-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
Authors: J. Lešták 1; Š. Pitrová 1; M. Žáková 1; M. Fůs 1; H. Hallová 1; K. Marešová 2
Authors place of work: 2. Oční klinika Lékařské fakulty Univerzity Palackého a Fakultní nemocnice Olomouc ; 1. Oční klinika JL Fakulty biomedicínského inženýrství ČVUT v Praze
Published in the journal: Čes. a slov. Oftal., 76, 2020, No. 6, p. 254-258
Category: Původní práce
doi: https://doi.org/10.31348/2020/35Summary
Purpose: The purpose of the study was to evaluate the visual functions after implantation of Acrysof monofocal intraocular lenses Alcon (SA60AT. MA50BM a SN60WF a SN6AT).
Materials and methods: Four works are presented in the overview. The first work deals with the effect of eye length. corneal optic power and anterior chamber depth on the uncorrected near visual acuity (UNVA) after IOL implantation. The second work compares the effect of eye position (horizontal and vertical) on the final UNVA. The third work deals with the influence of the spherical lenses (SA and MA) and yellow aspherical lenses (SN) on UNVA. The later work examines the effect of pupil width on UNVA.
Results: The first work showed the dependence of eye axial length (the largest in eyes bellow 22.5 mm. r=0.36) on UNVA. 77.4 % of eyes with axial length below 22.5 mm had UNVA better than 0.5 and 70.49 % of all evaluated eyes had UNVA better than 0.5. Uncorrected far visual acuity (UDVA) better than 1.0 was in 97.54 % eyes in the whole group. In the second work we found a mean correlation in eyes shorter than 22.5 mm with UNVA in horizontal position (r=0.39) and in the vertical position (r=0.49). UNVA improved in these eyes in horizontal position from 0.53 to 0.58 in vertical position of the eye. In all eyes from the group UNVA changed from 0.51 to 0.56. The third work demonstrated the effect of sphericity and chromaticity on UNVA. Better than 0.5 in the group of eyes shorter than 22.5 mm in SA IOL in 67 % and in SN IOL in 60 %. In eyes with mean axial length was UNVA better than 0.5 in SA IOL in 86.5 %. in MA IOL in 81 % and in SN IOL in 75 %. In eyes longer than 23.5 mm was UNVA better than 0.5 in SA IOL in 100 % of eyes, in MA IOL in 60 % and in SN IOL in 33 % of eyes.
In the fourth work the effect of pupil size was not demonstrated.
Conclusion: The works showed excellent results of UNVA and UDVA after implantation of Acrysof monofocal lenses.
Keywords:
uncorrected visual acuity – Acrysof monofocal intraocular lenses – axial length of the eye – anterior chamber depth – keratometry – eye position – aspheric and chromatic intraocular lenses – pupil depth
INTRODUCTION
The optical properties of refractive multifocal intraocular lenses (IOL) are similar to simultaneous vision of multifocal contact lenses, and are composed of zones with various optic power. As in the case of simultaneous vision with contact lenses, with IOLs also visual acuity is reduced, as is contrast sensitivity, especially upon low contrast. Almost 28 % of patients are able to read Jaeger no. 1 without correction 3 months after cataract surgery [1]. Urminský et al. recorded UDVA of 0.7 and better in 75.9 % of eyes and UNVA of 0.67 and better in 61 % of eyes after implantation of multifocal IOLs, using the model SA 40 N by the Allergan company [2].
Better results were attained by Cochener et al. following implantation of the multifocal diffractive IOLs ReSTOR®. Distance visual acuity equal to or better than 0.8 in 93.3% of patients, while 87.2 % of patients did not require glasses after surgery. 88.2 % of patients evaluated their vision as better than before surgery, and 93.1 % of patients believed that the operation had made a positive contribution for them [3].
Approximately the same results were attained also by Marešová et al. with the multifocal IOLs Acrysof ReSTOR SN6AD3. UDVA of 0.8 and better was recorded in 87.5 %, and UNVA worse than 0.6 was recorded in 10 % of eyes [4].
With the development of modern multifocal intraocular lenses there has been an improvement of resulting UDVA and UNVA. Veliká et al., by implantation of IOL LENTIS Mplus ad LENTIS MplusX (manufactured by Oculentis GmbH and Topcon Europe BV), attained UDVA of 1.0 and 0.9 respectively, and UNVA of 0.8 and 0.9 respectively [5].
