-
Medical journals
- Career
Influence of prophylactic melatonin administration on the incidence of early postoperative delirium in cardiac surgery patients
Authors: B. Bilý 1; F. Sabol 1; P. Török 2; P. Artemiou 1; M. Bilecová-Rabajdová 3; P. Kolarcik 4
Authors‘ workplace: University of P. J. Safarik in Kosice, Medical Faculty, Dept. of Cardiovascular Surgery, Eastern Slovak Institute for Cardiovascular Diseases, Kosice, Slovakia 1; University of P. J. Safarik in Kosice, Medical Faculty, Dept. of Cardiac Anesthesia, Eastern Slovak Institute for Cardiovascular Diseases, Kosice, Slovakia 2; University of P. J. Safarik in Kosice, Medical Faculty, Dept. of Clinical Biochemistry, Slovakia 3; University of P. J. Safarik in Kosice, Medical Faculty, Dept. of Public Health, Slovakia 4
Published in: Anest. intenziv. Med., 26, 2015, č. 6, s. 319-327
Category: Anaesthesiology - Original Paper
Overview
Objective:
Postoperative delirium in cardiac surgery is a severe complication. The circadian rhythm of melatonin secretion has shown to be altered postoperatively. It was hypothesized that by prophylactic supplementation of a substance that is capable of resynchronizing circadian rhythm such as melatonin may be possible to reduce the incidence of postoperative delirium.Design:
It is prospective interventional clinical study.Setting:
A specialized institute of tertiary level health care.Material and methods:
Two consecutive groups (control and melatonin group) of 250 consecutive patients were enrolled. In the melatonin group the patients received orally 5 mg of prophylactic melatonin treatment the evening before surgery and then every evening until postoperative day 3.Results:
The incidence of the delirium was 8.4% in melatonin group vs. 20.8% in control group (p = 0.001). Predictors of delirium in melatonin group were age (p = 0.001) and higher EuroSCORE II value (p = 0.001). In multivariate analysis of age and EuroSCORE II value (p = 0.014) were predictors of postoperative delirium. By comparing the group together main predictors of delirium were age (p = 0.001), EuroSCORE II value (p = 0.001), CPB time (p = 0.001), ACC time (p = 0.008), sufentanil dose (p = 0.001), mechanical ventilation (p = 0.033).Conclusion:
The administration of melatonin appears to be associated with a significant decrease of postoperative delirium incidence after cardiac surgery and it should be considered in patients scheduled for cardiac surgery.Keywords:
delirium – prevention – melatonin – cardiac surgeryINTRODUCTION
Postoperative delirium (POD) after cardiac surgery is a severe complication which can be developed in any patient during the early postoperative period and is characterized by altered consciousness and global cognitive disturbances. The delirium has been reported to occur in 10% to 60% of surgical patients [1]. Moreover in ICU, up to 81% of patients manifest delirium [2].
Melatonin is a neurohormone that is synthetized from tryptophan and secreted mainly by the pineal gland and is released directly into the bloodstream in a circadian pattern governed by the light and dark cycle. It produces hypnotic effects by accelerating sleep initiation and improving sleep maintenance and efficiency. This circadian rhythm of melatonin secretion has shown to be altered postoperatively and this may lead to changes in the sleeping patterns [3]. Moreover, its plasma levels are decreased after surgery and in hospitalized patients [4].
Delirium and perioperative sleep disturbance are potentially linked, either as predisposing factors or as symptoms of one another.
Delirium after cardiac surgery is associated with increased morbidity and mortality as well as prolonged length of stay in the intensive care unit and the hospital [5].
Thus it was hypothesized that by prophylactic supplementation of a substance that is capable of resynchronizing circadian rhythm such as melatonin may be possible to reduce the incidence of POD. Synthetic melatonin supplements were also proved to be successful when used as a premedication to decrease anxiety and sedate patients preoperatively with an excellent cognitive profile [6].
The aim of this prospective interventional study was to describe the effect of melatonin supplementation in the prevention of POD in cardiac surgery patients.
Design
It is prospective single center interventional non-randomized clinical study.
Setting
A specialized institute of tertiary level health care.
