-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Ocular Symptoms of Rosacea
Authors: D. Beran; A. Stepanov; J. Studnička; N. Jirásková
Authors place of work: Přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO ; Oční klinika, Fakultní nemocnice Hradec Králové
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 6, p. 329-333
Category: Kazuistika
doi: https://doi.org/10.31348/2019/6/6Summary
The authors present case reports of two women, who were hospitalized in Department of Ophthalmology, University hospital Hradec Králové for ocular symptoms of rosacea. In the beginning there were relatively severe objective findings in the anterior segment of the eye in both cases – significant cornea graying with superficial and deep cornea vascularization in both eyes. On faces of both patients there were more or less typical sings of general illness. Especially in the first case there were severe papulopustules with crust all over the face. Subjectively Patients describe characteristic symptoms of dry eye. After dermatological consultation local and general anti-inflammatory treatment was set with consequent condition improving in both cases patients. In both cases we use two different general therapy formula according to literature (Azitromycin x Doxyhexal). In one case report, we found distinctive non-compliance during aftercare on our department with serious consequences.
The purpose of our report is to point out ocular complications of rosacea and importance of oftalmologist´s and dermatologist´s cooperation during therapy of this illness with can lead to permanent damage of front segment of the eye and significant loss of visual acuity.
Keywords:
dry eye – rosacea – eye rosacea treatment – face rash
INTRODUCTION
Rosacea is a multifactorial chronic inflammatory pathology with a broad spectrum of clinical symptoms. It is primarily characterised as a skin disease chiefly afflicting the face. Typical symptoms of rosacea are erythema of the cheeks, nose and forehead, avoiding the periorbital and perioral regions, often together with papules, pustules, teleangiectases and changes in the form of hypertrophy and fibrosis of the sebaceous glands on the nose (so-called rhinophyma). The pathology occurs especially in women aged between 30 and 50 years, and is characterised by phases of exacerbation and remission [6,13]. The prevalence of the pathology across populations ranges from less than 1% to 22% [9]. According to its manifestations, we may differentiate rosacea into four subgroups, namely 1) erythmatous with teleangiectases, 2) papulo-pustulous, 3) phymatous, and 4) ocular, which occurs in 25% of the population of patients with rosacea, and covers affliction of the anterior segment of the eye [9]. This does not necessarily appear on a background of its skin form, and in fact in up to 20% of cases it precedes skin symptomatology [10]. In as many as 58-72% of patients it causes chronic inflammation of the eyelids and cornea [5,14]. Dysfunction of the Meibomian glands causes the onset of dry eye syndrome. Typical manifestations of ocular rosacea also include blepharitis, blepharoconjunctivitis and keratitis.
The most recent studies indicate that patients suffering from rosacea are exposed to an increased risk of the progression of dementia, in particular Alzheimer’s disease [10]. Certain subtypes of this pathology are also frequently linked with other neurological manifestations such as burning or pain of the affected area of the skin, migraine, and also neuropsychiatric symptoms. An association has been described between rosacea and Parkinson’s disease, and more frequent cardiovascular affliction, including arterial hypertension [10,8,11].
The cause of rosacea still remains unclear. It concerns a dysregulation primarily of the skin’s natural immunity, and is linked with an increased concentration of pro-inflammatory peptides and hyperreactivity of blood vessels. An important component in the pathogenesis of the disease is also breach of the skin barrier, in which there is an increased penetration of substances from the outside environment, a decrease of hydration and increased transepidermal loss of water take place upon a breach of the stratum corneum. Last but not least, a role is played also by a breach of the vascular system (active vasodilation upon presence of substances such as bradykinin, substance P or endorphins), often with the presence of pathogenic microorganisms. So-called “triggers” also have a large influence on the course of the pathology. This is a group of external influences, which do not directly cause rosacea, but exacerbate its symptoms. This group of provocative factors includes for example heat, stress, ultraviolet radiation, spicy food or hot drinks [1].
