-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Implementation of a Mental Health Care Package for Children in Areas of Armed Conflict: A Case Study from Burundi, Indonesia, Nepal, Sri Lanka, and Sudan
article has not abstract
Published in the journal: . PLoS Med 10(1): e32767. doi:10.1371/journal.pmed.1001371
Category: Health in Action
doi: https://doi.org/10.1371/journal.pmed.1001371Summary
article has not abstract
Summary Points
-
In the absence of existing mental health services, a newly developed community-based psychosocial and mental health care package for children was implemented and evaluated in five conflict-affected countries: Burundi, Indonesia, Nepal, Sri Lanka, and Sudan.
-
Routine monitoring and evaluation combined with rigorous research design allowed for improvement and fine-tuning of services in real-life settings, and highlighted key gaps in current knowledge.
-
The program has resulted in improved case detection with a developed and validated screening instrument, making care accessible to over 96,000 children, and generating empirical evidence on the effectiveness of interventions.
-
Future development requires broadening the scope of the care package (i.e., integration of treatment for severe mental disorders, stronger involvement of families, and strengthening of primary prevention approaches) and continued evaluation of new elements.
This case study is part of the PLOS Medicine series on Global Mental Health Practice.
Background
A recent review demonstrated that mental health problems are a leading cause of health-related disability in children and adolescents worldwide [1]. Even though children and adolescents constitute around 50% of the population in low - and middle-income countries (LMICs), their mental health needs are generally neglected [2],[3]. This is especially the case in settings where children are surrounded by perpetual violence and poverty [4],[5]. Violence may impact mental health and broader aspects of psychological and social well-being [4],[6]. This situation requires an intervention response that is comprehensive, as well as affordable, effective, and feasible to scale up.
Recent reviews have demonstrated that the evidence base for effective mental health interventions for children in LMICs, and specifically for children in areas of armed conflict, is slowly accruing [3],[7],[8]. Moreover, international guidelines have been developed to support establishment of services in LMICs [9],[10]. One core question is how to translate existing knowledge and guidelines into effective practice, and how to translate real-life practice into replicable and sustainable models that can be scaled up in other settings. This question is further complicated in conflict-affected areas and fragile states, because of severely disrupted health and community care structures [11] and the scarcity of effective and feasible service delivery models [7]. These challenges are emphasized by a recent review reporting a large gap between research and practice in humanitarian settings [8]. Globally, research–practice mismatches contribute to the limited availability and impact of child mental health interventions [2],[12]. McLennan and colleagues distinguish four types of research–practice gaps: “(1) the failure to implement interventions found to be effective, and the implementation of interventions (2) that have been demonstrated to cause harm, (3) that have evidence of no effect, and (4) where the effectiveness is unknown because of the lack of rigorous evaluation” [12].
The present case study describes an effort to address these challenges through an integrated intervention and research program. At the start of the program we were faced with a vast disparity between the number of children with psychosocial and mental health problems and the availability of evidence-based interventions in settings of armed conflict. Consequently, we followed a combined research–practice approach that aimed to overcome that disparity. We present a summary of the multi-tiered psychosocial and mental health care package, implemented between 2004 and 2010 in five countries [13]. We synthesize the interplay between research and practice in this program according to a set of principles extracted from guidelines on psychosocial support for children in areas of conflict [5],[14],[15] and emergency settings [9]. We conclude with recommendations to improve future uptake of psychosocial and mental health care. While several articles have been published on separate studies of the program [13],[16]–[21], we have thus far not provided an integrated overview of the overarching lessons learned through research and practice reflections.
Case Study of a Care Package
Development
The Child Thematic Program started in September 2004 in Burundi, Sudan, Sri Lanka, and Indonesia. Nepal was added to the program in July 2006. From the start, the care package was based on a public health model to include prevention, treatment, and rehabilitation interventions. The program was implemented through a number of partner organizations (Church World Services, Indonesia; Shantiham, Sri Lanka; Transcultural Psychosocial Organization, Nepal; HealthNet TPO, Burundi and Sudan).
