-
Medical journals
- Career
Peripheral exudative hemorrhagic chorioretinopathy
Authors: Z. Mazal
Authors‘ workplace: Oční oddělení Klaudiánovy nemocnice Mladá Boleslav, Přednosta: prim. MUDr. Zdeněk Mazal
Published in: Čes. a slov. Oftal., 75, 2019, No. 2, p. 80-84
Category: Case Report
doi: https://doi.org/10.31348/2019/2/4Overview
Peripheral exudative hemorrhagic chorioretinopathy (PEHCR) is relatively rare and especially less known and therefore less often diagnosed condition of the retina periphery predominantly in patients of higher age. Usually temporal periphery is affected. The finding is bilateral in approximately 30 %. Clinically it manifests by multibulbar prominences in periphery, which can sometimes resemble choroidal melanoma. It concerns exudations and hemorrhages under retina (sub-retinal) or under retinal pigment epithelium (sub-RPE). Within weeks or months hemorrhagy is resorbed and flattened and chorioretinal atrophy of various grade remains in affected area, sometimes combined with retinal fibrosis. If the affected area remains limited to the periphery, the central visual acuity does not have to be reduced. Affection is considered to be peripheral form of wet age-related macular degeneration or peripheral form of idiopathic polypoidal choroidal vasculopathy. By differential diagnosis is necessary to exclude especially malignant choroidal melanoma and choroidal detachment.
Case report: Own case of 83 years old patient with bilateral PEHCR is described and photo documented. Creation of new prominence - fresh bleeding under retina and RPE in superior periphery – had been captured. Photo documentation of lesion in early stage and in stage of resorbtion after several weeks. Affected areas remained limited to periphery and did not have influence on central vision. That was influenced by degeneration of macula and vitreomacular traction syndrome with distinct epiretinal membrane.
Conclusion: PEHCR is less frequent or less diagnosed condition of the retina periphery in old patients. Ongoing exudation and sub-retinal or sub-RPE bleeding. Within weeks heals with chorioretinal scars and subretinal fibrosis. Central vision does not have to be damaged, if lesions do not spread to macula.
Keywords:
peripheral exudative hemorrhagic chorioretinopathy – chorioretinal atrophy – subretinal fibrosis – choroidal melanoma
Introduction
Peripheral exudative haemorrhagic chorioretinopathy (PEHCR) was first described by Annesley in 1980 [1]. It represents a relatively rare affliction primarily of the temporal periphery of the retina, between the ora serrata and the equator, occurring in older patients aged around eighty years. Women are affected more frequently than men [5]. In 30% of cases the pathology is bilateral [1, 5, 11]. It is characterised by varying numbers of haemorrhages and exudations beneath the retina and beneath the retinal pigment epithelium (RPE). Sub-RPE haemorrhages generally have a slightly domed shape, are of dark grey colour, and may resemble choroidal melanoma [9, 10]. The macula is mostly not affected, and as a result there need be no influence on central vision [5]. The course of the pathology is variable, in most cases there is a gradual resorption of haemorrhages and exudates/transudates, and a flattening of lesions over the course of weeks to months. Lesions and areas of chorioretinal atrophy, hyperplasia of the RPE and subretinal fibrosis of various degrees then remain in the affected areas. During the course of healing fresh lesions may occur, and as a result we may see lesions in various stages of healing. The precise etiology is unclear. The pathology is considered to be a peripheral variant of wet-form age-related macular degeneration (ARMD) or polypoidal choroidal vasculopathy (PCV) [2-4, 10]. Fluorescence angiography (FA) usually shows a complete blockade of choroidal fluorescence [9, 11, 12], on ultrasound B (US-B) we see flat to slightly domed prominences with various degrees of reflexivity [9, 11, 12]. On the basis of an examination with indocyanine green angiography (ICGA), according to some authors this probably concerns a spectrum of peripheral vasculopathies, with or without choroidal polyps [5, 12]. Using differential diagnostics it is most important to distinguish the pathology from choroidal melanoma. PEHCR is usually localised between the ora serrata and the equator [11], whereas melanoma is mostly localised between the macula and the equator [11]. PEHCR often affects one and more quadrants, whereas melanoma mostly affects less than one quadrant [11]. PEHCR is frequently bilateral, while melanoma is mostly unilateral [9]. Application of preparations blocking vascular endothelial growth factor (anti-VEGF) is therapeutically attempted in cases of affliction of the macula [7, 12]. A beneficial “drying” effect has been demonstrated, which however is not always permanent [7].