CASE REPORTS
In January 2019 two women of different ages (20 and 72) reported to the outpatient Department of Ophthalmology at the University Hospital in Hradec Králové with similar ocular complaints in the form of burning, stinging and lachrymation of the eyes. On the anterior segment of the eye the finding was similar in both patients – mixed injection of conjunctiva, serous secretion and semitransparent cornea with neovascularisations. For a longer period of time, both patients had experienced primarily facial complaints in connection with rosacea.
Case report no. 1
A twenty year old woman was sent to the general outpatient section of the University Hospital in Hradec Králové by a local ophthalmologist, who had been observing the patient over the long term due to recurrent keratitis of both eyes since 2013. The primary skin diagnosis of the patient was acne vulgaris. On the face we recorded numerous papulopustules, some with a crust (Fig. 1). Swabs from the conjunctival sac taken 14 days before the patient’s visit to our outpatient clinic demonstrated the presence of Staphylococcus epidermidis. In the immediately preceding period the patient had been using Efflumidex gtt (Fluormetholone) 5x per daily in both eyes, as well as artificial tears. At our outpatient department she stated deterioration of the condition, primarily in the right eye. Best corrected visual acuity (BCVA) in the right eye was 6/18, in the left eye 6/7.5. The value of intraocular pressure was 18 torr bilaterally. On the anterior segment of both eyes there was evident mixed injection, the corneas were semitransparent with nubeculas and maculas following previous cases of keratitis, predominantly in the right eye. Another finding was superficial perilimbal neovascularisation of the cornea, in the right eye and deep (Fig. 2), on the surface there were perceptible fluorescein positive infiltrates (Fig. 3), the intraocular finding was physiological. The patient was hospitalised, on the day of admittance a consultation examination was performed at the dermato-venereological clinic with the following conclusion: rosacea with ocular manifestations. General anti-inflammatory therapy was set for the patient with Azitromycin 500 mg 1x per day within a regimen of three-day use, with a subsequent four-day pause, repeatedly with local use of Soolantra cream 10 mg/g on the skin (ivermectin) 2x per day. Of local therapy Floxal (ofloxacin 3 mg gtt.) with Dexamethasone gtt. was applied 5x per day into both eyes, together with artificial tears in the same regimen and Opatanol (olopatadine 1 mg gtt.) 2x per day due to subjective complaints of the patient in the form of itching and increased photophobia. After eight days of hospitalisation, we discharged the patient with the same BCVA as upon admittance in both eyes. The finding on the anterior segment of both eyes was markedly improved – injection of the conjunctiva had regressed and we recorded a reduction of the surface and number of corneal infiltrates. The patient reported to the general outpatient section for a follow-up examination 3 weeks after discharge with a deterioration of vision in the right eye to a value of 6/60 and with slight worsening of the ocular finding. The worsening of the patient’s condition was influenced to a certain degree by poor co-operation of the patient in her treatment. After repeated follow-up examinations with a gradual improvement of BCVA, we then retained treatment for the patient of Floxal ung. 2x per day applied to right and left eyes, Flucon (Fluometholone) gtt. to right eye 5x and left eye 3x per day, Optaonol gtt. 2x per day to right and left eye, Ikervis gtt (Cyclosporine) at night to right and left eye [2]. The patient remains on general antibiotic therapy in the same dose. At the last follow-up examination at our outpatient department the patient had BCVA of LE 6/7.5, RE 6/30, and also stated that she was in the 3rd month of pregnancy. Finding on anterior segment of both eyes: conjunctiva with superficial injection, cornea of right eye with vascular proliferation from the periphery with numerous maculas and nubeculas. Bilaterally the corneas manifest spotted colouring with fluorescein. Otherwise the finding was within the norm. Subsequently, due to the increased potential risk for the foetus (even despite exclusion of the teratogenic effects according to the sum of data on the pharmaceutical agent – SPC) we discontinued therapy with general antibiotics, Ikervis gtt., Floxal gtt, and we are continuing to observe the patient.
