-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
Reklama3D High Resolution Anorectal Manometry in functional anorectal evaluation
3D High Resolution anorektální manometrie ve funkčním hodnocení anorekta
Úvod:
Anorektální manometrie představuje diagnostickou modalitu vyhodnocující funkční parametry i koordinaci anorektální aktivity. V posledním desetiletí došlo k vývoji 3D High Resolution (HR) manometrie a jejímu rozšíření ve výzkumných i klinických podmínkách. Byl proveden průzkum literatury (v databázích PubMed a MEDLINE) zaměřen na studie zabývající se problematikou trojrozměrné HR manometrie. Cílem práce je nabídnout přehled současného postavení tohoto vyšetření v koloproktologii se zaměřením na indikace, protokol vyšetření a použitelnost jednotlivých parametrů v klinické praxi. Výsledky: Vývoj pevných katetrů s miniaturizovanými polovodičovými měřícími senzory umožnil velmi přesné měření s vysokým rozlišením a tvorbu 3D tlakových modelů anorekta. Ve srovnání s vodně – perfuzními manometrickými systémy poskytuje přesnější a detailnější data využitelná v posuzování funkčních poruch anorekta. Indikací k provedení anorektální manometrie jsou symptomy anální inkontinence a chronické obstipace. Další využití nachází tato modalita při biofeedback terapii, funkční anorektální bolesti a zhodnocení pacientů podstupujících nízkou resekci rekta s obnovením kontinuity GIT. Protokol vyšetření by měl obsahovat měření klidových anorektálních tlaků, manévr sevření řitního svěrače (squeeze), manévr vypuzení stolice (bear down), reflex zakašlání, vyšetření rektoanálního inhibičního reflexu, rektální senzitivity a compliance. Vyhodnocená data jsou následně základem pro stanovení léčby „na míru“ u pacienta trpícího funkční poruchou anorekta. Závěr: Anorektální 3D HR manometrie je cenným vyšetřením, které nabízí novou dimenzi v chápání funkčnosti anorekta a může odhalit nové patofyziologické mechanizmy. Klíčové slova: anorektální manometrie – poruchy pánevního dna – indikace – využití – vyšetřovací modality
Authors: P. Ihnát 1,2; P. Vávra 1,2; P. Guňková 1,2; A. Pelikán 1,2; P. Zonca 1,2
Authors place of work: Department of Surgical Studies, Faculty of Medicine, University of Ostrava, head of department: doc. MUDr. P. Zonča, Ph. D., FRCS 1; Clinic of Surgery of the University Hospital Ostrava, head of department: doc. MUDr. P. Zonča, Ph. D., FRCS 2
Published in the journal: Rozhl. Chir., 2014, roč. 93, č. 11, s. 524-529.
Category: Souhrnné sdělení
Summary
Introduction:
Anorectal manometry is a diagnostic tool designed for the evaluation of functional parameters and assessment of anorectal activity coordination. In the last decade, the development of 3D high-resolution (HR) manometry and its expansion in experimental and clinical settings has been evident. Literature search (in the MEDLINE and PubMed databases) focusing on studies about 3-dimensional HR manometry was performed. The aim of this paper is to offer an overview of the current state of the art of manometry while concentrating on indications, protocol of the procedure and applicability of this examination in clinical practice. Results: Development of solid catheters with miniaturized semiconductor sensors has enabled very precise measurement (high resolution) and creation of anorectal 3D pressure models. In comparison with water-perfused manometry systems, this method offers more accurate and more detailed data that can be employed in functional disorders assessment. The indications for anorectal manomery are symptoms of faecal incontinence and functional constipation. This modality can also be used in biofeedback therapy, in functional anorectal pain and when assessing patients undergoing continent rectal resection. The HR manometry protocol should comprise the measurement of anorectal resting pressures, the squeeze manoeuvre, the bear down manoeuvre, the cough reflex test, the rectoanal inhibitory reflex examination, rectal sensitivity testing and rectal compliance measurement. Processed data are fundamental in determining an individually tailored treatment plan for patients suffering from anorectal functional disorders. Conclusion: Anorectal 3D HR manometry presents a valuable diagnostic modality offering a new dimension in anorectal function understanding and can reveal new pathophysiologic mechanisms of anorectal functional disorders. Key words: anorectal manometry – pelvic floor disorders – indications – employment – diagnostic modalitiesINTRODUCTION
In developed countries, functional anorectal disorders currently affect 10-25% of the population [1−3]. Clinical manifestations of functional anorectal disorders are anal incontinence or functional constipation (with slow transit colon or obstructed defecation syndrome as the underlying condition). With regard to their incidence and significant impact on the quality of life, anorectal disorders represent a serious medical problem [1,2].