A group of facilitators received a brief training (15–20 days) for the community-level activities and Classroom-Based Intervention (CBI). Locally available counselors were trained (approximately three months) to deliver mental health interventions to children in need of further indicated care. See Table 1 for information on the context and program in each country.
Tab. 1. Program implementation details for each country. 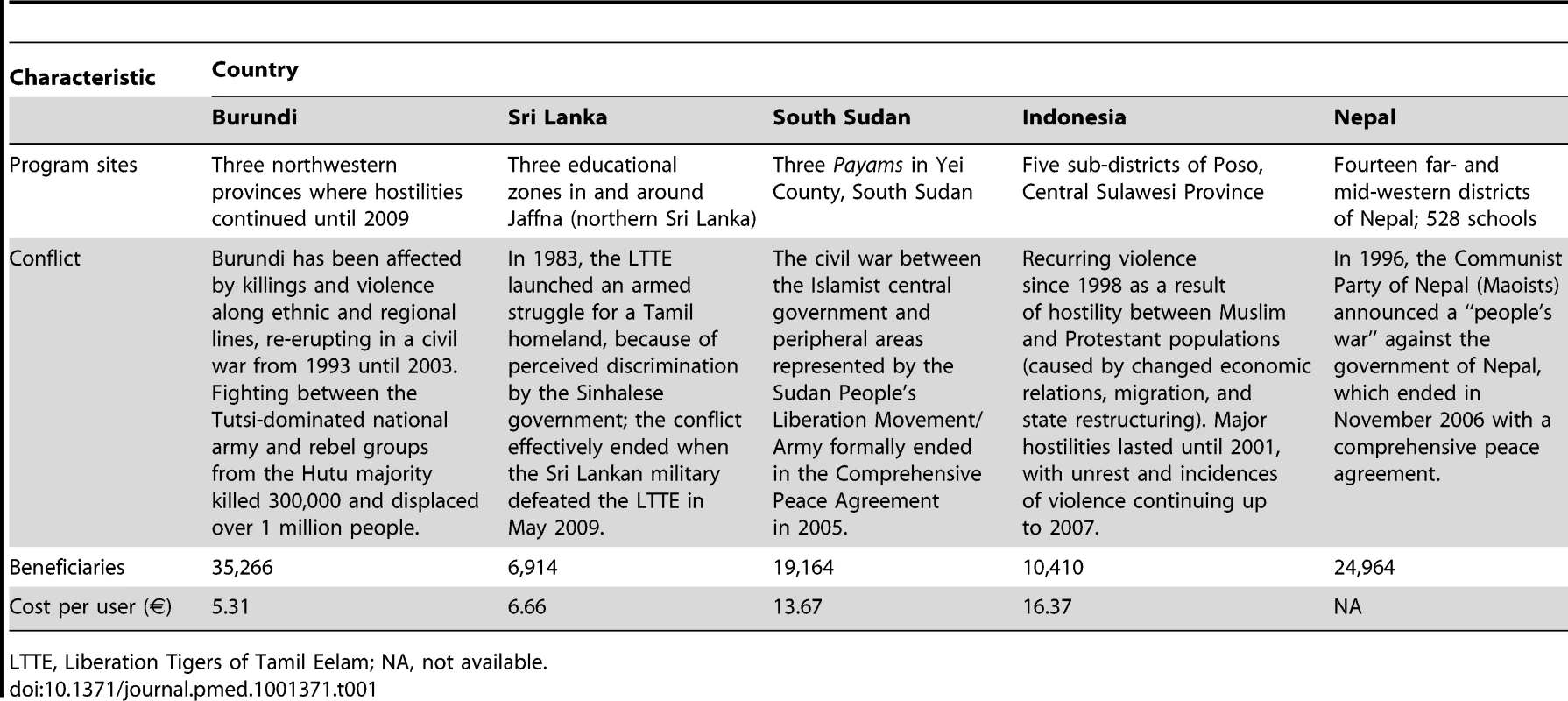
LTTE, Liberation Tigers of Tamil Eelam; NA, not available. Implementation
The multi-tiered care package consisted of a variety of interventions. The first tier comprised mental health promotion activities, aiming to increase adaptive adjustment and community resilience. This tier's activities included running peer groups, which were recreational activities combined with theme-centered group discussions for children without indication for care. Also, it included community sensitization and psycho-education to increase awareness of the mental health needs of children, as well as of existing coping strategies and resources. The second tier consisted of interventions that targeted subgroups of children with elevated psychosocial distress. This tier included a structured group intervention (CBI) aimed at decreasing symptoms of distress and strengthening protective factors. The third tier comprised treatment for children with severe mental health problems. This tier's actions included providing individual counseling to reduce symptoms and improve functioning. Children requiring specialized treatment were referred to a psychiatrist by the counselors, whenever necessary and possible. These interventions are further explained below, and Figure 1 presents the distribution of uptake of these interventions within the program (all sites combined).