Fig. 1. Face of patient from case report 1, papulopustules with crust visible on face 
Fig. 2. Right eye of patient from case report 1, visible mixed corneal vascularisation 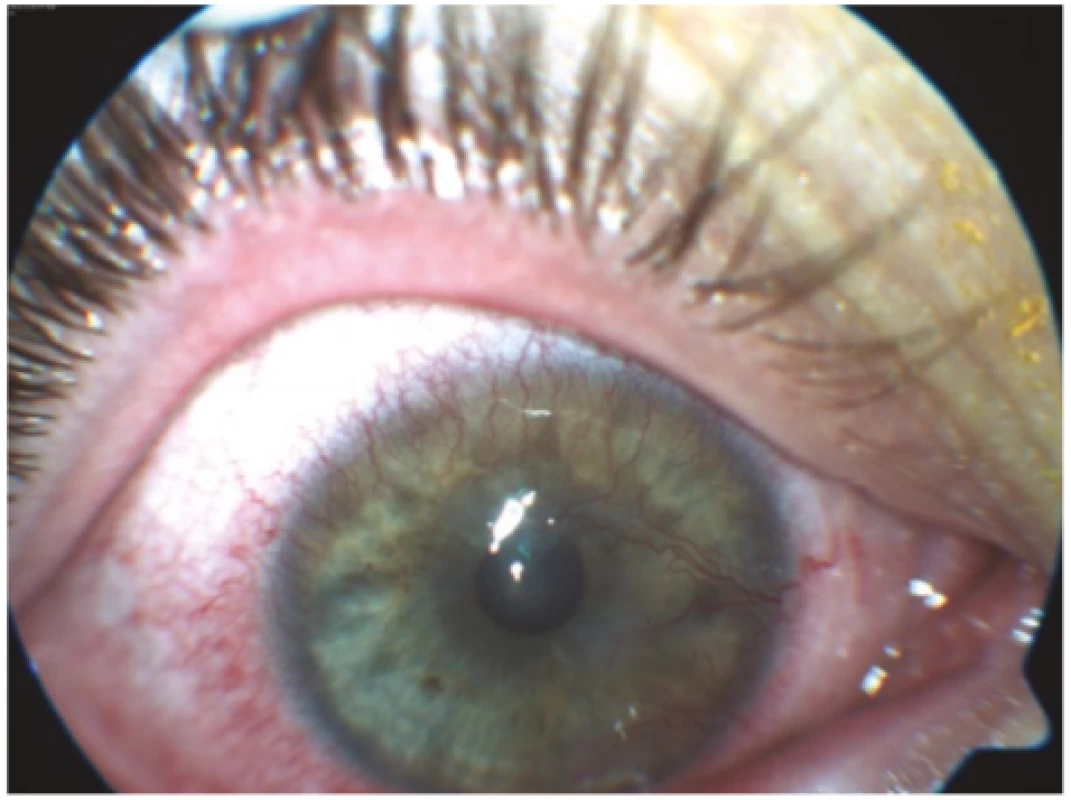
Fig. 3. Right eye of patient from case report 1, mixed injection of conjunctiva with incipient corneal ulcer by no. 7 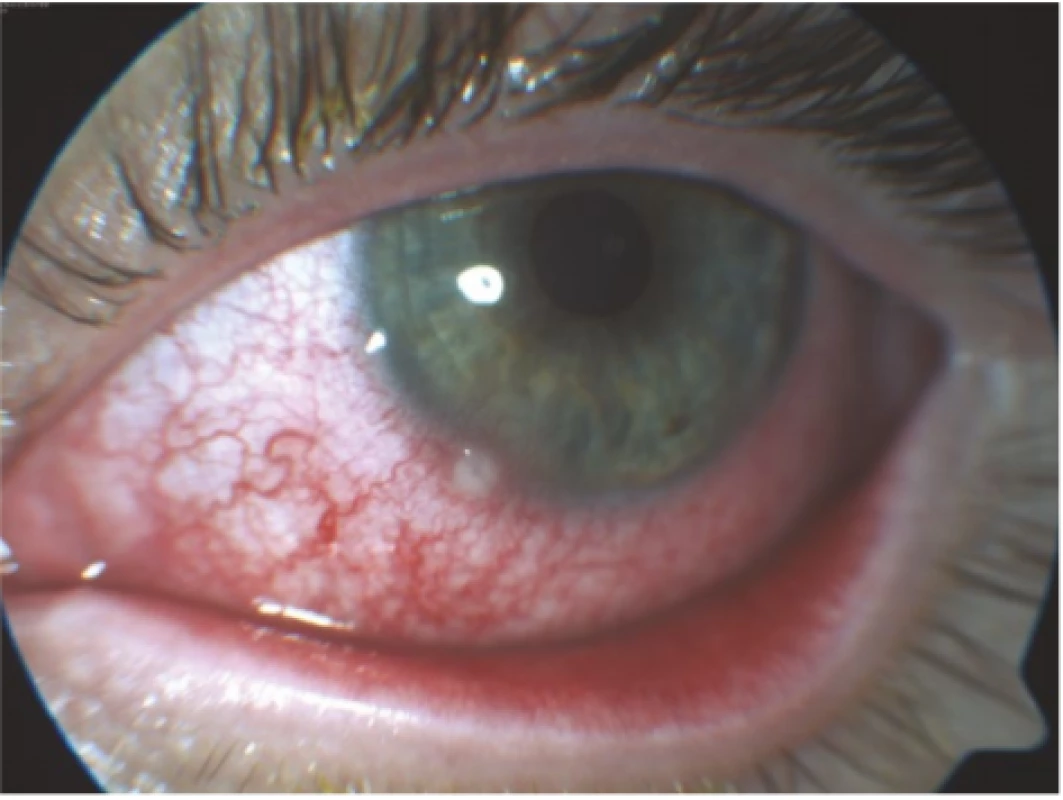
Case report no. 2
A seventy two year old woman was sent to our centre by a local ophthalmologist due to bilateral keratitis upon a background of general pathology of rosacea, for which she had been receiving treatment since 2016. She stated deterioration of vision over the course of approx. 3 weeks, lachrymation and reddening of the eyes. BCVA in the right eye was 1.5/60, in the left eye 0.3/60. Actinic keratosis was visible on the face (Fig. 4). The following finding on the anterior segment was recorded bilaterally: conjunctiva with mixed injection, seropurulent secretion and follicular reaction, cornea semitransparent, uneven surface, pronounced superficial and deep circular corneal neovascularisation by limbus, more in right eye (Fig. 5), intraocular finding physiological. The patient was hospitalised at our department with a diagnosis of keratoconjunctivitis bilaterally upon a background of general pathology of rosacea. Doxyhexal 200 mg (doxycyclin tablet) was administered 1x per day generally, with local application of Maxitrol gtt. (dexamethasone, Neomycin, Polymyxin-B) to both eyes every 2 hours, with rinsing with 5% Betadine solution. During hospitalisation a higher value of intraocular pressure was identified by chance in the patient in both eyes, which was well compensated by local antiglaucomatous therapy Simbrinza gtt. (combination of carboanhydrase inhibitor and selective alpha2 receptor agonist), Xalacom gtt. (combination of selective prostanoid FP receptor agonist with prostaglandin and non-selective beta-andrenergic receptor blocker). After 10 days of hospitalisation