Detailed evaluation of anorectal structure and function is essential for gaining information on the pathophysiology of the functional disorder, for establishing a proper diagnosis as well as for the selection of an adequate treatment modality. While a wide range of functional assessments of the anorectum is currently available, only a limited number of these examinations is routinely used in clinical practice – anorectal endosonography, manometry, defecography, colonic transit time, electromyography and pudendal nerve terminal motor latency testing [4,5].
Anorectal manometry represents a widely accepted diagnostic modality evaluating functional parameters as well as anorectal activity coordination [5]. The technological developments in the last decade have enabled the development of high-resolution (HR) anorectal manometry as well as its employment in both research and clinical settings [6,7]. The most modern type of HR manometry currently available is the possibility of performing three-dimensional (3D) HR manometry [7].
The authors would therefore like to shed some light on two issues: What is the current position of 3D high-resolution manometry in coloproctology? And, from the perspective of evidence-based medicine, what are the indications, the procedure of the examination and the usability of the outputs in therapeutic management of patients with a functional anorectal disorder?
Anorectal manometry
Anorectal manometry is a functional assessment of the anorectum perfomed to objectively evaluate the strength and function of the anal sphincters, rectal sensitivity and anorectal reflexes in response to distension of the rectal ampulla [8].
The basic indications for performing anorectal manometry in coloproctology patients can be divided into four groups [4]:
- faecal incontinence
- chronic constipation
- evaluation of anorectal function prior to and after therapeutic intervention (e.g. following biofeedback therapy)
- miscellaneous (functional anorectal pain, assessment before/after resection of the rectum with pouch construction or low colorectal/coloanal anastomosis)
The above indications are substantiated by the necessity to assess anorectal function (voluntary and reflex functions, rectal sensitivity) which is the basis for selecting individually tailored treatment for each patient.
Technical equipment and the principle of 3D HR manometry
The technology and the principle of manometric measurement depend on the equipment available. The development began with balloon manometry subsequently replaced by perfusion systems (single-channel or multi-channel) and continued with the introduction of solid-state catheters with semiconductor pressure sensors [8,9]. In clinical practice, not only technologically different systems of manometry, but also different measurement techniques (stationary or continuous pull through) are still used nowadays [2]. In the last decade, however, an expansion and domination of solid-state catheters with miniaturized semiconductor measurement sensors (the surface of the catheters is fitted with hundreds of sensors) can be observed; these catheters enable very accurate measurement with high resolution based on an increased number of sensors and reduced distance between individual sensors. Thus, HR manometry offers higher physiological resolution while minimising movement artifacts [7,9].
HR manometry in combination with sophisticated software makes it possible to convert the manometric values to high-detailed contour plots (spatiotemporal diagrams visualising isobaric values with the same spectral colour). Thanks to the high number of measured values from circumferentially placed sensors, 3D pressure models of the organ being diagnosed can be obtained [6,9].
The first apparatus in the Czech Republic (according to the official distributor’s information) enabling anorectal 3D HR manometric assessment is available at the Department of Surgery in University Hospital Ostrava. The ManoscanTM 3D workstation (Given Imaging, Los Angeles, CA) (Fig. 1) allows for three-dimensional physiologic mapping of anal sphincters with the possibility of functional assessment and visualisation of symmetry by means of a single introduction of the probe.
Fig. 1. The Manoscan<sup>TM</sup> 3D workstation (Given Imaging, Los Angeles, CA) 
Manoscan anorectal 3D catheter (Fig. 2) is a rigid HR probe with a centrally located lumen which enables inflation of a balloon at the end of the probe (necessary for the measurement of rectal sensitivity and anorectal reflexes) [10]. The measurement part of the probe has a diameter of 10 mm and is 64 mm long. It contains 256 pressure sensors arranged circumferentially in 16 rows of 16 sensors each. Each sensor measures pressure from an area 4 mm long and 2.1 mm wide. The manometric data are analysed and displayed visually (real-time) as 3D pressure models of the anorectum using the ManoViewTM (Given Imaging) software. The 3D image provides a new dimension not only in terms of imaging, but also as regards understanding of the function and potential pathophysiology of anorectal functional disorders.
