-
Medical journals
- Career
Guidelines for autopsy investigation of sudden cardiac death
Authors: Cristina Basso 1; Margaret Burke 2; Paul Fornes 3; Patrick J Gallagher 4; Rosa Henriques De Gouveia 5; Mary Sheppard 6; Gaetano Thiene 1; Allard Van Der Wal 7
Authors‘ workplace: University of Padua Medical School, Padua, Italy 1; Department of Histopathology, Harefield Hospital, UK 2; Department of Pathology, Hopital Européen G. Pompidou, Paris, France 3; Department of Pathology, Southampton University Hospital, UK 4; Department of Pathology, Hospital de Santa Cruz, Lisbon, Portugal 5; Department of Pathology, Royal Brompton Hospital, London, UK 6; Pathology, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands 7
Published in: Čes.-slov. Patol., 46, 2010, No. 2, p. 43-48
Category:
Overview
Athough sudden cardiac death is one of the most important mode of death in Western Countries, pathologists and public health physicians have not given this problem the attention it deserves. New methods of preventing potentially fatal arrhythmias have been developed, and the accurate diagnosis of the causes of sudden cardiac death is now of particular importance. Pathologists are responsible for determining the precise cause of sudden death but there is considerable variation in the way in which they approach this increasingly complex task. The Association for European Cardiovascular Pathology developed guidelines, which represent the minimum standard that is required in the routine autopsy practice for the adequate assessment of sudden cardiac death, including not only a protocol for heart examination and histological sampling, but also for toxicology and molecular investigation. Our recommendations apply to university medical centres, regional and district hospitals and all types of forensic medicine institutes. If a uniform method of investigation is adopted throughout the European Union, this will lead to improvements in standards of practice, allow meaningful comparisons between different communities and regions and, most importantly, permit future trends in the patterns of disease causing sudden death to be monitored.
Key words:
Autopsy – Guidelines – Protocol – Sudden cardiac deathS laskavým svolením nakladatelství Springer přetiskujeme článek publikovaný ve Virchows Archiv (2008), Vol. 452, s. 11–18.
Introduction
Sudden cardiac death (SCD) is the leading mode of death in all communities of the United States and of the European Union, but its precise incidence is unknown. Internationally accepted methods of death certification do not include a specific category of SCD. Estimates for the United States range from 250,000 to 400,000 adult people dying suddenly each year due to cardiovascular causes with an overall incidence of 1 to 2/1,000 population per year [13, 18, 29]. A task force of the European Society of Cardiology has adopted the incidence ranges from 36 to 128 deaths per 100,000 population per year [3, 19]. More than 60% of these are the result of coronary heart disease. Among the general population of adolescents and adults younger than the age of 30 years, the overall risk of SCD is 1/100,000 and a wider spectrum of diseases can account for the final event [9].
The major difficulties in interpreting epidemiological data on sudden death are the lack of standardization in death certificate coding and the variability in the definition of sudden death. Sudden death has been defined as “a natural, unexpected fatal event occurring within one hour from the onset of symptoms in an apparently healthy subject or whose disease was not so severe as to predict an abrupt outcome” [14]. This well describes many witnessed deaths in the community or in emergency departments. It is less satisfactory in pathological practice where autopsies may be requested on patients whose deaths were not witnessed, occurred during sleep or at an unknown time before their bodies were discovered. Under the latter circumstances, it is probably more satisfactory to assume that the death was sudden if the deceased was known to be in good health 24 h before death occurred [28]. Moreover, for practical purposes, a death can be classified as sudden if a patient is resuscitated after cardiac arrest, survives on life support for a limited period of time and then dies due to irreversible brain damage.
Pathologists are responsible for determining the precise cause of sudden death but there is considerable variation in the way in which they approach this increasingly complex task. A variety of book chapters, professional guidelines and articles have described how pathologists should investigate sudden death [1, 5, 11, 20, 23, 27]. However, there is little consistency among centres, even in individual countries. In this report, we describe the minimum standard that is required in the routine autopsy practice for the adequate assessment of SCD in the general population, excluding sudden infant death syndrome. Our recommendations apply to university medical centres, regional and district hospitals and all types of forensic medicine institutes. If a uniform method of investigation is adopted throughout the European Union, this will lead to improvements in standards of practice, allow meaningful comparisons between different communities and regions and, most importantly, permit future trends in the patterns of disease causing sudden death to be monitored
The role of the autopsy in sudden death
To establish or consider:
- whether the death is attributable to a cardiac disease or to other causes of sudden death;
- the nature of the cardiac disease, and whether the mechanism was arrhythmic or mechanical;
- whether the cardiac condition causing sudden death may be inherited, requiring screening and counselling of the next of kin;
- the possibility of toxic or illicit drug abuse and other unnatural deaths.
