular outcomes. During follow-up, 1329 major cardiovascular disease events (678 total myocardial infarctions, 651 total strokes, and 203 angina/coronary revascularization procedures) occurred. A total of 223 deaths due to cardiovascular disease occurred. Compared with women without migraine, those with a self reported physician’s diagnosis of migraine had a multivariable adjusted hazard ratio of 1.50 (95% confidence interval 1.33 to 1.69) for developing major cardiovascular disease. Findings were significant for all evaluated individual outcomes, and the highest estimates were seen for stroke (hazard ratio 1.62, 1.37 to 1.92) and angina/coronary revascularizations (1.73, 1.29 to 2.32).
Tab. 2. Age adjusted and multivariable adjusted hazard ratios for cardiovascular disease outcomes according to migraine status in Nurses’ Health Study II (n=115 541) 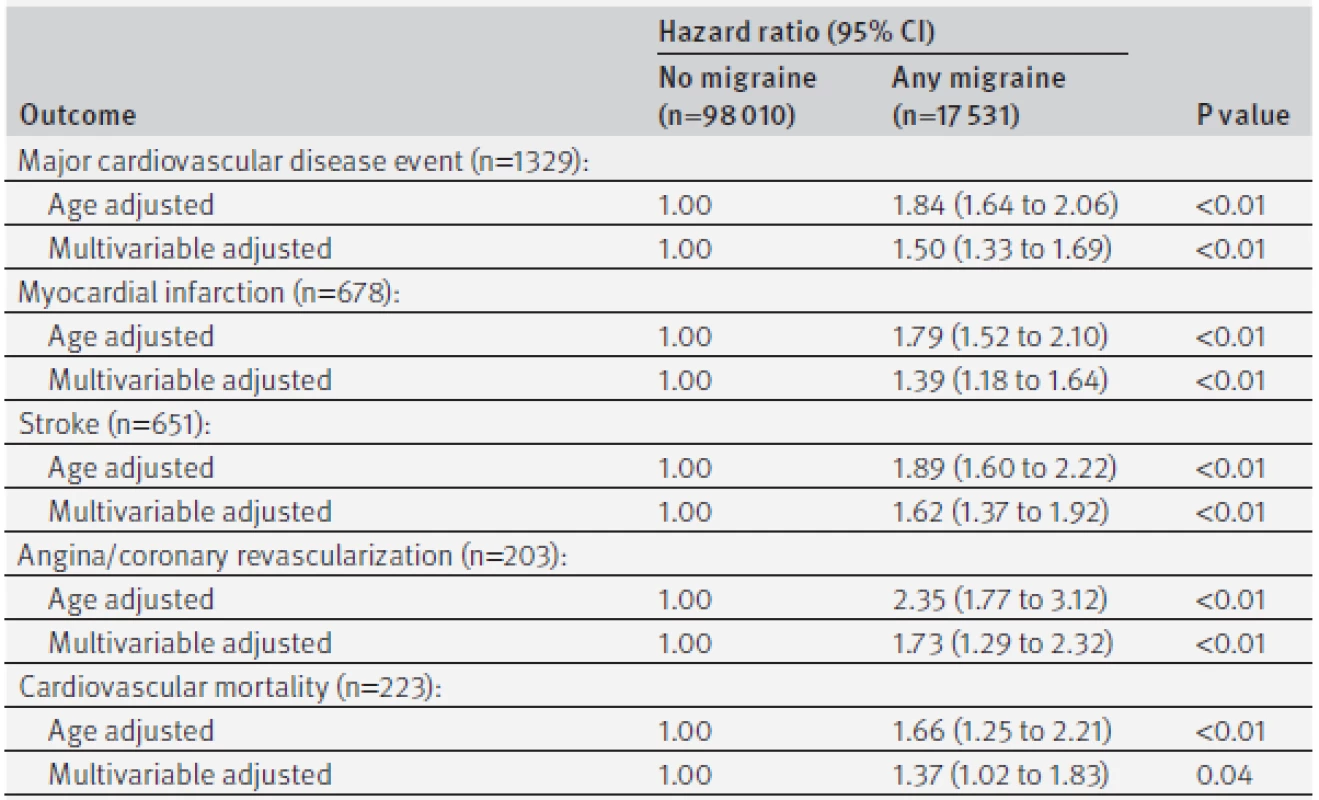
Multivariable models were adjusted for age (continuous), elevated cholesterol (yes/no), diabetes (yes/no), hypertension (yes/no), body mass index (<25, 25-29.9, ≥30), smoking status (never, past, current), alcohol consumption (0, >0-14.9, ≥15g/day), physical activity (METs in fifths), postmenopausal hormone use (never, past, current), menopausal status (premenopausal, postmenopausal, dubious), ever used oral contraceptive (never, past, current), aspirin use (<2, ≥2 days/week), acetaminophen (paracetamol) use (<2, ≥2 days/week), non-steroidal anti-inflammatory drug use (<2, ≥2 days/week), and family history of myocardial infarction before age of 60 (yes/no). The associations between migraine and cardiovascular disease outcomes (major cardiovascular disease, total myocardial infarction, and total stroke) were not modified by age (<50/≥50) (P for interaction all≥0.34), current postmenopausal hormone use (P for interaction all≥0.57), current oral contraceptive use (P for interaction all≥0.84), current smoking status (P for interaction all≥0.26), or hypertension (P for interaction all≥0.37). In sensitivity analyses, we restricted analysis to women with a report of migraine at baseline. The multivariable adjusted hazard ratios were 1.57 (1.38 to 1.77) for major cardiovascular disease, 1.77 (1.49 to 2.11) for total stroke, and 1.39 (1.17 to 1.66) for total myocardial infarction. The results of the association between migraine and major cardiovascular disease were very similar when we used multiple imputation (hazard ratio 1.50, 1.33 to 1.71) or when we excluded missing information (1.53, 1.35 to 1.74).
Discussion