Fig. 1. Service uptake of core interventions within the care package. 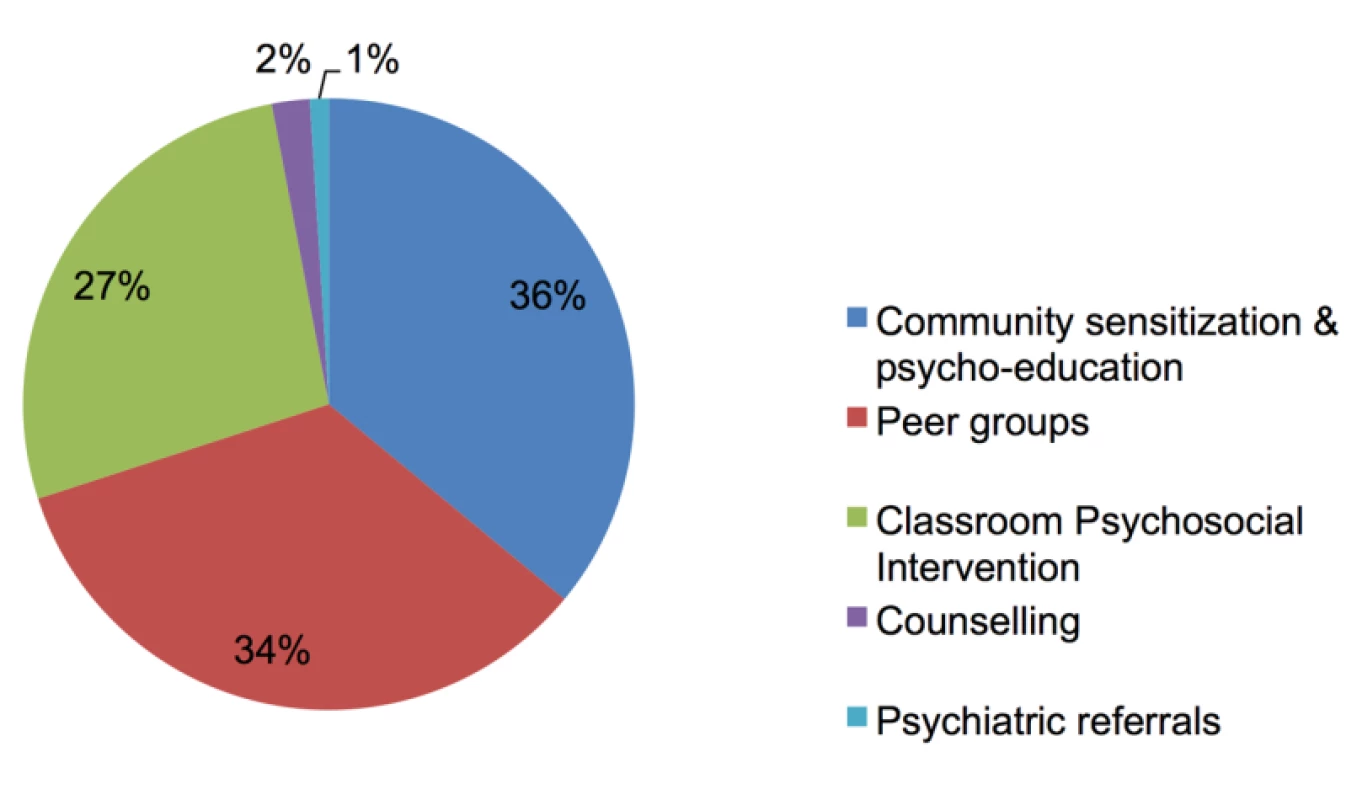
The first step in implementing the care package was to introduce the program to the communities and assess needs through qualitative research [11]. This stage involved receiving approvals from local stakeholders, conducting community awareness and sensitization sessions about the psychosocial and mental health needs of children, enlisting community participation and ownership, and increasing empowerment in dealing with the problems of youth.
