-
Medical journals
- Career
Aflibercept for Vascularised Serous Pigment Epithelial Detachment: One-Year Anatomical and Functional Results
Authors: J. Románek 1; H. Palyzová 2; J. Grygar 2; J. Ernest 2
Authors‘ workplace: TANA oční klinika, s. r. o. 1; Oční klinika 1. Lékařské fakulty Univerzity Karlovy a Ústřední vojenské nemocnice v Praze 2
Published in: Čes. a slov. Oftal., 76, 2020, No. 2, p. 88-93
Category: Original Article
doi: https://doi.org/10.31348/2020/16Overview
Purpose: To assess the effect of intravitreal aflibercept on pigment epithelial detachment (PED) secondary to occult choroidal neovascularization (CNV) in treatment-naive patients.
Patients and methods: Retrospective analysis of thirty-six patients (thirty-eight eyes) with mean age 77 (SD ± 7), who were treated with aflibercept 2.0 mg (Eylea, Bayer) at the Department of Ophthalmology of 1st Faculty of Medicine of the Charles University and the Military University Hospital Prague. All patients were treated in fixed regimen, which means 3 loading doases 1 month apart, followed by further
2-monthly doses over total 12-month period. Best corrected visual acuity (BCVA) was evaluated on Early Treatment Diabetic Retinopathy Study (ETDRS) charts. Diameters as PED height, width and central retinal thickness (CRT) were assesed using spectral-domain optical coherence tomography. All previously mentioned were analyzed et the baseline and than at every visit. Therapy complications were also evaluated.
Results: Borderline significant improvement in the mean of BCVA score of 3.2 letters (SD ± 11.6, p = 0.05) at the end of follow-up period was observed. Mean PED height at 12 months significantly decreased by 140 µm (SD ± 238, p < 0.01). Reductions in PED height were correlated with reductions in central macular thickness (R = 0.94, p < 0.001) simultaneously with PED width (R = 0.45, p < 0.01). There was no significant correlation between PED height decrease and visual acuity. PED rupture was observed in 3 eyes (8 %).
Conclusion: Aflibercept intravitreal therapy in fixed regimen in patients with PED secondary to occult CNV shows great anatomical effect. However, correlation between PED diameters and visual acuity was not observed.
Keywords:
anti-VEGF – aflibercept – pigment epithelial detachment – occult CNV
Sworn declaration
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company. The authors also declare that the study has not been submitted to any other journal or printed elsewhere.
INTRODUCTION
Age-related macular degeneration (ARMD) is a progressive chronic disorder, which is the most common cause of practical blindness in advanced countries in persons aged over 50 years [1]. This is due primarily to its exudative form, with the onset of choroidal neovascularisation [2]. In the diagnosis of exudative form of ARMD we differentiate between a number of subtypes, of which approximately 10 % represent vascular serous detachment of the retinal pigment epithelium [3]. Vascular serous detachment of the RPE upon a background of occult CNV or central retinal angiomatous proliferation (RAP) is a complicated condition with a different development in comparison with other neovascular lesions. In addition to the actual process of progression of CNV, the condition has a worse prognosis also due to affiliated atrophy of the RPE, the risk of its rupture, and in the final result the formation of a disciform scar [4]. Configuration of an ideal therapeutic plan is considered to be complex, not only due to the aforementioned complications, but also due to the generally low anatomical and functional effectiveness of treatment, which has been demonstrated by several studies [5,6,7,8]. The only approved treatment according to SPC at present is intravitreal anti-VEGF therapy. According to ongoing studies, a combination of photodynamic therapy and anti-VEGF appears to be effective [9].
The aim of this study is to present a retrospective evaluation of one-year treatment of a group of patients with newly diagnosed serous detachment of the RPE secondary to occult form of CNV, and to compare our results with those of clinical trials. In treatment, the aflibercept preparation was used in a fixed dose regimen.
COHORT AND METHOD
A total of 38 eyes of 36 patients were included in the retrospective study conducted at the Department of Ophthalmology, 1st Faculty of Medicine, Charles University and Central Military Hospital in Prague. The treatment took place within the period from January 2017 to June 2019. Table 1 summarises the basic demographic and clinical data on the cohort of patients.