the patient was discharged with a slightly improved finding in the anterior segment and compensated IOP in both eyes, with retained local and general therapy (Doxyhexal was reduced to 100 mg/day). At a follow-up examination after 14 days the finding on the anterior segment showed a slight improvement bilaterally. One month later the patient was again admitted to the Department of Ophthalmology at the University Hospital in Hradec Králové due to decompensation of IOL bilaterally (RE 58 torr, LE 43 torr), with a diagnosis of secondary open-angle glaucoma upon local use of dexamethasone. The patient was administered Glycerol orally, with the addition of Diluran (Acetazolamide) 250 mg tablet to the existing local antiglaucomatous therapy. Due to the different impact on intraocular pressure, we replaced the originally used Maxitrol gtt. with one of the forms of Fluorometholone (Flucon gtt.). After five days of hospitalisation we discharged the patient with compensated bilateral IOP and application of antiglaucomatous therapy (Simbrinza gtt., Xalacom gtt., Diluran tablet), and vision of 6/24 in right eye and 6/12 in left eye. At a follow-up examination one month after discharge, the patient had well compensated intraocular pressure and markedly alleviated facial rosacea. The patient had reddened eyelids on both eyes, especially lower eyelids, hyperaemic conjunctiva without secretion, greying of the corneas with uneven surface and numerous scars up to the stroma, in the periphery with deep vascularisation. The other finding on the anterior segment was within the norm. Therapy: bilateral Flucon gtt., 2x per day, due to good compensation of pressure (11 and 9 torr) we switched to a triple combination of antiglaucomatous therapy Dualcopt gtt. 2x per day, Monopost gtt. 1x per day, and Vidisic gel 3x per day. We discontinued Diluran tablets due to abdominal discomfort and well compensated IOP bilaterally. We are continuing to observe the patient at our department.
