-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaproLékaře.cz / Odborné časopisy / Česká a slovenská neurologie a neurochirurgie / 2022 - Supplementum 1The use of negative pressure wound therapy in a selected medical facility
Využití podtlakové terapie ran ve vybraném zdravotnickém zařízení
Cíl: Cílem studie bylo analyzovat využití podtlakové terapie ran (NPWT) ve vybrané fakultní nemocnici v České republice. Soubor a metodika: Retrospektivní neintervenční studie. Soubor zahrnoval všechny záznamy hospitalizovaných pacientů ošetřených NPWT ve vybraném zdravotnickém zařízení (FN) v období 2015–2017. Data byla extrahovaná z nemocničního informačního systému. Výsledky: Použití podtlakové terapie bylo vykázáno u 276 hospitalizovaných pacientů. Průměrná doba aplikace NPWT byla 19 dní (medián 10), průměrný počet výměn krytí 3,74 dny (medián 2) a interval výměny byl jednou za 2,99 dny (medián 2,33). Podrobná analýza roku 2017 ukázala, že v naprosté většině případů byl výsledek léčby NPWT pozitivní (n = 77; 84,62 %), pouze ve dvou případech nebyl efekt přínosný (2,20 %) a zbytek nebylo možné posoudit jasně (n = 12; 13,19 %). Závěry: NPWT je účinná pro léčba ran mnoha různých etiologií, existují však rozdíly v jejím použití. Vzhledem k tomu, že jsme identifikovali rozdílné přístupy v aplikaci a nedostatek standardizace, předpokládáme, že vzdělávání poskytovatelů zdravotní péče v této oblasti je nezbytným a zásadním aspektem pro podporu vhodného využívání NPWT a také pro sjednocení postupů pro zlepšování kvality péče.
Klíčová slova:
hojení ran – nemocniční informační systém – podtlaková terapie ran– retrospektivní studie
Authors: L. Krupová 1,2; A. Pokorná 3; D. Jarošová 2
Authors place of work: Dermatology Department, University Hospital Ostrava 1; Department of Health Sciences, Faculty of Medicine, University of, Ostrava 2; Department of Health Sciences, Masaryk University Brno 3
Published in the journal: Cesk Slov Neurol N 2022; 85(Supplementum 1): 15-20
doi: https://doi.org/10.48095/cccsnn2022S15Summary
Aim: The purpose of study was to analyse the use of negative pressure wound therapy (NPWT) in a selected university hospital in the Czech Republic. Patients and methods: A retrospective non-interventional study. The sample included all records of inpatients treated by NPWT in a selected medical facility (university hospital) in the period from 2015 to 2017. Data was extracted from the university hospital information system. Results: NPWT was reported in 276 hospitalized patients. The mean time of application of NPWT was 19 days (median 10), the average number of dressing changes was 3.74 (median 2), and the exchange interval was once every 2.99 days (median 2.33). Detailed analysis of 2017 showed that in the vast majority of cases the outcome of NPWT treatment was positive (N = 77, 84.62%), in only two cases the effect was not beneficial (2.20%) and rest of cases was not possible to assess clearly (N = 12, 13.19%). Conclusion: NPWT is an effective treatment for wounds of many different aetiologies, but there are differences in its use. As we identified different approaches in application and lack of standardisation, we assume that education of health care providers in this area is a necessary and essential aspect to support the appropriate use of NPWT and for the unification of procedures for the quality of care improvement.
Keywords:
Wound healing – negative pressure wound therapy – hospital information system – retrospective study
Introduction
Negative pressure wounds therapy (NPWT) refers to a controlled negative pressure (sub-atmospheric) system that is applied topically onto the wound. The wound is filled with a porous material (wound filler) and hermetically sealed with an airtight adhesive drape. A drain connects wound filler to the vacuum source that delivers a negative pressure. The suction is propagated from the vacuum source to the wound bed, leading to a negative pressure filler and removal of exudate [1].
NPWT stabilizes the wound, reduce edema, reduces the bacterial load, improve tissue perfusion, and stimulate granulation tissue [2]. It improves the possibility of spontaneous wound healing and reduces the need for major plastic surgical procedures. NPWT is simple and effective substitute for the management of various wounds than conventional dressings in terms of reduction in wound size, treatment duration and cost. Indications for NPWT are acute, chronic, and dehisced surgical wounds, diabetic, pressure, and venous leg ulcers, open abdominal wounds, fasciotomies, split-thickness skin graft recipient sites, flaps, and partial-thickness burns [3].
Benefits of NPWT for wound healing include reduction of the wound area and wound retraction, stimulation of granulation tissue formation, continuation of effective mechanical wound cleansing, continuous removal of wound exudate, reduction of the fluid concentration of wound healing-impairing proteases. In terms of handling NPWT offers bacteria proof wound dressing for sealing the wound, continuous clinical monitoring (as dressing is transparent), odourless and hygienic dressing technique, and reduction of required dressing changes [1]. It as well provides comfort for patients due to easy and early mobilization and visually appealing, clean exudate free dressing conditions. This leads to better quality of life in patients with non-heling wound [4].