1. Baseline demographic and clinical characteristics (number of patients n = 36) 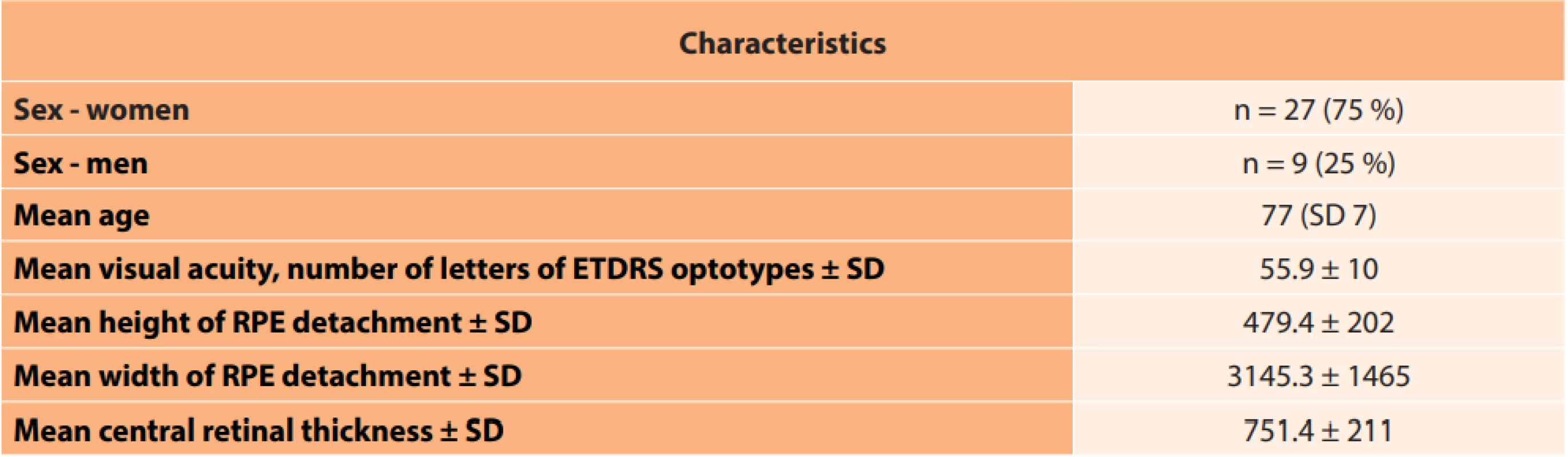
ETDRS = Early Treatment Diabetic Retinopathy Study, n = number of patients, RPE = retinal pigment epithelium, SD = standard deviation A condition for inclusion in the study was a treatment-naive patient with newly diagnosed vascular serous RPE detachment, which was treated using the aflibercept preparation in a fixed dose regimen for a period of at least 12 months. The treatment was based on summary data on the preparation, thus commencement with three intravitreal injections of 2 mg of aflibercept at intervals of one month, followed by four injections at intervals of two months. The entrance criteria, in addition to the above-stated diagnosis, were best corrected visual acuity within the range of 35–70 letters of ETDRS optotype, size of lesion up to 8 DA (disc area – surface of optic nerve papilla), scope of haemorrhage maximally up to 25 % of the lesion and demonstration of active CNV by fluorescence angiography and spectral domain optical coherence tomography (SD-OCT). The present vascular serous RPE detachment had to have subfoveal localisation (within the range of maximum 500 µm from the fovea) and initial height greater than 250 µm. At each follow-up visit a complete examination was conducted, covering determination of BCVA on ETDRS optotypes and SD-OCT (Heidelberg Spectralis; Heidelberg Industries, Heidelberg, Germany). Fluorescence angiography was performed at the initial visit in order to confirm the presence of choroidal neovascularisation associated with serious RPE detachment (Fig. 1). Central retinal thickness was defined as the distance between the membrana limitans interna (MLI) and the Bruch’s membrane. The height of RPE detachment was measured using a software caliper as the maximum vertical dimension from the RPE to the Bruch’s membrane (Fig. 2). The width of RPE detachment was measured by an identical method as the maximum horizontal dimension.