Own observation
In a routine examination of an 83-year-old female patient before cataract surgery, prominent greyish sub-retinal haemorrhages and haemorrhagic ablations of the RPE were detected in the upper and nasal periphery of the left eye (LE), some of them already in gradual resorption (fig. 1). In the temporal lower periphery there were areas of chorioretinal atrophy. In the central landscape there was a pronounced epiretinal membrane, with vitreoretinal traction. FA demonstrated a complete blockade of basal fluorescence in the places of fresh sub-retinal and sub-RPE haemorrhages (fig. 2). US-B demonstrates low prominences of various reflexivity and on optical coherence tomography (OCT) we see haemorrhagic ablation of the RPE (fig. 3a, 3b). In the right eye (RE) areas of older chorioretinal atrophy were determined primarily in the lower periphery, with sub-retinal fibrosis and irregular hyperplasia of retinal pigment (fig. 4). The patient was observed regularly. During the course of the observation, cataract surgery was performed on the LE, and later pars plana vitrectomy for vitreomacular traction syndrome (VMTS). The peripheral haemorrhages and exudations in the LE were gradually resorbed, and chorioretinal atrophy appeared in the affected areas. After 18 months a fresh blackish-grey prominence formed in the upper temporal quadrant of the left eye, caused by sub-retinal and sub-RPE haemorrhage (fig. 5a). Over the course of a number of weeks we observed clear resorption, flattening and formation of sub-retinal fibrosis (fig. 5b). During the observation period of approximately 30 months, the lesions did not spread across the vascular arcade, and did not influence central vision. This is influenced partially by dry-form ARMD, and partially by the effects of VMTS, but not as a consequence of PEHCR. For this reason I do not state the values of vision. In the right eye the finding was unchanged, and throughout the entire observation period the original chorioretinal atrophy persisted, with sub-retinal fibrosis of an older provenance.
1. a. Sub-retinal and sub-RPE haemorrhages in LE 
Fig. 1.b. Sub-retinal and sub-RPE haemorrhages in partial resorption in LE 
2. FA of peripheral lesions – blockade of basal fluorescence in LE 
3. a. US-B peripheral lesions in LE 