MATERIALS AND METHODS
In this clinical study the patients were divided into two consecutive groups. The clinical study was realized from September 2012 to July 2013. The first group (group A) which was the control group included 250 consecutive patients needing various types of cardiac surgery and operated in an elective or urgent regime. The second group (group B) included 250 subsequent, consecutive patients presenting the same conditions and treatments, and receiving prophylactic perioperative melatonin treatment. The patients received orally 5 mg of melatonin (Circadin®, Neurim Pharmaceuticals EEC Limited, UK). The first dose was given in the evening before surgery and the treatment was continued orally every evening the same time until the postoperative day 3. Patients that were operated on an emergency regimen were excluded from the study. Medical history, preoperative (concomitant diseases or risk factors such as hypertension, diabetes mellitus, hypercholesterolemia, smoking, alcoholism, previous psychiatric disease), perioperative (type of operation, duration of cardiopulmonary bypass and aortic cross-clamp, doses of opiates and benzodiazepines administered during the operation) and post-operative (duration of mechanical ventilation > 24 hours, ICU and hospital stay) of all enrolled patients were recorded.
The use of physical supporting aids for walking (G-apparatus) and as much as possible early mobilization could be an effective preventive strategy to decrease the development of postoperative delirium. In our protocol was an attempt that patients with an uncomplicated postoperative course were mobilized to 2nd postoperative day.
The EuroSCORE II value was calculated to evaluate the operative risk. It was calculated for all patients in both groups and they were categorized into three groups as high, moderate and low score (low risk < 1.6%, moderate risk 1.6–6.7%, high risk > 6.7%).
Cardiac surgery, the anesthetic procedures and the postoperative management were standardized.
Ethical approval
Institution’s ethics committee approved the study. Written informed consent was obtained from all participants in the study.
Anesthetic technique
All patients in both groups received premedication of 10 mg oxazepam the evening before surgery and 7.5 mg of midazolam 1 to 2 h before surgery. Anesthesia was induced by 2.5–5 mg midazolam, 2–2.5 mg/kg propofol, sufentanil 0.01–0.025 mg and sevoflurane 1–2 %. Tracheal intubation was facilitated by 0.6–1 mg/kg atracurium. Anesthesia was maintained with sufentanil infusion 0.0005 mg/kg/h and sevoflurane 1–2% while neuromuscular blockade was maintained with the administration of atracurium 50 mg every 40 minutes. No propofol was administrated during anesthesia maintenance.
Surgery-conduct of cardiopulmonary bypass
All surgery procedures were performed through median sternotomy. For patients undergoing off-pump surgery anticoagulation was achieved with heparin (half of the standard dose) to maintain an activated clotting time about 280 s and distal anastomoses were performed with the help of a tissue vacuum stabilizer (ACROBAT V, MAQUET Holding GmbH). No-touch aorta technique was used in off-pump surgery. Nasopharyngeal temperature was maintained above 35 °C and systolic blood pressure was kept at 80 mmHg or greater throughout the procedure.
For patients undergoing on-pump surgery anticoagulation was achieved with heparin to maintain an activated clotting time above 480 s and the cardiopulmonary bypass circuit was primed with 1 L of Ringer’s Lactate, 250 ml of 20% mannitol and 16 mg of dexamethasone. Mild hypothermia of 34–35 °C was induced during cardiopulmonary bypass, the pump flow rate was 2.4–2.8 l/min/m2 and the mean perfusion pressure were between 70–75 mmHg. A perfusionist kept the desired blood pressure by the following maneuvers: flow correction, correction of drainage and administration of inotropic support (0.2 mg of noradrenaline). Hematocrit was kept between 25–35%. Myocardial protection was achieved with intermittent blood-enriched cold cardioplegic solution (3–6 °C of St. Thomas cardioplegic solution) using a blood to crystalloid ratio of 5 : 1. Fractional concentration of inspired oxygen was adjusted to keep arterial oxygen tension between 150–250 mmHg, and gas flow was adjusted to maintain arterial carbon dioxide tension between 35–40 mmHg without temperature correction (α-stat).
After all distal anastomoses were done, the aortic cross-clamp was removed and proximal anastomoses where then performed by means of a single side-clamp on the aorta.