The NPWT is applied to various non-healing wounds since 1990s and use is constantly increasing up to now [5–8]. A review of the literature evidence on NPWT performed by Apelqvist et al [1] identified 3287 publications published in 685 different journals between 1990 and 2015. One of the main outcomes of the review was that it has to be recognised that the impact on resource use and economic cost with regard to the use and indications of NPWT in patients with surgical wounds and chronic wounds is more complex than just healing rate and time-to-heal. NPWT impacts on health-care organisations and calls for relevant adaptation in terms of competence of staff, in - and out-patient organisation and updated reimbursement system and illustrates the transformation in wound care from passive topical treatment to an era of complex treatment modalities.
NPWT is an effective treatment for complex wounds in both inpatient and outpatient care [9]. Treatment by NPWT has a higher rate of complete healing, shorter healing time, and fewer amputations [10]. NPWT significantly decreases the time to complete wound healing, hastens granulation tissue formation, and reduces the wound size compared to conventional dressing [11]. NPWT is a major breakthrough in wound healing with significant potential use both in the hospital but also in the community [12]. Vaidhya et al [13] confirm that rate of healing is faster using NPWT and also NPWT is more cost-effective with right setup.
In selected university hospital in the Czech Republic, NPWT is used, but the use is not centrally controlled. The documentation is divided into medical and nursing parts. The main significance of our study is to be seen in the identification of a sample of patients to whom NPWT is applied and to describe the main characteristics for this type of treatment in a particular university hospital. We believe that data from descriptive retrospective analyses are the first step in refining documentation and optimizing the quality of care for patients with wounds treated with NPWT.
This study aimed to analyse the use of negative pressure wound therapy in a selected university hospital. The study is a starting point that will lead to an improvement in the process of documenting the use of NPWT.
Material and methods
Design
A retrospective non-interventional study carried out by analysing administrative data extracted from a hospital information system.
Sample
The sample included all records of inpatients treated by NPWT in a selected medical facility (university hospital) in the period from 2015 to 2017. A total of 276 records, was extracted from the hospital information system. The inclusion criterion was report of procedure no. 51850 (Wound dressing by NPWT method based on controlled vacuum) during hospitalization in the relevant period.
A valuable source for analysis was the electronic records of nursing documentation, which, as part of it, contains a detailed structured record of the wound (wound symptomatology description). Such an enriched sample of data was available only for 2017 and contained 91 patients.
Data collection
Data were extracted from the digital records in the hospital information system of reported procedures for health insurance companies. The extraction was performed by structured bulk export using SQL language directly from the database in the reporting module for insurance companies. Subsequently, data for hospitalizations for 2017 were enriched with manually retrieved information from electronic nursing documentation (for 2015 and 2016, this was not possible because the electronic nursing documentation took place in 2016), which includes a detailed record of non-healing wound care.
Data structure was patient identification, hospital department, main and secondary diagnoses, amount of reported procedures no. 51850, wound location, wound type, hospitalization period, period of NPWT application, number of NPWT coverage changes. Some data was computed based on extracted data – length of hospitalization, length of NPWT application, gender, diabetes mellitus and consistency of reporting between medical and nursing documentation.
Data analysis
Descriptive statistics and the following analyses were processed: the influence of gender, type of wound and diabetes over the length of hospitalization and the time of NPWT application (Kruskal-Wallis test and Mann-Whitney U test). Data analysis was performed by Microsoft Excel and IBM SPSS software (significance level 0.05).
NPWT is applied and changed by physicians with assistance of nurse. As the documented parameters in the medical records and in nursing documentation were different, a retrospective analysis showed the importance of sharing information on the application of NPWT among physicians and nurses not only related to wound care but also in documentation management. We have been aware that some gaps in documentation exist and therefore we have implemented the new electronic version of nursing documentation in 2016 and wanted to explore whether it was beneficial step. This was reflected in the fact that although some data would also be traceable in paper form documentation, the data of electronic nursing documentation was, more comprehensive, more accessible, more transparent, and more systematic. So, the nursing documentation (protocol of wound care) has been more precise. In the medical records the important data about the local status of the wound were missing.
Results
Between 2015 and 2017, NPWT was reported in 276 hospitalized patients. The use of NPWT in individual years was similar: 99 for 2015, 86 for 2016, and 91 for 2017. Of the total number, 156 (56.52%) were men and 120 (43.48%) women. The age of the patients ranged from 10 to 95, mean was 60. The average length of stay in the medical facility was 45.62 days (median 35). For details of descriptive statistics see Tab. 1.