Fig. 2. Manoscan anorectal 3D catheter 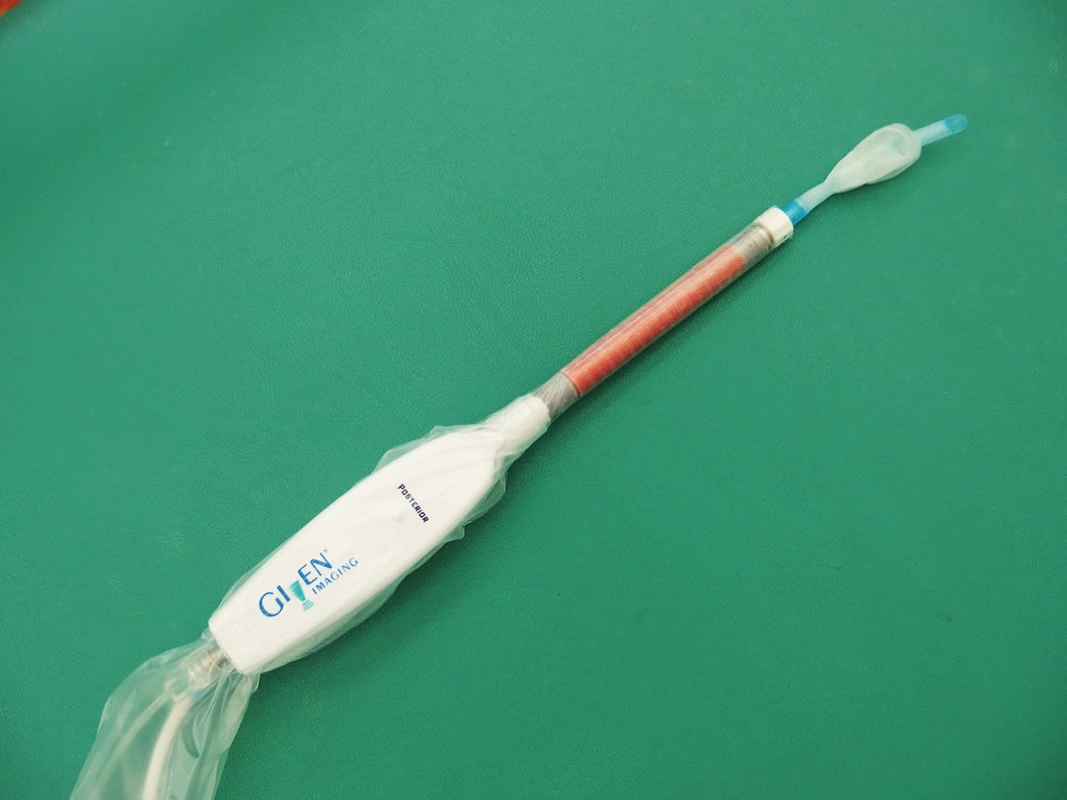
Protocol of the examination and samples of 3D HR imaging
Proper and detailed instruction of the patient as regards the course of the manometric assessment is very important not only for increased patient comfort, but also for a positive effect on the results obtained. In his study, Heinrich showed that enhanced instruction and motivation of the patient during the examination improves the manometric findings, changing them from “pathologic” to “normal” values in 31−45% of patients [11].
Although no special preparation of the patient is required prior to manometry, many authors recommend irrigation of the rectal ampulla 2 hours before the procedure using Yal or a small enema. It is advisable to perform manometry in a calm environment with the patient lying in the left lateral position with knees and hips bent [4,8]. After inserting the Manoscan anorectal 3D catheter, pressures are recorded according to the following protocol:
Anorectal resting pressures
After anorectal probe placement it is recommended to wait for approximately 5 minutes to give the patient sufficient time to relax. Following this run-in period, anorectal resting pressures are measured over 30 seconds. The software evaluates the resting pressures, specifies the functional length of the anal canal and creates two - and three-dimensional pressure models. Figure 3 shows an example image of a healthy individual’s pressure morphology comprising a “pressure circle” (Fig. 3a), a 3D image (Fig. 3b) and a 2D image (Fig. 3c). The pressure circle (Fig. 3a) schematically outlines the circumferential distribution of pressures in the given axial localization (the external yellow circle representing a pressure of 0 mm Hg, the internal yellow circle a pressure of 200 mm Hg). 3D mapping of resting pressures (Fig. 3b) typically has the form of a cylinder that may be rotated on the monitor so that the morphology of the anorectum can be viewed from all sides [7].