Postoperative management
After surgery, all the patients were admitted to the cardiosurgical ICU, where was implemented an internal standard protocol of institution for sedation, analgesia and management of mechanical ventilation in all of the patients. Patients were extubated according to the following criteria: responsive and cooperative, pO2 of 10–11 kPa and oxygenation index of PaO2/FiO2 > 300. In the ICU patients were sedated with propofol until extubation. Analgesia was provided with intravenous morphine infusion at 2 mg/h, Algifen® (active ingredients: metamizole, pitofenone, fenpiverinium; Zentiva Group a.s. Czech Rep.) 2.5 g every 8 hours and intravenous tramadol 100 mg every 8 hours.
Delirium assessment
Delirium was assessed with the CAM-ICU (The Confusion Assessment Method for the Intensive Care Unit) every 12 h postoperatively [7]. The CAM-ICU allows the monitoring of delirium in both ventilated and extubated patients. It is based on the Diagnostic and Statistical Manual of Mental Disorders criteria and includes a 4-step algorithm. The patient is determined to be delirious (CAM-positive) if he or she manifests standard features for delirium.
All cardiovascular ICU staff was educated and well trained in the application of the CAM-ICU in both ventilated and non-ventilated patients.
The level of sedation (level of arousal) was assessed by means of the Richmond Agitation Sedation Scale (RASS) [8].
Statistical analysis
Data are given as mean value ± standard deviation (SD). Categorical variables are presented as numbers of patients (percentage). A univariate analysis was performed to identify perioperative risk factors in both groups associated with delirium using Chi-square analyses or Fisher’s Exact Test. Different cut-off points for continuous variables were examined to determine the best association with delirium. Odds ratios (OR) were calculated to indicate the effect size of perioperative risk factors on delirium. Variables associated with outcome with a p value < 0.05 in the univariate analyses and variables considered clinically significant were entered into multiple logistic regression model for delirium in order to identify independent risk factors. This was performed by using stepwise logistic regression technique. Finally, both groups A and B were between them statistically matched, analyzed and compared.
For statistical analysis the SPSS software version 22 (SPSS Inc., Chicago, IL, USA) was used.
RESULTS
Two groups of 250 patients were enrolled in the study. Fifty two (20.8%) patients from the control group developed POD. POD developed in 21 (8.4%) patients from the melatonin group (p = 0.001). The patients developed a hyperactive and mixed type of delirium.
The preoperative and perioperative clinical patient’s characteristics of the two groups are shown in Table 1.
1. The preoperative, perioperative and postoperative clinical patient's characteristics: comparison of the control group and melatonin group 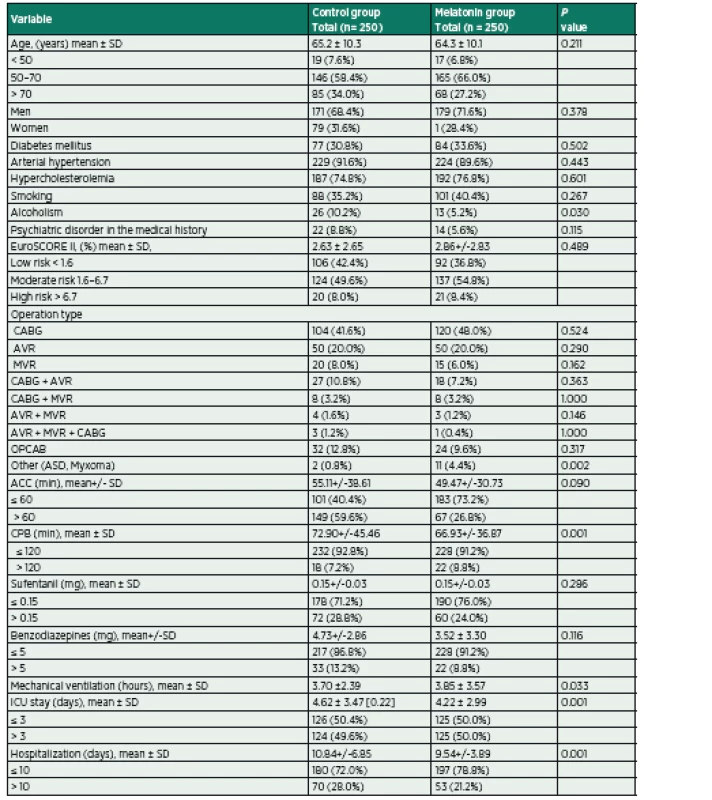
Abbreviations: n = number, SD = standard deviation, CABG = coronary artery bypass graft surgery, AVR = aortic valve replacement, MVR = mitral valve replacement, OPCAB = off - pump coronary artery bypass, ASD = atrial septal defect, ACC = aortic cross-clamping, min = minute, CPB = cardio-pulmonary bypass, mg = milligram, ICU = intensive care unit Patients with postoperative delirium in both groups had a longer ICU stay (p <0.0001, p = 0.001 respectively). Also hospital stay was prolonged(p < 0.0001, p = 0.002 respectively).
