-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
MEASUREMENT OF DIMENSIONAL STABILITY OF DENTAL ARCH MODELS PRINTED FROM THERMOPLASTIC MATERIALS WITH THE FUSED DEPOSITION MODELING METHOD DURING THE VACUUMING PROCESS
Authors: Z. Hlavenková 1; J. Milde 2; A. Thurzo 3; S. Dianišková 1
Authors place of work: Department of Orthodontics, Faculty of Medicine, Slovak Medical University in Bratislava, Slovakia 1; Institute of Production Technologies, Faculty of Materials Science and Technology in Trnava, Slovak University of Technology in Bratislava, Trnava, Slovakia 2; Department of Stomatology and Maxillofacial Surgery, Faculty of Medicine, Comenius University Bratislava, and St. Elisabeth's Cancer Institute, Bratislava, Slovakia 3
Published in the journal: Česká stomatologie / Praktické zubní lékařství, ročník 122, 2022, 3, s. 67-78
Category: Původní práce - experimentální studie
doi: https://doi.org/10.51479/cspzl.2022.008Summary
Introduction and aim: In recent decades, the whole field of medicine has been undergoing a digital revolution. This phenomenon is making its way into dental fields as well, including orthodontics, and gradually more and more workflow procedures are being digitalized. The digital models of dental arches can be obtained with the help of an intraoral scanner, and afterwards, using a 3D printer, they can be transformed into physical models. In the field of orthodontics, dental models are needed as study models for diagnostic analysis and determining the therapeutical plan. Dental models at the end of orthodontic therapy are very important as working models for the production of retention devices. The thermoplastic retention plates are very frequently given to patients as retention apparatus and are very popular among them. They are being manufactured at high temperatures in a vacuum machine in a process also known as vacuuming. Conventionally this manufacturing tends to be performed on classic gypsum models. With the growing popularity of digital dental models and their subsequent 3D printing, it is important to know whether dental models made in this way are also suitable for the production of thermoplastic retention plates. Currently, the most widely used method for 3D printing is called Fused Deposition Modeling, using molten plastics as a material for the printing.
The aim of this research was to evaluate 3 thermoplastic materials – ABS, ASA, and Z-Ultrat and to measure their dimensional stability while being exposed to the conditions of vacuuming during the production of the thermoplastic plates. It was important to determine which of them would retain its dimensional stability under given conditions in the best way.
Methods: To obtain the necessary data, we first made intraoral scans of the upper dental arch of two patients using an iTero intraoral scanner. With the use of Zortrax M200 3D printer, these scans were then used to produce physical 3D models. The following parameters were set for the 3D printing: layer thickness – 0.09 mm, density of the infill – 70%, and orientation of the model in the Z axis – 45°. The physical 3D models were then digitized again with GOM ATOS TripleScan extraoral 3D scanner, placed in a vacuum machine, and then scanned again. GOM Inspect software was used to evaluate the dimensional accuracy of manufactured parts. The maximum clinically acceptable deviation between the first 3D scan and the scan of the physical model after vacuuming was determined by the authors to be +/ - 0.50 mm.
Results: Dental models from all 3 examined thermoplastic materials have shown a statistically significant change in their dimensions. However, the magnitude of these deviations is acceptable for clinical practice. All models printed from ABS and Z-Ultrat met the maximum clinically permissible deviation of +/ - 0.50 mm.
Conclusions: Certified material Z-Ultrat, having a chemical composition of PC-ABS, showed the best dimensional
Keywords:
Orthodontics – 3D digitalization – digital dental models – retention – thermoplastic foils – vacuuming – Fused Deposition Modeling – acrylonitrile butadiene styrene – acrylonitrile styrene acrylate – Z-Ultrat
INTRODUCTION AND AIM
Each orthodontic treatment consists of two parts: an active phase and a retention phase. During the active phase, the orthodontic appliances generate a force that acts directly on the teeth. As a result of this prolonged action, the bone around the tooth root slowly remodels, and the teeth move to the new desired position. However, this newly acquired position must be considered potentially unstable. In order to achieve excellent long-term results and ensure the stability of the achieved condition, it is crucial to diminish the orthodontic control of the position of the teeth gradually - it is necessary to keep the teeth in the newly acquired position with the help of retention devices. There are two main groups of retention devices: fixed retainers and removable retainers. Thermoplastic retention plates are a frequently indicated and popular type of removable retainers. They are made of flat transparent foils based on polypropylene. During the vacuum forming process in the vacuum thermoforming machine, they are first heated. Their composition becomes elastic, and afterwards, with the additional vacuum pressure applied by the vacuum machine, they are firmly pressed against the dental model, exactly copying its shape. Thermoplastic retention plates have gained great popularity in recent decades and are currently the most widely used retention apparatus in the upper dental arch [1]. During the conventional method of creating a thermoplastic retention plate, it is necessary to make an alginate impression of the patient's aligned dental arch. This impression is then filled with gypsum, which creates a hard plaster working model. However, nowadays, we can witness the trend of digitalization, and more and more procedures in dental clinics are being digitalized. In addition to photographs, X-ray records, and 3D visualizations of the result of the orthognathic surgery, dental models are the latest diagnostic data used so far mainly in physical form. But they are gradually being replaced by their digital version, and more and more orthodontists, appreciating their benefits, are getting used to working with them. In this new procedure, the aligned dental arch is scanned using an intraoral scanner, obtaining a digital model of the dental arch. It can then be converted to physical form in a short time, thanks to one of the Rapid Prototyping (RP) methods.
RP methods can be defined as "the process of rapidly making a physical model using 3D data, mostly in STL form; 3D scanning is usually at one end, and the 3D printer is at the other end of the chain" [2]. RP technologies can be divided into two basic categories: one consists of material removal to create a physical object and the other one of material addition – this second group is widely known under the name Additive Manufacturing (AM) [3].
The AM method used in this experiment is called Fused Deposition Modeling (FDM). Taking into consideration all the fields, not just dentistry, FDM is the most widely used additive technology, and consists of applying layers of molten semi-liquid plastic [4].
Following the influence of digitalization in orthodontic clinics, the dental arch models are increasingly more frequently being acquired in digital form. Then, the need for transforming the digital model into a physical form arises because the orthodontists need a working model to produce a thermoplastic retention plate.