Clinical information relevant to the autopsy
In practice the amount of information that is available before autopsy is variable. Any potential source of information should be interrogated (e.g. family members, general practitioner, etc), preferentially before autopsy is carried out. Ideally, the following information is required:
- age, gender, occupation, lifestyle (especially alcohol or smoking), usual pattern of exercise or athletic activity;
- circumstances of death: date, time interval (instantaneous or <1 h), place of death (e.g. at home, at work, in hospital, at recreation), circumstances (at rest, during sleep, during exercise—athletic or non-athletic—, during emotional stress), witnessed or un-witnessed, any suspicious circumstances (carbon monoxide, violence, traffic accident, etc);
- medical history: general health status, previous significant illnesses (especially syncope, chest pain, and palpitations, particularly during exercise, myocardial infarction, hypertension, respiratory and recent infectious disease, epilepsy, asthma, etc), previous surgical operations or interventions, previous ECG tracings and chest X-rays, results of cardiovascular examination, laboratory investigations (especially lipid profiles);
- prescription and non-prescription medications;
- family cardiac history: ischaemic heart disease and premature sudden death, arrhythmias, inherited cardiac diseases;
- ECG tracing taken during resuscitation, serum enzyme and troponin measurements.
The autopsy procedure
All sudden death autopsies should be sequential structured examinations. They should specifically address the major causes of extra-cardiac and cardiac sudden death. Principles and rules relating to autopsy procedures should adhere to the Recommendations on the Harmonisation of Medico - Legal Autopsy Rules produced by the Committee of Ministers of the Council of Europe [5].
External examination of the body
- Establish body weight and height (to correlate with heart weight and wall thickness [16, 21, 22]).
- Check for recent intravenous access, intubation, ECG pads, defibrillator and electrical burns, drain sites and traumatic lesions;
- Check for implantable cardioverter defibrillator (ICD)/ pacemaker; if in situ, see MDA Safety Notice 2002 for safe removal and interrogation [17].
Full autopsy with sequential approach to the causes of sudden death
Exclusion of non-cardiac causes of sudden death
Any natural sudden death can be considered cardiac in origin after the exclusion of non-cardiac causes. Thus, a full autopsy with sequential approach should be always performed to exclude common and un-common extra-cardiac causes of sudden death, especially:
- Cerebral (e.g. sub-arachnoid or intra-cerebral haemorrhage, etc)
- Respiratory (e.g. asthma, anaphylaxis, etc)
- Acute haemorrhagic shock (e.g. ruptured aortic aneurysm, peptic ulcer, etc)
- Septic shock (Waterhouse–Friderichsen syndrome)
Search for cardiac causes of sudden death
Many cardiovascular diseases can cause SCD, either through an arrhythmic mechanism (electrical SCD) or by compromising the mechanical function of the heart (mechanical SCD). These disorders may affect the coronary arteries, the myocardium, the cardiac valves, the conducting system, the intra-pericardial aorta or the pulmonary artery, the integrity of which is essential for a regular heart function (Table 1).
