-
Medical journals
- Career
Sensitivity and specificity of spectral OCT in patients with early glaucoma.
Authors: M. Bočková 1,2; P. Veselý 1,2; S. Synek 1,2; L. Hanák 1,2; P. Beneš 1,2
Authors‘ workplace: Oddělení nemocí očních a optometrie, Fakultní nemocnice u svaté Anny, Pekařská 53, 65691 Brno. Přednosta: MUDr. Lubomír Hanák, MBA. 1; Katedra optometrie a ortoptiky, Lékařská fakulta, Masarykova univerzita, Kamenice 5, 62500 Brno. Přednosta: doc. Mgr. Pavel Beneš, Ph. D. 2
Published in: Čes. a slov. Oftal., 75, 2019, No. 5, p. 260-264
Category: Original Article
doi: https://doi.org/10.31348/2019/5/3Overview
This work deals with sensitivity and specificity in spectral OCT in detection of early glaucoma. Our goal was to evaluate data from RNFL analysis and compare them with resulted diagnosis of glaucoma neuropathy based on visual field changes. This retrospective study contains 31 subjects who undergone OCT examination in our department between years 2008 and 2017. Test statistic showed RNFL OCT sensitivity 63.64 % and specificity 90 %. Test ROC (receiver operating characteristic curve) showed AUC (area under curve) 0.734, which was statistically significant (p = 0.0097). We found that spectral OCT SLO with RNFL analysis is useful and effective instrument in analysis of glaucoma.
Keywords:
glaucoma – RNFL analysis – spectral OCT – sensitivity – specificity
INTRODUCTION
Glaucoma is a multifactorial, progressive and irreversible neuropathy of the optic nerve, characterised by a loss of retinal ganglion cells and atrophy of the optic nerve. Glaucoma neuropathy is accompanied by specific damage to the visual field. The most significant risk factor is considered to be elevation of intraocular pressure. The fundamental methods of examination are measurement of intraocular pressure, biomicroscopic evaluation of the optic nerve disc, gonioscopy and perimetric examination. However, as a rule these examinations fail to detect very early glaucomatous changes. It is considered that before the actual initial detection of defects in the visual field with the aid of automated perimetry, more than 35% of retinal ganglion cells may already be lost (7). The finding that structural changes precede detectable functional deficits has led to increased interest in imaging technology. Imaging methods now play an irreplaceable role in the current diagnosis of glaucoma. Most often we proceed to perform these examinations precisely within the framework of diagnosis of early stages of glaucoma, and subsequently upon monitoring glaucoma over time for the purpose of detecting its progression. The imaging methods used for diagnosis and monitoring of glaucoma include HRT examination (Heidelberg retinal tomography), OCT examination (optical coherence tomography) and GDx (nerve fibre analyser). Here we shall focus especially on OCT examination. OCT provides a quantity of analyses for diagnosis of glaucoma pathology – analysis of the retinal nerve fibre layer (RNFL), analysis of the papilla of the optic nerve and more recently also analysis of macular changes in glaucoma, specifically analysis of the ganglion cell layer (GCL) and posterior pole asymmetry analysis (PPAA) of maps of macular thickness of the retina. A modern diagnostic analysis is also measurement of the minimum thickness of the neuroretinal rim from the edge of the Bruch’s membrane (BMO-MRW – Bruch’s Membrane Opening Minimum Rim Width), which is currently provided only by certain types of spectral OCT. OCT can also be used for evaluating the anterior segment, especially for measurement of diffuse optical pachymetry,measurement of the anterior chamber angle and analysis of pathologies of the angle and iris.
One of the most important functions of OCT is the possibility of subsequent scanning, which enables monitoring of the patient and any applicable progression of the pathology over time. Monitoring can be performed in two ways. The first is software post-processing, comparing the recorded data with previous examination with the aid of retinal (mostly vascular) registration. The second, more precise and modern option is “eye tracking”, which produces only a minimum deviation between two consecutive measurements on the level of approx. 1 µm (9).
At our centre we have at our disposal the instrument Spectral OCT SLO from the manufacturer OPKO Instrumentation/OTI OPKO Health, Inc. This is an instrument with an axial resolution of 5 µm and transverse resolution of 15 µm. The scanning speed is 27 thousand A-scans per second. We use the instrument primarily for structural examination of the macular region of the retina, for example in patients with age-related macular degeneration. Thanks to the possibility of analysis of the RNFL (retinal nerve fibre layer) and measurement of the topography of the optic nerve papilla, at our centre we regularly examine also patients with suspected glaucoma neuropathy, most frequently within the framework of early diagnosis of primary open angle glaucoma (POAG).