This more modern way of obtaining orthodontic data and creating a working model, consisting of intraoral scanning and FDM manufacturing technology, is associated with many benefits. First of all, the archiving of patients' data is simplified because dental models printed on a 3D printer by the FDM method weigh much less than gypsum dental models. And thanks to the possibility of data storage in electronic form, the need for physical space for their storage is often eliminated completely. Other advantages are the higher speed of receiving diagnostic data, the possibility of information transfer in digital form, which is practical especially in interdisciplinary cooperation, or the possibility of creating a virtual set-up. Also, during the creation of a thermoplastic plate on a gypsum model, teeth are often broken off while the plate is being removed from the model. These fractures tend to happen especially in the frontal area of the dental arch. Models made of thermopolymers are more flexible than gypsum models and thus remain during this activity undamaged. For many orthodontists, it is more convenient that this production process eliminates the need to mix alginate and then gypsum, which makes the whole process cleaner. Last but not least, this process is more comfortable for patients, as they avoid a not-so-pleasant alginate impression [5–7].
Due to the growing interest in this more modern process – obtaining a dental model in digital form with an intraoral scanner, and its subsequent transformation into physical form by FDM – it is important to find out which materials used in the FDM method are most suitable for this purpose. In this experiment, 3 thermoplastic materials were compared – ABS, ASA, and Z-Ultrat. The main goal of the experiment was to evaluate which of the three investigated materials will retain the best dimensional stability while being exposed to the conditions in a vacuum thermoplastic machine during the production process of thermoplastic retention plates.
The research is part of the attestation work of MDDr. Zuzana Hlavenková, written during a specialization study in the field of Orthodontics, carried out at the Slovak Medical University in Bratislava.
3D MODELS OF UPPER DENTAL ARCHES USED IN THE EXPERIMENT
Digital information that is directly provided by an intraoral scanner is not automatically sufficient in itself to be used for the production of physical models; some additional processing is required before printing. The received 3D scan shows only the outer surface of the dental arch – it is open at the bottom, hollow, has no flat base, and also contains the contours of the surrounding tissues. First, all unnecessary data and artifacts, basically anything that is not part of the dental arch, must be removed. Then a coordinate system is created, and the digital model is inserted into it so that its base sits on the area created by the X and Y axes. The hollow model is then completely filled, and the surface of the model base is aligned and trimmed. For the purposes of this experiment and to ensure the correct placement of the printed models into the GOM ATOS TripleScan 3D scanner, a so-called cube-shaped setting element was created on the models. All these adjustments were made in a software program called MeshMixer [8].
After all these adjustments, the modified 3D digital models were ready for printing, so they were inserted in STL format into the Z-Suite "slicing program", compatible with the Zortrax M200 3D printer, which was used for their printing. Afterwards, the exact printing parameters were defined in it. It has been experimentally proven that digital 3D models, when transformed into physical models by 3D printing, best retain their mechanical properties when the density of their inner filling is set at 70%, the thickness of the outer layer is 0.09 mm, and the angles at which the vertical layers of the infill are touching the outer wall of the model is set to 45 ° – so the parameters in this experiment were set exactly to these values [9].
3 MATERIALS – THERMOPLASTIC POLYMERS
As mentioned above, when all disciplines are taken into account, including the technical ones, Fused Deposition Modeling is the most commonly used additive technology. Molten thermoplastic polymers are used for printing when using FDM. Polymers are long-chain molecules that are formed during the polymerization process when a large number of repeating units – monomers – are being joined together. A polymer chain consisting only of one type of monomer is called a homopolymer. If two or three kinds of monomers are present in the chain, it is then referred to as copolymer or terpolymer [10]. Thermoplastic polymers are amorphous substances, and they contain heterogeneities of various kinds. Therefore, it is not possible to determine a specific melting temperature for them. At low temperatures, they are hard and brittle, referred to as their glassy state. By heating, they melt into their rubbery state, in which their deformability is several orders of magnitude higher. As this deformation is still completely reversible, it is called highly elastic deformation. The temperature range between the glassy and highly elastic state is called the glass-transition temperature Tg. It is one of the basic properties that characterizes every thermopolymer. When the temperature is further increased, the polymer gets into a plastic state; this deformation is already irreversible. The transition between the highly elastic and plastic state is determined by the temperature interval referred to as the flow temperature Tf. After cooling, the thermopolymers solidify again [11].
The physico-chemical properties of thermopolymers are determined by the type of monomers used in them and also by their distribution in the chain. To modify the properties of polymers, various additives can subsequently be added to them, and by that, their stiffness, toughness, weather resistance, dimensional stability, etc., can be influenced. [10].
Thermoplastic materials suitable for the FDM printing method are available on the market from various vendors and come in various price categories. Manufacturers store them wound on a spool in the form of long and thin fibers; hence they are known under the name filaments [8].
Acrylonitrile butadiene styrene (ABS)
Acrylonitrile butadiene styrene is a terpolymer made by polymerization of acrylonitrile, butadiene, and styrene. It is characterized by excellent toughness, good dimensional and geometric stability, good workability, chemical resistance, and low price. Its key properties are as follows: density 0.9 g/cm3 – 1,53 g/cm3, glass-transition temperature ~105 °C. The standard temperature for printing is 230 °C [12].
Acrylonitrile styrene acrylate (ASA)
Acrylonitrile styrene acrylate is a terpolymer in which monomers of acrylonitrile, styrene, and acrylate are combined. It was developed as an alternative to ABS in order to create a material with much higher weather resistance. ASA is characterized by high toughness and stiffness, good chemical resistance and thermal stability, it has high resistance to aging and yellowing, and the material is characterized by high gloss [13].
Z-Ultrat
It is a relatively new and not yet very well-researched thermoplastic material. It is manufactured by Zortrax company and designed for printers of this brand. However, it can also be used on printers from other manufacturers. From a chemical point of view, it is a mixture of polymers in which ABS is in a suitable ratio mixed with polycarbonate (PC). PC is added to the mixture in order to achieve even higher hardness and durability compared to conventional ABS. The manufacturer promises that Z-Ultrat can reliably achieve the properties of plastic objects produced by injection molding technology. The properties of this material include exceptional hardness, resistance to high temperatures, excellent surface quality, and easy postprocessing. Its relative density is 1.18 g/cm³, and the glass-transition temperature is 106.4 °C [14].
The aim of this research was to evaluate 3 thermoplastic materials – ABS, ASA, and Z-Ultrat and to find out their reaction to the conditions to which they will be exposed in a vacuum thermoforming machine. It was important to determine which one of them would retain the best dimensional stability under the given conditions.