1. Fluorescence angiography at baseline examination
A. Early phase of fluorescence angiography identifying hyperfluorescent lesion of choroidal neovascularisation with infiltration on the upper edge of the lesion, peripheral filling of RPE detachment, on lower edge evident hypofluorescence corresponding to haemorrhage
B. Middle phase with progressive filling of deposit of RPE detachment with fluorescein
C. Late phase identifying homogeneous hyperfluorescence with sharp edges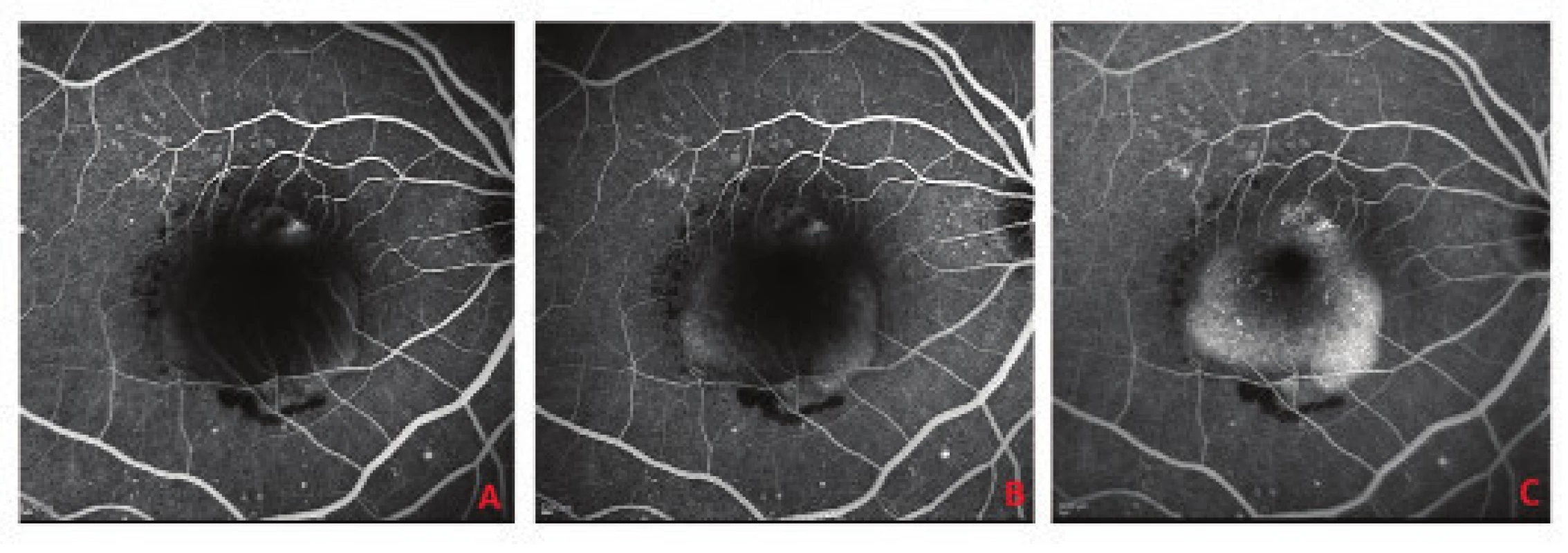
2. SD-OCT image of vascular serous detachment of retinal pigment epithelium upon a background of occult choroidal neovascularisation
A. Method of measurement of height of RPE detachment
B. Method of measurement of width of RPE detachment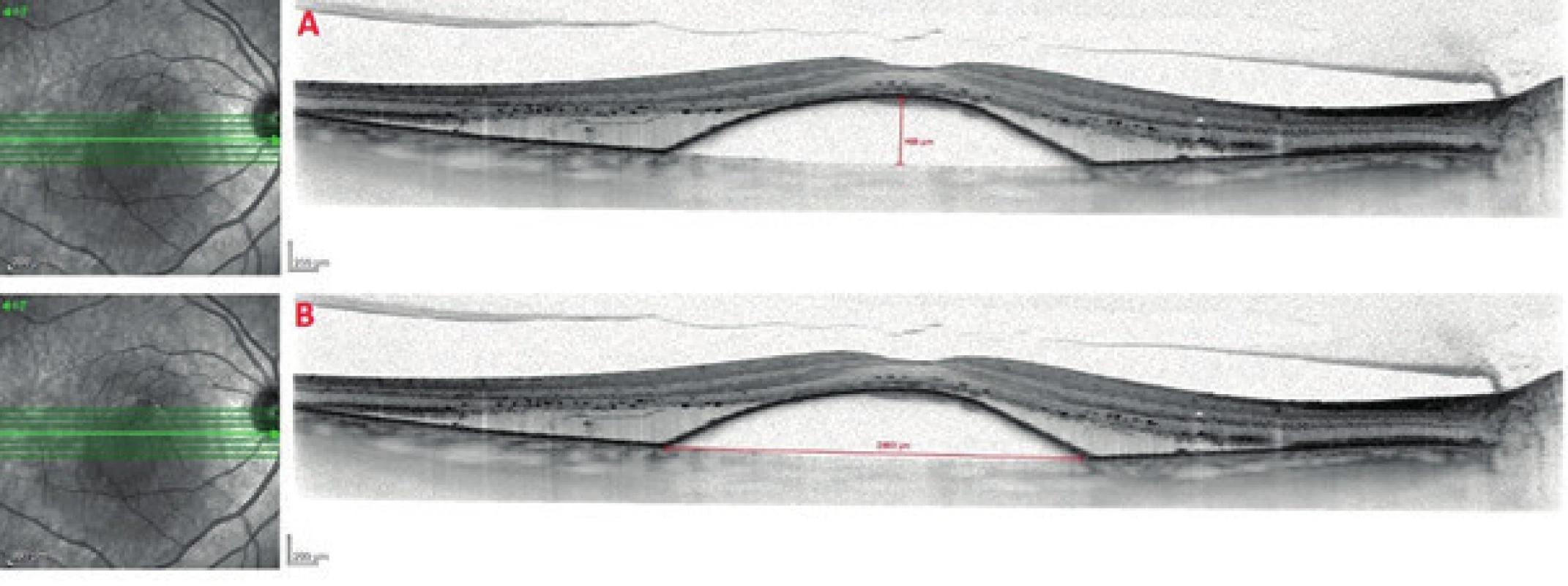
Statistical analysis
Quantitative values were defined by the mean and standard deviation. They were subsequently analysed using a Kolmogorov-Smirnov normality test. Their changes were evaluated with the aid of a Student t-test. The correlation between changes of the height and width of RPE detachment and CRT was determined with the aid of a Pearson correlation coefficient. Statistical significance was set at p < 0.05.
RESULTS
In the selected cohort of patients (38 eyes), an improvement of BCVA against the baseline values was recorded after the first three intravitreal applications of aflibercept, on average by 4.8 letters (SD ± 9.0) of ETDRS optotype. Average BCVA was 61 letters (SD ± 12). This change was evaluated as significant on the level of significance of p < 0.01. An improvement by more than 15 letters was recorded in 4 eyes (11 %), by 10 to 14 letters in 10 eyes (26 %), and within the range of 3 to 9 letters in 9 eyes (24 %).