According to certain studies (5), in the case of spectral domain OCT it is possible to attain sensitivity of as high as 96% and specificity of 76%. The aim of our retrospective study was to evaluate data obtained thanks to RNFL analysis in 4 observed summary quadrants and compare it with the resulting diagnosis of glaucoma neuropathy determined subsequently primarily on the basis of changes in the visual field. A specific feature of our study is the categorisation (0-2) of changes of the RNFL in individual quadrants, based on the method of the instrument software.
1. Special Optical Coherence Tomography instrument 
METHOD
The study numbered a total of 31 probands, who underwent an RNFL examination at our centre with the aid of an OCT instrument in the period from 2008 to 2017. This cohort comprised 16 women and 15 men. The average age of the patients at the time of examination was 52 years (maximum 77, minimum 28) with standard deviation of 15 years. In all patients we concentrated on evaluating the classification of RNFL thickness in their right eyes. Included in the study were patients with a suspected finding at a biomicroscopic examination (C/D ratio greater than 0.5), without a positive finding on the perimeter and without anti-glaucomatous therapy. Evaluated were both RNFL thickness itself and the adjusted classification comparing RNFL thickness with the normative database in the individual 4 quadrants. We chose the designation as follows: we designated values corresponding to 95% of the normative database with number 0, corresponding to less than 5% of the normative database with number 1 and corresponding to less than 1% of the normative database with number 2. Number 0 therefore meant a negative result – there was no thinning of the RNFL beneath the normative value. By contrast, number 2 meant maximal thinning of the RNFL beneath the normative value (pathological finding). Number 1 then expressed partial thinning of the RNFL beneath the normative value (suspected finding). For a statistical evaluation of sensitivity and specificity we worked with the average numerical value of RNFL thickness in micrometres and the numerical value of the classification from all 4 quadrants, as well as the sum of values from all 4 quadrants.
The probands continued to be monitored at our centre for a minimum period of one year (minimum 1 year, maximum 9 years, average 3.72 years). In some patients, there was a demonstrated progression of the glaucoma pathology on the basis of changes in the visual field in the observed eye, and therapy was applied. We designated these probands with number 1. Probands designated with number 0 were those in whom no glaucoma pathology was manifested within the observation period (and up to today). The visual field of these patients is intact.
The results of measurement were converted into an MS Excel table and subsequently statistically evaluated with the aid of the statistical program Statistika version 12 from the company STATSOFT and MedCalc. The selected statistical level of significance was p = 0.05.
RESULTS
Progression of glaucoma took place in a total of 11 right eyes of the patients (designation 1). This means that 20 right eyes of the patients were without progression (designation 0) in the observation period. At the time of the first examination, a total of 21 eyes were negative (0) according to OCT in all quadrants. From this it ensues that only 1 eye produced a false negative. The average simplified categorised value of RNFL thickness in the individual quadrants in patients with designation 1 and 0 is presented in graph 1. The average value of all quadrants in patients with designation 1 is 0.59 and in patients with 0 is 0.18. A Student parametric test demonstrated a statistically significant difference between these values (p = 0.0027).
1. Average categorised values of RNFL thickness in individual quadrants in patients with designation 1 (with pathology) and 0 (without pathology) 
2. Receiver Operating Characteristic curve for Spectral Optical Coherence Tomography instrument. Sensitivity 63.64%, specificity 90.00%, association criterion >1 
The test statistics on the cohort of 31 right eyes of probands for OCT examination demonstrated sensitivity of 63.64% and specificity of 90% (Table 1). With the aid of an ROC (receiver operating characteristic curve) test, an AUC (area under curve) value of 0.734 was determined, on a statistically significant level of p = 0.0097.