MATERIALS AND METHODS
The first step in the experiment was to obtain intraoral scans of the upper dental arch of 2 patients using an iTero intraoral scanner (Align Technology, USA). These two digital models are called CAD models and, in the experiment, were also referred to as nominal models. Using the program GOM ATOS Professional v7.5 SR2, three different cuts were made on both nominal models: Cut 1 indicating the distance between two specific points on the vestibular surface of the second molars, Cut 2 between two specific points on the vestibular surface of the second premolars, and Cut 3 between the two specific points on the vestibular surface of the canines. Afterwards, these models were in STL format exported to the Z-SUITE program, CAM software designed for the Zortrax M200 3D printer (Zortrax, Poland). 3 thermoplastic materials were selected for 3D printing of these CAD models – ABS, ASA (both from the manufacturer Gembird, the Netherlands), and Z-Ultrat with the chemical composition PC-ABS (Zortrax, Poland).
Prior to printing, the parameters for printing physical 3D models were set and used as follows: layer thickness – 0.09 mm, density of the inner filling – 70% and orientation of the model in the Z axis – 45°. Nominal models of both patients were extruded from each thermoplastic material 5 times, creating a total of 30 physical 3D models; these were also referred to as master models. Subsequently, the shape and size of the examined samples were evaluated on an extraoral GOM ATOS II Triple Scan optical 3D scanner (GOM, Germany) with a measuring volume of MV 170 (170 x 130 x 130 mm). These newly acquired digital STL models were also referred to in the experiment as the actual No.1. The same points were applied to these STL models as to the nominal model, thus generating new values for Cut 1, Cut 2, and Cut 3. These new values were actually deviations in the length of cuts between the nominal model and each actual No. 1 and tell us how precisely the printed physical models correspond to the situations in the oral cavity. Both nominal models were printed from each of the 3 materials precisely 5 times so that the average value of these 3 distances could be calculated, and the results were more meaningful (Fig. 1).
All 30 master models were used to create thermoplastic plates on them using Erkoform 3d+ vacuum thermoforming machine (Erkodent, Germany) (Fig. 2). The foils selected for the experiment were from the brand Ercodur and had a thickness of 1 mm (Erkodent, Germany). The examined master models were then again for the second time scanned while using the GOM ATOS II Triple Scan optical 3D scanner. These newly acquired STL models were referred to in the work as actual No. 2 and again points were applied to them in the same places as on the nominal model. Thus, new values were obtained for Cut 1, Cut 2 and Cut 3. Again, the arithmetic mean between the values on all 5 models was calculated. These new values give information about the extent to which vacuuming changed the shape of the printed physical models compared to the condition in the oral cavity.
Fig. 2 Manufacturing of essix plates 
All values obtained during the research were put into two sets of tables. The first set contains all the values of the cuts before vacuuming, namely the distance of the points on the nominal model and the deviation from it on each of the 30 actuals No. 1.
The second set contains all values of point distances on the nominal model and the deviation from it on each of the 30 actuals No. 2. It, therefore, tells us about the change in the dimensions of the master model after vacuuming.
The arithmetic mean of the deviations of the distances between the points was recorded in the graphs.
More attention was paid to comparing the values of Cuts between the nominal model and actual No. 2 (Fig. 3).
Fig. 3 Comparision between Nominal and Actual, the difference of the values of all three cuts 
Statistical processing of the acquired data was performed in the statistical software IBM SPSS 19. A paired t-test was used to compare the values of continuous random variables (in our case, the deviation of the length of the cuts from the nominal) before and after the intervention (vacuuming). As for the differences before and after the intervention, the normal distribution was not rejected. Comparisons were made separately for each patient and each material. We worked at a significance level of α = 0.05. A general linear model for repeated measures was used to monitor changes in deviations of the cuts from nominal after vacuuming. The influence of the patient and the material was taken into account.
RESULTS
Both sets of tables (before and after vacuuming), into which the measurement results were recorded, were compiled according to the same pattern. The first line marked whether it was a print of the dental arch of Patient No. 1 or Patient No. 2, the material from which the model was printed, and whether the measured model has not yet passed or has already undergone a vacuum process. The individual cuts in the Y axis were marked in the rows; they were as follows: Cut 7–7 (simply also referred to as Cut 1), Cut 5–5 (Cut 2), and Cut 3–3 (Cut 3). The first column contains the values of the distances between the points on the nominal model (intraoral scan in the oral cavity), so it is the same in all tables. The next 5 columns show the values of the dimensional change of the Cut in the individual prints with respect to the nominal model, and in the last column, the arithmetic mean of the values of the deviations of all 5 printed models was recorded. The maximum clinically permissible deviation of the dimensional difference between the scan and the model after vacuuming was determined by the authors to be +/ - 0.50 mm.
The measured values were then plotted into graphs. For a better representation of the change, the values for each material both before vacuuming (blue curve) and after vacuuming (red curve) were plotted into one graph. The colored dot is the value of the arithmetic mean of the values and the black line shows the variance of the values of all 5 prints with the incorporation of the standard error of the deviations.
In Tables 1, 3, 5, 7, 9, and 11, the nominal value was compared with the actual No. 1 - these numbers tell us how accurately printed physical models correspond to the situation in the oral cavity (intraoral scan). In Tables 2, 4, 6, 8, 10, and 12, the nominal value was compared with the actual No. 2 – these numbers indicate the extent to which the vacuuming process changed the shape of the printed physical models, meaning how much the physical models that have already undergone the process of vacuuming correspond to situations in the oral cavity (intraoral scan) (Tables 1–12, Graphs 1–6).