Fig. 3. Anorectal resting pressure morphology 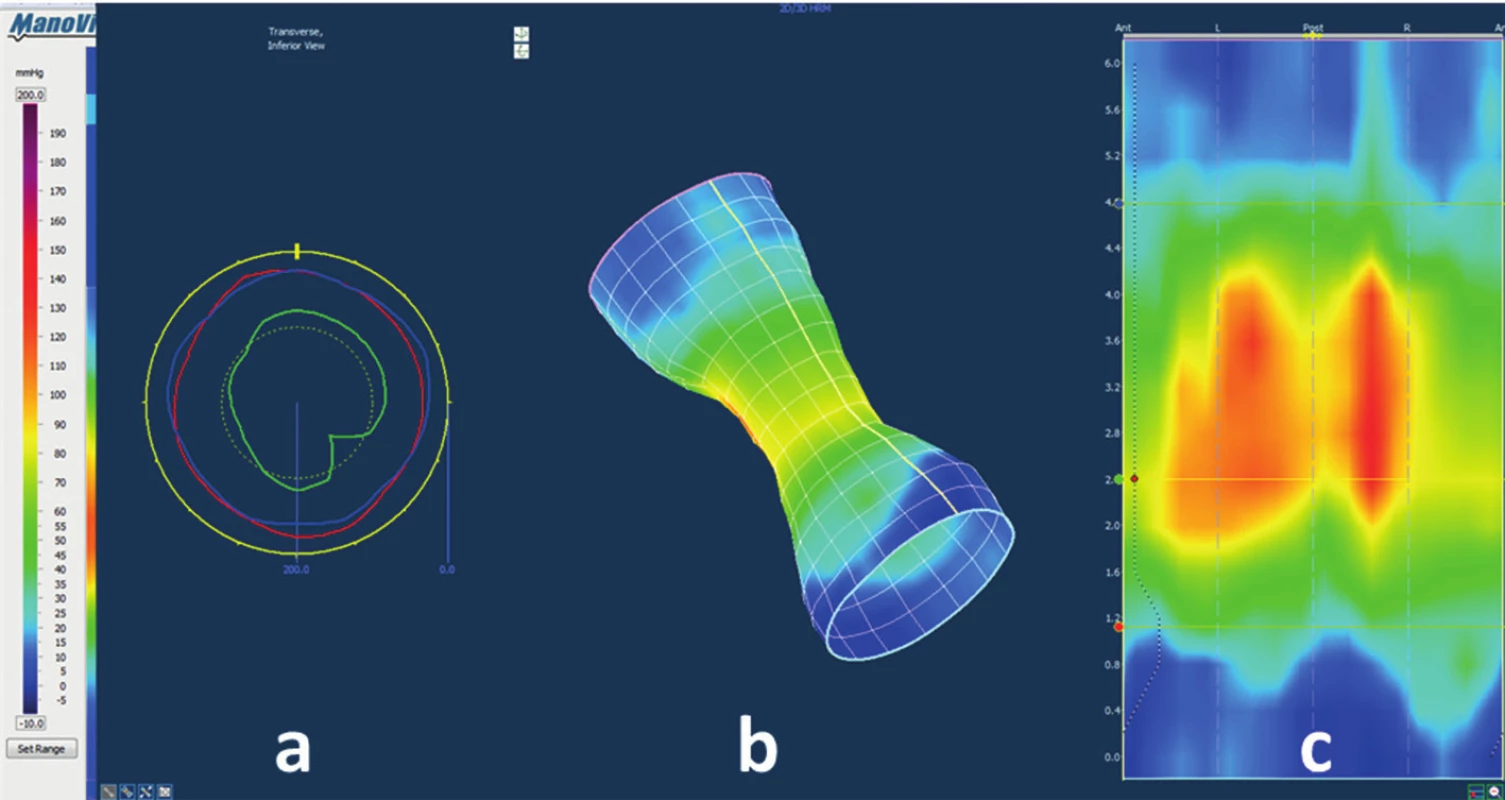
In healthy individuals, intrarectal resting pressure usually ranges between 10 and 15 mm Hg, resting anal pressure between 56 and 88 mm Hg. It has been observed that higher age and female gender are associated with lower resting anal pressures [6−8,12]. Resting pressure in the anal canal is largely a function of the internal anal sphincter that is responsible for 55−80% of the resting tone [5,13]. Symptoms of passive faecal incontinence correlate with low resting anal tone which is usually due to internal anal sphincter weakness, or degeneration [5]. 3D models of anorectal resting pressures make it possible to visualize and localize a potential defect in the structure of the internal sphincter.
Functional anal canal length is defined as the area over which the resting anal pressures exceed the resting intrarectal pressure by at least 5 mm Hg. In healthy individuals, the functional length of the anal canal is 3.6−4.2 cm [8,12]. A greater age, decreased anal canal resting pressure values and the alteration of rectal sensation increase the risk for anal incontinence [14].
The squeeze manoeuvre
The squeeze manoeuvre assesses pressure while the patient selectively and intensely squeezes the anal muscles. The patient is instructed to squeeze the anal sphincter as strongly as they can and to maintain the squeeze for as long as possible, for a maximum of 30 seconds. The manoeuvre is repeated a total of 3 times, with a rest interval lasting 1 minute. During the squeeze manoeuvre, the patient’s voluntary ability to control the striated muscles of the anorectum is measured.
The typical image of the squeeze manoeuvre during 3D HR manometry can be seen in Fig. 4. The yellow ring representing resting anal pressure (as displayed in Fig. 3b) changes into a high-pressure red ring (Fig. 4) which has a characteristic shape of a sandglass. High pressures (the red ring in the middle) decrease both in the proximal and distal direction via lower (yellow) pressures to zero (blue) pressures.