In this large, prospective cohort study of female nurses aged 25 to 42 at inclusion who were free of cardiovascular disease at the start of follow-up and with more than 20 years of follow-up, we found consistent associations between migraine and cardiovascular disease events. We found an approximately 50% increased risk for major cardiovascular disease. This association persisted after adjustment for traditional vascular risk factor and was apparent for myocardial infarction, stroke, and coronary artery procedures as well as for angina. We also found an increased risk of cardiovascular disease mortality.
Comparison with other studies
Most studies evaluating the association between migraine and vascular events have been limited to ischemic stroke.4 28 Some studies have reported an association between migraine and cardiovascular disease.18 19 20 21Results of our study are in line with findings from the Women’s Health Study,18 another large prospective cohort study among female health professionals aged 45 or older at inclusion. In the Women’s Health Study, migraine was associated with an increased risk of major cardiovascular disease events (hazard ratio 1.42, 95% confidence interval 1.16 to 1.074), including cardiovascular disease mortality (1.63, 1.07 to 2.50). In the Women’s Health Study, the increased risk was apparent only for women who reported migraine with aura. In our study, information on aura was not available.
In a matched cohort study of 11 541 patients with migraine who were aged 18 to 45 years and an equal number of controls from the Taiwan National Health Insurance database, Wang and colleagues reported an increased risk of ischemic heart disease for people with migraine (hazard ratio 2.50, 1.78 to 3.52).20 The Reykjavik Study, which included 18 725 men and women, showed very similar results for the association between overall migraine and cardiovascular disease mortality.21 After adjustment for potential confounders, participants with any indication of migraine had a 16% increased risk of dying from any cause (hazard ratio 1.16, 1.04 to 1.29). This risk was stronger for people with migraine with aura (hazard ratio 1.21, 1.12 to 1.30) and was higher for mortality from cardiovascular disease (1.27, 1.13 to 1.43) compared with people without headache. Results from the American Migraine Prevalence and Prevention study also indicate an increased risk of cardiovascular disease events. In this population based case-control study of 6102 patients with migraine and 5243 controls, migraine overall was associated with a relative risk for myocardial infarction of 2.16 (1.70 to 2.76) and for total stroke of 1.54 (1.16 to 2.05).19
Two studies have found an association between migraine with aura and angina but not myocardial infarction.29 30The lack of association with myocardial infarction may be related to shorter follow-up time. In our data, women with migraine had an increased risk for myocardial infarction, as well as for angina and coronary revascularization procedures.