Although multifocal IOLs may help patients attain better near visual acuity, they also result in an increase of higher order aberrations and reduced contrast sensitivity. Aspherical monofocal IOLs, in contrast with multifocal IOLs, reduce aberrations and improve contrast sensitivity [6].
Other authors have also reached similar conclusions. According to them, multifocal IOLs as against monofocal lenses are effective in the improvement of near vision. However, there is uncertainty with regard to the effect. Whether or not this improvement outweighs the negative effects of multifocal IOLs such as glare and halo differs according to individuals. A decisive factor will probably be motivation to become independent of glasses [7,8,9,10,11].
From our long-term clinical experience of implantation of monofocal intraocular lenses, we know that certain patients had both very good distance vision and reading vision without the use of glasses following an operation performed with the implantation of a monofocal intraocular lens. We wished to know the precise reason for this finding from a number of perspectives: 1) the role played by eye length, corneal optical power and anterior chamber depth, 2) the influence of eye position (horizontal and vertical), 3) the influence of spherical lenses (SA and MA) and yellow aspherical lenses (SN), and 4) the influence of pupil width.
1. Influence of axial eye length, keratometry and anterior chamber depth on UNVA following the implantation of monofocal IOLs [12]
In the first study we attempted to determine the influence on resulting uncorrected visual acuity exercised by the axial length of the eye, keratometry in the centre and axis of vision, and anterior chamber depth. We divided the cohort, which comprised 122 eyes, into three groups according to axial eye length. The first group comprised eyes with a length equal to or shorter than 22.5 mm, the second within a range of > 22.5 but shorter than or equal to 23.5 mm, and the third longer than 23.5 mm. Uncorrected distance visual acuity (UDVA) was 1.0 or better in 97.54 % of eyes for the entire cohort. For the individual eye lengths, UDVA was 1.0 or better in 97.37 %, 96.15 % and 100 % respectively. UDVA of 0.8 was recorded in 2.46 %. Correction did not improve this value. Uncorrected near visual acuity better than 0.5 was recorded in 70.49 % of eyes throughout the entire cohort. According to individual eye lengths, 77.4 %, 83.9 % and 62.9 % respectively. UNVA of 1.0 was recorded in 7.7 % of eyes, which were only from the first group (shorter than 22.5 mm). We demonstrated a medium dependency of UNVA on AXL in eyes shorter than 22.5 mm (r = -0.36), and of UDVA on KC in eyes with a length of > 22.5 but < 23.5 mm (r = 0.46). An ETDRS chart was used for examination of UDVA on all the individuals included in the cohort. To determine UNVA we used Zeiss reading charts with a reading distance of 40 cm. Values of vision are stated in the decimal system for both UDVA and UNVA.
If we are to summarise our findings in one sentence, then 77.4 % of eyes with an axial length of less than 22.5 mm had uncorrected near visual acuity (UNVA) better than 0.5, and 70.49 % of all evaluated eyes had UNVA better than 0.5. UDVA of 1.0 or better in 97.54 % of eyes. In this our results approach the results of eyes with an implanted MF IOL [13,14].
2. Influence of eye position on UNVA
In the second study, we evaluated the influence of eye position on UNVA (horizontal versus vertical) on the same cohort. With the aid of correlation coefficients we observed the relationship of keratometry in the centre (KC), keratometry in the visual axis (KVA), anterior chamber depth (ACD) and axial length of the eye (AXL).
In the case of vertical eye position (visual axis directed downward), UNVA was higher or the same as in horizontal gaze direction. Average UNVA in a horizontal direction was 0.508, in a vertical direction 0.555. Within the framework of the entire cohort, we determined a weak correlation between UNV and KC, KVA and AXL. We recorded the largest change of visual acuity in eyes shorter than and equal to 22.5 mm in length (p < 0.001, r = -0.39 for horizontal position, r = -0.45 for vertical eye position). This was followed by eyes longer than 22.5 mm but shorter than or equal to 23.5 mm (p < 0.001) and eyes with AXL larger than 23.5 mm (p < 0.001).