In the second step, all children in schools in the program's catchment areas were screened for psychosocial distress using a newly developed instrument (see below) [16],[22]. A prescreening briefing for children and parents was conducted to provide information on the program's objective and process (i.e., availability of different interventions). Furthermore, this briefing aimed to reduce the risk of stigma being associated with the screening.
In the third step, children scoring above a screening cutoff were offered CBI. This standardized intervention consisted of 15 sessions of 1.5 hours over five weeks involving cognitive behavioral techniques (psycho-education, strengthening coping, and guided exposure to past traumatic events through drawing) and creative expressive elements (cooperative games, structured movement, music, drama, and dance) with groups of around 15 children. All other children were offered the opportunity to participate in structured recreational peer group programs (these included sports activities, meditation and yoga, and games), including a psycho-educational element, taking place in the schoolyard. These groups served as an alternative intervention to CBI, to reduce stigma and to strengthen existing resilience by encouraging social support systems and normalization.
In the fourth step, children with sustained and serious mental health problems after termination of CBI were referred to the next tier of the system: problem-solving counseling, either individually or with their families (parental psycho-education sessions). The average number of counseling sessions ranged from 2.2 to 7.5, depending on the country. Throughout the program, biweekly supervision by a psychologist or senior counselor was provided for both the facilitators of CBI and the counselors providing treatment for children with more severe problems.
In the fifth step, children identified by counselors as having psychiatric problems were referred to a mental health specialist (if available), with follow-up and case management by the counselor. To maximize access to care, most interventions were offered within a school setting and implemented by people trained in the communities in which the interventions were implemented. Offering services outside the health sector was intended to minimize levels of stigma, and to increase involvement and mutual collaboration in often fragmented local communities. In this way, access to care was available to 96,718 children and parents.
Impact and Barriers: The Interplay between Practice and Research
Beyond the implementation of services per se, the program aimed to work towards an evidence-based approach to the provision of psychosocial and mental health services. This was achieved by combining practice-based evidence, generated through an elaborate monitoring and evaluation system, with a number of scientific studies embedded within real-life practice. The interaction between research and practice allowed for continuous fine-tuning or adaptation of the care model being implemented. Table 2 summarizes the mutual influence of research and implementation, based on four identified key principles: multileveled care, effectiveness, context sensitivity, and resilience. Table 2 also provides an overview of the main outputs stemming from the program.
Tab. 2. Presentation of practice and research. 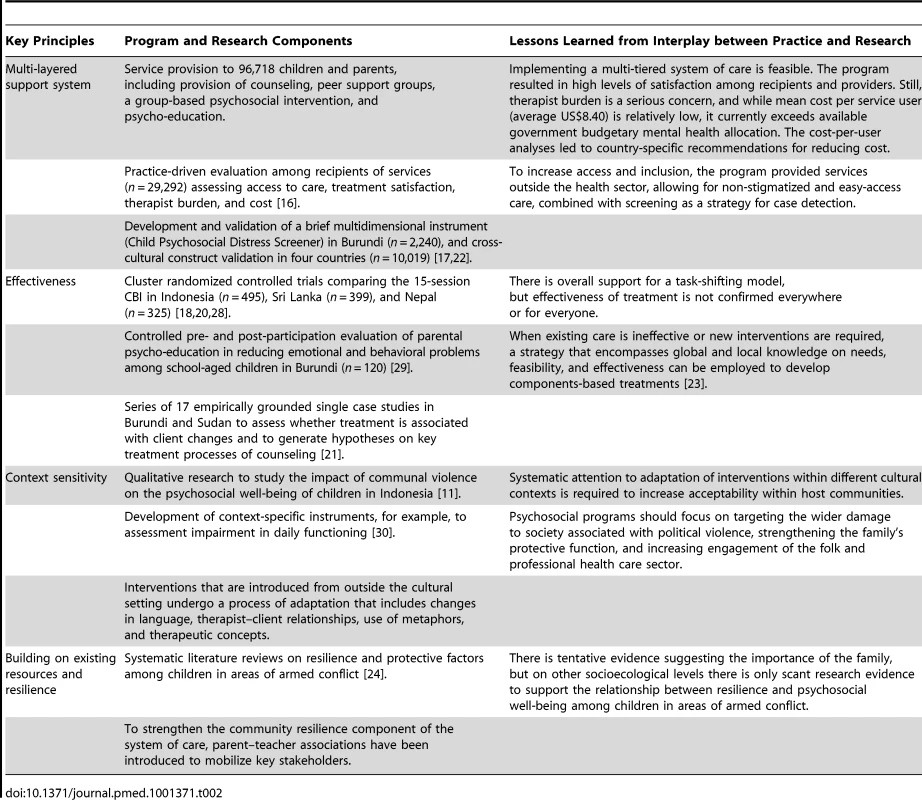
1. Multi-Layered Support
Following the overarching aim to develop a care system, an initial focus on individual components of the package gradually shifted to a focus on measuring the impact and feasibility of the overall package. Feasibility (e.g., client satisfaction and cultural sensitivity) and access to care were assessed through practice-driven evaluations. Results allowed for changes to be made in the delivery framework. For example, the level of stress among facilitators and counselors was found to be too high across the settings, which required a change in assigned roles and increased supervision [16]. Furthermore, expenses related to the development and implementation of services were closely monitored to allow cost analyses.