Tab. 1. Characteristics of the research sample. 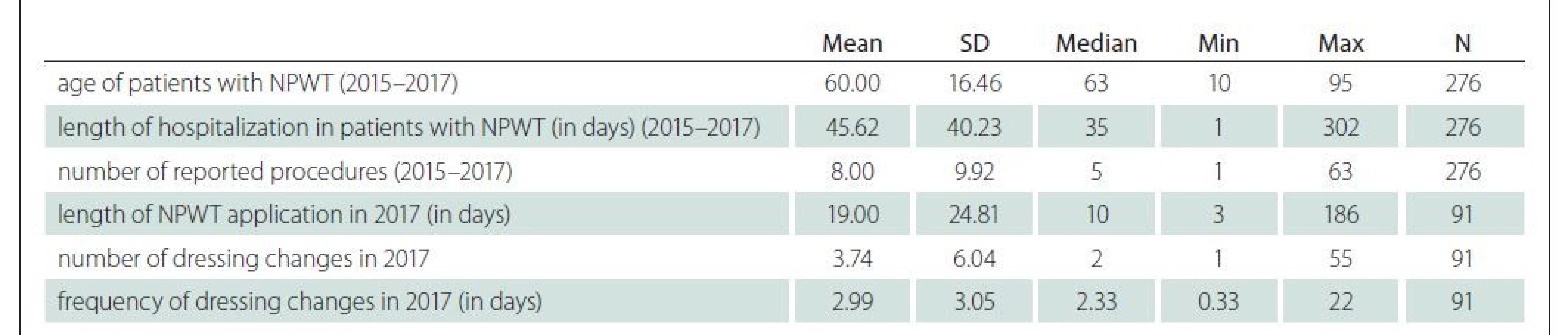
NPWT – negative pressure wound therapy; SD – standard deviation; N – number of respondents; Min – minimum value; Max – maximum value Most applications of NPWT (Tab. 2.) were in the Surgery (N = 86, 31.16%), Trauma Centre (N = 74, 26.81%) and Cardiac Surgery (N = 52, 18.84%).
Tab. 2. The use of NPWT based on department/clinic (2015–2017). 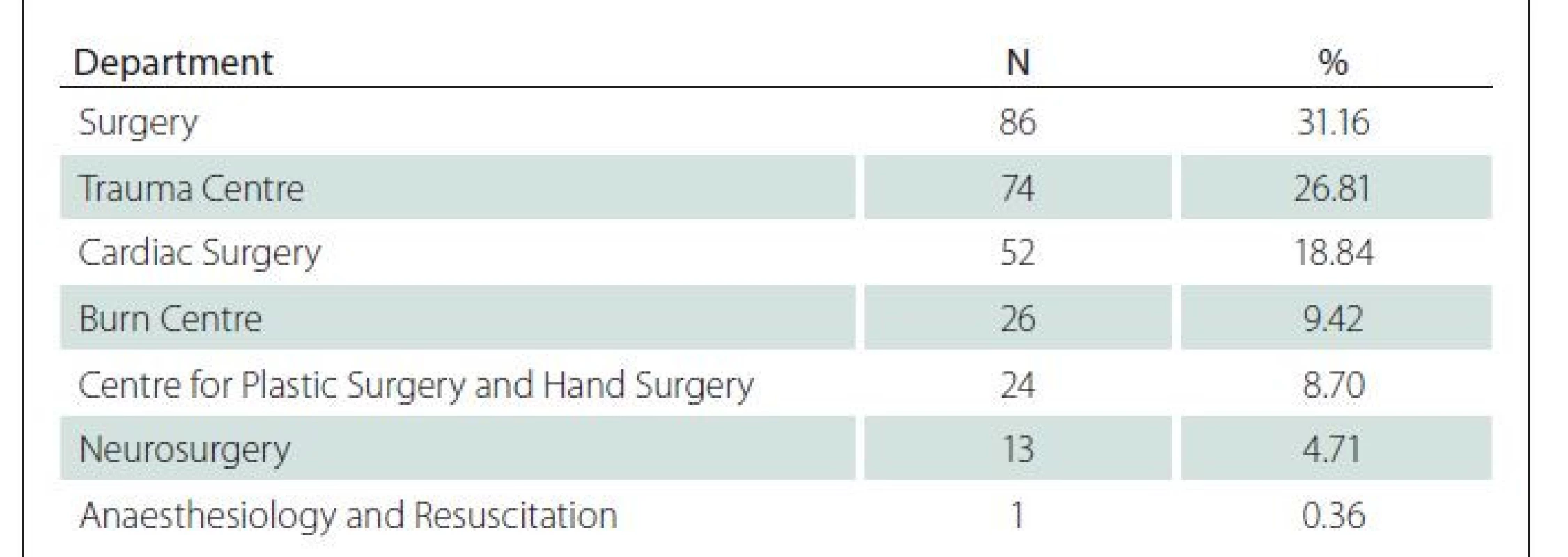
NPWT – negative pressure wound therapy; N – absolute count of cases; % – relative frequency The most common diagnosis in patients with NPWT according to the ICD-10 was T81.4: Infection following a procedure, not elsewhere classified, and T81.3: Disruption of operation wound, not elsewhere classified and Y83.2: Surgical operation with anastomosis, bypass or graft.
The number of reported procedures (51850 – Wound dressing by NPWT method based on controlled vacuum) ranged from 1 to 63, mean was eight, and median five.
As a source for analysis was the electronic records of nursing documentation, which, as part of it, contains a detailed structured record of the wound (wound symptomatology description). Data on the type of wound, location of the wound, time of application of NPWT, and assessment of the effect of treatment were added from the electronic nursing documentation. The number of dressings changes was also checked. It was possible to compare this figure with the number of reported performances and thus assess the consistency of the documentation. Unfortunately, the transition to electronic nursing documentation from the paper form took place in the selected medical facility during 2016. Therefore, it was possible to enrich only data on hospitalizations in 2017.