1. Result of Receiver Operating Characteristic of test for Spectral Optical Coherence Tomography instrument 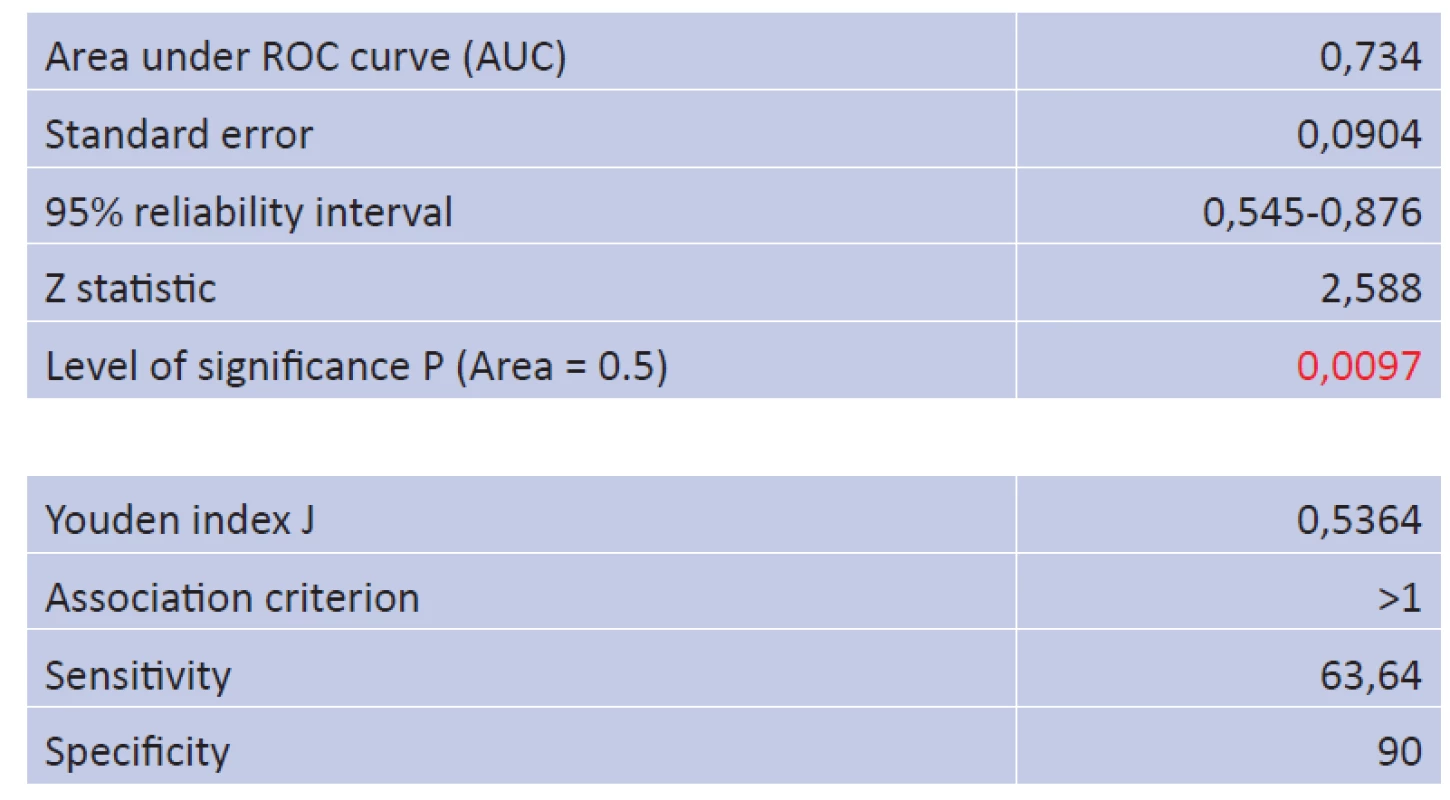
With reference to the result of the further statistical test (Youden index) of J = 0.5364, we can state that the instrument used is capable of reliably dividing healthy subjects and affected patients. The association criterion is categorisation with number 1. This means that a proband with this designation of reduction of RNFL thickness beneath 5% of the normative database or suspect finding in at least one quadrant is the same proband in whom glaucoma pathology was subsequently manifested.
Sensitivity and specificity related to RNFL thickness in all quadrants showed the same results as upon use of categorised values (63.64% and 90% respectively). For evaluation of sensitivity and specificity we used the sum of RNFL thickness in all quadrants in micrometres (the average value for probands with number 1 was 357.27 µm, and for probands with number 0 this was 401.30 µm).