Univariate analysis considering only patients from group A showed that older age (p < 0.0001), higher EuroSCORE II value (p < 0.0001), longer CPB (p < 0.0001) and ACC (p < 0.0001) time and sufentanil dose (p = 0.001) were associated with POD.
In multivariate analysis all the previously described associations, also benzodiazepine dose and CABG as type of operation were shown predictors of POD (Table 2).
2. Multivariate analysis of all enrolled patients 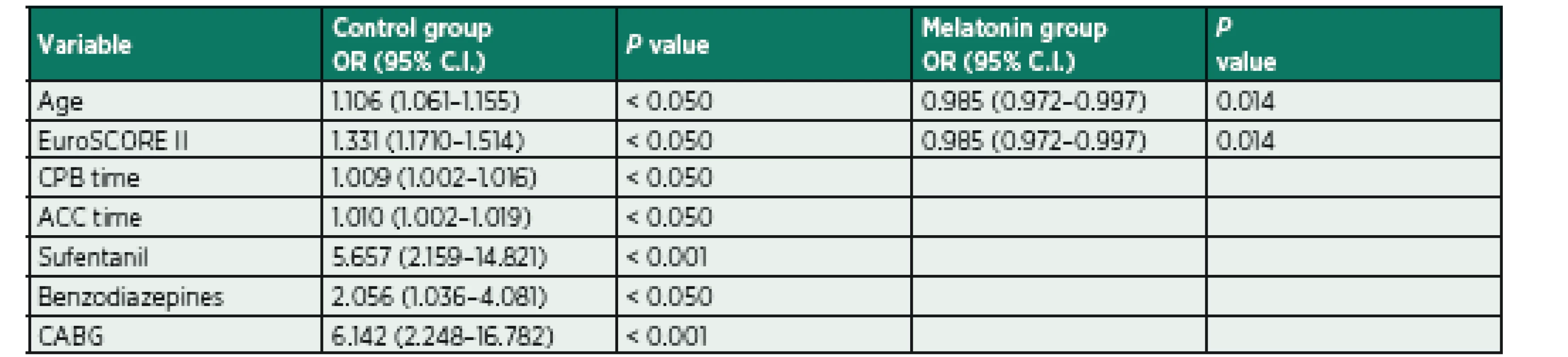
Abbreviations: OR = odds ratio, C.I. = confidence interval, CPB = cardio-pulmonary bypass, ACC = aortic cross-clamping, CABG = coronary artery bypass graft surgery Univarate analysis considering only patients from group B showed that only age (p = 0.001) and EuroSCORE II value (p = 0.001) were associated with POD development. Same trend was present concerning CPB time > 120 min (p = 0.097).
Benzodiazepine administration was shown in the control group to be a predictor of POD (p < 0.050). In the melatonin group this finding was not demonstrated (p = 0.809).
Table 2 shows the multivariate analysis of the enrolled patients.
After matching, the two groups were found to be comparable. The only variable that could not match was consumption of alcohol. The number of the patients was low so it could not have any effect on the results. The comparison of the two groups is shown in Table 1.