1. SCD at postmortem Cardiovascular substrates 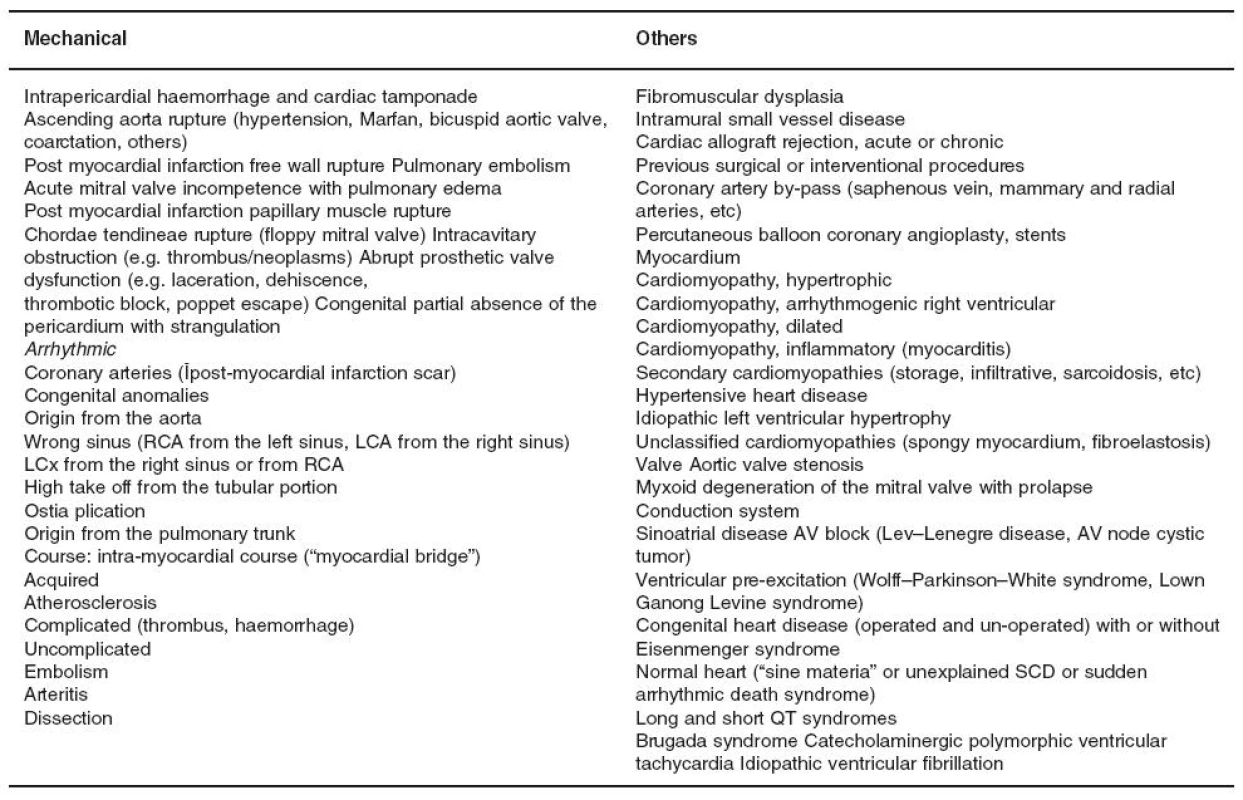
AV atrioventricular; LCA left coronary artery; LCx left circumflex branch; RCA right coronary artery The standard gross examination of the heart
- Check the pericardium, open it and explore the pericardial cavity.
- Check the anatomy of the great arteries before transecting them 3 cm above the aortic and pulmonary valves.
- Check and transect the pulmonary veins. Transect the superior vena cava 2 cm above the point where the crest of the right atrial appendage meets the superior vena cava (to preserve sinus node). Transect the inferior vena cava close to the diaphragm.
- Open the right atrium from the inferior vena cava to the apex of the appendage. Open the left atrium between the pulmonary veins and then to the atrial appendage. Inspect the atrial cavities, the inter-atrial septum and determine whether the foramen ovale is patent. Examine the mitral and tricuspid valves (or valve prostheses) from above and check the integrity of the papillary muscles and chordae tendineae.
- Inspect the aorta, the pulmonary artery and the aortic and pulmonary valves (or valve prosthesis) from above.
- Check
coronary arteries:
- (a) examine the size, shape, position, number and patency of the coronary ostia;
- (b) assess the size, course and “dominance” of the major epicardial arteries;
- (c) make multiple transverse cuts at 3 mm intervals along the course of the main epicardial arteries and branches such as the diagonal and obtuse marginal, and check patency;
- (d) heavily calcified coronary arteries can sometimes be opened adequately with sharp scissors. If this is not possible, they should be removed intact, decalcified and opened transversely;
- (e) coronary artery segments containing a metallic stent should be referred intact to labs with facilities for resin embedding and subsequent processing and sectioning;
- (f) coronary artery bypass grafts (saphenous veins, internal mammary arteries, radial arteries, etc) should be carefully examined with transverse cuts. The proximal and distal anastomoses should be examined with particular care. Side branch clips or sutures may facilitate their identification, particularly when dealing with internal mammary grafts.