Conclusion: We recorded a change of UNVA upon a change of gaze in eyes of all different axial lengths (p = 0.001), on average in all eyes from 0.51 to 0.5. The highest attained average UNVA was in vertical position in eyes shorter than and equal to 22.5 mm (0.58), followed by eyes > 22.5 mm but shorter than or equal to 23.5 mm (0.56), and eyes longer than 23.5 mm (0.52) [15].
We believe that in short eyes in which an IOL with higher optic power was implanted, the same value of its shift in a direction towards the cornea generates higher myopia than in the case of an IOL with lower optic power.
3. Influence of asphericity and chromaticity of monofocal IOL on UNVA
Chromatic aberration may also stimulate pseudo-accommodation. SN60WF and SN6AT IOLs should have lower spherical aberration than conventional spherical IOLs, because they have an aspherical optic surface. In addition to this, pseudo-accommodation should be reduced in the case of these lenses due to their yellow tint. It is therefore possible to expect that pseudo-accommodation shall be reduced in eyes that have implanted aspherical or aspherical yellow IOLs in comparison with eyes with implanted spherical clear IOLs [16].
Nishi et al. also demonstrated lower pseudo-accommodation in the case of yellow aspherical lenses in comparison with spherical monofocal IOLs [17].
In another unpublished study, we focused on the influence of asphericity and chromaticity of IOLs on UNVA. Again this concerned the same cohort of 122 eyes. Table 1.
Tab. 1. Division of cohort according to UNVA, eye length and implanted IOLs.. 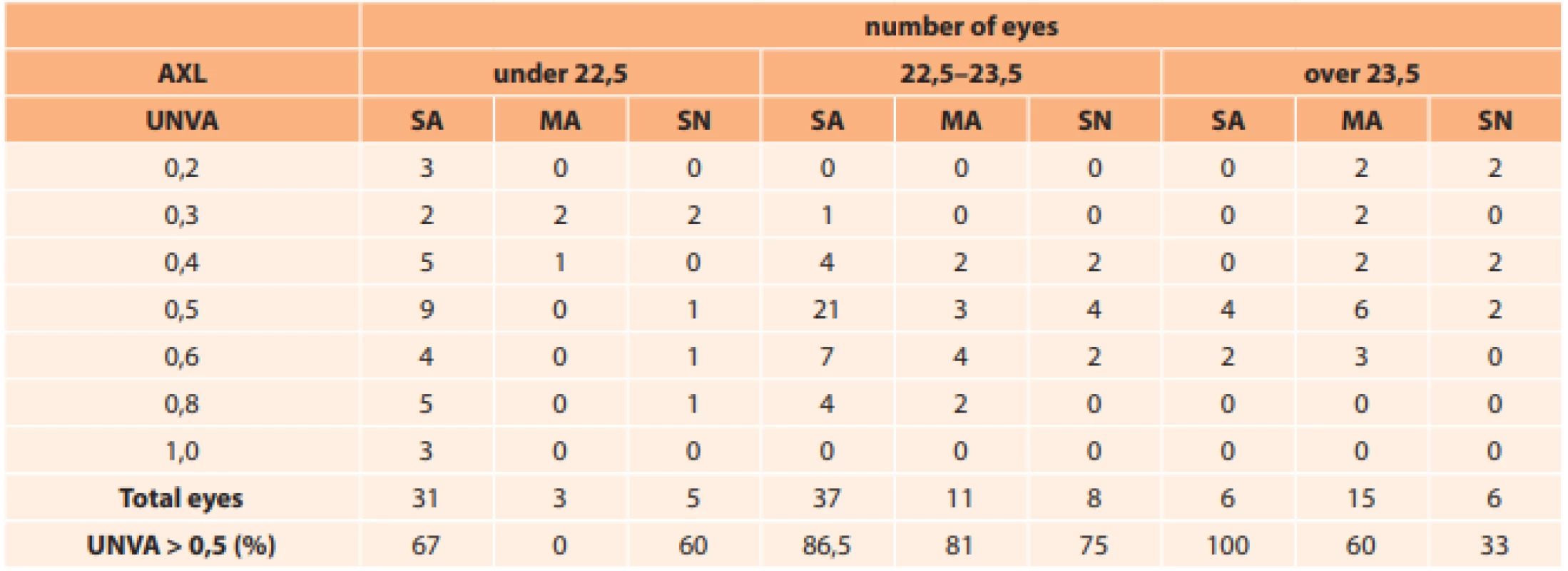
Our results are also similar. With regard to the fact that this does not concern an equal representation of all implanted IOLs for the individual eye lengths, it is not possible to accept these values as 100 %. Nevertheless, even these relatively small numbers demonstrate excellent results of UNVA with all types of used IOLs.