Fig. 3.b. OCT haemorrhagic ablation of RPE 
4. Atrophic lesion with fibrosis in RE 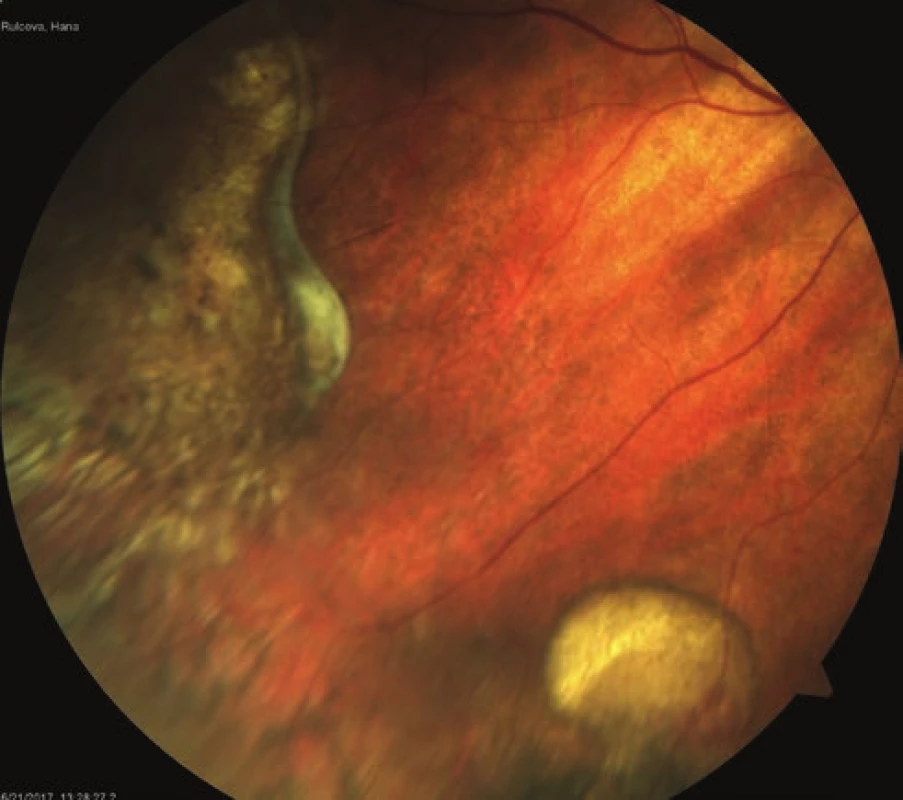
5. a. Fresh lesion of sub-RPE haemorrhage in LE 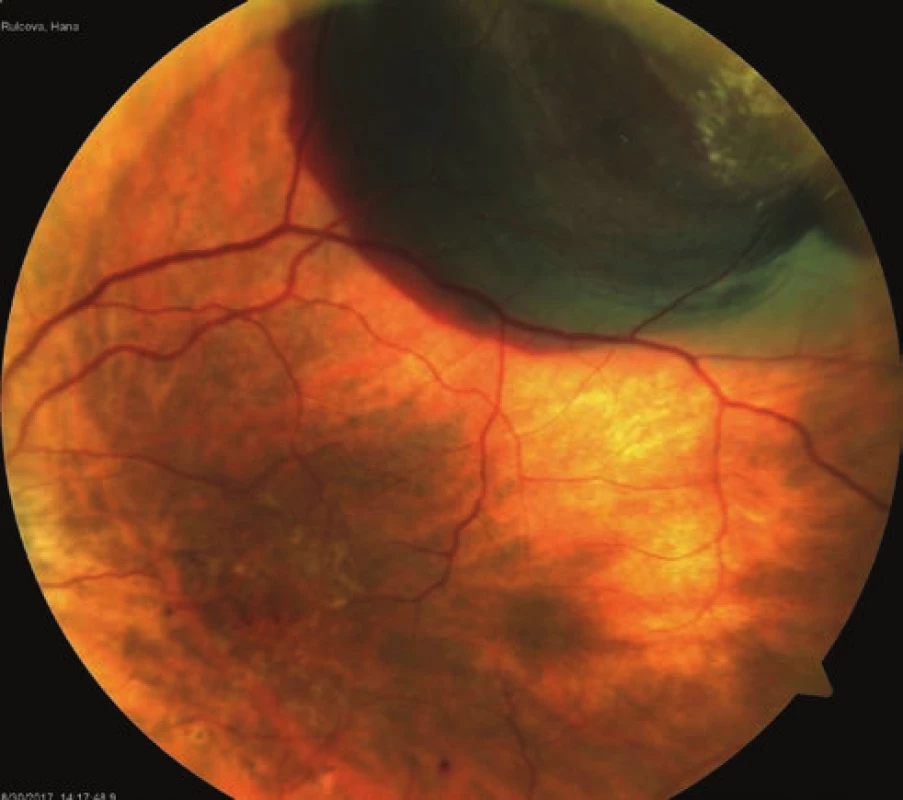
Fig. 5.b. Condition of the same lesion after 2 months of continual resorption 
Discussion
PEHCR is considered a relatively rare pathology. This may be contributed to by the peripheral localisation of the described lesions, which very often do not influence central vision, and are therefore not diagnosed in the acute phase. Following spontaneous resorption, only areas of non-specific chorioretinal atrophy with hyperplasia of the RPE remain, in some cases with sub-retinal fibrosis. The diagnosis rests upon an ophthalmoscopic and biomicroscopic finding supplemented with FA or ICGA, and also US-B and OCT. Quality photo-documentation of the peripheral lesions with a regular fundus camera may be difficult, especially in the case of a more constricted pupil. In differential diagnostics it is necessary to consider above all choroidal or ciliary body melanoma, and also to consider ciliochoroidal ablation (following intraocular surgery, ocular decompression syndrome), or ciliochoroidal effusion (idiopathic, uveitis, scleritis, nanophthalmos). It is necessary to observe patients above all in the acute phase, and to exclude the possibility of the aforementioned choroidal melanoma.
The finding in our patient fully corresponds to the descriptions found in the literature [1-13].
Conclusion
PEHCR is a rarely diagnosed affliction of the retinal periphery in older patients, in which haemorrhage and exudation occurs beneath the retina and/or retinal pigment epithelium. After a number of weeks to months, the lesions begin to flatten, leaving areas of chorioretinal atrophy with hyperplasia of the RPE. In some cases sub-retinal fibrosis occurs. PEHCR need not have an influence on central vision. In the initial phases we must above all differentiate the condition from malignant melanoma of the choroid and ciliary body, and as a result it is necessary to observe the patient. The pathology is considered a peripheral form of wet-form ARMD and/or PCV. Therapeutically, anti-VEGF preparations are applied to patients with affliction of the macula.