- Make a complete transverse (short-axis) cut of the heart at the mid-ventricular level and then parallel slices of ventricles at 1 cm intervals towards the apex and assess these slices carefully for morphology of the walls and cavities.
- Once
emptied of blood, note the followingmeasurements:
- (a) Total heart weight: assess weight of heart against tables of normal weights by age, gender and body weight [16, 21, 22];
- (b) Wall thickness: inspect endocardium, measure thickness of mid cavity free wall of the left ventricle, right ventricle and of the septum (excluding trabeculae) against tables of normal thickness by age, gender and body weight [16, 21, 22];
- (c) Heart dimensions: the transverse size is best calculated as the distance from the obtuse to the acute margin in the posterior atrioventricular sulcus. The longitudinal size is obtained from a measurement of the distance between the crux cordis and the apex of the heart on the posterior aspect.
- Dissect the basal half of the heart in the flow of blood and complete examination of atrial and ventricular septa, atrioventricular valves, ventricular inflows and outflows, and semi-lunar valves. In case of ECG documented ventricular pre-excitation, the atrioventricular rings should be maintained intact.
The standard histologic examination of the heart Myocardium: take mapped labelled blocks from a representative transverse slice of the ventricles to include the free wall of the left ventricle (anterior, lateral and posterior), the ventricular septum (anterior and posterior), and the free wall of the right ventricle (anterior, lateral and posterior), and right ventricular outflow tract and one block from each atria. In addition, any area with significant macroscopic abnormalities should be sampled. H & E and a connective tissue stain (van Gieson, trichrome or Sirius red) are standard. Other special stains and immunohistochemistry should be performed as required.
Coronary arteries: in the setting of coronary artery disease, most severe focal lesions should be sampled for histology in labelled blocks and stained as before.
Other cardiac samples (such as valvular tissue, pericardium and aorta) as indicated.
If the clinical history or ECG tracing suggest a conduction abnormality, conduction system investigation by serial sections technique should be performed.
Electron microscopy investigation If there is the suspicion of rare cardiomyopathies (mitochondrial, storage, infiltrative, etc) a small sample of myocardium (1 mm) should be fixed in 2.5% glutaraldehyde for ultrastructural examination.
Referral of hearts to specialised centres Best practice is that the entire heart is retained and sent to specialized centres. The referring pathologist should complete steps 1 – 5 of the standard gross examination of the heart, make a transverse apical section of the heart and empty the heart of blood. Tissues, blood and other fluids for toxicology and molecular pathology should be taken before fixing the heart in formalin 10% (see “Molecular pathology” below). If the heart cannot be retained, it is essential that extensive photographic documentation is made, indicating where individual blocks are taken.
Other tissues for histological examination
Specimens from the main other organs should be taken routinely and stained with H & E and a connective tissue stain.
Further laboratory tests
Molecular or toxicologic studies may be required at some stage in the future. To this end, appropriate storage of autopsy tissues/fluids is essential in SCD autopsies. If these laboratory tests are needed and no on-site facilities are available, the stored material should be sent to specialised labs established at regional or national levels.
Toxicology In investigating out-of-hospital deaths, the question is almost always raised of whether toxic substances are involved. Depending on the circumstances surrounding the death and toxicological data, the manner of death can be natural, accidental or criminal. Even when the heart is found to be abnormal at gross and/or microscopic examination, and death occurred suddenly, the question still remains of whether a substance may have triggered the death, acting as additional factor to the anatomic substrate. Particularly in the athlete and in the young, doping and recreational drugs may precipitate SCD. Moreover, SCD may be caused by medications with cardiac side effects, such as neuroleptic or even cardiac drugs. The proper selection, collection, and submission of specimens for toxicological analyses is mandatory if analytical results are to be accurate and scientifically useful. The types and minimum amounts of tissue specimens and fluids needed for toxicological evaluation are frequently dictated by the analytes that must be identified and quantitated. For the purpose of sudden death investigation, the following amounts are adapted from the Guidelines of the Society of Forensic Toxicologists and the American Academy of Forensic Sciences [24]: heart blood 25 ml, peripheral blood from femoral veins 10 ml, urine 30–50 ml, bile 20–30 ml (when urine is not available). All samples are stored at 4°C. A lock of hair (100–200 mg) should be cut from the back head (or from the pubic hair when head hair is not available). Toxicological analyses should be quantitative.