Deterioration of BCVA by more than 15 letters was not recorded in any of the studied eyes, deterioration by 10 to 14 letters was recorded in 2 eyes (5 %) and by 3 to 9 letters in 6 eyes (16 %). Seven eyes (18 %) were evaluated as stable (range from loss of 2 letters to gain of 2 letters).
Upon evaluation of BCVA after the final seven applications, the mean value was 59 letters (SD ± 13), mean gain in comparison with baseline visual acuity was 3.2 letters (SD ± 11.6). However, according to statistical significance this change is on the borderline of significance (p = 0.05). Improvement by > 15 letters was recorded in 5 eyes (13 %), improvement by 10–14 letters also in 5 eyes (13 %), and improvement by 3–9 letters in 12 eyes (32 %). By contrast, 3 eyes (8 %) deteriorated by > 15 letters, 2 eyes (5 %) by 10–14 letters and 6 eyes (16 %) by 3–9 letters. Stability (range from loss of 2 letters to gain of 2 letters) was recorded in 5 eyes (13 %). The development of the absolute values of BCVA during the course of application is illustrated in Graph 1.
1. Change of best corrected visual acuity during the course of one year of observation 
Average height of RPE detachment at the baseline examination was 479 µm (SD ± 202). During the course of application it was significantly reduced. After the third application there was a reduction of the height of RPE detachment by 132 µm (SD ± 205) upon comparison with the baseline values (p < 0.01). Complete absorption of the detachment in this phase of treatment was not recorded in any of the observed eyes. If we are to evaluate anatomical regression of the finding as a reduction of height by > 50 µm, then this improvement was recorded in 23 eyes (61 %). By contrast, increase of the height of RPE detachment by > 50 µm was recorded in 4 eyes (11 %).