After matching of the two groups older age (p = 0.001), higher EuroSCORE II (p = 0.001), CABG type of operation (p = 0.003) and CABG and combined valve operations (p = 0.018, p = 0.010 respectively) were all confirmed to be associated with an increased risk for the development of POD. Perioperative predictors connected with the operative time, such as CPB time (p = 0.001), ACC time (p = 0.008), sufentanil dose >0.15 mg (p = 0.001) were also associated with the development of POD. Increased ventilation time (p = 0.033) was also associated with the POD. Patients suffered from POD had prolonged ICU stay (p = 0.001). Also hospital stay was prolonged (p = 0.001).
The statistical analysis of the variables of both groups based on the incidence of the postoperative delirium is shown in Table 3.
3. The statistical comparison analysis of both groups based on the incidence of the postoperative delirium 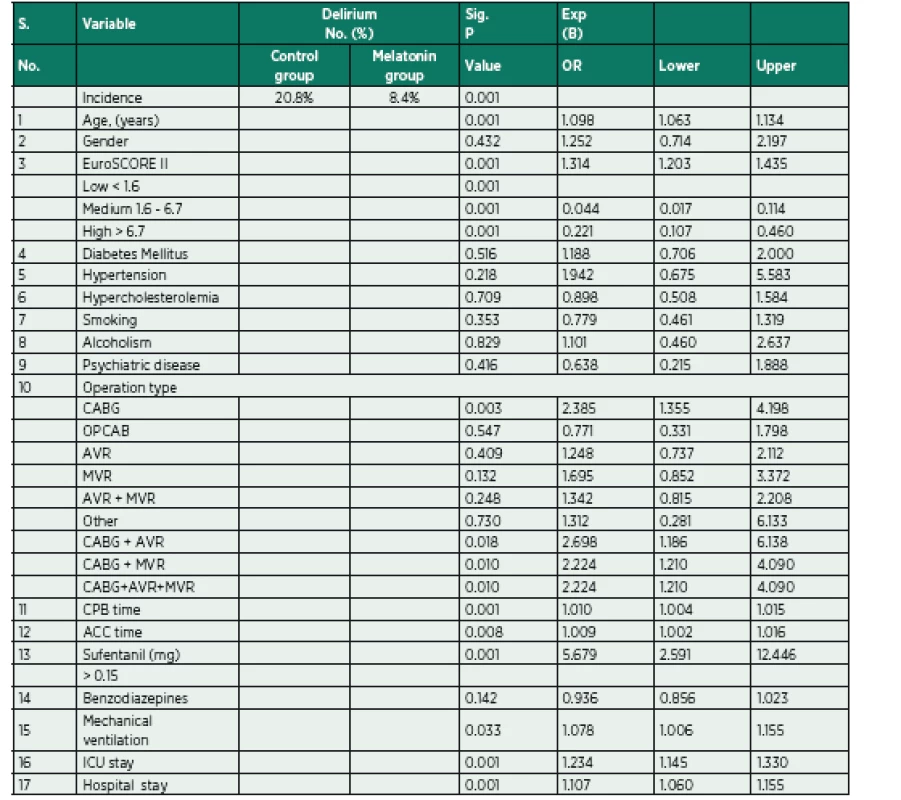
Abbreviations: S. = subject, No. = number, sig. = significant, Exp(B) = coefficient, OR = odds ratio, C.I. = confidence interval, CABG = coronary artery bypass graft surgery, OPCAB = off-pump coronary artery bypass, AVR = aortic valve replacement, MVR = mitral valve replacement, CPB = cardio-pulmonary bypass, ACC = aortic cross-clamping, mg= milligram, ICU = intensive care unit The hospital mortality in each group of patients was 1.6%.
DISCUSSION
In the present study the incidence of postoperative delirium in the melatonin group was 8.4%. It was significantly lower than the incidence of 20.8% in the control group. Sultan SS [9] showed in his study of three hundred patients scheduled for hip arthroplasty that only preoperative melatonin administration succeeded significantly in decreasing the incidence of postoperative delirium to 9.43%. Recently, a study concluded that low-dose melatonin in elderly medical patients admitted in the emergency department decreases the risk of delirium [10]. On the contrary, recently was realized multicentre randomized controlled trial in the Netherlands among elderly patients with hip fracture by A de Jonghe et al. [11]. The result of the study was that treatment with melatonin did not reduce the incidence of delirium.