Fig. 4. Face of patient from case report 2 with long-term well treated facial rosacea, with isolated actinic keratoses 
Fig. 5. Right eye of patient from case report 2 with mixed injection of conjunctiva, semitransparent cornea and peripheral limbal superficial and deep corneal vascularisation 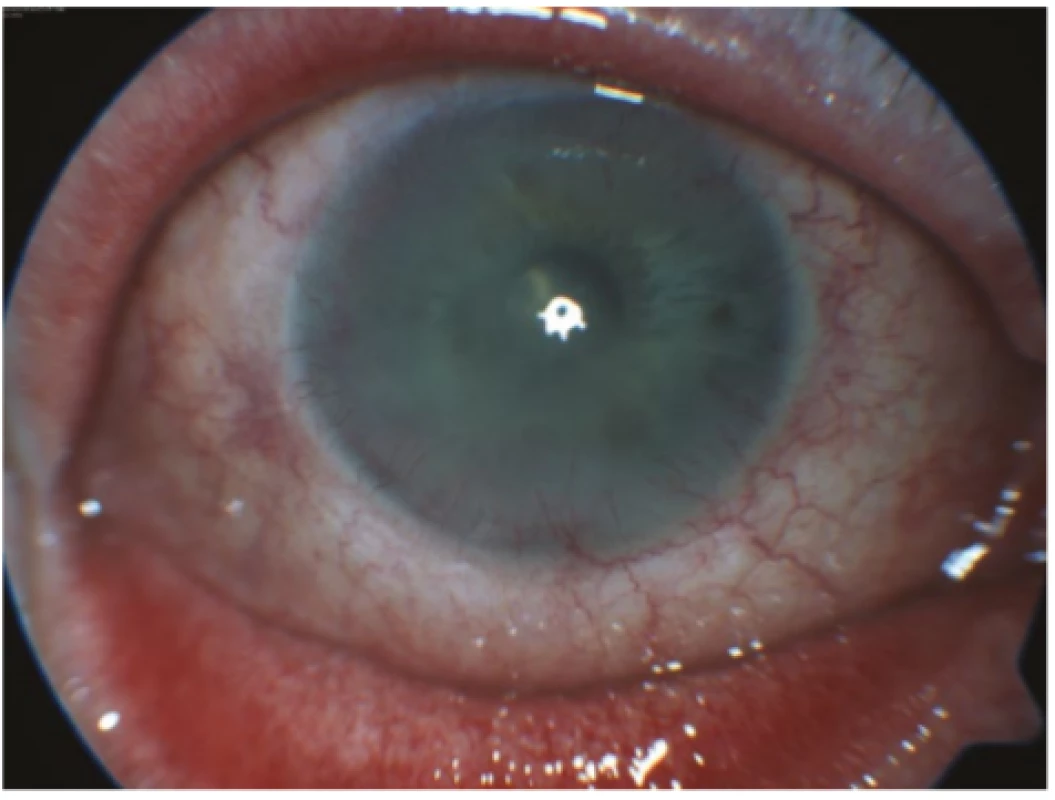
DISCUSSION
The literature states a relatively wide prevalence of rosacea at around 5% in women and almost 4% in men [3,7]. The probability of ocular complications is independent of sex, and is manifested in approximately ¾ of patients with a general pathology of rosacea. The most common objective symptoms found in patients are blepharitis, teleangiectases on the edge of the eyelid which frequently lead to its thickening, dysfunction of the Meibomian gland and papillary-follicular reactions on the tarsal conjunctiva [4,5]. Patients also frequently suffer from instability of the lachrymal film, with potential subsequent occurrence of keratopathy and corneal thinning [4,5]. In the case of our patients also, we recorded classic manifestations of ocular complications of rosacea.