As for the type of wound (Tab. 3), the most common categories were dehiscence of a surgical wound (N = 59, 64.84%), burns (N = 9, 9.89%), traumatic wounds (N = 8, 8.79%) and pressure ulcers (N = 5, 5.49%).
Tab. 3. Wound types (hospitalisation in 2017). 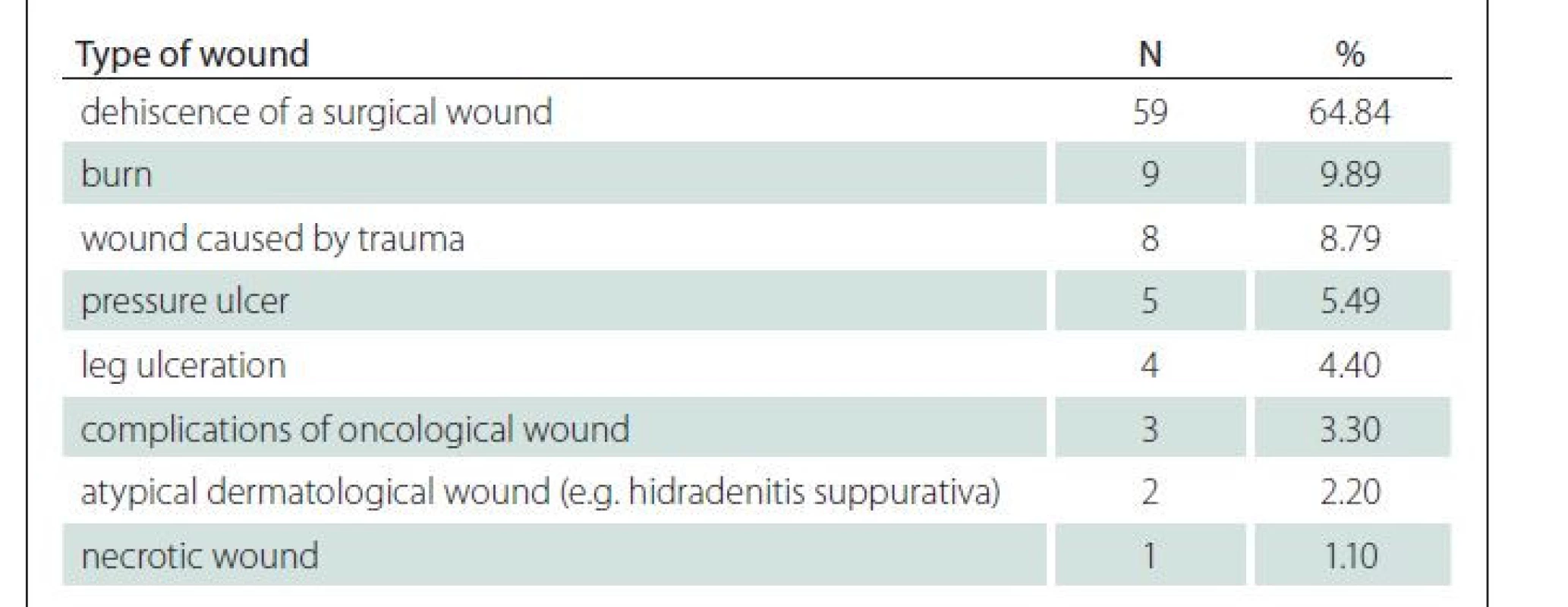
N – absolute count of cases; % – relative frequency Wound locations are summarized in Tab. 4. The most common location was lower limb (N = 34, 37.36%).