As regards the influence of coloured (yellow) and aspherical IOLs, we determined worse UNVA in comparison with clear spherical IOLs. UNVA better than 0.5 appeared in the group with eyes shorter than or equal to 22.5 mm in 67 % of cases, and with SN in 60 % (difference 7 %). In medium-length eyes UNVA was better than 0.5 with an SA IOL in 86.5 % of cases, MA in 81 % and SN in 75 % of eyes (average difference between SA and MA compared with SN was 8.75 %). In eyes longer than 23.54 mm, UNVA was better than 0.5 with SA in 100 % of eyes, with MA in 60 % and SN in 33 % of eyes (average difference between SA and MA compared with SN was 47 %).
Zeng et al. focused on the influence of pupil width, conducting an analysis of 124 eyes with cataract, divided into 3 groups according to implanted IOLs manufactured by Alcon (monofocal spherical, monofocal aspherical and multifocal). They did not determine statistically significant differences in visual acuity, pupil diameter and corneal aberrations in IOL-corrected eyes. They demonstrated higher spherical aberration in the case of multifocal IOLs in comparison with monofocal IOLs. With monofocal IOLs, spherical aberration was higher in spherical than aspherical IOLs. Contrast sensitivity was higher in monofocal spherical IOLs in comparison with multifocal IOLs (most pronouncedly in the spatial frequencies 3, 6, 12 and 18). Although multifocal IOLs can help attain better near visual acuity, they lead to an increase of higher order aberrations, and negatively influence contrast sensitivity in the patient’s eye. Aspherical monofocal IOLs reduce aberrations and improve contrast sensitivity in comparison with multifocal IOLs. The authors conclude the study by stating that multifocal IOLs may provide better near vision, but may increase higher order aberrations and negatively influence contrast sensitivity. An aspherical IOL may reduce aberration and improve contrast sensitivity in comparison with a multifocal IOL [3].From the calculated values of the correlation coefficient (Table 3) we determined that UNVA showed a medium dependency with axial length of the eye. The shorter the eye, the better UNVA was. The relationship between UNVA and the delta of change of pupil width showed a very weak correlation. This means that pupil width did not play a significant role in near vision.We included in the cohort 14 women with an average age of 71.1 years (64 to 83 years) and 6 men with an average age of 69.6 years (51 to 83 years). In all subjects we determined AXL, UNVA in horizontal eye position and pupil width. This was measured with the aid of photography of the eye from a distance of 40 cm in distance gaze and then in near gaze. The measuring instrument used was glasses with calibration at a distance of 1.5 cm from the corneal apex. The delta of change was calculated from the difference in values. The measured values are presented in table 2.