Tab. 1. Dimensional deviations of the ABS master model before vacuuming (patient 1) 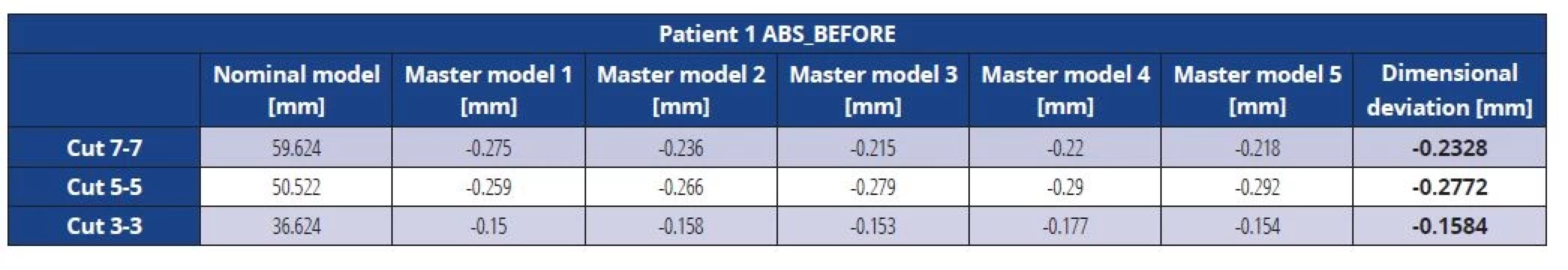
Tab. 2. Dimensional deviations of the ABS master model after vacuuming (patient 1) 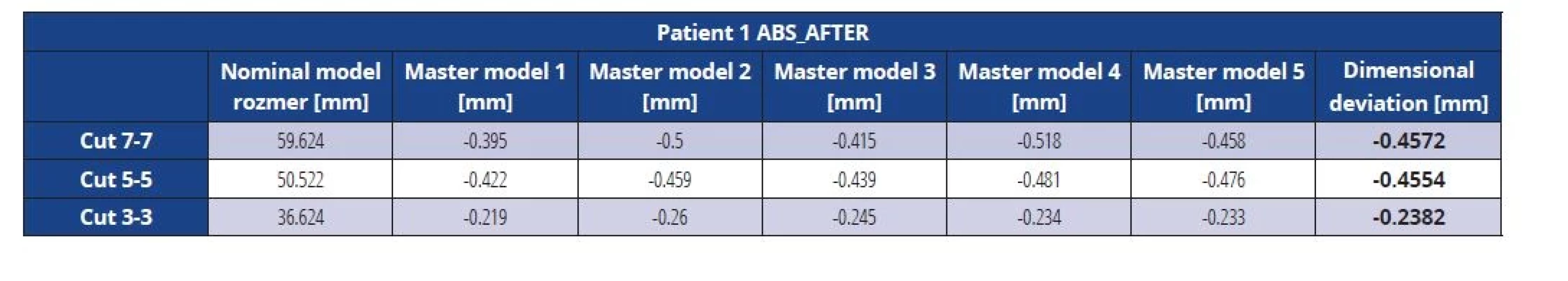
Tab. 3. Dimensional deviations of the ASA master model before vacuuming (patient 1) 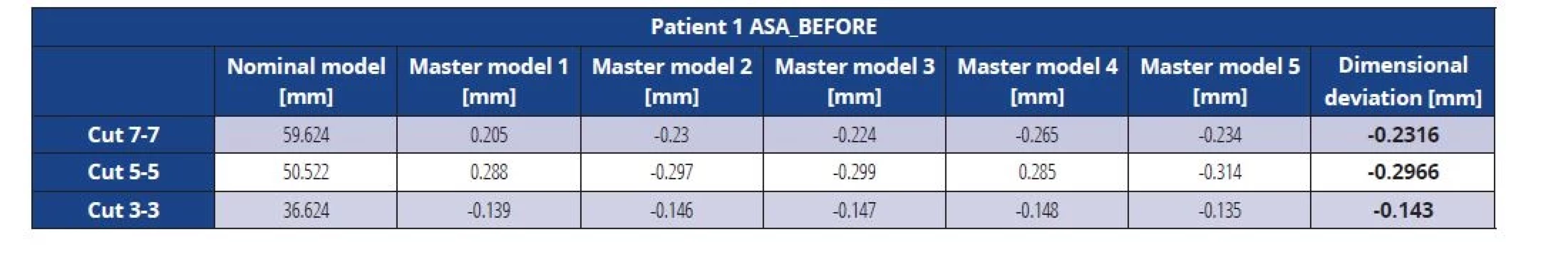
Tab. 4. Dimensional deviations of the ASA master model after vacuuming (patient 1) 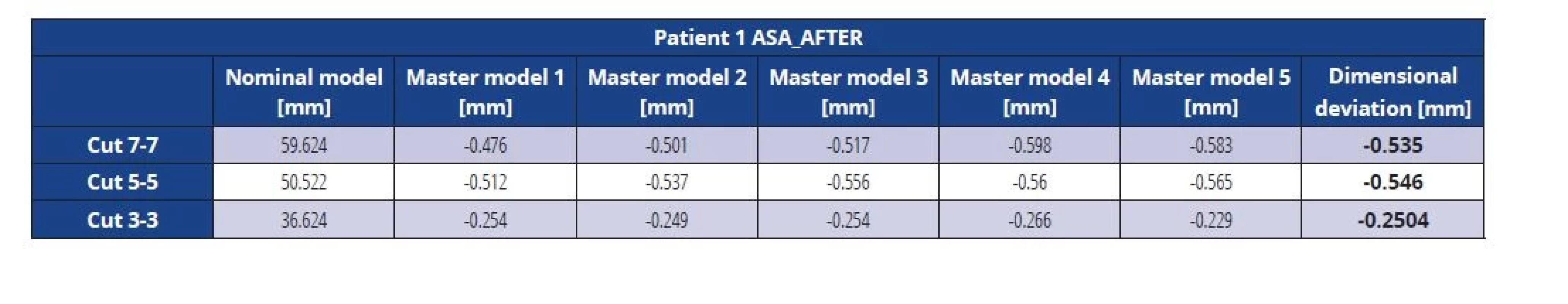
Tab. 5. Dimensional deviations of the Z-Ultrat master model before vacuuming (patient 1) 
Tab. 6. Dimensional deviations of the Z-Ultrat master model after vacuuming (patient 1) 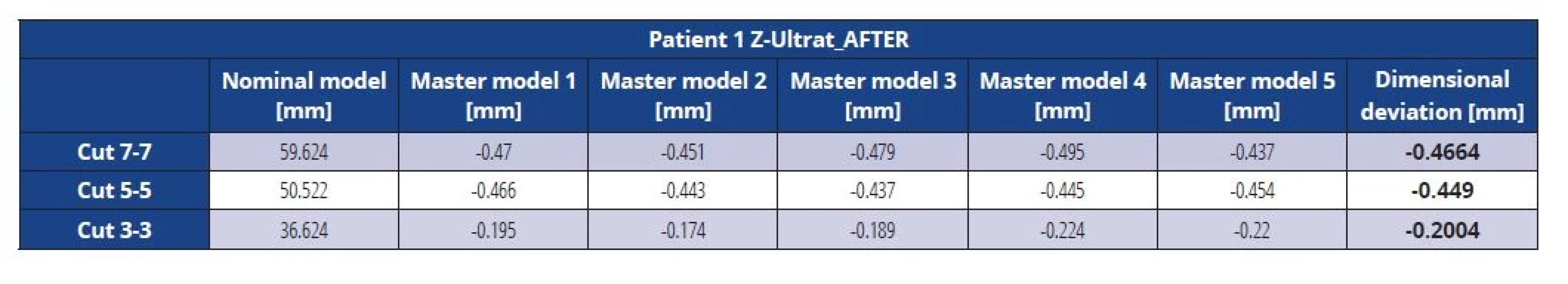
Tab. 7. Dimensional deviations of the ABS master model before vacuuming (patient 2) 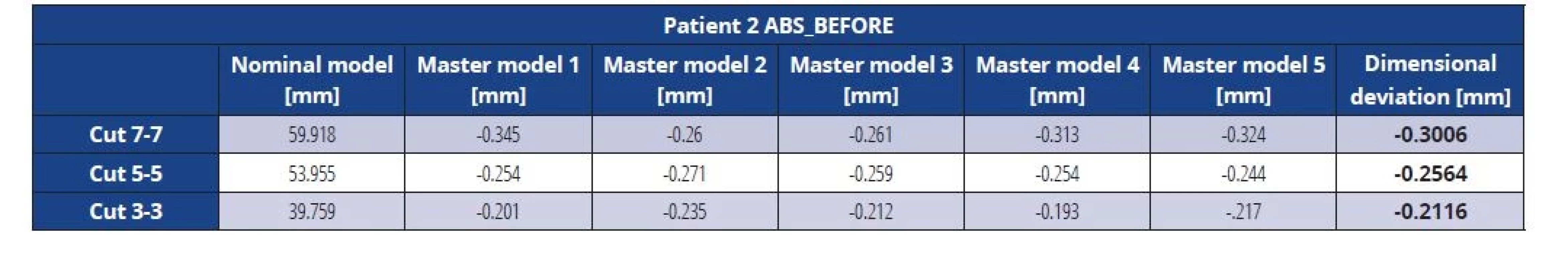
Tab. 8. Dimensional deviations of the ABS master model after vacuuming (patient 2) 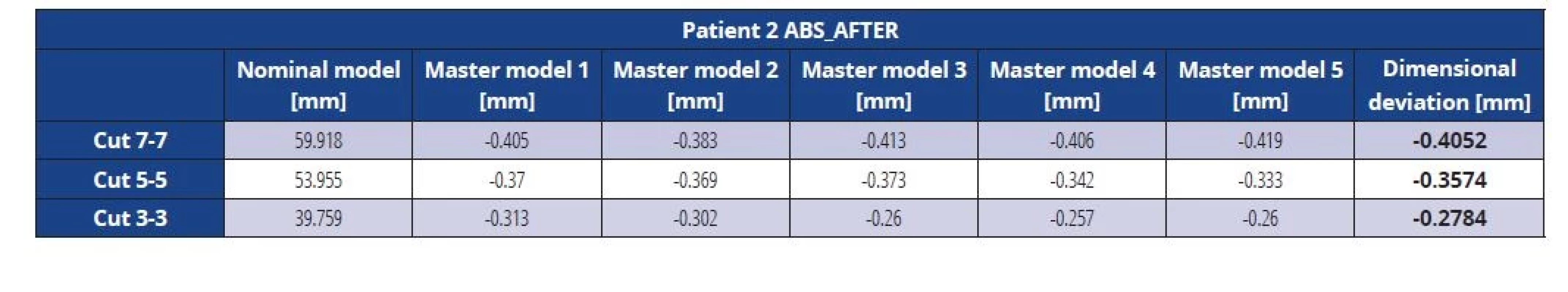
Tab. 9. Dimensional deviations of the ASA master model before vacuuming (patient 2) 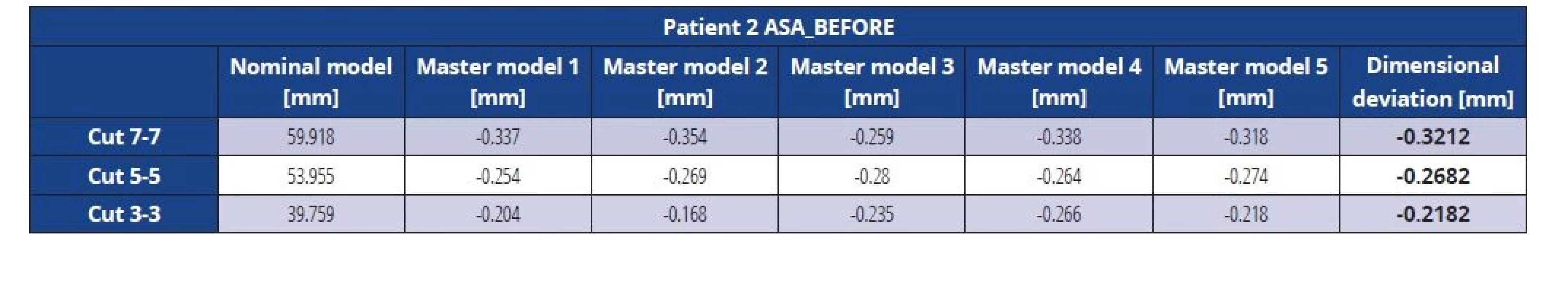
Tab. 10. Dimensional deviations of the ASA master model after vacuuming (patient 2) 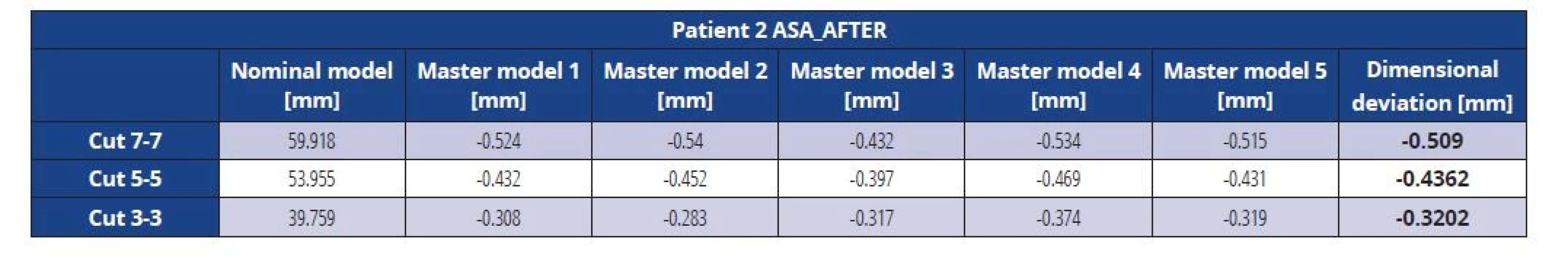
Tab. 11. Dimensional deviations of the Z-Ultrat master model before vacuuming (patient 2) 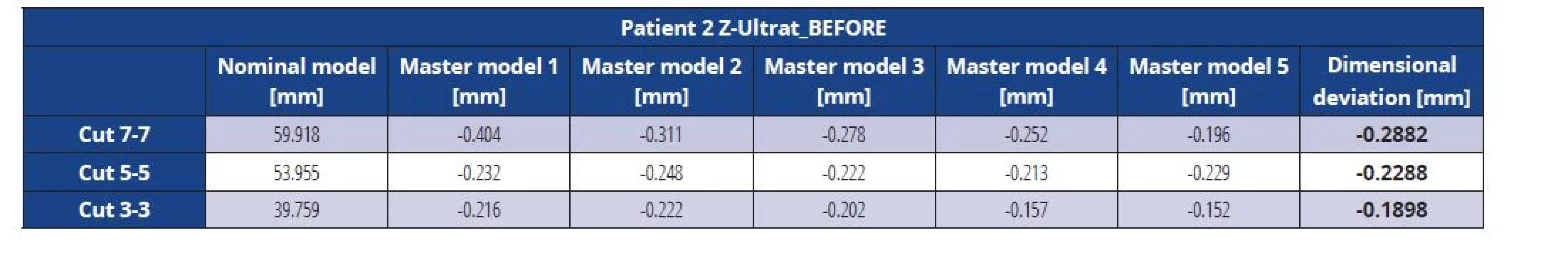
Tab. 12. Dimensional deviations of the Z-Ultrat master model after vacuuming (patient 2) 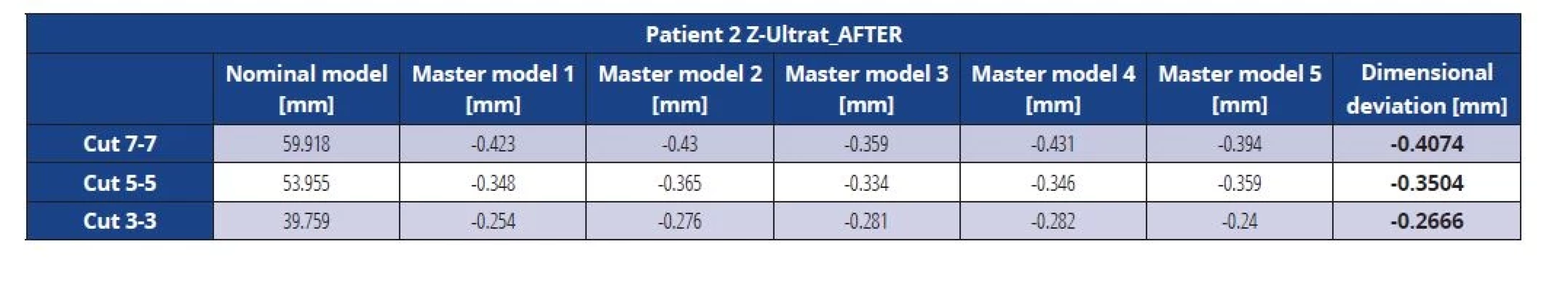