Tab. 4. Wound locations (hospitalization in 2017). 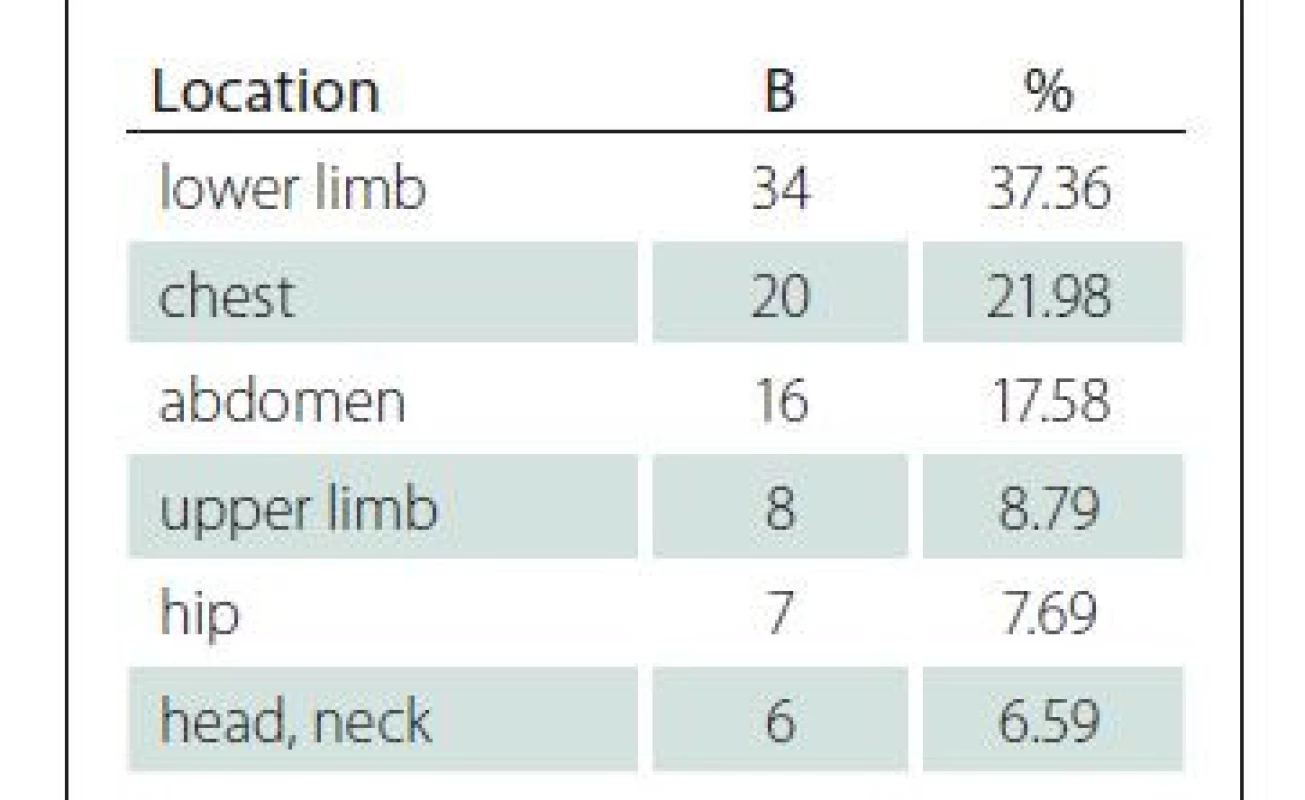
N – absolute count of cases; % – relative frequency The mean time of application of NPWT was 19 days (median 10), the average number of dressing changes was 3.74 (median 2), and the exchange interval was once every 2.99 days (median 2.33). For details, see Tab. 1.
The outcome of NPWT treatment was analysed in electronic nursing documentation. The effect was evaluated on the basis of changes in the description of the local finding from the electronic nursing documentation – according to exudation, granulation, epithelialization. In the vast majority of cases, the outcome was positive (N = 77, 84.62%). In only two cases, the effect was not beneficial (2.20%), and the rest of the cases was not possible to assess clearly (N = 12, 13.19%) due to the lack of reported information. The healing outcomes were evaluated based on Wound Healing Continuum (WHC) evaluation. It was evaluated as an improvement if the WHC category changed to a wound bed color showing better condition – from the worst black to the best pink or the wound was completely closed.
Because diabetes mellitus (DM) is significant comorbidity that negatively affects wound healing, we analysed the effect of DM on the total length of hospital stay and the length of NPWT application. The results showed that DM is not statistically related to either the length of hospital stay (Kruskal--Wallis test; P = 0.996) or the duration of NPWT (Kruskal-Wallis test; P = 0.677). However, statistical results are affected by the small number of cases of patients with DM (N = 18 of which N = 4 for 2017). In this respect, it will certainly be interesting to continue the analysis of a larger sample of data.
Gender is not statistically related to either the length of hospital stay (Kruskal-Wallis test; P = 0.767) or the duration of NPWT (Kruskal-Wallis test; P = 0.800).
Type of wound is not statistically related to either the length of hospital stay (Kruskal-Wallis test, P = 0.117) or the duration of NPWT (Kruskal-Wallis test; P = 0.216). For dependence of length of hospital stay the pairwise Mann-Whitney tests showed that statistical difference is only between dehiscence of a surgical wound and pressure ulcer (P = 0.017). For the summary of statistical analysis see Tab. 5.