Individual quadrants were also evaluated. The average thickness of the RNFL layer in the lower quadrant in healthy eyes was 114.1 µm as against 103.45 µm in eyes with demonstrated glaucoma pathology, in the upper quadrant this was 123.55 µm in healthy eyes as against 107.9 µm in the affected probands, in the nasal quadrants 83.85 µm in healthy eyes vs. 80.82 in affected patients and in the temporal quadrant 79.8 µm vs. 65.09 µm. The difference between average RNFL thickness in the probands with progression and without progression was therefore most pronounced in the upper quadrant (15.65 µm), followed by the temporal quadrant (14.71 µm) and the lower quadrant (10.65 µm), whereas the difference in the nasal quadrant was negligible (3.03 µm).
DISCUSSION
RNFL analysis is currently considered the standard tool for detection of early glaucoma. Numerous studies have demonstrated a correlation between thinning of the RNFL and affliction of the visual field (1). The aim of our study was to confirm this correlation and evaluate the sensitivity and specificity of spectral OCT examination in detecting early glaucoma.
The sensitivity of the time-domain instrument StratusOCT on patients with already demonstrated glaucomatous changes in the visual field has been investigated by Budenz et al. (2). The sensitivity and specificity of the instrument upon an abnormal value of RNFL thickness in one and more quadrants on the level of less than 5% was as follows: 89% for sensitivity and 95% for specificity. With the arrival of spectral OCT, distinguished by better resolution on the basis of a larger number of A-scans in comparison with time-domain OCT and at the same time better reproducibility for various levels of severity of glaucoma, an increase in precision of diagnosis of glaucoma neuropathy was also expected. Studies were conducted comparing sensitivity and specificity in the case of time-domain and spectral-domain OCT. One of these was the study by Chang et al. (5), which for time-domain OCT (StratusOCT) in one or more abnormal quadrants on a level of 5% determined sensitivity of 96% and specificity of 76%, whereas for spectral-domain OCT (Cirrus OCT) this was 98% and 80%. They also studied parameters which are distinguished by the highest sensitivity and specificity. The highest sensitivity was determined for the meridian of 12 on the clock face (0.98), average thickness of RNFL (0.96) and upper quadrant (0.9) (8). A further development of the analytical possibilities of OCT brought evaluation of the ganglion cell layer in the macular region and analysis of symmetry of the macular region to the diagnosis of glaucoma. However, according to the study by Kaushik et al. (6) from 2018, at present measurement of GCA (ganglion cell analysis) provided by SD-OCT has not surpassed measurement of RNFL in the diagnosis of pre-perimetric glaucoma. This was confirmed also by a meta-analysis in a total of thirty-seven studies which investigated a comparison between macular and RNFL parameters measured with the aid of RTVue OCT (Optovue Inc., Fremont, CA), (19 studies, 3094 subjects), Cirrus OCT (Carl Zeiss Meditec Inc., Dublin, CA), (14 studies, 2164 subjects) and 3D Topcon OCT (Topcon, Inc., Tokyo, Japan), (4 studies, 522 subjects). Studies in general stated sensitivity, at fixed specificities on a level of 0.90 or 0.95, in the most effective parameters between 0.65 and 0.75. In the case of all OCT instruments, macular parameters in comparison with RNFL parameters manifested a similar or slightly lower precision for detection of glaucoma (10). Sensitivity and specificity of RNFL analysis in our study was congruent with the studies evaluated by this meta-analysis (sensitivity 63.64% and specificity 90%). It is therefore possible to state that the instrument Spectral OCT SLO (OPKO Instrumentation/OTI OPKO Health, Inc.) is an effective tool for the detection of glaucoma pathology. In comparison with some of the above-mentioned studies, the sensitivity we demonstrated is slightly lower, which may be due in particular to an assessment of only the first performed OCT in the right eye, the relative size of the cohort (n = 31) and the subsequent difference in the length of the observation interval (1 to 9 years), during which the neuropathy could progress. Last but not least this may also be due to the simplified categorisation itself, in which the category of RNFL 1 – patients on the borderline of a physiological finding may have found themselves beneath 5% of the normative database or with a suspected finding. For this reason, in addition to the above-mentioned simple categorisation it is important to take into account the evaluation of the RNFL thickness itself, including evaluation of the individual 4 quadrants and sub-segments. The average value of RNFL thickness from the total of all quadrants in our study was 357.27 µm in group 1 (with progression) and 401.30 µm in group 0 (without progression). Early glaucoma is typified by a reduction in RNFL thickness in the temporal inferior and temporal superior sub-segment. In our study also the greatest difference in RNFL thickness between probands in group 0 and group 1 (i.e. without and with glaucoma pathology) was manifested in the upper and temporal quadrant, followed by the lower quadrant, with only a minimal difference in the nasal quadrant. An essential component of early diagnosis is also monitoring of changes of RNFL thickness over time and comparison thereof with the initial measurement.