In addition to this, 11 eyes (28 %) remained stable. The mean reduction of the height of RPE detachment after the 7th application, in comparison with the baseline measurements, was 140 µm (SD ± 238, p < 0.01). An overall improvement of the finding (reduction of height by > 50 µm) was achieved in 23 eyes (61 %). An overall deterioration of the finding (increase of height by > 50 µm) occurred in 5 eyes (13 %), with 10 eyes (26 %) remaining stable. In one case complete absorption of RPE detachment took place.
Changes in the values of the height of RPE detachment correlated with changes of CRT (R = 0.94, p < 0.001). This correlation is given by the subfoveolar deposit of the RPE detachment. The reduction in detachment width also correlated with the decrease in detachment height (R = 0.45, P < 0.01). The same applied upon a comparison of the development of the values of the width of RPE detachment and CRT (R = 0.46, p < 0.01). The development of the absolute values of height of RPE detachment, width of RPE detachment and CRT is illustrated in Graph 2.
2. Change of height and width of RPE detachment and central retinal thickness during the course of one year of observation 
The OCT finding at the final follow-up visit did not manifest any signs of exudative activity (presence of intraretinal or subretinal fluid) in 15 eyes (39 %). In two eyes (5 %) the presence of a crack in the RPE was recorded at the baseline visit. In the case of another 3 eyes (8 %) a rupture of the RPE occurred, in all cases immediately after the initial application. No other complications were observed in connection with the intravitreal application of pharmaceuticals.
DISCUSSION
Occult CNV associated with serous RPE detachment is considered a specific entity of exudative ARMD, which is difficult to treat [10,11,12]. According to Pauleikhoff et al. [12], it results in a significant loss of BCVA by more than 3 rows in 40–50 % of eyes during the course of one year.
Knahani et al. [13] analysed a number of retrospective studies examining the influence of anti-VEGF therapy, at various dosing intervals, on the development of RPE detachment secondary to CNV. Five of the analysed retrospective studies recorded an anatomical and functional improvement, the same number of studies described visual stability and anatomical improvement, and one study described a decrease in the values of visual acuity despite an anatomical improvement of the finding. The conclusion of this broad analysis is that it is difficult to predict anatomical and functional change, and that there is an absence of their correlation.
Chen et al. [14] evaluated the influence of treatment with aflibercept over the course of one year in 28 eyes with RPE detachment secondary to occult CNV. The study demonstrated an improvement of BCVA by 4.5 letters (SD ± 23) of ETDRS optotype. Our results demonstrate an identical trend, with an improvement by 3.2 letters (SD ± 11.6). We attribute the smaller gain in our study to the different therapeutic schema, since in the study by Chen et al. the treatment took place more intensively, commencing with six monthly applications before switching to dosing every two months. It is precisely the length of the “loading phase” that probably contributed to the better development of BCVA. In our study, average BCVA of 61 letters (SD ± 12) after 3 applications decreased to 59 letters (SD ± 14) after the 7th application. It is probable that this was contributed to by the change of monthly interval from the loading phase to the interval of dosing every two months. This conclusion is in accordance with other clinical trials engaging with the treatment of occult CNV associated with serous RPE detachment within a regimen of a two-monthly application interval [15,16].
Broadhead et al. [15] analysed anatomical changes within the framework of one year of treatment with aflibercept in 43 eyes with RPE detachment secondary to CNV. This concerned a cohort of patients with a finding of resistant RPE detachment following prior anti-VEGF therapy. At the end of the observation period they recorded an anatomical improvement with a reduction in height by > 50 µm in 42 % of eyes (in our cohort 61 % of eyes), a stable finding in 56 % of eyes (in our cohort 26 %) and anatomical deterioration in 2 % of eyes (in our cohort 13 %). The different proportional distribution in the above study, with a predominance of stable findings, can be attributed to the previous anti-VEGF therapy. However, in this study also, as in ours, the changes in the decrease in height of RPE detachment are evaluated as significant.
The reduction in the height of RPE detachment from an average 479 µm (SD ± 205) to 340 µm (SD ± 179) after one year of observation in our study is smaller in comparison with the extensive study published by Cho et al. [17]. This study analyses a cohort of 202 eyes with RPE detachment secondary to CNV within the framework of one year of treatment with ranibizumab or aflibercept, with a three-month loading phase and subsequent pro re nata (PRN) regimen. The authors state a reduction in the height of RPE detachment from an initial average 453 µm (SD ± 261) to 230 µm (SD ± 142).