Molecular pathology Molecular studies of SCD include both detection of viral genomes in inflammatory cardiomyopathies, and gene mutational analysis in both structural and nonstructural genetically determined heart diseases [1, 7, 8, 26]. For these purposes, 10 ml of EDTA blood and 5 g of heart and spleen tissues are either frozen and stored at –80°C, or alternatively stored in RNA later at 4°C for up to 2 weeks.
Formulation of a diagnosis and the clinicopathological summary
The report should conclude with a clear clinicopathological summary (epicrisis). As far as possible this should relate the pathological findings to the clinical history, the circumstances of the death and any investigation performed close to the time of the death. There will be inevitable variations in the format of the death certificate between the states of the European Union.
In the majority of SCDs, a clear pathological cause can be identified, albeit with varying degrees of confidence. Wherever possible, the most likely underlying cause should be stated and the need for familial clinical screening and genetic analysis clearly indicated [4, 27].
It is important to accept that different degrees of certainty exist in defining the cause–effect relationship between the cardiovascular substrate and the sudden death event. Table 2 lists the commonest substrates of SCD, classifying each as certain, highly probable or uncertain. In the probable, and especially the uncertain categories, each case should be considered on its individual merits. The clinical history and the circumstances of death may influence the decision making process.
2. Certainity of diagnosis in SCD autopsies 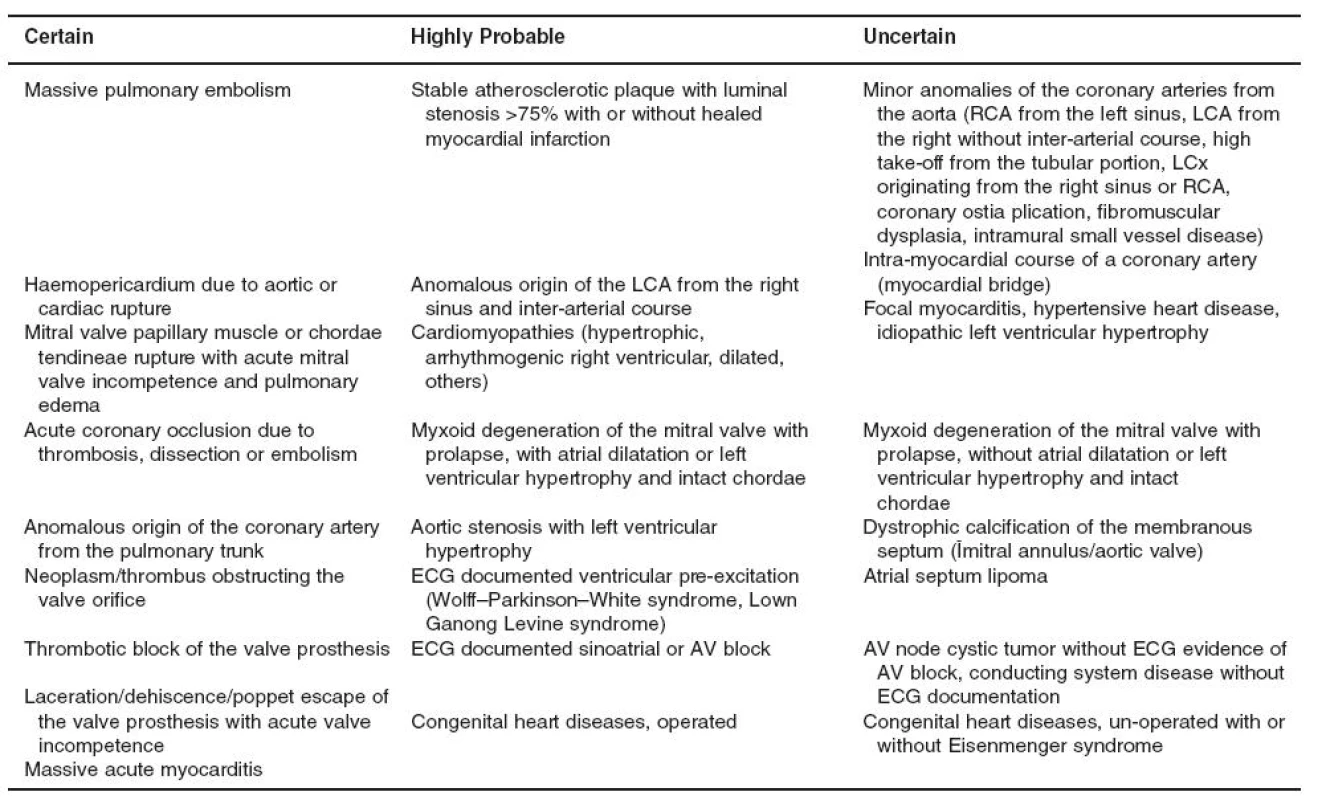
AV atrioventricular; ECG electrocardiogram; LCA left coronary artery; LCx left circumflex branch; RCA right coronary artery Finally, there are myocardial diseases in which the border between physiological and pathological changes is poorly defined. Some of these diagnostic gray zones are described in Table 3 [2, 6, 15, 25]. In everyday practice, pathologists should make a detailed macroscopic and microscopic description of their findings without implying a cause and effect relationship. If there is real doubt as to whether the changes are physiological or pathological, an expert opinion should be sought (see “Referral of hearts to specialised centres” above).