Tab. 5. The relation of the monitored parameters to the treatment process. 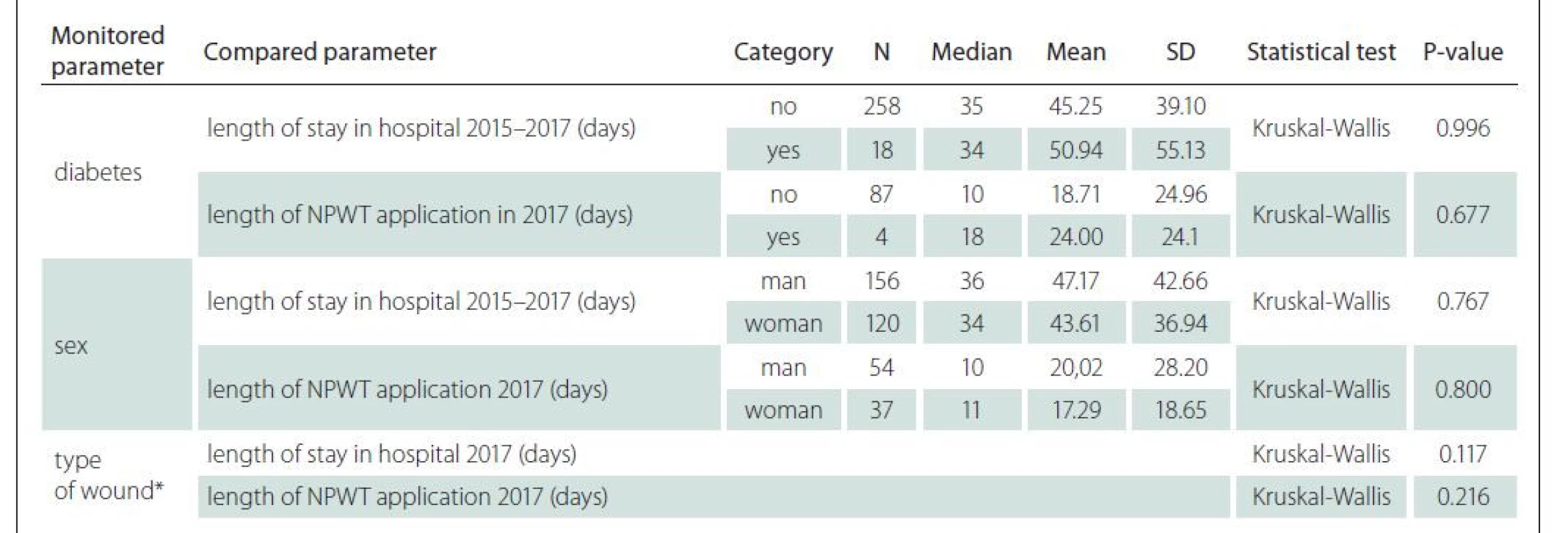
NPWT – negative pressure wound therapy; N – absolute count of cases; SD – standard deviation; P-value – value of statistical significance
* types of wound for the test were same as in the Tab. 4There were only four children (age less than 18 years) in the sample. Three of them suffered from burn and one child had a surgical wound.
Comparison between reported procedures for insurance companies in medical records and evidence of dressing changes in nursing documentation showed that only in 36 (39.56%) cases the number of reported procedures corresponds to the number of dressing changes and 55 (60.44%) cases are not consistent.
Discussion
As described in the methodology, the patient sample was compiled based on the reporting of procedure associated with the NPWT application for health insurance companies in the electronic records of the hospital information system. At this point, it is important to note that the knowledge of NPWT application and its availability is not equally widespread in all inpatient wards and therefore the composition of wound types when NPWT was used may not correspond to the composition of all wound types of patients treated in the university hospital or population of inpatients in the region in general. This also applies to the number of diabetic patients who received NPWT in 2017. It is surprising to us that there were only four such patients in the entire calendar year, which does not mean that there were no more diabetic patients for whom NPWT was appropriate. Also because of this, the results of the retrospective analysis were presented to selected departments and clinics of university hospital and educational seminars were organized to expand the general knowledge of NPWT and the benefits of its application.
According to Apelqvist et al [1], even in the case of a heavily draining wound, the NPWT dressing requires changing only every 2 to 3 days. It corresponds to the analysed average frequency of dressing changes in our study, which was 2.99 days.
The types of wounds in our analysed sample corresponds to indications for NPWT mentioned by Joshi et al [3]. The analysis also showed that the top primary and secondary diagnoses correspond to stated indications.
For diabetic foot ulcers (DFU), NPWT appears to be more effective, safe, and patient satisfactory compared to conventional dressings [14]. High quality studies approved the effectiveness, safety and cost benefit of the NPWT therapy for DFU [15]. However, Seidel et al [16] concludes their study aimed on a comparison of NPWT with standard moist wound care (SMWC) on DFU with finding that NPWT was not superior to SMWC in diabetic foot wounds in German clinical practice. The authors admit that documentation deficits and deviations from treatment guidelines negatively impacted validity of the results.
Nonetheless, our results did not confirm that DM is statistically related to either the length of hospital or the duration of NPWT application. However, analysis was affected by the small number of cases of patients with DM and although statistical significance has not been proven, the means of the individual groups vary.
Overall positive outcome of NPWT therapy (84.62%) corresponds to results of Krejčí et al [17] who reported in their retrospective study that in 84.6% complete wound healing was achieved.
During the detailed analysis, it was confirmed that several types of NPWT from different manufacturers are used in the selected medical facility. Unfortunately, data on the use of a specific type of device are not recorded in the documentation. Therefore, it was not possible to evaluate how often the individual devices are used and whether the results of the application differ according to the type of NPWT used. If in the future, it was possible to link devices to electronic documentation, this would lead to greater accuracy, and information would be available for usability and efficiency analysis. Because different types of devices need different consumables, despite the lack of data, the logical conclusion seems to be standardization to devices from one manufacturer.