This study was presented in an abridged form as a lecture at the Congress of the Czech Vitreoretinal Society [ČVRS] 2017 in Mikulov.
Declaration
The author of the study declares that no conflict of interest exists in the compilation and theme of this professional communication, and that it is not supported by any company.
Received by the Editorial Department on: 01 February 2019
Accepted for printing on: 07 March 2019
MUDr. Zdeněk Mazal
Havlíčkova 880
29301 Mladá Boleslav
e-mail: zdenek.mazal@onmb.cz
Sources
1. Annesley, WH Jr.: Peripheral exudative hemorrhagic chorioretinopathy. Trans Am Ophthalmol Soc, 78; 1980 : 321-364.
2. Collaer, N., James, C.: Peripheral exudative and hemorrhagic chorio-retinopathy…the peripheral form of age-related macular degeneration? Report on 2 cases. Bull Soc Belge Ophtamol, 305; 2007 : 23-26.
3. Goldman, DR., Freund, KB., McCannel, CA.: Peripheral polypoidal chorioideal vasculopathy as a cause of peripheral exudative hemorrhagic chorioretinopathy: A report of 10 eyes. Retina, 33(1); 2013 : 48-55.
4. Mantel, I., Schalenbourg, A., Zografos, I.: Peripheral exudative hemorrhagic chorioretinopathy: polypoidal chorioideal vasculopathy and hemodynamic modifications. Am J Ophthalmol, 153(5); 2012 : 910-922.e2.
5. Mantel, I., Uffer, S., Zografos, I.: Peripheral exudative hemorrhagic chorioretinopathy: a clinical, angiografic and histologic study. Am J Ophthalmol, 148(6); 2009 : 932-938.
6. Mashayekhi, A., Shields, CL., Shields, JA.: Peripheral exudative hemorrhagic chorioretinopathy: a variant of polypoidal chorioideal vasculopathy? J Ophthalmic Vis Res, 33(1); 2013 : 264-267.
7. Sabherwal, NS., Chris, JL., Shields, CL.: Peripheral exudative hemorrhagic chorioretinopathy simulating chorioideal melanoma. Retina Today, 4; 2014 : 47-49.
8. Seibel, I., Hager, A., Duncker, T., et al.: Anti-VEGF therapy in symptomatic peripheral exudative hemorrhagic chorioretinopathy(PEHCR) involving the macula. Graefes Arch Clin Exp Ophthalmo, 254(4); 2016 : 653-659.
9. Shields, CL., Furuta, M., Thangappan, A., et al.: Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol, 127; 2009 : 989-998.
10. Shields, JA., Mashayekhi, A., Ra, S.: Pseudomelanomas of the posterior uveal tract: the 2006 Taylor R.Smith Lecture. Retina, 25(6); 2005 : 767-771.
11. Shields, CL., Sakazar, PF., Mashayekhi, A.: Peripheral exudative hemorrhagic chorioretinopathy simulating chorioideal melanoma in 173 eyes. Ophthalmology, 116(3); 2009 : 529-535.
12. Studnička, J.: Periferní exudatívní hemoragická chorioretinopatie. In Studnička, J. et al.: Onemocnění sítnice a cévnatky v praxi. Praha, Mladá fronta, 2018, s. 142-144.
13. Warren, A., Welch, J., Shields, CL.: Peripheral exudative hemorrhagic chorioretinopathy with polyps. Retina Today, 12(2); 2017 : 38-40.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 2-
All articles in this issue
- Očná klinika Lekárskej fakulty Univerzity Komenského v Bratislave oslavuje 100-TÉ VÝROČIE činnosti – 1. časť
- Normal tension vs high tension glaucoma: an – overview
- Correction of myopia and myopic astigmatism by femtosecond laser in situ keratomileusis
- Effect of Botulinum toxin A application in neuro-ophtalmologic indications on Schirmer’s test and tears osmolarity.
- Peripheral exudative hemorrhagic chorioretinopathy
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Normal tension vs high tension glaucoma: an – overview
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Peripheral exudative hemorrhagic chorioretinopathy
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