A key challenge of this care system was ensuring that the different interventions were appropriately matched with the target population, and ensuring the successful flow of clients between the components of the system. To facilitate this process of intervention allocation, an instrument was developed to identify children with elevated psychosocial distress. The Child Psychosocial Distress Screener is a multidimensional tool that combines assessment of children's problems (e.g., distress and school absenteeism) and their protective factors (e.g., coping and social support). To ensure context sensitivity across different settings, we developed a core template of seven items, with content of adjoining probes specified in each setting through qualitative enquiry. We first assessed construct and concurrent validity and other psychometric properties within one setting (Burundi), and then assessed construct validity across the different settings using multi-sample confirmatory factor analyses [17],[22]. The assessment confirmed the reliability and validity of the instrument across settings and indicated an optimal cutoff point for detecting children with an indication for psychosocial care. Consequently, the instrument was integrated into the practice of the care package. As a result of screening outcomes, 59% of children were offered the opportunity to participate in recreational peer group activities, and 41% were offered the opportunity to participate in the more therapeutic group intervention (CBI). From the latter group, 7% were referred for counseling or to other mental health specialists (1%). (Percentages are based only on children that entered the screening process, which explains why these numbers differ from those presented in Figure 1.) Through this triage method, we were able to systematically provide access to support or care services to the entire school-going population in the program catchment areas. The down-side of this approach was that children who were not going to school, often a particularly vulnerable group, were not reached. In a later stage of the program this was adjusted by asking key community members to help in the outreach to this group of children.
2. Effectiveness of Care
Given the limited evidence base for interventions for children in LMICs, an initial priority was to establish the efficacy of the utilized interventions. Cluster randomized trials in Burundi, Indonesia, Sri Lanka, and Nepal evaluated the efficacy of CBI. Evaluated treatment outcomes included changes in symptoms (e.g., post-traumatic stress disorder, depression, anxiety, and aggression), functional impairment, and positive attitudes and behaviors (hope, prosocial behavior, and coping). Whilst CBI showed efficacy in Indonesia, Sri Lanka, and Nepal (with differential effects across populations and outcome measures) [18]–[20], preliminary results in Burundi did not indicate significant lasting change. As a result of the latter findings, we decided to refocus our intervention efforts in Burundi to target children within their family context. To develop the family-based intervention, we used a new strategy that combined global and local knowledge into a context-sensitive modular intervention. The strategy comprised a qualitative phase to determine intervention objectives, a global expert panel to prioritize intervention modalities, a systematic literature review and distillation of evidence-based treatments, and stakeholder meetings to explore sociocultural acceptability of the intervention [23]. The intervention that we developed through this approach is now being implemented and tested in Burundi and South Sudan.