3. The gray zone between physiological and pathological changes in myocardial disease 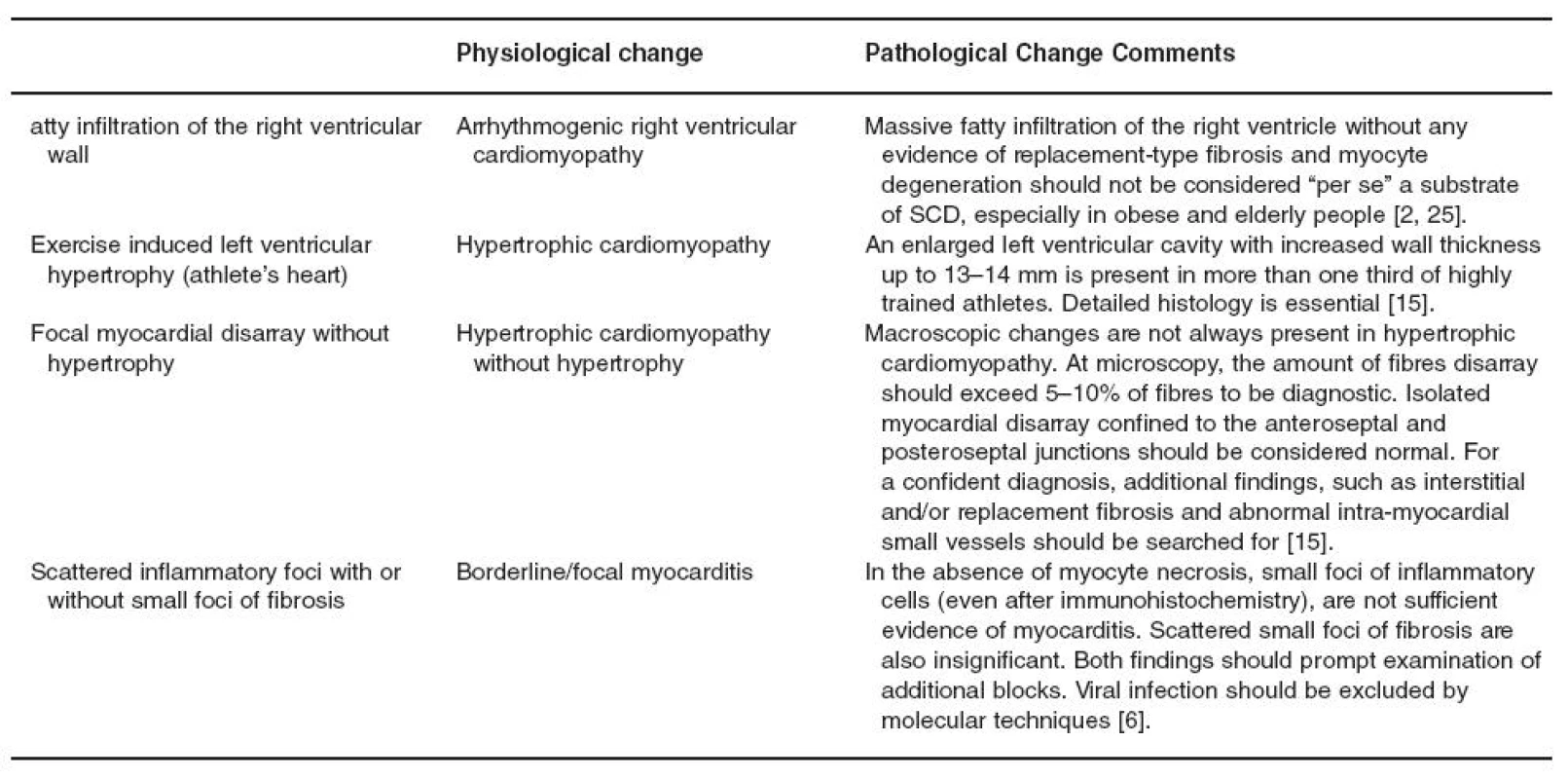
Deaths that remain unexplained after careful macroscopic, microscopic and laboratory investigation should be classified as sudden arrhythmic death syndrome [4, 10, 12]. We strongly suspect that the numbers of these unexplained deaths have been under-estimated in the past. There is increasing evidence that SCD in these instances might be due to inherited ion channel disorders, such as long QT and short QT syndromes, Brugada syndrome and catecholaminergic polymorphic ventricular tachycardia, which present with well-defined abnormalities of basal or effort ECG. In this setting, the availability of ECG tracings may be crucial for the diagnosis and molecular studies are essential. First degree relatives should undergo clinical screening and subsequent genetic analysis when indicated.
Conclusions
Although SCD is one of the most important mode of death in the European Union, pathologists and public health physicians have not given this problem the attention it deserves. Ventricular fibrillation is the nightmare of Western countries’ populations. New methods of preventing potentially fatal arrhythmias have been developed and the accurate diagnosis of SCD is now of particular importance. The guidelines we produced represent the minimum standards of practice that should be adopted throughout the European Union and elsewhere. Further detailed information on the investigation of SCD and the diagnosis of specific entities will be available on the web site of the Association for European Cardiovascular Pathology (http://anpat.unipd.it/aecvp/).
Sources
1. Basso C, Calabrese F, Corrado D, Thiene G (2001) Postmortem diagnosis in sudden cardiac death victims: macroscopic, microscopic and molecular findings. Cardiovasc Res 50 : 290–330
2. Basso C, Thiene G (2005) Adipositas cordis, fatty infiltration of the right ventricle, and arrhythmogenic right ventricular cardiomyopathy. Just a matter of fat? Cardiovasc Pathol 14 : 37–41
3. Becker LB, Smith DW, Rhodes KV (1993) Incidence of cardiac arrest: a neglected factor in evaluating survival rates. Ann Emerg Med 22 : 86–91
4. Behr E, Wood DA, Wright M, Syrris P, Sheppard MN, Casey A, Davies MJ,McKennaW (2003) Sudden arrhythmic death syndrome steering group. Cardiological assessment of first-degree relatives in sudden arrhythmic death syndrome. Lancet 362 : 1457–1459
5. Brinkmann B (1999) Harmonization of medico-legal autopsy rules. Committee of Ministers. Council of Europe. Int J Legal Med 113 : 1–14