Many studies have focused on the evaluation of potential modifying factors and on the identification of a subgroup of patients with migraine who are at high risk for developing a subsequent stroke. Studies have consistently found that the association between migraine and stroke was observable only among younger people and was stronger among women.28 Among women, several studies have focused on the role of smoking and oral contraceptive use.2831 32 In particular, the combination of smoking and oral contraceptive use among young women with migraine with aura markedly increased the risk of ischemic stroke, reaching a 10-fold increase for current cigarette smokers and oral contraceptives users.33 However, for overall vascular risk status, several studies indicate that the association between migraine and ischemic stroke is apparent only among those with a low cardiovascular risk profile.33 34
Studies on modifying effects of other cardiovascular disease events are sparse. Findings of the Women’s Health Study indicate that migraine with aura and an increased vascular risk profile resulted in a higher risk of incident myocardial infarction.34 However, the event rate among women with migraine with aura was still too small to robustly evaluate the role of individual vascular risk factors, including postmenopausal hormone use.
Potential biological mechanisms
Several mechanisms that have been implied for migraine have also been linked with increased risk of cardiovascular disease, such as increased thrombogenic susceptibility,10 shared genetic markers,12 13 and inflammation processes.16 17 Our findings confirm results of other studies that women with migraine have a higher prevalence of vascular risk factors, such as hypertension, higher body mass index, and hypercholesterolemia.11 19 However, as all studies evaluating the association between migraine and cardiovascular disease have controlled for these factors, the association between migraine and cardiovascular disease is unlikely to be explained by this. Evidence suggests that the pathophysiology of migraine can also be viewed in part as a systemic disorder affecting the endovascular system.9 35 36 37 38 39
Strengths and limitations of study
Our study has several strengths, including the prospective design, large number of participants and outcome events, long follow-up, high participation rate, standardized evaluation of migraine and cardiovascular disease risk factors, confirmation of outcomes by physician’s review, and the homogeneous nature of the cohort (all were nurses), which may reduce confounding by factors such as access to medical care.
Several limitations should be considered when interpreting our results. Firstly, physician diagnosed migraine status was self reported, leading to potential misclassification. In addition, people with mild migraines may not have reported symptoms to a clinician and thus not received a diagnosis. Because of the prospective design, however, such misclassification would probably result in underestimation of relative risks and would be unlikely to explain the observed association pattern. Furthermore, a previous report in a comparable study of female health professionals showed that self reported migraine had good agreement with the second edition of the International Classification of Headache Disorders,22 and our prevalence of migraine is close to that reported in other population based studies.18 40 41 Secondly, we had no information on the presence or absence of migraine aura, and migraine with aura has been suggested to be the subgroup carrying most of the risk of cardiovascular disease.4 18 Furthermore, no information on frequency of migraine or migraine specific information was available. Thirdly, residual confounding—for example, by markers of inflammation or genetic factors10 12 13 —remains a potential alternative explanation, as our data are observational. Finally, participants in this study were all nurses aged 25 to 42 at baseline and mostly white, so generalizability to other populations might be limited. However, we have no reason to believe that that the biological mechanisms by which migraine might be associated with vascular events and mortality would be different in other populations of women.