Besides establishing efficacy, we needed more knowledge on how intervention effects may have been sorted, given the differential effects across settings. For the counseling intervention we explored treatment processes through single case studies. In these studies we aimed to systematically associate client changes (measured with quantitative indicators) to treatment processes (qualitative data), in order to identify treatment processes underlying effective counseling. We learned that counselor performance was highly stable (i.e., there were counselors with consistently positive results and counselors with consistently negative results), which reemphasized the importance of our clinical supervision and evaluation mechanisms, for example, for early identification of counselors performing poorly. Furthermore, results showed that the combination of universal treatment variables (therapeutic alliance and trust, and a non-moralistic and non-normative counselor) with specific treatment components (active problem-solving, narrative exposure, and cognitive restructuring) was associated with positive client trajectories [21]. These findings resulted in changes in the training curricula and led to the exploration of a components-based intervention approach.
3. Context Sensitivity
While we used a generic framework across settings, the program was receptive to differences in sociocultural context and care systems. To accommodate these differences, we started the program with qualitative research into how conflict affected children in the different settings, which helped us understand the context and specific needs of the children in the areas where the program was planned [11]. This study established the importance of aspects of community resilience in the different settings. For example, in Burundi, where creating associations is commonly seen as a viable strategy to increase community mobilization, “child-to-child self-help groups” were established as part of the care package.
From practice we learned the importance of adapting psychosocial treatments in new settings. For example, while we had made adaptations in the interventions (including changes in language, therapist–client relationships, use of games and metaphors, and therapeutic concepts), in some settings we were faced with resistance from the community to the group-based intervention (e.g., in Sudan, the group intervention that included hand gestures to show rain and sunshine was perceived as a new religion).
4. Utilization of Existing Resources
The systematic literature review we undertook demonstrated the lack of available evidence for primary-prevention-level mental health interventions for children in complex emergencies [24]. Indeed, one of the most challenging aspects of building a care system was to integrate the package within existing community structures and to make use of existing resources. In the program, peer recreational and support groups were included, as explained above. However, more integration is required for a locally relevant and sustainable primary prevention approach. As a result of this, in light of the results of the literature review, we initiated a new strategy within the overall framework, namely, to work with parent–teacher associations in order to promote the psychosocial well-being of children within the school context. Overall, we feel that a shift in emphasis may be required from epidemiology to understanding health systems, when conducting research in conflict-affected settings.
Looking to the Future
Findings from the different studies presented above have reinforced the notion that a “system of care” approach, however rudimentary, is a necessity not a luxury [25]. We posit that to establish psychosocial and mental health care for children, a care package should be tailored to the context and target population; this can be accomplished by assembling a set of practice components [23],[26]. This approach does not focus narrowly on either a community-based psychosocial intervention (e.g., recreational activities for distressed children) or more specialized psychotherapeutic care (e.g., cognitive behavioral therapy for symptoms of post-traumatic stress disorder); rather, it prioritizes the facilitated transfer of clients between components along a continuum of care, thereby aiming to broadly cover a population at large [2]. Once services are available, non-stigmatizing detection of children in need of care is an integral strategy to improve access. In our case, a two-stage case-identification strategy of school-based detection followed by service-provider-based assessments proved feasible. The accuracy of such a stepped procedure should be evaluated in the future, as it is important in optimizing the match between access to, and provision of, mental health care. To improve upon present limitations to the program, future implementation and research should further include the following: increased emphasis on primary prevention interventions that target resilience at the bottom of the public health pyramid (e.g., integration with other humanitarian initiatives or poverty reduction programs) [8], filling a gap in family approaches [7], increased attention for severe child and adolescent mental disorders (e.g., developmental disorders) through treatment procedures described by the World Health Organization's Mental Health Gap Action Programme [10], and balanced attention to conflict-specific stressors and the burden of daily stressors [27]. Furthermore, future work needs to focus on developing and evaluating strategies to integrate the care package into existing governmental structures to ensure sustainability.