We attribute the less pronounced reduction in the height of detachment to the smaller number of patients in our cohort (38 eyes in comparison with 202 in the study by Cho et al.). An associated result of the aforementioned study is the significantly greater effectiveness of aflibercept on reducing the height of RPE detachment in comparison with ranibizumab (Lucentis, Novartis) [17].
The finding of CNV activity confirmed on OCT in 61 % of eyes in our study after the 7th application was in accordance with the results published by Zinkernagel et al. [16], who state a finding of presence of intraretinal or subretinal fluid in 55 % of eyes in the final evaluation.
The absence of a significant correlation between reduction of height of detachment and gain of letters in our study is consistent with the results of other studies focusing on the influence of anti-VEGF therapy on the dimensions of RPE detachment [8,15,22]. In these patients, there is strong suspicion that improvement of BCVA is due to the influence of other factors than only change of the size of RPE detachment, such as the presence or absence of intraretinal or subretinal fluid [8,15,22]. On the contrary, the studies published by Zinkernagel et al. [16] and Chen et al. [14] assert that complete absorption of detachment leads to a higher incidence of RPE atrophy, and therefore that complete anatomical correction is not necessary or even desirable for the success of therapy with regard to visual acuity.
Rupture of the RPE, according to localisation, may be a condition which complicates therapy. It occurs upon a background of contraction of the neovascular membrane after application of an anti-VEGF preparation. An increased risk exists primarily in the case of more extensive vascular detachments of the RPE due to greater intraluminal pressure [18]. Height of detachment greater than 400 µm is considered a risk factor [19]. The described incidence of RPE ruptures is 17–26 % [18,20], with predominant occurrence in the initial phases of therapy [21]. In our study we recorded an incidence of rupture in 8 % of the observed cases (3 eyes). The discrepancy in the incidence is again due to the smaller cohort of patients, but in all the recorded cases the rupture occurred immediately after the first application of the anti-VEGF preparation, which is in accordance with the results presented by the aforementioned study [21].
The limitations of our study are its retrospective design, the smaller cohort of patients and the absence of a control group of patients treated with another anti-VEGF preparation.
CONCLUSION
In conclusion it is possible to state that our study confirmed the influence of aflibercept on anatomical improvement of a finding of vascular serous RPE detachment, with a significant reduction. The absence of a correlation between the reduction of detachment and the gain in letters indicates that the treatment of this subtype of CNV is insufficient in current therapy, and requires further studies examining new procedures or methods.
Sources
1. Klein, R., Klein, BE., Knudtson, MD., Meuer, SM., Swift, M., Gangnon, RE.: Fifteen-year cumulative incidence of age-related macular degeneration. Ophthalmology. 2007;114(2):253–262.
2. Bressler, NM.: Age-related macular degeneration is the leading cause of blindness. JAMA. 2004; 291(15):1900–1901.
3. Lommatzsch, APOD., Heimes, B., Gutfleisch, M. et al.: Serous pigment epithelial detachment in age-related macular degeneration: comparison of different treatments. Eye. 2009;23 : 2163–2168.
4. Poliner, LS., Olk, RJ., Burgess, D., Gordon, ME.: Natural history of retinal pigment epithelial detachments in age-related macular degeneration. Ophthalmology. 1986;93(5):543–551.
5. Suzuki, M., Nagai, N., Izumi-Nagai, K. et al.: Predictive factors for non-response to intravitreal ranibizumab treatment in agerelated macular degeneration. Br J Ophthalmol. 2014;98(9):1186–1191.
6. Ashraf, M., Souka, A., Adelman, RA.: Age‐related macular degeneration: using morphological predictors to modify current treatment protocols. Acta Ophthalmol. 2018;96 : 120-133.
7. Patel, KH., Chow, CC., Rathod, R. et al.: Rapid response of retinal pigment epithelial detachments to intravitreal aflibercept in neovascular age-related macular degeneration refractory to bevacizumab and ranibizumab. Eye (Lond). 2013;27 : 663–667.
8. Parodi, MB., Iacono, P., Papayannis, A. et al.: Intravitreal ranibizumab for pigment epithelial detachment with subfoveal occult neovascularization: a prospective 24-month case series. Am J Ophthalmol. 2013;155 : 103–108.