Implications of findings
The results of our study support the findings of other population based studies linking migraine with increased risk of cardiovascular disease.18 19 20 Although most studies link migraine with aura with increased risk of ischemic stroke,4 28 emerging evidence indicates that this risk extends to other cardiovascular disease as well. Our data support consideration of a history of migraine as a marker for increased risk of any cardiovascular disease event.
To date, no clear mechanisms have been identified that could explain the increased risk of cardiovascular disease and mortality among patients with migraine, and no data exist on whether prevention of migraine attacks reduces these risks. Data from the National Health and Nutrition Examination Survey and results of a randomized clinical trial provide initial evidence that the combination of a statin and vitamin D may reduce the burden of migraine,42 43which may be explained by the anti-inflammatory effects of these drugs. Future targeted research, such as on whether statins and vitamin D reduce the burden of migraine and cardiovascular disease, is urgently warranted to provide answers to patients and their treating physicians.
Conclusions
Results of this large, prospective cohort study among women support the hypothesis that migraine is a marker for increased risk of any cardiovascular events. Given the high prevalence of migraine in the general population, an urgent need exists to understand the biological processes involved and to provide preventive solutions for patients.
Contributors
TK and ACW contributed equally to the study. TK, ACW, and KMR were responsible for the study concept and design. KJM, EBR, WCW, JEM, and KMR were involved in data acquisition. All authors were involved in analysis and interpretation of data. TK, ACW, and KMR drafted the manuscript, and all authors revised it critically for important intellectual content. TK, ACW, RD, and KMR had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. TK and ACW are the guarantors.
Funding
This study had no specific funding. The Nurses' Health Study II is supported by grants from the National Institutes of Health (HL-088521, HL-34594, CA-050385, CA-176276). The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no support from any organization for the submitted work; TK has received investigator initiated research funding from the French National Research Agency, the US National Institutes of Health, and the University of Bordeaux and has received honorariums from the BMJ and Cephalalgia for editorial services; ACW is supported by funds from Washington University School of Medicine, the Barnes-Jewish Hospital Foundation, and Siteman Cancer Center and has received funding from the Craig H Neilsen Foundation and the National Institutes of Health; AHE, KJM, EBR, WCW, JEM, and KMR receive funding by grants from the National Institutes of Health; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval
The Nurses’ Health Study II was approved by the institutional review board of the Brigham and Women’s Hospital, Boston, MA, and the return of the completed self administered questionnaire was considered to imply informed consent.
Data sharing
No additional data available.
Transparency
The lead authors affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Accepted 25 April 2016
Published 31 May 2016
Correspondence to:
T Kurth
Zdroje
1 Stovner Lj, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007;27 : 193-210. doi:10.1111/j.1468-2982.2007.01288.x.
2 Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33 : 629-808. doi:10.1177/0333102413485658.
3 Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache 2015;55 : 21-34. doi:10.1111/head.12482.
4 Spector JT, Kahn SR, Jones MR, Jayakumar M, Dalal D, Nazarian S. Migraine headache and ischemic stroke risk: an updated metaanalysis. Am J Med 2010;123 : 612-24. doi:10.1016/j.amjmed.2009.12.021.
5 Sacco S, Ornello R, Ripa P, Pistoia F, Carolei A. Migraine and hemorrhagic stroke: a meta-analysis. Stroke 2013;44 : 3032-8. doi:10.1161/STROKEAHA.113.002465.
6 Kurth T, Chabriat H, Bousser M-G. Migraine and stroke: a complex association with clinical implications. Lancet Neurol 2012;11 : 92-100. doi:10.1016/S1474-4422(11)70266-6.
7 Mawet J, Kurth T, Ayata C. Migraine and stroke: in search of shared mechanisms. Cephalalgia 2015;35 : 165-81. doi:10.1177/0333102414550106.
8 Napoli R, Guardasole V, Zarra E, et al. Vascular smooth muscle cell dysfunction in patients with migraine. Neurology 2009;72 : 2111-4. doi:10.1212/WNL.0b013e3181aa53ce.