A feature of interest is that some symptoms of the general pathology are linked to age and sex [3,10]. For example, erythema and facial skin flush are typical symptoms for patients of a young age. In older patients rosacea is more often manifested as teleangiectasia on the skin of the cheeks, and so-called rhinophyma occurs almost exclusively in patients of male sex [3]. This is partially confirmed also by our case reports, in which the first patient suffered from skin flush with numerous papulopustules. In the second case report this concerned a patient whose skin complaints are well compensated over the long term. Even despite severe ocular complications, there were no signs of erythema, papules or pustules.
Upon treatment of manifestations of rosacea, both local and general anti-inflammatory therapy is important.
Treatment of manifestations of the pathology most often takes place with the aid of locally administered gels containing beta-blockers or alpha-agonists, in the case of inflammatory manifestations preparations with azelaic acid, metronizadole or ivermectin are administered locally. In the case of an insufficient response to local therapy, doxycycline or azithromycin is administered generally.
In the Czech Republic, the following preparations containing metronizadole are available: Rozex 0.75% cream, Rosalox 1% cream. Also Ivermectin (broad-spectrum anti-parasitic agent), in which a beneficial effect has been demonstrated in 66% of patients [2]. Ivermectin belongs to the group of avermectins, which have anti-parasitic and anti-inflammatory effects. Its anti-inflammatory effects are the result of inhibition of inflammatory cytokine formation (TNFα, IL 10). It acts both on ectoparasites and on endoparasites. The anti-inflammatory effects are triggered primarily as a consequence of selective and affine bonds to glutamate-gated chloride channels in the nervous and muscular cells of invertebrates. In humans it does not influence motor neurones, and is therefore non-toxic. Through its anti-parasitic effect it leads to a reduction of the number and extermination of Demodex mites. Ivermectin in the form of cream is the medication of choice for papulopustulous rosacea and demodicosis. The recommended application is 1x per day (preferably in the evening) for 12-16 weeks. It is possible to repeat the therapeutic course. However, if no alleviation of the inflammatory manifestations is achieved within three months, it is necessary to terminate the treatment. One preparation with a content of ivermectin is available for treatment in the Czech Republic: Soolantra 1% cream.
Of non-pharmacological treatment, the recommended method of first choice is to adhere to strict hygiene of the eyelids (in the literature the use of diluted children’s shampoo is stated), together with application of warm face packs and the use of artificial tears [4]. In general therapy the most proven is the use of tetracycline [10]. Doxycycline is recommended for use in a dose of 100 mg 1-2 per day for 6-12 weeks. A dosage of 40 mg per day for a period of 16 weeks also appears to be effective [13]. Of local therapy, treatment with Metronidazole has been confirmed to be effective in trials. Metronidazole (a synthetic nitroimidazole derivative) has an anti-microbial, anti-parasitic and antioxidant effect. In the treatment of rosacea its anti-inflammatory effect is also applied (inhibition of chemotaxis leukocytes), as well as its antioxidant and vascular effect on the capillary endothelium. It is the pharmaceutical of choice in the treatment of papulopustulous rosacea, with recommended application 2x per day over a period of 8-12 weeks. In both our patients we used a different model of general and local treatment. In a comparison of these two cases we had better results in case report 2 (general therapy with Doxycycline 200 mt, locally with Maxitrol gtt. + rinsing with Betadine 5%), also within the framework of the subsequent follow-up examinations. However, the better result was also partially upon a background of well compensated skin symptoms of rosacea in patient 2, in whom essentially no local skin treatment was applied, and also of a certain degree of non-compliance on the part of the patient in case report 1.
CONCLUSION
On the basis of our case reports it is evident that even despite combined therapy with the participation of a dermatologist and ophthalmologist, the treatment of rosacea is highly complex, long-term and requires good co-operation of the patient in order to maintain the condition in remission. A further problem is the fact that the pathology often remains undiagnosed, and we therefore do not know its precise global prevalence.