Tab. 2. Summary measured data (AXL – eye length, Ø – pupil width, UNVA – uncorrected near visual acuity). 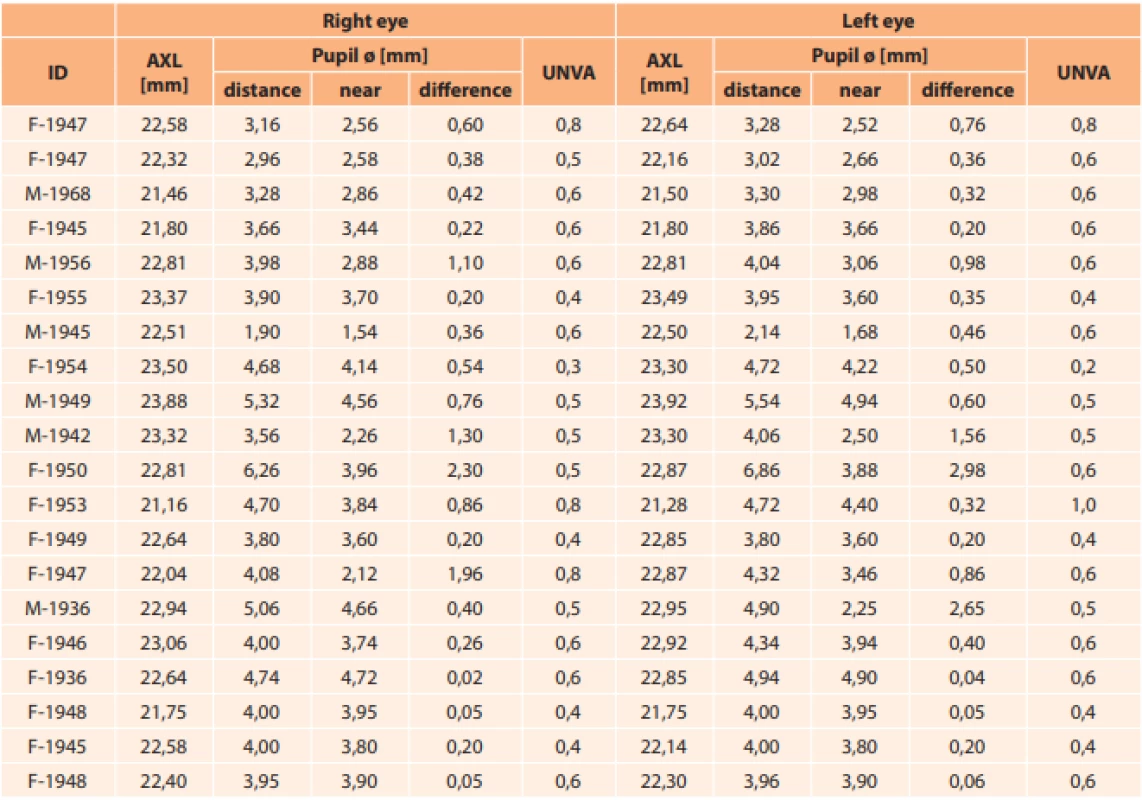
Tab. 3. Resulting values of Pearson correlation coefficient. UNVA – uncorrected near visual acuity; axl – axial eye length; delta – change of pupil diameter.. 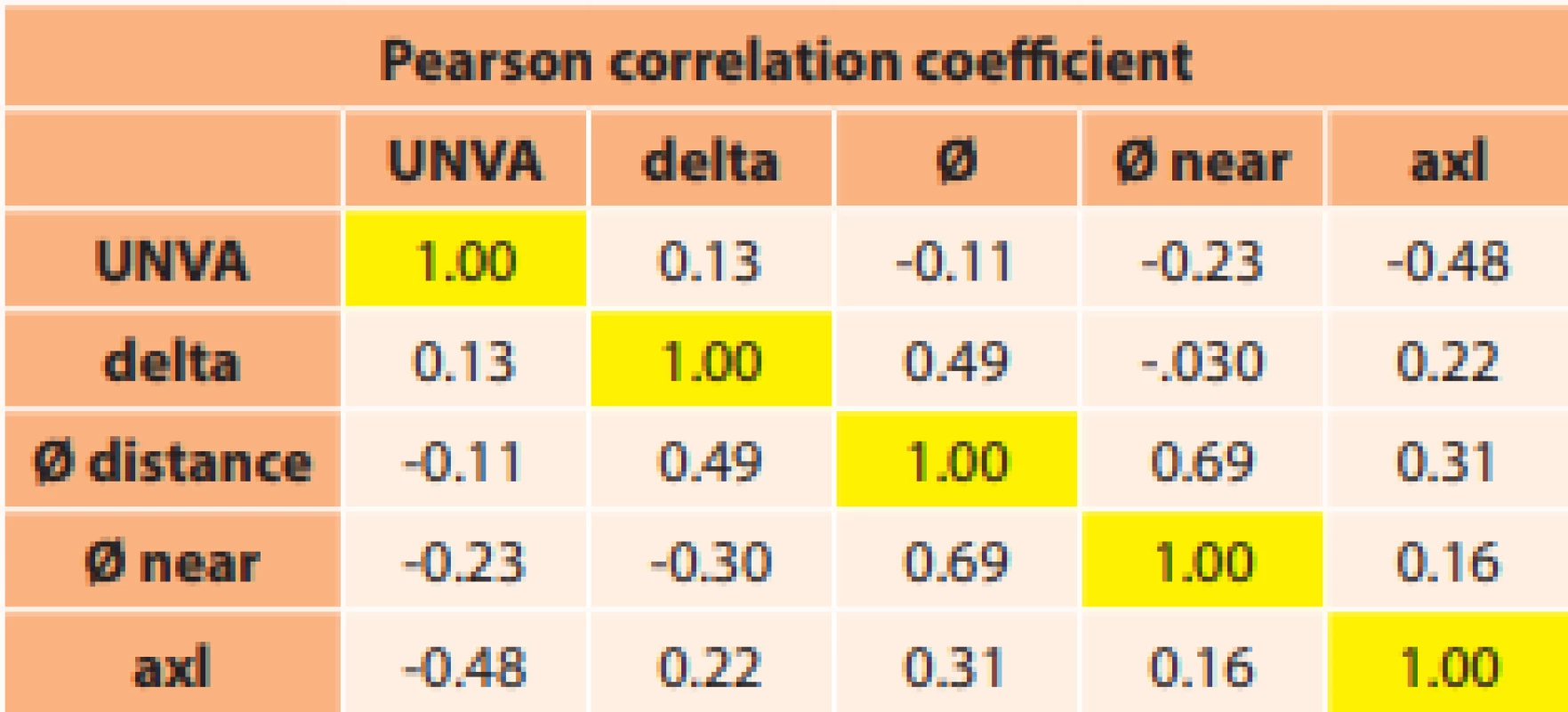
4. Influence of pupil width on UNVA
Our results are in accordance with the conclusions of the above-stated studies that pupil width has no fundamental influence on UNVA.
5. Conclusions ensuing from the above overview
The first study demonstrated a dependency of eye length (largest in eyes shorter than 22.5 mm, r = 0.36) on UNVA. 77.4 % of eyes with an axial length of less than 22.5 mm had UNVA better than 0.5, and 70.49 % of all evaluated eyes had UNVA better than 0.5. Uncorrected distance visual acuity (UDVA) was better than 1.0 in 97.54 % of eye throughout the entire cohort.
In the second study we determined a medium correlation in eyes shorter than 22.5 mm with UNVA in horizontal position (r = 0.39), and in vertical position (r = 0.49). In these eyes UNVA improved from 0.53 in horizontal position to 0.58 in vertical position.