9 Liman TG, Bachelier-Walenta K, Neeb L, et al. Circulating endothelial microparticles in female migraineurs with aura. Cephalalgia 2015;35 : 88-94. doi:10.1177/0333102414529671.
10 Tietjen GE, Al-Qasmi MM, Athanas K, Utley C, Herial NA. Altered hemostasis in migraineurs studied with a dynamic flow system. Thromb Res 2007;119 : 217-22. doi:10.1016/j.thromres.2005.12.020.
11 Scher AI, Terwindt GM, Picavet HSJ, Verschuren WM, Ferrari MD, Launer LJ. Cardiovascular risk factors and migraine: the GEM population-based study. Neurology 2005;64 : 614-20. doi:10.1212/01.WNL.0000151857.43225.49.
12 Malik R, Freilinger T, Winsvold BS, et al. International Headache Genetics Consortium METASTROKE Collaboration of the International Stroke Genetics Consortium. Shared genetic basis for migraine and ischemic stroke: A genome-wide analysis of common variants. Neurology 2015;84 : 2132-45. doi:10.1212/WNL.0000000000001606.
13 Schürks M, Buring JE, Ridker PM, Chasman DI, Kurth T. Genetic determinants of cardiovascular events among women with migraine: a genome-wide association study. PLoS One 2011;6:e22106. doi:10.1371/journal.pone.0022106.
14 Eikermann-Haerter K. Spreading depolarization may link migraine and stroke. Headache 2014;54 : 1146-57. doi:10.1111/head.12386.
15 Dreier JP, Reiffurth C. The stroke-migraine depolarization continuum. Neuron 2015;86 : 902-22. doi:10.1016/j.neuron.2015.04.004.
16 Waeber C, Moskowitz MA. Migraine as an inflammatory disorder. Neurology 2005;64(Suppl 2):S9-15. doi:10.1212/WNL.64.10_ suppl_2.S9.
17 Longoni M, Ferrarese C. Inflammation and excitotoxicity: role in migraine pathogenesis. Neurol Sci 2006;27(Suppl 2):S107-10. doi:10.1007/s10072-006-0582-2.
18 Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA 2006;296 : 283-91. doi:10.1001/jama.296.3.283.
19 Bigal ME, Kurth T, Santanello N, et al. Migraine and cardiovascular disease: a population-based study. Neurology 2010;74 : 628-35. doi:10.1212/WNL.0b013e3181d0cc8b.
20 Wang Y-C, Lin C-W, Ho Y-T, Huang YP, Pan SL. Increased risk of ischemic heart disease in young patients with migraine: a population-based, propensity score-matched, longitudinal follow-up study. Int J Cardiol 2014;172 : 213-6. doi:10.1016/j.ijcard.2014.01.005.
21 Gudmundsson LS, Scher AI, Aspelund T, et al. Migraine with aura and risk of cardiovascular and all cause mortality in men and women: prospective cohort study. BMJ 2010;341:c3966. doi:10.1136/bmj.c3966.
22 Schürks M, Buring JE, Kurth T. Agreement of self-reported migraine with ICHD-II criteria in the Women’s Health Study. Cephalalgia 2009;29 : 1086-90. doi:10.1111/j.1468-2982.2008.01835.x.
23 Stampfer MJ, Willett WC, Speizer FE, et al. Test of the National Death Index. Am J Epidemiol 1984;119 : 837-9.
24 Rose GA, Blackburn H, Gillum RF, et al. Cardiovascular survey methods.World Health Organization, 1982.
25 Walker AE, Robins M, Weinfeld FD. The National Survey of Stroke. Clinical findings. Stroke 1981;12(Suppl 1):I13-44.
26 Kurth T, Gaziano JM, Cook NR, et al. Migraine and risk of cardiovascular disease in men. Arch Intern Med 2007;167 : 795-801. doi:10.1001/archinte.167.8.795.
27 Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women–2011 update: a guideline from the american heart association. Circulation 2011;123 : 1243-62. doi:10.1161/CIR.0b013e31820faaf8.