Fig. 4. Anorectal pressure morphology during the squeeze manoeuvre 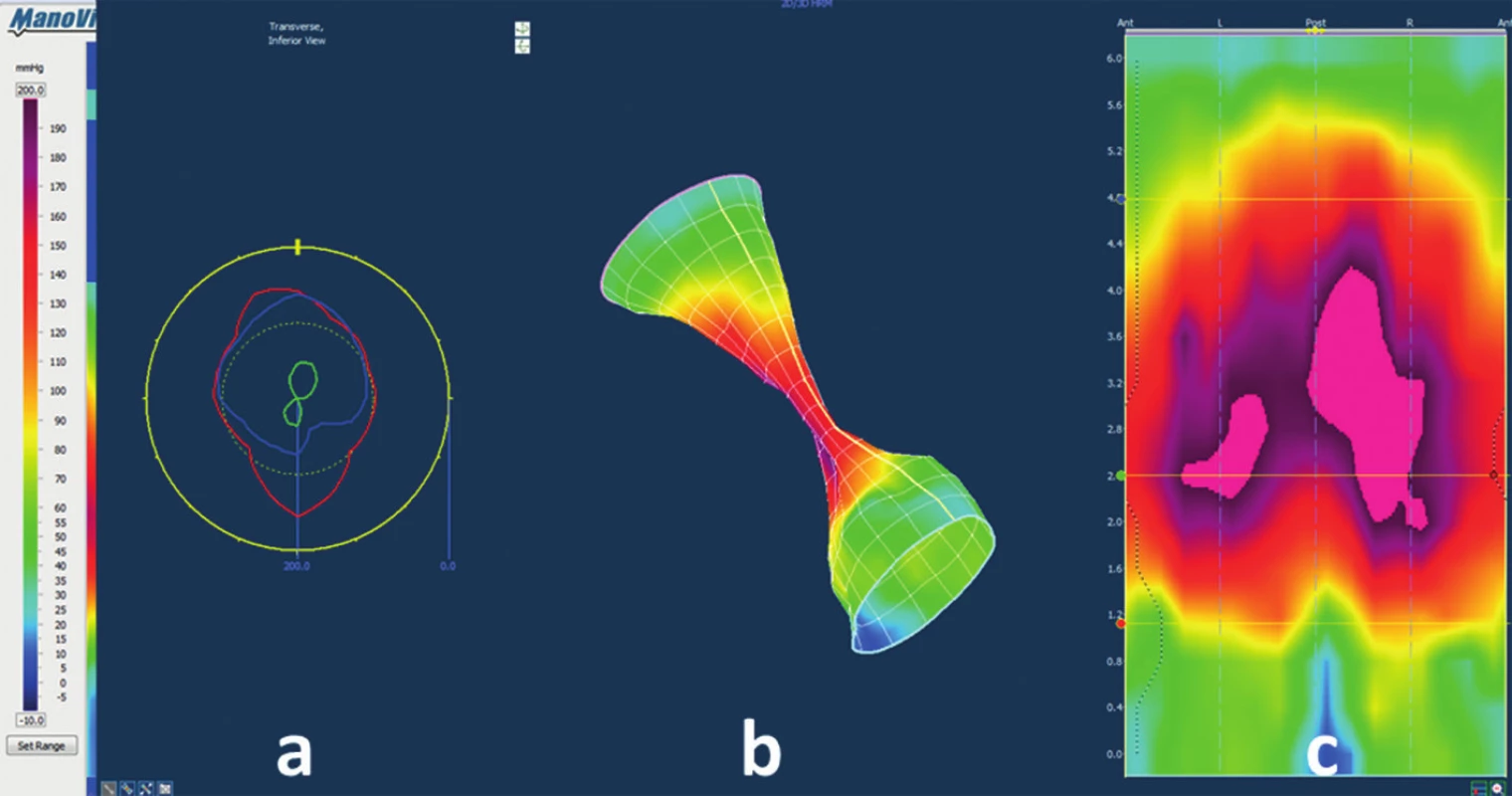
The maximum squeeze pressure is reported to range from 167 to 199 mm Hg in female patients, and from 194 to 247 mm Hg in males. Duration of contraction is defined as the time interval in which pressure greater than or equal to 50% of the maximum squeeze pressure was maintained. Duration of the squeeze manoeuvre in healthy individuals usually ranges from 13 to 29 seconds [7,8,12]. Symptoms of urge or stress faecal incontinence often correlate with low anal squeeze pressures that are due to external sphincter weakness caused for instance by an injury. The authors regard the possibility to identify the site of the defect in pressure mapping during the squeeze manoeuvre, and thus to localize the site of injury (defect) to the external sphincter, as the most important practical application of 3D HR manometry. 3D HRM, therefore, constitutes a valuable examination modality alternative to anorectal endosonography, which, unlike sonography (information on structural muscle defect) principally provides information on the actual functional pressure defect.
In their physiological study, Liu et al. proved that the squeeze manoeuvre is contributed to not only by the contraction of the external anal sphincter, but also by contraction of the puborectalis muscle (the external sphincter is responsible for contraction in the distal part and the puborectalis muscle for contraction in the proximal part of the anal canal) [13]. The proven contribution of the puborectalis muscle to anorectal contraction can also provide an explanation regarding why sphincteroplasty (targeted at a damaged external sphincter) fails to have satisfactory results (short-term success rate is 43−89%, long-term success rate with further gradual deterioration) [2]. Liu believes that it is the neglect of surgical repair of the puborectlais muscle that is the reason for the low success rate of sphicteroplasty procedures [13].