Probably the most important result for the practice was that the analysis showed significant discrepancies between the reported procedures and the records from the electronic nursing documentation (more than 60% of cases did not match). In general, it is not possible to say which part of the documentation was more accurate. Each case had to be analysed separately by manual review of all available records, and results varied from case to case. In most cases, the number of reported procedures in medical records was higher than the recorded changes of dressing in nursing records. A detailed analysis revealed that it was a combination of several causes. In few cases, when the difference was extreme, there was a system error in the reporting methodology, where the number of reported procedures corresponded to the number of days of the application instead of the number of dressings. Another reason was insufficient documentation of dressing changes in nursing documentation. The exact cause of the difference in the data could not be verified in the rest of the records.
Limitations of the study
A limitation of this study is the focus on a single selected inpatient medical facility. Extending the analysis to more medical facilities would undoubtedly provide more general conclusions. Another limitation is that although the data of reported procedures were analysed for years from 2015 to 2017, manual retrieval of data from electronic nursing documentation was possible only for 2017 because the digitization of the nursing part of the documentation took place in a selected medical facility during 2016. Therefore, the research conclusions cannot be generalized due to the small sample. The authors plan to conduct extended research, where the research set will be expanded to include cases of patients from 2018–2020. A larger sample will make possible to verify the relationships between the monitored variables and will lead to higher validity of the results, including the possibility of their generalization to the entire population.
Conclusion
A retrospective analysis in a selected inpatient medical facility (University Hospital) in the Czech Republic has shown that NPWT is used for the treatment of wounds of many different aetiologies, but there are differences in its use. We have verified that in most of the patients treated with the NPWT the wound status has been positively changed based on Wound Healing Continuum (WHC). We also identified lack of standardisation and different approaches in NPWT application, thus we assume that education of health care providers in this area is a necessary and essential aspect to support the appropriate use of NPWT and for the standardization of procedures for improving the quality of care.
As we stated already, we have used retrospective analyses and we have to highlight that some data could be missing. The management of documentation, although in electronic form, is significantly influenced by the human factor. The care can be great, but when records are imperfect, the potential for retrospective analyses and the process of continuous improvement, in general, is limited. It is necessary to carry out regular, systematic control in the form of audits. The main benefit of our study is that we have proven discrepancies in the wound care documentation among nurses and physicians and highlighted the need for accurate wound care records which influence not only the quality of care but also the reimbursement from the insurance companies and planning for further care. The obvious goal in the future is to improve both the procedure reporting in medical records and the more accurate nursing documentation management. A useful improvement could also be the introduction of computer-assisted consistency checks in the hospital information system. Specifically, we recommend linking medical records and nursing documentation. We expect that when a physician documents the application of NPWT or on the basis of evidence of NPWT application for the insurance company, a specific nursing diagnosis is automatically generated, to which the nurse responds in the realization of care or in the detailed wound care record. For this purpose, the electronic form in the hospital information system for recording wound care will be extended to include structured items that explicitly record the use of NPWT, including the type of device used. So, both medical and nursing interventions will be recorded.
Based on findings, specific steps were implemented – educational workshops for physicians and non-medical health professionals focused on the effective use of NPWT in the treatment of wounds to increase awareness of NPWT in the university hospital and proposals for supplementing the functionality of the hospital information system, which will support the accuracy and consistency of medical and nursing documentation. In the future, we also plan to analyse in what percentage of all hospitalised patients the NPWT was applied to evaluate whether it is not underused or overused based on treatment results and comparison with data available from other studies.
Ethical aspects and conflict of interest
The authors solemnly declare that the manuscript has not yet been published or submitted for publication by another journal. They have no conflict of interest regarding the topic, creation, and publication of this article, and it received no support from commercial organizations. The authors declare that the present study involves no conflicts of interest. All used bibliographical sources have been cited. The data analysed in the study were retrieved from the electronic hospital system in the healthcare facility where the main author work. All data were analysed anonymously, and study was approved by the local ethical committee (the IRB number has not been given as it is not necessary for anonymous retrospective studies).
Acknowledgement
The article relates to the research grant project SGS13/ LF/2018 – Optimalization of use of NPTW in University hospital Ostrava, supported by student grant competition of the University of Ostrava.
Author contributions
Conception and design (LK, AP, DJ), data analysis and interpretation (LK), manuscript draft (LK), critical revision of the manuscript (AP, DJ), final approval of the manuscript (LK, AP, DJ).
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.Mgr. Lenka Krupová, Ph.D., MBA
Dermatology Department
University Hospital Ostrava
17. listopadu 1790/5
708 52 Ostrava-Poruba
e-mail: lenka.krupova@fno.cz
Zdroje
1. Apelqvist J, Willy C, Fagerdahl AM et al. EWMA document: negative pressure wound therapy. J Wound Care 2017; 26 (Suppl 3): S1–S154. Doi: 10.12968/jowc.2017.26.Sup3.S1.
2. Agarwal P, Kukrele R, Sharma D. Vacuum assisted closure (VAC) /negative pressure wound therapy (NPWT) for difficult wounds: a review. J Clin Orthop Trauma 2019; 10 (5): 845–848. doi: 10.1016/j.jcot.2019.06.015.