Graph 1 Dimensional deviations before and after vacuuming, patient 1 (material ABS) 
Graph 2 Dimensional deviations before and after vacuuming, patient 1 (material ASA) 
Graph 3 Dimensional deviations before and after vacuuming, patient 1 (material Z-Ultrat) 
Graph 4 Dimensional deviations before and after vacuuming, patient 2 (material ABS) 
Graph 5 Dimensional deviations before and after vacuuming, patient 2 (material ASA) 
Graph 6 Dimensional deviations before and after vacuuming, patient 2 (material Z-Ultrat) 
For a better overview of the reactions of the individual thermoplastic materials to the identical vacuum conditions to which they were subjected, the values of the dimensional deviations of all three materials were plotted together in one graph. This created 4 graphs –Graph 7 for the model from patient No. 1 before vacuuming, graph 8 for the model from patient No. 1 after vacuuming, graph 9 for the model from patient No. 2 before vacuuming, and graph 10 for the model from patient No. 2 after vacuuming. Blue color represents values for material ABS, red color values for material ASA and green color values for material Z-Ultrat (Graphs 7–10).
Graph 7 Comparison of all materials, patient 1, before vacuuming 
Graph 8 Comparison of all materials, patient 1, after vacuuming 
Graph 9 Comparison of all materials, patient 2, before vacuuming 
Graph 10 Comparison of all materials, patient 2, after vacuuming 
Table 13 summarizes the comparison of cut length deviations from the nominal model before and after vacuuming.
Tab. 13. P values calculated by statistical analysis of differences of deviations before and after vacuuming for every patient, material and cut 
DISCUSSION
The results show that the individual materials show different dimensional stability. It was interesting to observe that the printed physical models showed shrinkage against the scan of the dental arch in the oral cavity (nominal) in both Patients in each of the 3 Cuts. After insertion into the vacuum thermoforming machine, the master models (actual No. 2) showed approximately twice as large shrinkage compared to the nominal than the master models before vacuuming (actual No. 1). Prior to the vacuuming process, the shrinkage ranged from -0.143 mm in Cut 3 in Patient No. 1 in models printed from thermoplastic material ASA to the value -0.3212 mm in Cut 1 in Patient No. 2 also in models printed from ASA. After the vacuuming process, the lowest shrinkage rate was -0.2004 mm in Patient No. 1 in Cut 3 in models printed from thermoplastic material Z-Ultrat, and the highest shrinkage rate of -0.546 mm was in Patient No. 1 in Cut 2 in models printed from thermoplastic material ASA. It is, therefore, clear that the more frontal parts of the models of dental arches underwent a smaller dimensional change before and after the vacuuming process than the more posterior parts of the models.