In the present study in the melatonin group only older age and the higher EuroSCORE II value were shown to be strongly associated with the development of delirium. Certain variables such as CPB, ACC time and sufentanil dose are all linked to a common parameter – the operative time. Supplementation of melatonin reduced the parameter of time in the development of POD.
After matching the two groups older age, higher EuroSCORE II, CABG type of operation and CABG combined with valve operations were all confirmed to be associated with an increased risk for the development of POD.
Age has consistently been reported as a predictor of postoperative delirium [12].
Concerning, EuroSCORE value Osse RJ et al. [13] found that EuroSCORE value greater than 6 was associated with the incidence of the postoperative delirium.
Chronic alcoholism is in the available literature considered as a risk factor for postoperative delirium [14]. In our clinical study alcoholism (a chronic, progressive disease that includes problems controlling of alcohol consumption) was not strongly associated with delirium. The relatively small sample size of cardiac surgery patients with alcohol abuse could be responsible for the fact that in our patient’s population chronic alcoholism was not significantly associated with the development of POD.
Another two intraoperative predictors found in our study to be associated with POD represent longer CPB and ACC times. Patients who had CPB time more than 120 min had a 15 times higher risk for developing POD. Also, the longer the ACC time the higher the risk for POD. Other reports in the literature have similar results. Andrejaitiene J et al. [15] found that ACC time > 68 min is associated with the development of delirium. Similar results are reported also by other authors [16]. It has been hypothesized that cerebral atherosclerosis combined with postsurgical inflammatory changes may inhibit cerebral blood flow. This condition may be exacerbated by the non-pulsatility of CPB [17]. Longer duration of surgery is correlated with longer CPB. Brown WR et al. [18] showed that increased duration of CPB was associated with increased gaseous embolic load to the brain. Longer surgical duration may also mean a more complex procedure. These cases require more heart and major vascular manipulation with resultant embolic phenomena.
Increased ventilation time was also associated with the development of POD. Other authors showed that the duration of ventilation (prolonged ventilation > 24 hours) is as independent predictor of POD [19].
Furthermore, it was here shown that the higher the sufentanil dose (the patients in our study were running a fixed dose per kg per minute), the higher the risk for developing POD. The sufentanil dose is linked with time. So the longer the duration of the operation, the higher the sufentanil dose, the higher risk for developing POD. Burkart CS et al. [20] showed that an increasing dose of fentanyl administered intraoperatively appeared to be a risk factor for POD.
Gunaydin B et al. [21] found a higher rate of delirium in patients after high dose fentanyl ane-sthesia compared with barbiturate anesthesia without the use of fentanyl.
It was here shown that the benzodiazepine dose in the control group represented a weak predictor for developing POD, whereas in the melatonin group did not. Pandharipande P et al. [22] also showed that exposure to benzodiazepines is one of the strongest modifiable risk factors for POD development. In our study the patients developed a hyperactive and mixed type of delirium. McPherson JA et al. [23] showed that patients who received benzodiazepines and are restrained after heart surgery had hypoactive type of delirium. Avoiding chemicals restrains via use of benzodiazepines and as much as possible early mobilization appear like an effective preventive strategy in order to decrease the development of the POD. In our department a patients with an uncomplicated postoperative course were usually mobilized on 1st or 2nd postoperative day. Patients with complicated postoperative course were mobilized later on 4th to 7th postoperative day, so there is room for improvement in this issue.
In our study from different types of the operation only CABG and CABG combined with valve operation were associated with the development of POD. Other authors showed also a higher incidence of delirium in patients undergoing valve replacement and combined surgery with valve replacement and CABG compared with patients undergoing isolated CABG [24]. The reason for this according to the authors may be the embolization of air which is trapped within the cardiac chambers during the valve replacement surgery. In presented study, the relatively small sample size of valve replacement patients compared with the CABG patients sample could be responsible for the fact that in our patients population CABG surgery alone or combined with valve surgery and not valve surgery is associated with the development of POD.
In our study the time frame for early post cardiac surgery delirium is defined 2–6 days after the operation. Delirium diagnosed on the first or after the sixth day following cardiac surgery might not be directly connected to the surgery [5].