The third study demonstrated the influence of sphericity and chromaticity on UNVA. UNVA better than 0.5 was recorded in the group of eyes shorter than 22.5 mm in 67 % of eyes with SA IOL, and in 60 % with SN. In medium-length eyes UNVA better than 0.5 was recorded in 86.5 % eyes with SA IOL, 81% with MA and 75 % with SN. In eyes longer than 23.5 mm UNVA better than 0.5 was recorded in 100 % of eyes with SA IOL, in 60 % with MA and 33 % of eyes with NS.
In the fourth study no influence of pupil size was demonstrated on UNVA.
List of abbreviations
IOL intraocular lens
SA60AT monofocal, hydrophobic, single-piece, spherical lens with diameter of optic part 6 mm
MA50BM monofocal, hydrophobic, three-piece, spherical lens with diameter of optic part 6.5 mm
SN60WF monofocal, hydrophobic, single-piece, aspherical, yellow lens with diameter of optic part 6 mm
SN6AT monofocal, hydrophobic, single-piece, aspherical, yellow toric lens with diameter of optic part 6 mm
UDVA uncorrected distance visual acuity
UNVA uncorrected near visual acuity
KC keratometry in centre
KVA keratometry in visual axis
ACD anterior chamber depth
AXL axial length of eye
Zdroje
1.Benjamin WJ. Borish´s Clinical Refraction, 2006, Elseviever, ISBN-13 : 978-0-7506-7524-6
2.Urminský J, Rozsíval P, Feuermannová A, Lorencová V, Jirásková N. Implantace multifokální nitrooční čočky. [Implantation of multifocal intraocular lenses]. Cesk Slov Oftalmol. 2004;60 : 30–36. Czech.