The largest deviations were observed on models printed from ASA thermoplastic material. ABS and Z-Ultrat generally had very similar values, which is also logical, as in both cases, we are dealing with ABS. Z-Ultrat, with a chemical structure of PC-ABS, is expected to have greater hardness and resistance to high temperatures than regular ABS. It can be stated that the results of the experiment confirmed this hypothesis. In each section, both pre - and post-vacuuming process PC-ABS showed the lowest shrinkage values, with three exceptions. The first exception was the value of Cut 3 in Patient No. 1 before vacuuming, where the master model printed from material ASA had a slightly smaller deviation. The second and third exceptions were the value of Cut 1 after vacuuming, where the master models of both patients printed from ABS had slightly lower shrinkage than the master models printed from material Z-Ultrat.
It is also interesting that in models of 2 different dental arches, the greatest shrinkage occurred in different places of the dental arch. In Patient No.1, the largest contraction was noted in Cut 2 before the vacuuming process. After the vacuuming, the most noticeable contraction was very similar in Cut 1 and Cut 2. In Patient No. 2, the largest contraction was observed in Cut 1 both before and after the vacuuming process. The thermoplastic material used in both patients did not have any influence in this matter.
The statistical evaluation shows that all comparisons showed a statistically significant difference before and after the vacuuming process. The thermoplastic material Z-Ultrat came out of the statistical analysis as the best material, whereas thermoplastic material ASA came out of it as the worst one.
The evaluation of the data in a general linear model for repeated measures gave us the following result: the values for Cut 1 and Cut 2 were influenced by both the material and the patient. Cut 3 was only affected by the material, and the patient from whom the data was collected did not matter. No interaction was observed between the statistical values, which would suggest that any material is better for one patient.
Looking at the results in the tables, it is clear that the average values of the deviations of the lengths of the Cuts after vacuuming (actual No. 2) from the lengths of the Cuts on the initial scan (nominal) are smaller than the maximum clinically permissible deviation determined by the authors as +/ - 0.50 mm. Only three exceptions showed higher values, namely, Cut 1 and Cut 2 in Patient No. 1 in the model printed from the material ASA and Cut 1 in Patient No. 2 also in the model made from material ASA. Based on the above data, it can be stated that the models printed by the FDM method can be used as working models for the production of thermoplastic retention plates as long as the thermoplastic materials ABS and Z-Ultrat are used. Regarding the comparison of materials Z-Ultrat and ABS, the difference in the values of measured deviations between them is negligible for clinical practice. Because of that and the significantly higher price of thermoplastic material Z-Ultrat, the conventional ABS is recommended for printing dental models with FDM method as working models for creating thermoplastic retention plates. Based on the obtained results, we can conclude that material ASA is not recommended for this purpose. There are the following reasons for this conclusion: it has a higher price than ABS and shows a higher shrinkage rate when exposed to vacuum conditions.
At the time of writing the attestation work in the winter of 2020, according to my information, no articles were published in the professional literature examining the influence of the vacuuming process on the degree of dimensional stability of models from thermoplastic materials printed by the FDM method. Therefore, the results measured on these 30 samples cannot be compared with the results from other authors. Published articles on digitalization and 3D printing in orthodontics, meanwhile, largely focus on comparing the accuracy between the condition in the oral cavity and the intraoral scan or between the scan and the printed model. The lack of articles comprehensively dealing with this issue was one of the motivations for conducting this research.
In the discussion, I would like also to mention that the most widely used additive technologies in the field of dentistry are Stereolithography (SLA) and Selective Laser Melting (DMLS) [15]. DMLS additive technology is used to create metal structures in dentistry. Stereolithography, like FDM, is used to transform digital models into physical form, and it is often used to produce the working models for creating the thermoplastic retention plates mentioned in this experiment. This additive technology uses liquid resin as the material, which is cured in layers by an ultraviolet laser beam [16]. Models printed by this technology are stronger and more durable than models printed by the FDM method, so this additive technology is often used in orthodontic offices for the production of working models. However, SLA is significantly more costly than the FDM method [17]. Therefore, it is very good news that SLA can be reliably replaced by the FDM additive manufacturing technology for this purpose.
The conclusion for the practice, however, is our recommendation to conduct further research on the topic. There is virtually no data in renowned professional journals examining the effect of the vacuuming process on the dimensional stability of dental models printed from thermoplastic materials. It is, therefore, desirable that the results from this experiment, collected on the basis of only 30 samples, be supplemented.
CONCLUSION
The measurements in this experiment show that the vacuuming process caused a statistically significant change in the dimensions of the dental models printed by the FDM method in all 3 examined thermoplastic materials in all 3 Cuts. However, the magnitude of these deviations is small and acceptable in clinical practice. All models printed from ABS and Z-Ultrat met the maximum clinically permissible deviation of the dimensional difference between the scan and the model after vacuuming, determined by the authors to be +/ - 0.50 mm. Only models printed from thermoplastic material ASA showed higher valuesin Patient No. 1 in Cut 1 and Cut 2 and in Patient No. 2 in Cut 1.
The results of the measurements also confirmed that the models of dental arches printed by the FDM method can be used in clinical practice as working models for the production of thermoplastic retention plates.
As for the individual materials, the best dimensional stability was shown by the certified material Z-Ultrat with the chemical composition PC-ABS.
MDDr. Zuzana Hlavenková
Katedra čeľustnej ortopédie
Lekárska fakulta
Slovenská zdravotnícka univerzita
Limbová 12
833 03 Bratislava
Slovenská republika
e-mail: zuz.hlavenkova@gmail.com
Zdroje
1. Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics. 4. vyd. St. Louis: Mosby Elsevier; 2013, 725.
2. Junek I. 3D technológie. Prešov: Centrum celoživotného a kompetenčného vzdelávania Prešovskej Univerzity v Prešove; 2019, 119.
3. Slota J, Mantič M, Gajdoš I. Rapid prototyping a reverse engineering v strojárstve. Košice: TU v Košiciach, Strojnícka fakulta; 2010, 207.
4. Hudák R. Aditívne technológie v personalizovanej implantológii a tkanivovývh náhradách. Košice: TU v Košiciach, Strojnícka fakulta; 2019, 64.
5. McGuinness NJ, Stephens CD. Storage of orthodontic study models in hospital units in the UK. Br J Orthod. 1992; 19 : 227–232.
6. Fleming PS, Marinho V, Johal A. Orthodontic measurements on digital study models compared with plaster models: a systematic review. Orthod Craniofac Res. 2011; 14 : 1–16.
7. Mullen SR, Martin CA, Ngan P, Gladwin M. Accuracy of space analysis with emodels and plaster models. Am J Orthod Dentofacial Orthop. 2007; 132 : 346–352.