6. Calabrese F, Thiene G (2003) Myocarditis and inflammatory cardiomyopathy: microbiological and molecular biological aspects. Cardiovasc Res 60 : 11–25
7. Carturan E, Tester DJ, Brost BB, Basso C, Thiene G, Ackerman MJ (2007) Postmortem genetic testing for conventional autopsy negative sudden unexplained death: an evaluation of different DNA extraction protocols and the feasibility of mutational analysis from archival paraffin embedded heart tissue. Am J Clin Pathol (in press)
8. Chugh SS, Senashova O, Watts A, Tran PT, Zhou Z, Gong Q, Titus JL, Hayflick SJ (2004) Postmortem molecular screening in unexplained sudden death. J Am Coll Cardiol 43 : 1625–1629
9. Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G (2006) Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 296 : 1593–1601
10. Corrado D, Basso C, Thiene G (2001). Sudden cardiac death in young people with apparently normal heart. Cardiovasc Res 50 : 399–408
11. Davies MJ (1999) The investigation of sudden cardiac death. Histopathology 34 : 93–98
12. Fabre A, Sheppard MN (2006) Sudden adult death syndrome and other non-ischaemic causes of sudden cardiac death. Heart 92 : 316–320
13. Gillum RF (1989) Sudden coronary death in the United States: 1980–1985. Circulation 79 : 756–765
14. Goldstein S (1982) The necessity of a uniform definition of sudden coronary death: witnessed death within 1 hour of the onset of acute symptoms. Am Heart J 103 : 156–159
15. Hughes SE (2004) The pathology of hypertrophic cardiomyopathy. Histopathology 44 : 412–427
16. Kitzman DW, Scholz DG, Hagen PT, Ilstrup DM, Edwards WD (1988) Age-related changes in normal human hearts during the first 10 decades of life. Part II (maturity): a quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc 63 : 137–146
17. Medical Devices Agency Safety Notice 2002(35) (2002) Removal of implantable cardioverter defibrillators (ICDs). http://www.mhra. gov.uk/home/idcplg?IdcService=SS_GET_PAGE&useSecondary= true&ssDocName=CON008731&ssTargetNodeId=420 (pp 1–3)
18. Myerburg RJ, Castellanos A (2001) Cardiac arrest and sudden cardiac death. In: Braunwald E (ed) Heart disease: a textbook of cardiovascular medicine. Saunders, Philadelphia, PA, pp 890–931
19. Priori SG, Aliot E, Blomstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P, Camm AJ, Cappato R, Cobbe SM, Di Mario C, Maron BJ, McKenna WJ, Pedersen AK, Ravens U, Schwartz PJ, Trusz-Gluza M, Vardas P, Wellens HJ, Zipes DP (2001) Task force on sudden cardiac death of the European Society of Cardiology. Eur Heart J 22 : 1374–1450