While we promote the current emphasis on accountability and the need to demonstrate the effect of interventions in humanitarian settings, we advocate a broader research agenda that also focuses on care/health system variables, as well as implementation and intervention mechanisms [28].
In the program described here, embedding research in a service delivery framework allowed for generating, and responding to, important implementation issues such as task-shifting, costs of care, burden for caregivers, and how to make interventions culturally compatible.
Zdroje
1. KielingC, Baker-HenninghamH, BelferM, ContiG, ErtemI, et al. (2011) Child and adolescent mental health worldwide: evidence for action. Lancet 378 : 1515–1525.
2. Belfer M, Remschmidt H, Nurcombe B, Okasha A, Sartorius N (2007) A global programme for child and adolescent mental health: a challenge in the new millennium. In: Remschmidt H, Nurcombe B, Belfer M, Sartorius N, Okasha A, editors. The mental health of children and adolescents: an area of global neglect. West Sussex: John Wiley & Sons.
3. PatelV (2008) Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry 49 : 313–334.
4. United Nations Children's Fund (2009) Machel study 10-year strategic review: children and conflict in a changing world. New York: United Nations Children's Fund.
5. BarenbaumJ, RuchkinV, Schwab-StoneM (2004) The psychosocial aspects of children exposed to war: practice and policy initiatives. J Child Psychol Psychiatry 45 : 41–62.
6. AttanayakeV, McKayR, JoffresM, SinghS, BurkleF, et al. (2009) Prevalence of mental disorders among children exposed to war: a systematic review of 7,920 children. Med Confl Surviv 25 : 3–17.
7. JordansMJD, TolWA, KomproeIH, de JongJTVM (2009) Systematic review of evidence and treatment approaches: psychosocial and mental health care for children in war. Child Adolesc Ment Health 14 : 2–14.
8. TolWA, BarbuiC, GalappatttiA, SiloveD, BetancourtTS, et al. (2011) Mental health and psychosocial support in humanitarian settings: linking practice and research. Lancet 378 : 1–11.
9. Inter-Agency Standing Committee (2007) IASC guidelines on mental health and psychosocial support in emergency settings. Geneva: Inter-Agency Standing Committee.
10. World Health Organization (2010) mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Geneva: World Health Organization.
11. TolWA, ReisR, SusantyD, de JongJTVM (2010) Communal violence and child psychosocial wellbeing: qualitative findings from Poso, Indonesia. Transcult Psychiatry 47 : 112–135.
12. McLennanJD, WathenCN, MacMillanHL, LavisJN (2006) Research-practice gaps in child mental health. J Am Acad Child Adolesc Psychiatry 45 : 658–665.
13. JordansMJD, TolWA, KomproeIH, SusantyD, VallipuramA, et al. (2010) Development of a multi-layered psychosocial care system for children in areas of political violence. Int J Ment Health Syst 4 : 1–12.
14. StichickT (2001) The psychosocial impact of armed conflict on children. Rethinking traditional paradigms in research and intervention. Child Adolesc Psychiatr Clin N Am 10 : 797–814.
15. Save the Children (1995) Promoting psychosocial well being among children affected by armed conflict and displacement: principles and approaches. London: Save the Children Federation.
16. JordansMJD, KomproeIH, TolWA, SusantyD, VallipuramA, et al. (2010) Practice-driven evaluation of a multi-layered psychosocial care package for children in areas of armed conflict. Community Ment Health J 47 : 267–277 doi:10.1007/s10597-010-9301-9.
17. JordansMJD, KomproeIH, TolWA, de JongJTVM (2009) Screening for psychosocial distress amongst war affected children: cross-cultural construct validity of the CPDS. J Child Psychol Psychiatry 50 : 514–523.
18. TolWA, KomproeIH, SusantyD, JordansMJD, MacyRD, et al. (2008) School-based mental health intervention for children affected by political violence in Indonesia: a cluster randomized trial. JAMA 300 : 655–662.
19. TolWA, KomproeIH, JordansMJD, VallipuramA, SipsmaH, et al. (2012) Outcomes and moderators of a preventive school-based mental health intervention for children affected by war in Sri Lanka: a cluster randomzed trial. World Psychiatry 11 : 114–122.