Bear down manoeuvre
This manoeuvre measures pressure during attempted defecation, or so-called simulated defecation. The test focuses on the evaluation of functional coordination of the anus and the rectum. The manoeuvre is repeated a total of 3 times, with a rest interval lasting 1 minute. During the bear down manoeuvre we can observe an increase in intrarectal pressures due to the Valsalva manoeuvre, and the drop of pressures in the anal canal. Intrarectal pressures usually range from 34 to 60 mm Hg, whereas anal pressures range between 39 and 70 mm Hg [7,12].
The 3D HR image of the bear down manoeuvre (Fig. 5) shows the change of resting pressures (of cylindrical shape) to trumpet shape as a result of increased intrarectal pressures and reduced anal pressures. The inability to perform the bear-down manoeuvre is perceived as the major pathophysiologic mechanism in patients with functional defecation disorders – so-called anal dyssynergia, anismus or pelvic floor dyssynergia [15,16]. Identification of a pathologic course of the bear down manoeuvre, and its potential topographic localization in the anterior rectal wall (using 3D pressure models), may for example also help differentiate between asymptomatic rectocele and a rectocele involved in the pathophysiology and anorectal symptoms of obstructed defecation syndrome.
Fig. 5. Anorectal pressure morphology during the bear down manoeuvre 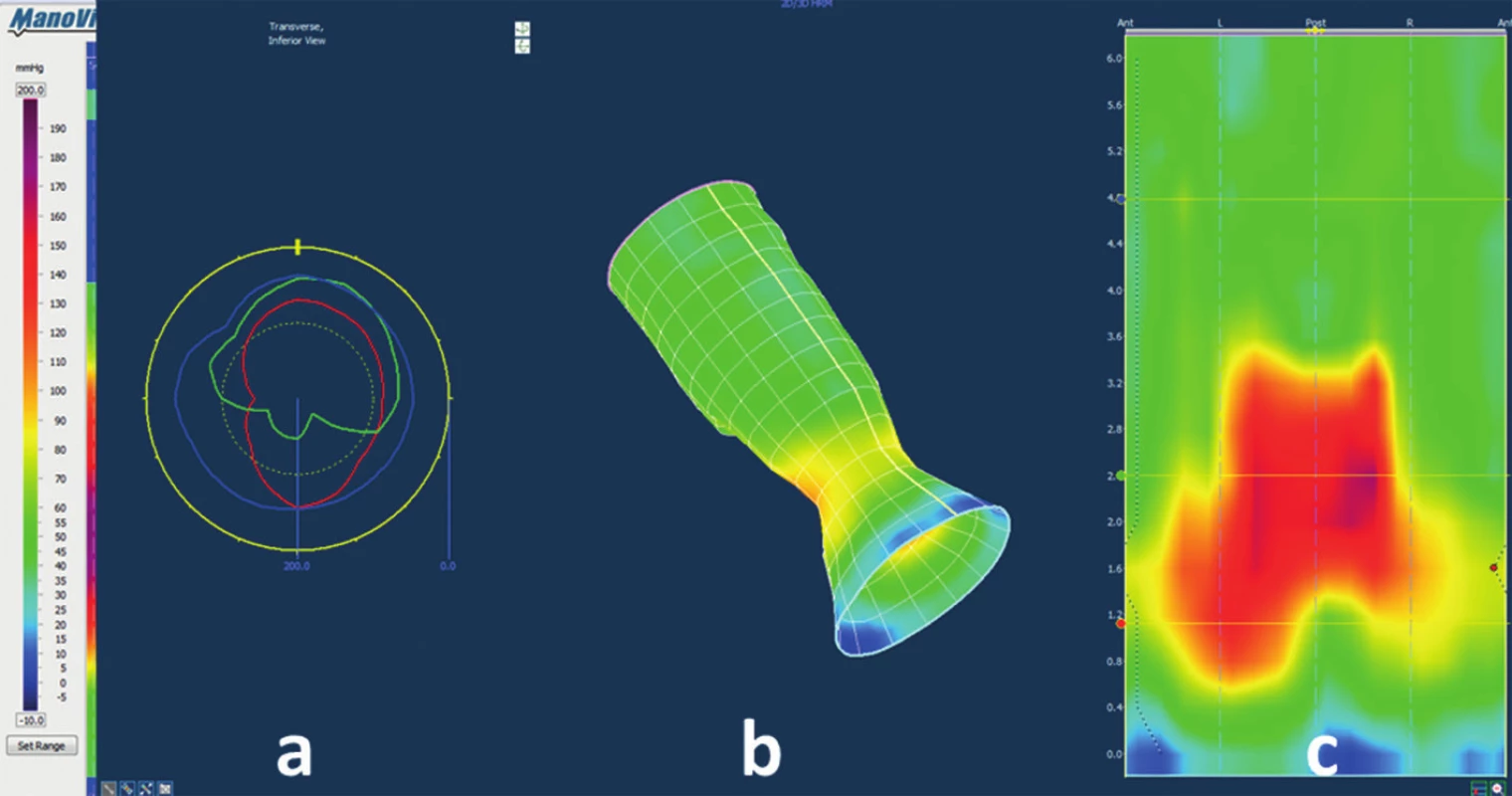
Cough reflex test
The evaluation of anorectal pressures during a voluntary cough enables to verify the presence of the reflex increase in the anal canal pressures during abrupt rise in intraabdominal pressure (which is an important mechanism in maintaining continence).