3. Joshi CJ, Hsieh JC, Hassan A et al. Application of negative pressure wound therapy on closed incisions. IntechOpen 2019. doi: 10.5772/intechopen.88658
4. Krupová L, Pokorná A. Quality of life in patient with non-healing wounds. Cesk Slov Neurol N 2019; 82/115 (Suppl 1): S40–S43. doi: 10.14735/amcsnn2019S40.
5. Liu S, He C, Cai Y et al. Evaluation of negative-pressure wound therapy for patients with diabetic foot ulcers: systematic review and meta-analysis. Ther Clin Risk Manag 2017; 13 : 533–544. doi: 10.2147/TCRM.S131193.
6. Iheozor-Ejiofor Z, Newton K, Dumville JC et al. Negative pressure wound therapy for open traumatic wounds. Cochrane Database Syst Rev 2018; 7 (7): CD012522. doi: 10.1002/14651858.CD012522.pub2.
7. Kirsner R, Dove C, Reyzelman A et al. A prospective, randomized, controlled clinical trial on the efficacy of a single-use negative pressure wound therapy system, compared to traditional negative pressure wound therapy in the treatment of chronic ulcers of the lower extremities. Wound Repair Regen 2019; 27 (5): 519–529. doi: 10.1111/wrr.12727.
8. Webster J, Liu Z, Norman G et al. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst Rev 2019; 3 (3): CD009261. doi: 10.1002/14651858.CD009261. pub4.
9. Bobkiewicz A, Banasiewicz T, Ledwosiński W et al. Medical terminology associated with Negative Pressure Wound Therapy (NPWT). Under-standing and Misunder - standing in the field of NPWT. Negative Pressure Wound Therapy 2014; 1 (2): 69–73.
10. Everett E, Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci 2018; 1411 (1): 153–165. doi: 10.1111/nyas.13569.
11. James SM, Sureshkumar S, Elamurugan TP et al. Comparison of vacuum-assisted closure therapy and conventional dressing on wound healing in patients with diabetic foot ulcer: a randomized controlled trial. Niger J Surg 2019; 25 (1): 14–20. doi: 10.4103/njs.NJS_14_18.
12. Panayi AC, Leavitt T, Orgill DP. Evidence based review of negative pressure wound therapy. World J Dermatol 2017; 6 (1): 1–16. doi: 10.5314/wjd.v6.i1.1.
13. Vaidhya N, Panchal A, Anchalia MM. A new cost-effective method of NPWT in diabetic foot wound. Indian J Surg 2015; 77 (Suppl 2): 525–529. doi: 10.1007/s12262-013-0907-3.
14. Lone AM, Zaroo MI, Laway BA et al. Vacuum-assisted closure versus conventional dressings in the management of diabetic foot ulcers: a prospective case-control study. Diabet Foot Ankle 2014; 5 : 23345. doi: 10.3402/dfa.v5.23345.
15. Mohseni S, Aalaa M, Atlasi R et al. The effectiveness of negative pressure wound therapy as a novel management of diabetic foot ulcers: an overview of systematic reviews. J Diabetes Metab Disord 2019; 18 (2): 625–641. doi: 10.1007/s40200-019-00447-6.
16. Seidel D, Storck M, Lawall H et al. Negative pressure wound therapy compared with standard moist wound care on diabetic foot ulcers in real-life clinical practice: results of the German DiaFu-RCT. BMJ Open 2020; 10 (3): e026345. doi: 10.1136/bmjopen-2018-026345.
17. Krejčí M, Novotný T, Staffa R et al. The use of negative pressure wound therapy for wound complication management after vascular procedures. Cesk Slov Neurol N 2019; 82/115 (Suppl 1): S29–S32. doi: 10.14735/amcsnn2019S29.
Štítky
Dětská neurologie Neurochirurgie Neurologie
Článek vyšel v časopiseČeská a slovenská neurologie a neurochirurgie
Nejčtenější tento týden
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Zolpidem může mít širší spektrum účinků, než jsme se doposud domnívali, a mnohdy i překvapivé
- Magnosolv a jeho využití v neurologii
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- Skin grafting in surgical treatment of pressure ulcers
- The use of negative pressure wound therapy in a selected medical facility
- Monitoring the prevalence of pressure ulcers – a comparison of national data with data of a specific health care provider – University Hospital Ostrava
- The use of incontinence devices and urinary/ faecal diversion management devices in hospitalised patients as a possible cause of unwanted immobilization
- Can different type of the pressure ulcers debridement affect oxidative stress parameters?
- Nurses‘ knowledge in the field of specific prevention and treatment of heels pressure injuries
- Identification of barriers and benefits of Negative Pressure Wound Therapy
- Standardization of wound care for patients in Austria, Germany and Slovakia
- Determiners of pressure ulcers formation – analyses from hospital information system
- Advanced practice nursing in the field of wound management
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Nurses‘ knowledge in the field of specific prevention and treatment of heels pressure injuries
- Monitoring the prevalence of pressure ulcers – a comparison of national data with data of a specific health care provider – University Hospital Ostrava
- Standardization of wound care for patients in Austria, Germany and Slovakia
- Advanced practice nursing in the field of wound management
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