9. Gonzalez, A., Khurshid, G.: Treatment of retinal pigment epithelial detachment secondary to exudative age-related macular degeneration. Am J Ophthalmol Case Rep. 2017;9 : 18–22.
10. Gass, JD.: Serous retinal pigment epithelial detachment with a notch. A sign of occult choroidal neovascularization. Retina 1984;4(4):205–220.
11. Bird, AC., Marshall, J.: Retinal pigment epithelial detachments in the elderly. Trans Ophthalmol Soc. 1986;105 : 674–682.
12. Pauleikhoff, D., Loffert, D., Spital, G. et al.: Pigment epithelial detachment in the elderly. Clinical differentiation, natural course and pathogenetic implications. Graefes Arch Clin Exp Ophthalmol. 2002;240(7):533–538.
13. Khanani, AM., Eichenbaum, D., Schlottmann, PG., Tuomi, L., Sarraf, D.: Optimal management of pigment epithelial detachments in eyes with neovascular age-related macular degeneration. Retina. 2018;38(11):2103–2117.
14. Chen, X., Al-Sheikh, M., Chan, CK. et al.: Type 1 versus type 3 neovascularization in pigment epithelial detachments associated with age-related macular degeneration after anti-vascular endothelial growth factor therapy: a prospective study. Retina. 2016;36(S1):S50–S64.
15. Broadhead, GK., Hong, T., Zhu, M. et al.: Response of pigment epithelial detachments to intravitreal aflibercept among patients with treatment-resistant neovascular age-related macular degeneration. Retina. 2015;35 : 975–981.
16. Zinkernagel, MS., Wolf, S., Ebneter, A.: Fluctuations in pigment epithelial detachment and retinal fluid using a bimonthly treatment regimen with aflibercept for neovascular age-related macular degeneration. Ophthalmologica. 2016;235 : 42–48.
17. Cho, HJ., Kim, KM., Kim, HS. et al.: Response of pigment epithelial detachment to anti-vascular endothelial growth factor treatment in age-related macular degeneration. Am J Ophthalmol. 2016;166 : 112–119.
18. Introini, U., Torres Gimeno, A., Scotti, F. et al.: Vascularized retinal pigment epithelial detachment in age-related macular degeneration: treatment and RPE tear incidence. Graefes Arch Clin Exp Ophthalmol. 2012;250 : 1283–1292.
19. Chan, CK., Abraham, P., Meyer, CH. et al.: Optical coherence tomography-measured pigment epithelial detachment height as a predictor for retinal pigment epithelial tears associated with intravitreal bevacizumab injections. Retina. 2010;30 : 203–211.
20. Chang, LK., Sarraf, D.: Tears of the RPE: an old problem in a new era. Retina. 2007;27 : 523–527.
21. Cunningham, ET. Jr., Feiner, L., Chung, C. et al.: Incidence of retinal pigment epithelial tears after intravitreal ranibizumab injection for neovascular age-related macular degeneration. Ophthalmology. 2011;118 : 2447–2452.
22. Panos, GD., Gatzioufas, Z., Petropoulos, IK. et al.: Effect of ranibizumab on serous and vascular pigment epithelial detachments associated with exudative age-related macular degeneration. Drug Des Devel Ther. 2013;7 : 565–569.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2020 Issue 2-
All articles in this issue
- Zemřela prof. MUDr. Jarmila Boguszaková DrSc.
- Vzpomínka na doc. MUDr. Cigánka, CSc.
- EPIGENETIC CHANGES IN MALIGNANT UVEAL MELANOMA AND POSSIBILITIES OF THEIR THERAPEUTIC TARGETING
- Primary Intrabulbar Neurofibroma
- Does adjuvant intracameral triamcinolone acetonide increase the effectiveness of phacotrabeculectomy? A Case-Control Study
- Non-arteritic anterior ischaemic optic neuropathy: treatment and risk factors
- Aflibercept for Vascularised Serous Pigment Epithelial Detachment: One-Year Anatomical and Functional Results
- Betaxolol, Brimonidin and Carteolol in the Therapy of Normal-Tension Glaucoma
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Non-arteritic anterior ischaemic optic neuropathy: treatment and risk factors
- Vzpomínka na doc. MUDr. Cigánka, CSc.
- Betaxolol, Brimonidin and Carteolol in the Therapy of Normal-Tension Glaucoma
- Aflibercept for Vascularised Serous Pigment Epithelial Detachment: One-Year Anatomical and Functional Results
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