Absence of the cough reflex, or more precisely its significant attenuation, can be observed in patients with the symptoms of urge and stress anal incontinence.
Rectoanal inhibitory reflex (RAIR)
RAIR is an intramural reflex mediated by the myenteric plexus and modulated via the spinal cord. Internal anal sphincter relaxation occurs in response to distension of the rectum (and an increase in intrarectal pressure) which allows the intestinal contents to come into contact with receptors in the mucosa at the proximal end of the anal canal (to discriminate between formed or liquid stools and gaseous material) [2]. RAIR testing during manometry consists in filling the intrarectal balloon with 50 mL liquid or air (the balloon is attached to the end of the Manoscan anorectal 3D catheter – Fig. 2) and evaluating subsequent anal canal relaxation.
The RAIR is typically absent in patients with Hirschsprung’s disease due to a developmental defect affecting their myenteric plexus (aganglionosis) responsible for the existence of RAIR. An abnormal RAIR response occurs in patients with damaged sacral reflex arc either at the level of the sacral segments of the spinal cord or the pudendal nerves. Such patients usually suffer from urge incontinence and have symptoms of the cauda equina syndrome or pudendal neuropathy [17].
Rectal sensitivity and compliance
Rectal sensitivity testing involves progressive filling of the rectal balloon with an increasing volume of liquid. In the beginning, the balloon is filled with 10mL; subsequently, the volume is increased in increments of 10 mL (at a rate of ca. 10 mL per 3-5 seconds). We are interested in the volume at which the patient can perceive the presence of the inflated balloon – this is referred to as the first sensation. During further gradual inflation we record the volume at which the patient reports the feeling of the desire to defecate, and the volume at which they already report discomfort. It is not recommended to inflate the balloon with more than 250 mL.
In healthy individuals, the first sensation is reported at volumes of 32-44 mL, the desire to defecate at volumes of 77−98 mL, and discomfort at volumes of 140−159 mL [6−8].
Rectal compliance is measured from the data obtained during intermittent intrarectal balloon insufflations. Balloon distension causes an initial increase in the intra balloon (rectal) pressure which is followed by a gradual decline in pressure to a steady state value (as the rectum accommodates to the increased volume). Compliance is then calculated as change in balloon volume divided by change in intra balloon pressure.
Decreased rectal compliance (due to increased rectal wall stiffness) can be observed in patients with idiopathic bowel inflammation, chronic ischaemia or after pelvic radiotherapy. Increased rectal compliance points to an excessively weak rectal wall in patients with megarectum or functional constipation.
CONCLUSION
Anorectal 3D HR manometry is a valuable diagnostic tool offering a new dimension in understanding anorectal function. It allows to reveal the pathophysiologic mechanisms of functional disorders, and provides the basis for correctly selected therapeutic management. Compared to water-perfusion manometric system, 3D HRM provides more accurate and detailed data [9].
The principal indications for performing 3D HR manometry are the symptoms of faecal incontinence and chronic constipation. This modality is also used to assess biofeedback therapy, functional anorectal pain and patients undergoing continent rectal resection.
We can find sufficient evidence in the literature worldwide supporting the application of manometry in clinical practice. Studies investigating the clinical impact of functional assessments (in patients with incontinence or constipation) have shown that the information obtained considerably improved diagnosis and directly influenced or altered the therapeutic management in a significant number of cases [5,18,19].
MUDr. Peter Ihnát, Ph.D., MBA
Chirurgická klinika FN Ostrava,
17. listopadu 1790
708 52 Ostrava
e-mail: peterihnat@yahoo.com
Zdroje
1. Remes-Troche JM, Rao SS. Defecation disorders: neuromuscular aspects and treatemnt. Curr Gastroenterol Rep 2006;8 : 291−299.
2. Herold A. Incontinence. In Herold A, Lehur PA, Matzel KE, O’Connel PR. European manual of medicine: Coloproctology. Springer 2008 : 83−92.
3. Gundling F, Seidl H, Scalercio N, Schmidt T, Schepp W, et al. Influence of gender and age on anorectal function: normal values from anorectal manometry in a large Caucasian population. Digestion 2010;81 : 207−213.