8. Hlavenková Z. Meranie rozmerovej stability modelov zubných oblúkov z termoplastických materiálov vytlačených metódou FDM počas procesu vákuovania [atestačná práca]. Slovenská zdravotnícka univerzita. Bratislava. 2021.
9. Milde J. Využitie 3D digitalizácie a aditívnych technológií v medicíne [dizertačná práca]. Trnava. Slovenská technická univerzita v Bratislave; Materiálovotechnologická fakulta so sídlom v Trnave; Ústav výrobných technológií. 2018.
10. Hrivňák I. Progresívne materiály a technológie biokompatibilné materiály. Technická univerzita v Košiciach, Hutnícka fakulta: Emilena; 2010.
11. Porubská M. Termoplastické materiály. Nitra: Univerzita Konštantína filozofa; 2008, 88.
12. Milde J, Hrušecký R, Zaujec R, Morovič L, Görög A. Research of ABS and PLA materials in the process of Fused Deposition Modelling method. Ann DAAAM Proceedings. 2017; 28 : 812–820.
13. Prospector. Acrylonitrile Styrene Acrylate (ASA) Plastic. [cit. 2020-11-28]. Dostupné z: https://plastics. ulprospector.com/generics/8/acrylonitrilestyrene - acrylate-asa
14. Zortrax. Z-ULTRAT. [cit. 2020-11-28]. Dostupné z: https://zortrax.com/filaments/z-ultrat/
15. Mohd Javaid, Abid Haleem. Current status and applications of additive manufacturing in dentistry: A literature-based review. J Oral Biol Craniofac Res. 2019; 3 : 179–185.
16. Materialise. Stereolitografie. [cit. 2021-12-19]. Dostupné z: https://www.materialise.com/cs/ manufacturing/technologie-materialy-adokoncovaci-upravy/stereolitografie
17. 3D Solved. Resin-vs-Filament-cost-in-3D-printing. [cit. 2021-12-19]. Dostupné z: https://3dsolved. com/resin-vs-filament-cost-in-3d-printing/
Štítky
Chirurgie maxilofaciální Ortodoncie Stomatologie
Článek EDITORIALČlánek DEN VÝZKUMNÝCH PRACÍ 2022
Článek vyšel v časopiseČeská stomatologie / Praktické zubní lékařství
Nejčtenější tento týden
2022 Číslo 3- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Orální lichen planus v kostce: Jak v praxi na toto multifaktoriální onemocnění s různorodými symptomy?
- Význam ústní sprchy pro čištění mezizubních prostor
- MIH – komplexní problém s nutností komplexního přístupu
- Benzydamin v léčbě zánětů v dutině ústní
-
Všechny články tohoto čísla
- VYUŽITÍ MIKRO-CT V ZUBNÍM LÉKAŘSTVÍ
- PŘÍPRAVA TKÁŇOVÝCH PREPARÁTŮ PRO HODNOCENÍ BIOLOGICKÝCH VLASTNOSTÍ NOVÝCH TYPŮ BIOMATERIÁLŮ
- EDITORIAL
- DOC. MUDR. VĚRA HUBKOVÁ, CSC., OSLAVILA VÝZNAMNÉ ŽIVOTNÍ JUBILEUM
- NAŠE POCTA JESENSKÝM, HRDINŮM HEYDRICHIÁDY
- MERANIE ROZMEROVEJ STABILITY MODELOV ZUBNÝCH OBLÚKOV Z TERMOPLASTICKÝCH MATERIÁLOV VYTLAČENÝCH METÓDOU FUSED DEPOSITION MODELING POČAS PROCESU VÁKUOVANIA
- DENTÁLNÍ A SKELETÁLNÍ ZMĚNY MAXILLY PO RYCHLÉ MAXILÁRNÍ EXPANZI
- DENTÁLNÍ KERAMIKA – MECHANICKÉ VLASTNOSTI
- DEN VÝZKUMNÝCH PRACÍ 2022
- UVOLŇOVÁNÍ BISFENOLU A Z DENTÁLNÍCH MATERIÁLŮ
- NANOČÁSTICE UVOLŇOVANÉ PŘI OPRACOVÁNÍ KOMPOZITNÍCH MATERIÁLŮ A JEJICH VLIV NA MARKERY OXIDAČNÍHO STRESU V PLAZMĚ
- VÝVOJ MUSKULOSKELETÁLNÍCH PORUCH U STUDENTŮ ZUBNÍHO LÉKAŘSTVÍ V PRŮBĚHU STUDIA
- PÉČE DENTÁLNÍ HYGIENISTKY O PACIENTA SE SNÍMACÍM ORTODONTICKÝM APARÁTEM
- NEOPTERIN, KYNURENIN A TRYPTOFAN JAKO MARKERY AKTIVACE IMUNITNÍHO SYSTÉMU U PARODONTITIDY
- PREVENTIVNÍ PŘÍSTUP K LÉČBĚ ORÁLNÍHO LICHEN PLANUS/LICHENOIDNÍ STOMATITIDY
- VZTAH MEZI ORÁLNÍ A GENITÁLNÍ KANDIDÓZOU
- STANOVENÍ BEZPEČNÝCH RESEKČNÍCH SLIZNIČNÍCH OKRAJŮ U ORÁLNÍCH DLAŽDICOBUNĚČNÝCH KARCINOMŮ
- DIFUZNÍ REFLEXNÍ SPEKTROSKOPIE JAKO ALTERNATIVNÍ METODA DETEKCE ZUBNÍHO KAZU – SROVNÁVACÍ STUDIE IN VITRO
- VLIV NÁSTROJE NA SKLOVINU PŘI SEJMUTÍ FIXNÍHO ORTODONTICKÉHO APARÁTU
- Česká stomatologie / Praktické zubní lékařství
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- DENTÁLNÍ KERAMIKA – MECHANICKÉ VLASTNOSTI
- DENTÁLNÍ A SKELETÁLNÍ ZMĚNY MAXILLY PO RYCHLÉ MAXILÁRNÍ EXPANZI
- NEOPTERIN, KYNURENIN A TRYPTOFAN JAKO MARKERY AKTIVACE IMUNITNÍHO SYSTÉMU U PARODONTITIDY
- MERANIE ROZMEROVEJ STABILITY MODELOV ZUBNÝCH OBLÚKOV Z TERMOPLASTICKÝCH MATERIÁLOV VYTLAČENÝCH METÓDOU FUSED DEPOSITION MODELING POČAS PROCESU VÁKUOVANIA
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