28 Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ 2009;339:b3914. doi:10.1136/bmj.b3914.
29 Sternfeld B, Stang P, Sidney S. Relationship of migraine headaches to experience of chest pain and subsequent risk for myocardial infarction. Neurology 1995;45 : 2135-42. doi:10.1212/WNL.45.12.2135.
30 Rose KM, Carson AP, Sanford CP, et al. Migraine and other headaches: associations with Rose angina and coronary heart disease. Neurology 2004;63 : 2233-9. doi:10.1212/01.WNL.0000147289.50605.DC.
31 Oral contraceptives and stroke in young women. Associated risk factors. JAMA 1975;231 : 718-22. doi:10.1001/jama.1975.03240190022010.
32 Tzourio C, Tehindrazanarivelo A, Iglésias S, et al. Case-control study of migraine and risk of ischaemic stroke in young women. BMJ 1995;310 : 830-3. doi:10.1136/bmj.310.6983.830.
33 MacClellan LR, Giles W, Cole J, et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke 2007;38 : 2438-45. doi:10.1161/STROKEAHA.107.488395.
34 Kurth T, Schürks M, Logroscino G, Gaziano JM, Buring JE. Migraine, vascular risk, and cardiovascular events in women: prospective cohort study. BMJ 2008;337:a636. doi:10.1136/bmj.a636.
35 Liman TG, Neeb L, Rosinski J, et al. Peripheral endothelial function and arterial stiffness in women with migraine with aura: a case-control study. Cephalalgia 2012;32 : 459-66. doi:10.1177/0333102412444014.
36 González-Quintanilla V, Toriello M, Palacio E, et al. Systemic and cerebral endothelial dysfunction in chronic migraine. A case-control study with an active comparator. Cephalalgia 2016;36 : 552-60. doi:10.1177/0333102415607857.
37 Totaro R, Marini C, De Matteis G, Di Napoli M, Carolei A. Cerebrovascular reactivity in migraine during headache-free intervals. Cephalalgia 1997;17 : 191-4. doi:10.1046/j.1468-2982.1997.1703191.x.
38 Vanmolkot FH, Van Bortel LM, de Hoon JN. Altered arterial function in migraine of recent onset. Neurology 2007;68 : 1563-70. doi:10.1212/01.wnl.0000260964.28393.ed.
39 Rose KM, Wong TY, Carson AP, Couper DJ, Klein R, Sharrett AR. Migraine and retinal microvascular abnormalities: the Atherosclerosis Risk in Communities Study. Neurology 2007;68 : 1694-700. doi:10.1212/01.wnl.0000261916.42871.05.
40 Launer LJ, Terwindt GM, Ferrari MD. The prevalence and characteristics of migraine in a population-based cohort: the GEM study. Neurology 1999;53 : 537-42. doi:10.1212/WNL.53.3.537.
41 Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001;41 : 646-57. doi:10.1046/j.1526-4610.2001.041007646.x.
42 Buettner C, Burstein R. Association of statin use and risk for severe headache or migraine by serum vitamin D status: a cross-sectional population-based study. Cephalalgia 2015;35 : 757-66. doi:10.1177/0333102414559733.
43 Buettner C, Nir R-R, Bertisch SM, et al. Simvastatin and vitamin D for migraine prevention: A randomized, controlled trial. Ann Neurol 2015;78 : 970-81. doi:10.1002/ana.24534.
Štítky
Stomatologie
Článek vyšel v časopiseBMJ
Nejčtenější tento týden
2016 Číslo i2610- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Orální lichen planus v kostce: Jak v praxi na toto multifaktoriální onemocnění s různorodými symptomy?
- Význam ústní sprchy pro čištění mezizubních prostor
- MIH – komplexní problém s nutností komplexního přístupu
- Benzydamin v léčbě zánětů v dutině ústní
Nejčtenější v tomto čísle
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