3.Cochener B, Fernández-Vega L, Alfonso JF, Maurel F, Meunier J, Berdeaux G. Spectacle independence and subjective satisfaction of ResTOR® multifocal intraocular lens after cataract or presbyopia surgery in two european countries, Clin Ophthalmol. 2010;4 : 81-89.
4. Marešová K, Mlčák P, Vláčil O. Výsledky operací katarakty s implantací Acrysof ReSTOR SN6AD3. [Results of the cataract with the Acrysof ReSTOR SN6AD3 intraocular lens implantation]. Cesk Slov Oftalmol. 2010;66 : 26-28. Czech
5.Veliká V, Hejsek L, Raiskup F. Clinical Results of the Implantation Two Types of Multifocal Rotational Asymmetric Intraocular Lenses. Cesk Slov Oftalmol. 2017;73 : 3-12. Available from: http..//www.cs-ophthalmologz.cz/en/journal/articles/13
6. Zeng M, Liu Y, Liu X, Yuan Z, Luo L, Xia Y. el al. Aberration and contrast sensitivity comparison of aspherical and monofocal and multifocal intraocular lens eyes, Clin Exp Ophthalmol. 2007;35 : 355-360.
7. Alió JL, Piñero DP, Plaza-Puche AB, Chan MJ. Visual outcomaes and optical performace of a monofocal intraocular lens and new-generation multifocal intraocular lenses. J Cataract Refract Surg. 2011;37 : 241-250.
8. Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses after cataract extraction Cochrane Database Syst Rev. 2003;(3):CD003169.
9. Shah S, Peris-Martinez C, Reinhard T, Vinciguerra P. Visual outcomes after cataracta surgery: Multifocal versus monofocal intraocular lenses. J Refract Surg. 2015;31 : 658-666.
10. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169.
11. Zhang W, Sun K, Xie J, Luo S, Lu Q, Hong J, Huang Y. The observation of visual quality after the implantation of apodised difractive multifocal intraocular lens.Yan Ke Xue Bao. 2007;23 : 79-83.
12.Lešták J, Pitrová Š, Fůs M, Žáková M. The Uncorrected Near Visual Acuity after the Monofocal Intraocular Lens Implantation. Cesk Slov Oftalmol. 2017;73 : 127–133. Available from http://www.cs-ophthalmology.cz/en/journal/articles/36
13.Cillino S, Casuccio A, Di Pace F, et al. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology. 2008;115 : 1508-1516.
14.Shah S, Peris-Martinez C, Reinhard T, Vinciguerra P. Visual outcomes after cataracta surgery: Multifocal versus monofocal intraocular lenses. J Refract Surg. 2015;31 : 658-666.
15.Zakova M, Fus M, Lestak J, Pitrova S. Effects of a change in the direction of view to near uncorrected visual acuity following implantation of monofocal intraocular lens. Biomed Rep. 2019;10 : 271–276. doi: 10.3892/br.2019.1203
16.Pandita D, Raj SM, Vasavada VA, Vasavada VA, Kazi NS, Vasavada AR. Contrast sensitivity and glare disability after implantation of AcrySof IQ Natural aspherical intraocular lens: prospective randomized masked clinical trial. J Cataract Refract Surg. 2007;33 : 603–610.
17.Nishi T, Nawa Y, Ueda T, Masuda K, Taketani F, Hara Y. Effect of total higher-order aberrations on accommodation in pseudophakic eyes. J Cataract Refract Surg. 2006;32 : 1643–1649.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2020 Číslo 6- Stillova choroba: vzácné a závažné systémové onemocnění
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Familiární středomořská horečka
- Kontaktní dermatitida očních víček
-
Všechny články tohoto čísla
- Uveal Melanoma Biopsy. A Review
- VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
- Evaluation of Patients Presenting to the Ophthalmology Department of a Tertiary Hospital for Nonemergency Reasons During the Covid-19 Pandemic
- Changed Eye Functions and Quality of Life of Seniors with Diabetic Retinopathy
- Can Visual Function Be Affected by an Open Foramen Ovale?
- Late Functional and Morphological Findings after Methylalcohol Poisoning
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Can Visual Function Be Affected by an Open Foramen Ovale?
- VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
- Late Functional and Morphological Findings after Methylalcohol Poisoning
- Uveal Melanoma Biopsy. A Review
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