20. Royal College of Pathologists (2005) Guidelines on autopsy practice 2005, scenario 1: sudden death with likely cardiac pathology. http://www.rcpath.org/index.asp?PageID=687 (pp 1–7)
22. Schulz DM, Giordano DA (1962) Hearts of infants and children: weights and measurements. Arch Pathol 73 : 464–471
21. Scholz DG, Kitzman DW, Hagen PT, Ilstrup DM, Edwards WD (1988) Age-related changes in normal human hearts during the first 10 decades of life. Part I (growth): a quantitative anatomic study of 200 specimens from subjects from birth to 19 years old. Mayo Clin Proc 63 : 126–136
23. Sheppard M, Davies MJ (1998) Investigation of sudden cardiac death. In: Sheppard M, Davies MJ (eds) Practical cardiovascular pathology. Arnold, London, pp 191–204
24. SOFT and AAFS (2002) Forensic toxicology laboratory guidelines. www.soft-tox.org/docs/Guidelines.2002.final.pdf pp 1–23
25. Tansey DK, Aly Z, Sheppard MN (2005) Fat in the right ventricle of the normal heart. Histopathology 46 : 98–104
26. Tester DJ, Ackerman MJ (2006) The role of molecular autopsy in unexplained sudden cardiac death. Curr Opin Cardiol 21 : 166–172
27. Thiene G, Basso C, Corrado D (2001). Cardiovascular causes of sudden death. In: Silver MD, Gotlieb AI, Schoen FJ (eds) Cardiovascular pathology. Churchill Livingstone, Philadelphia, pp 326–374
28. Virmani R, Burke AP, Farb A (2001) Sudden cardiac death. Cardiovasc Pathol 10 : 211–218
29. Zheng ZJ, Croft JB, Giles WH, Mensah GA (2001) Sudden cardiac death in the United States, 1989 to 1998. Circulation 104 : 2158–2163
Labels
Anatomical pathology Forensic medical examiner Toxicology
Article was published inCzecho-Slovak Pathology

2010 Issue 2-
All articles in this issue
- Fibroblasts – Known or Unknown Cells
- Blood Vessels and Lymphatics in Calcific Aortic Stenosis –In Support of its Inflammatory Pathogenesis
- Histologic Findings after Sodium Phosphate Bowel Preparation for ColonoscopyDiagnostic Pitfalls of Colonoscopic Biopsies
- Guidelines for autopsy investigation of sudden cardiac death
- Czecho-Slovak Pathology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Fibroblasts – Known or Unknown Cells
- Histologic Findings after Sodium Phosphate Bowel Preparation for ColonoscopyDiagnostic Pitfalls of Colonoscopic Biopsies
- Blood Vessels and Lymphatics in Calcific Aortic Stenosis –In Support of its Inflammatory Pathogenesis
- Guidelines for autopsy investigation of sudden cardiac death
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