In the literature there are not enough studies examining the role of prophylactic melatonin in the prevention of POD, especially in post cardiac surgery patients. Moreover, in the literature there is not enough evidence concerning the predictors of POD after melatonin supplementation. These two aspects may be considered the strengths of this study.
The study has some limitations. Firstly, we did not perform baseline psychiatric and cognitive screening tests. Any psychiatric disorders that were examined in our study were obtained from the medical history of the patient and their incidence could be underestimated. Finally, the CAM-ICU assessment was performed in the cardiovascular ICU and was not extended to the cardiac surgical floor, so our findings can only be applied to early postoperative delirium.
CONCLUSION
The supplementation of melatonin seems to significantly decrease the incidence of postoperative delirium after cardiac surgery. Moreover, it could reduce various risk factors here found related to postoperative delirium development in patients who did not received melatonin treatment. Even, after the melatonin treatment, risk factors such as age, EuroSCORE II value, cardio-pulmonary bypass and aortic cross-clamping time, sufentanil dose, ventilation time and operation type may increase in lesser degree the risk of postoperative delirium, another perioperative strategies should be developed, in order to decrease more the incidence of postoperative delirium in cardiac surgery patients.
- All authors declare none conflict of interest.
- All authors have read and approved of the manuscript being submitted.
- The clinical research was done according to ethical standards. All the study participants provided a written informed consent.
- No institution provided financial support for the conduct of the research and/or preparation of the manuscript.
- All authors declare, that submitted manuscript or any parts of its essential substance /tables/ have not been published previously in print form or electronically.
Do redakce došlo dne 1. 7. 2015.
Do tisku přijato dne 1. 9. 2015.
Adresa pro korespondenci:
MUDr. Boris Bílý
UPJŠ LF a VÚSCH a. s.
Ondavská 8
040 11 Košice
Slovenská republika
e-mail: boris_bil@yahoo.co.uk
Sources
1. Norkiene, I., Ringaitiene, D., Misiuriene, I. et al. Incidence and precipitating factors of delirium after coronary artery bypass grafting. Scan Cardiovasc. J., 2007, 41, 3, p. 212–217.
2. Afonso, A., Scurlock, C., Reich, D. et al. Predictive model for postoperative delirium in cardiac surgical patients. Semin. Cardiothorac. Vasc. Anesth., 2010, 14, 3, p. 212–217.
3. Dispersyn, G., Pain, L., Challet, E., Touitou, Y. General anesthetics effects on circadian temporal structure: an update. Chronobiol. Int., 2008, 25, p. 835–850.
4. Cronin, A. J., Keifer, J. C., Davies, M. F. et al. Melatonin secretion after surgery. Lancet, 2000, 356, p. 1244–1245.
5. Bucerius, J., Gummert, J. F., Borger, M. A. et al. Predictors of delirium after cardiac surgery delirium: effect of beating heart (off-pump) surgery. J. Thorac. Cardiovasc. Surg., 2004, 27, p. 57–64.
6. Caumo, W., Torres, F., Moreira, N. L. et al. The clinical impact of preoperative melatonin on postoperative outcomes in patients undergoing abdominal hysterectomy. Anesth. Analg., 2007, 105, p. 1263–1271.
7. Ely, E. W., Margolin, R., Francis, J. et al. Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Critical Care Medicine, 2001, 29, p. 1370–1379.
8. Ely, E. W., Truman, B., Shintani, A. et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation Sedation Scale (RASS). JAMA, 2003, 289, p. 2983–2991.
9. Sultan, S. S. Assessment of role of perioperative melatonin in prevention and treatment of postoperative delirium after hip arthroplasty under spinal anesthesia in the elderly. Saudi J. Anaesth., 2010, 4, 3, p. 169–173.
10. Al-Alma, T., Brymer, C., Gutmanis, I. et al. Melatonin decreases delirium in elderly patients: A randomized, placebo-controlled trial. Int. J. Geriatr. Psychiatry, 2011, 26, p. 687–694.
11. de Jonghe, A., van Munster, B. C., Gosling, J. C. et al. Effect of melatonin on incidence of delirium among patients with hip fracture: a multicentre, double-blind randomized controlled trial. CMAJ, 2014, 186, 14, p. E547–E556.