20. JordansMJD, KomproeIH, TolWA, KohrtB, LuitelN, et al. (2010) Evaluation of a school based psychosocial intervention in conflict-affected Nepal: a randomized controlled trial. J Child Psychol Psychiatry 51 : 818–826.
21. JordansMJD, KomproeIH, TolWA, SmallegangeE, NtamatumbaP, et al. (2012) Potential treatment mechanisms of counselling for children in Burundi: a series of n = 1 studies. Am J Orthopsychiatry 82 : 338–348.
22. JordansMJD, KomproeIH, VentevogelP, TolWA, de JongJT (2008) Development and validation of the child psychosocial distress screener in Burundi. Am J Orthopsychiatry 78 : 290–299.
23. JordansMJD, KomproeIH, TolWA (2011) Mental health interventions for children in adversity: pilot-testing a research strategy for treatment selection in low-income settings. Soc Sci Med 73 : 456–466.
24. Tol WA, Jordans MJD, Reis R, de Jong JTVM (2009) Ecological resilience: working with child-related psychosocial resources in war-affected communities. In: Brom D, Pat-Horenczyk R, Ford J, editors. Treating traumatized children: risk, resilience, and recovery. London: Routledge.
25. PatelV, ThornicroftG (2009) Packages of care for mental, neurological and substance use disorders in low - and middle-income countries: PLoS Medicine series. PLoS Med 6: e1000160 doi:10.1371/journal.pmed.1000160.
26. ChorpitaBF, DaleidenEL (2009) Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J Consult Clin Psychol 77 : 566–579.
27. MillerKE, KulkarniM, KushnerH (2006) Beyond trauma-focused psychiatric epidemiology: bridging research and practice with war-affected populations. Am J Orthopsychiatry 76 : 409–422.
28. TolWA, KomproeIH, JordansMJD, GrossA, SusantyD, et al. (2010) Mediators and moderators of a psychosocial intervention for children affected by political violence. J Consult Clin Psychol 78 : 818–828.
29. JordansMJD, TolWA, NdayisabaA, KomproeI (2012) A controlled evaluation of a brief parenting psychoeducation intervention in Burundi. Soc Psych Psych Epid In press.
30. TolWA, KomproeIH, JordansMJD, SusantyD, de JongJTVM (2011) Developing a function impairment measure for children affected by political violence: a mixed methods approach in Indonesia. Int J Qual Health Care 23 : 373–383.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 1- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Antikoagulační léčba u pacientů před operačními výkony
-
Všechny články tohoto čísla
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- More Data and Appropriate Statistical Methods Needed to Fully Measure the Displacement Effects of Development Assistance for Health
- Preventing Antiretroviral Treatment Interruptions among HIV/AIDS Patients in Africa
- Translating Coverage Gains into Health Gains for All Women and Children: The Quality Care Opportunity
- Implementation of a Mental Health Care Package for Children in Areas of Armed Conflict: A Case Study from Burundi, Indonesia, Nepal, Sri Lanka, and Sudan
- Toward an Understanding of Disengagement from HIV Treatment and Care in Sub-Saharan Africa: A Qualitative Study
- Tackling Non-Communicable Diseases In Low- and Middle-Income Countries: Is the Evidence from High-Income Countries All We Need?
- Change in the Body Mass Index Distribution for Women: Analysis of Surveys from 37 Low- and Middle-Income Countries
- Getting More Generous with the Truth: Clinical Trial Reporting in 2013 and Beyond
- Reducing Vulnerability to Climate Change in Sub-Saharan Africa: The Need for Better Evidence
- Erectile Dysfunction Severity as a Risk Marker for Cardiovascular Disease Hospitalisation and All-Cause Mortality: A Prospective Cohort Study
- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
- Considerations in Assessing the Evidence and Implications of Aid Displacement from the Health Sector
- Prioritizing Congenital Syphilis Control in South China: A Decision Analytic Model to Inform Policy Implementation
- Balancing Community and Hospital Care: A Case Study of Reforming Mental Health Services in Georgia
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