4. Rao SSC, Azpiroz F, Diamant N, Enck P, Tougas G, et al. Minimum standards of anorectal manometry. Neurogastroenterol Mot 2002;14 : 553−559.
5. Scott SM, Gladman MA. Manometric, sensorimotor, and neurophysiologic evaluation of anorectal function. Gastroenterol Clin N Am 2008;37 : 511−538.
6. Noelting J, Ratuapli SK, Bharucha A, Harvey DM, Ravi K, et al. Normal values for high-resolution anrectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am J Gastroenterol 2012;107 : 1530−1536.
7. Li Y, Yang X, Xu C, Zhang Y, Zhang X. Normal values and pressure morphology for three-dimensional high-resolution anorectal manometry of asymptomatic adults: a study in 110 subjects. Int J Colorectal Dis 2013;28 : 1161−1168.
8. Gruppo Lombardo per lo Studio della Motilita Intestinale. Anorectal manometry with water-perfused catheter in healthy adults with no functional bowel disorders. Colorectal Dis 2010;12 : 220−225.
9. Jones MP, Post J, Crowell MD. High-resolution manometry in the evaluation of anorectal disorders: a simultaneous comparison with water-perfused manometry. Am J Gastroenterol 2007;102 : 850−855.
10. Cheeney G, Remes-Troche JM, Attaluri A, Rao SSC. Investigation of anal motor characteristics of the sensorimotor response (SMR) using 3-D anorectal pressure topography. Am J Physiol Gastrointest Liver Physiol 2011;300:G236−240.
11. Heinrich H, Fruehauf H, Sauter M, Steingotter A, Fried M, et al. The effect of standard compared to enhanced instruction and verbal feedback on anorectal manometry measurements. Neurogastroenterol Motil 2013;25 : 230−237.
12. Cross – Adame E, Nguyen M, Valestin J, Meduri K, Rao SS. Evaluation of anorectal function in healthy adults with 3D High Definition Manometry. Gastroenterol 2012;142:Supp AB 2028.
13. Liu J, Guaderrama N, Nager CW, Pretorius D, Master S, et al. Functional correlates of anal canal anatomy: puborectalis muscle and anal canal pressure. Am J Gastroenterol 2006;101 : 1092−1097.
14. Ciriza-de-los-Ríos C, Ruiz-de-León-San-Juan A, Díaz-Rubio-García M, Tomás-Moros E, García-Durán F, et al. Differences in the pressures of canal anal and rectal sensitivity in patients with fecal incontinence, chronic constipation and healthy subjects. Rev Esp Enferm Dig 2010;102 : 683−690.
15. Rao SS. Constipation: evaluation and treatment. Gastroenterol Clin North Am 2003;32 : 659–683.
16. Bharucha AE, Wald A, Enck P, et al. Functional anorectal disorders. Gastroenterology 2006;130 : 1510–1518.
17. Azpiroz F, Enck P, Whitehead WE. Anorectal functional testing: review of collective experience. Am J Gastroenterol 2002;97 : 232–240.
18. Rao SS, Patel RS. How useful are manometric tests of anorectal function in the management of defecation disorders? Am J Gastroenterol 1997;92 : 469–475.
19. Wexner SD, Jorge JM. Colorectal Physiological tests: use or abuse of technology? Eur J Surg 1994;160 : 167−174.
Štítky
Chirurgie všeobecná Ortopedie Urgentní medicína
Článek Komplikace v chirurgii
Článek vyšel v časopiseRozhledy v chirurgii
Nejčtenější tento týden
2014 Číslo 11- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Perorální antivirotika jako vysoce efektivní nástroj prevence hospitalizací kvůli COVID-19 − otázky a odpovědi pro praxi
-
Všechny články tohoto čísla
- Komplikace v chirurgii
- 3D High Resolution anorektální manometrie ve funkčním hodnocení anorekta
- Efekt dekomprese krční míchy při spondylogenní myelopatii na korové funkce mozku
- Vztah antikoagulační a antigregační terapie u nemocných s chronickým subdurálním hematomem k závažnosti předoperačního stavu a výsledku chirurgické léčby
- Pilonidální sinus – diagnóza na pomezí všeobecné a plastické chirurgie
- Cerebral salt wasting syndrom (CSWS) – nezvyklá kazuistika z chirurgického pracoviště
- Karcinóm sigmy v inkarcerovanej slabinovej prietrži
- Audit českých chirurgických pracovišť
- Nový atlas varixov dolných končatín
- Rozhledy v chirurgii
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Cerebral salt wasting syndrom (CSWS) – nezvyklá kazuistika z chirurgického pracoviště
- Pilonidální sinus – diagnóza na pomezí všeobecné a plastické chirurgie
- Karcinóm sigmy v inkarcerovanej slabinovej prietrži
- Komplikace v chirurgii
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