12. Kazmiersky, J., Kowman, M., Banach, M. et al. Incidence and predictors of delirium after cardiac surgery. Results from the IPAC study. J. Psychom. Res., 2010, 69, 2, p. 179–185.
13. Osse, R. J., Fekkes, D., Tulen, J. H. et al. High preoperative plasma neopterin predicts delirium after cardiac surgery in older patients. J. Am. Geriatr. Soc., 2012, 60, 4, p. 661–668.
14. Robinson, T. N., Eiseman, B. Postoperative delirium in the elderly: diagnosis and management. Clin. Interv. Aging., 2008, 3, 2, p. 351–355.
15. Andrejaitiene, J., Sirviskas, E. Early post-cardiac surgery delirium risk factors. Perfusion, 2011, 27, 2, p. 105–112.
16. Guenther, U., Theuerkauf, N., Fromman, I. et al. Predisposing and precipitating factors of delirium after cardiac surgery. A prospective observational cohort study. Ann. Surg., 2013, 257, 6, p. 1160–1167.
17. Rudolf, J. L., Jones, R. N., Levkoff, S. E. et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation, 2009, 119, p. 229–236.
18. Brown, W. N., Moody, D. M., Chalva, V. R. et al. Longer duration of cardiopulmonary bypass is associated with greater number of cerebral microemboli. Stroke, 2000, 31, p. 707–713.
19. Lin, Y., Chen, J., Wang, Z. Meta-analysis of factors which influence delirium following cardiac surgery. J. Card. Surg., 2012, 27, 4, p. 481–492.
20. Burkhart, C. S., Dell-Kuster, S., Gamberini, M. et al. Modifiable and non-modifiable risk factors for postoperative delirium after cardiac surgery with cardiopulmonary bypass. J. Cardiothorac. Vasc. Anesth., 2012, 4, p. 555–559.
21. Gunaydin, B., Babacan, A. Cerebral hypoperfusion after cardiac surgery and anesthetic strategies: A comparative study with high dose fentanyl and barbiturate anesthesia. Ann. Thorac. Cardiovasc. Surg., 1998, 4, p. 12–17
22. Pandharipande, P., Cotton, B. A., Shintani, S. et al. Prevalence and risk factors for development of delirium in a surgical and trauma intensive care unit patients. J. Trauma, 2008, 65, p. 34–41.
23. McPherson, J. A., Wagner, C. E., Boehm, L. M. et al. Delirium in the cardiovascular ICU: exploring modifiable risk factors. Crit. Care Med., 2013, 41, 2, p. 405–413.
24. Hudetz, J. A., Igbal, Z., Gandhi, S. D. et al. Postoperative delirium and short-term cognitive dysfunction occur more frequently in patients undergoing valve surgery with or without coronary artery bypass graft surgery compared with coronary artery bypass graft surgery alone: results of a pilot study. J. Cardiothorac. Vasc. Anesth., 2011, 25, 5, p. 811–816.
Labels
Anaesthesiology, Resuscitation and Inten Intensive Care Medicine
Article was published inAnaesthesiology and Intensive Care Medicine

2015 Issue 6-
All articles in this issue
- Can we decrease incidence of postoperative delirium in children by changing premedication?
- Fast differential diagnostics of acute respiratory insufficiency using ultrasound
- Effect of implementation of a new preventive measure bundle on the incidence of ventilator associated pneumonia
- Echocardiographic evaluation of the aortic valve in the unstable patient – basic considerations
- Calculation of cerebral perfusion pressure in the management of traumatic brain injury: joint position statement by the councils of the Neuroanaesthesia and Critical Care Society of Great Britain and Ireland (NACCS) and the Society of British Neurological Surgeons (SBNS)
- Influence of prophylactic melatonin administration on the incidence of early postoperative delirium in cardiac surgery patients
- Anaesthesiology and Intensive Care Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Echocardiographic evaluation of the aortic valve in the unstable patient – basic considerations
- Fast differential diagnostics of acute respiratory insufficiency using ultrasound
- Can we decrease incidence of postoperative delirium in children by changing premedication?
- Effect of implementation of a new preventive measure bundle on the incidence of ventilator associated pneumonia
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