Our study demonstrated that the instrument Spectral OCT CLO (OPKO Instrumentation/OTI OPKO Health, Inc.) is an effective tool for the detection of glaucoma pathology. Within the framework of RNFL analysis we succeeded in designating probands in whom the progression of glaucoma pathology had occurred on a statistically significant level.
Received: 27. 3. 2019
Accepted: 21. 10. 2019
Available on-line: 17. 2. 2020
MUDr. Magdaléna Bočková
Oddělení nemocí očních a optometrie Fakultní nemocnice u sv. Anny
Pekařská 53,
656 91 Brno
Sources
1. Ajtony, C., Balla, Z., Somoskeoy, S. et al.: Relationship between visual field sensitivity and retinal nerve fiber layer thickness as measured by optical coherence tomography. Invest Ophthalmol Vis Sci, 48; 2007 : 258–63.
2. Budenz, DL., Michael, A., Chang, RT. et al.: Sensitivity and specificity of the StratusOCT for perimetric glaucoma. Ophthalmology, 112; 2005 : 3-9.
3. Bussel, I., Wollstein, G., Schuman, JS.: OCT for glaucoma diagnosis, screening and detection of glaucoma progression. British Journal of Ophthalmlogy, 98; 2014 : 2.
4. Gupta, D., Asrani, S.: Macular thickness analysis for glaucoma diagnosis and management. Taiwan J Ophthalmol, 6; 2016 : 3-7.
5. Chang, RT., Knight, OJ.: Sensitivity and specificity of time-domain versus spectral-domain optical coherence tomography in diagnosing early to moderate glaucoma. Ophthalmology, 116; 2009 : 2294-9.
6. Kaushik, S., Kataria P., Jain V. et al.: Evaluation of macular ganglion cell analysis compared to retinal nerve fiber layer thickness for preperimetric glaucoma diagnosis. Indian J Ophthalmol, 66; 2018 : 511-516.
7. Kerrigan-Baumrind, LA., Quigley, HA., Pease, ME. et al.: Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci, 41; 2000 : 741-8.
8. Mansoori, T., Viswanath, K., Balakrishna, N.: Ability of spectral domain optical coherence tomography peripapillary retinal nerve fiber layer thickness measurements to identify early glaucoma. Indian J Ophthalmol, 59; 2011 : 455-9.
9. Němec, P. OCT angiografie. In: Němec, P., Löfflerová, V., Kousal, B.: Optická koherenční tomografie Klinický atlas sítnicových patologií, Praha: Mladá fronta a.s., 2015. s. 275-280. ISBN 978-80-204-3810-2.
10. Oddone, F., Michelessi, M., Parravano, M. et al.: Macular versus Retinal Nerve Fiber Layer Parameters for Diagnosing Manifest Glaucoma: A Systematic Review of Diagnostic Accuracy Studies. Ophthalmology, 123; 2016 : 939-49.
11. Řehák, J. Onemocnění sítnice. In: Rozsíval, P. a kol.: Oční lékařství. Praha: Galén, 2006. s. 243-276. ISBN 80-7262404-0.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 5-
All articles in this issue
- Vodiace psy sa cvičia na Slovensku už 25 rokov
- The long-term monitoring of sympathetic ophthalmia in the diagnostic and terapeutic view. Review Department of Ophthalmology
- The optic nerve drusen and haemodynamics
- Sensitivity and specificity of spectral OCT in patients with early glaucoma.
- Nanolaser in cataract surgery and its impact on corneal endotelium
- Molecular genetic cause of achromatopsia in two patients of Czech origin
- INTRAVITREAL THERAPY OF ENDOGENOUS ENDOPHTALMITIS DUE TO UROSEPSIS – A CASE REPORT
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Molecular genetic cause of achromatopsia in two patients of Czech origin
- INTRAVITREAL THERAPY OF ENDOGENOUS ENDOPHTALMITIS DUE TO UROSEPSIS – A CASE REPORT
- Sensitivity and specificity of spectral OCT in patients with early glaucoma.
- The long-term monitoring of sympathetic ophthalmia in the diagnostic and terapeutic view. Review Department of Ophthalmology
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