Timely diagnosis of the pathology with application of appropriate therapy and regular inter-disciplinary co-operation are fundamental and necessary. Also important is emphatic instruction of the patient to avoid the triggers of the pathology.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
The authors of the study declare that this study has not been submitted to any other journal or printed elsewhere.
MUDr. David Beran
U Koupaliště 149,
Jablonné nad Orlicí, 56164
Received: 15. 11. 2019
Accepted: 14. 1. 2020
Available on-line: 20. 5. 2020
Zdroje
1. Abram, K., Silm, H., Maaroos, HI., et al.: Risk factors associated with rosacea. J Eur Acad Dermatol Venereol, 24; 2010 : 565–571.
2. Arman, A., Demirseren, DD., Takmaz, T.: Treatment of ocular rosacea: comparative study of topical cyclosporine and oral doxycycline. Int J Ophthalmol, 8 (3); 2015 : 544–549.
3. Buddenkotte, J., Steinhoff, M.: Recent advances in understanding and managing rosacea. Br J Dermatol, 181 (1); 2019 : 65-79.
4. Deepika, D., Chintan, M., Arun, KJ.: Ocular rosacea – a review. US Ophthalmic Review, 10 (2); 2017 : 113–8.
5. De Marchi, SU., Cecchin, E., De Marchi, S.: Ocular rosacea: an underdiagnosed cause of relapsing conjunctivitis-blepharitis in the elderly. BMJ Case Rep, 2014
6. Elewski, BE., Draelos, Z., Dréno, B., et al.: Rosacea - global diversity and optimized outcome: proposed international consensus from the Rosacea International Expert Group. J Eur Acad Dermatol, 25 (2); 2010 : 188-200.
7. Gether, L., Overgaard, LK., Egeberg A. et al.: Incidence and prevalence of rosacea: a systematic review and meta-analysis. Br J Dermatol. 179 (2); 2018 : 282–289.
8. Hua, TC.: Cardiovascular comorbidities in patient with rosacea: a nationwide case control study from Taiwan. J Am Acad Dermatol, 73; 2015 : 249–255.
9. Nevoralová, Z.: Léčba rosacey. Remedia, 27; 2017 : 219–225.
10. Powell, FC.: Clinical practice. Rosacea. N Engl J Med, 352 (8); 2005 : 793–803.
11. Rainer, BM., Fisher, AH., Luz Felipe da SD. et al.: Rosacea is associated with chronic systemic dis eases in a skin severity dependent manner: results of a case control study. J Am Acad Dermatol, 734; 2015 : 604–608.
12. Sannino, M., Lodi, G., Dethlefsen, MW. et al.: Fluorescent light energy: Treating rosacea subtypes 1, 2, and 3. Clin Case Rep, 6 (12); 2018 : 2385–2390.
13. Esther, JvZ.: Rosacea. N Engl J Med, 377; 2017 : 1754-1764
14. Vieira, AC., Höfling-Lima, AL., Mannis, MJ.: Ocular rosacea review. Arq Bras Oftalmol, 75 (5); 2012 : 363-9.
Štítky
Oftalmologie
Článek OCENĚNÍ ČLS JEPČlánek CENA PREZIDENTA ČLK
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 6- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
-
Všechny články tohoto čísla
- Innovative strategies for treating retinal diseases
- Assessment of the efficacy of photodynamic therapy in patients with chronic central serous chorioretinopathy
- Sensitivity and specificity in methods for examination of the eye astigmatism
- Evaluation of retinal light scattering, visual acuity, refraction and subjective satisfaction in patients after Acrysof IQ PanOptix intraocular lens implantation
- Eyelid edema as a first sign of lymphoma
- Ocular Symptoms of Rosacea
- 100 let od narození prof. MUDr. Heleny Lomíčkové, DrSc. 40 let oční kliniky dětí a dospělých v Motole
- OCENĚNÍ ČLS JEP
- CENA PREZIDENTA ČLK
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ocular Symptoms of Rosacea
- Eyelid edema as a first sign of lymphoma
- Assessment of the efficacy of photodynamic therapy in patients with chronic central serous chorioretinopathy
- Innovative strategies for treating retinal diseases
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



