-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
proLékaře.cz / Odborné časopisy / Česká a slovenská neurologie a neurochirurgie / 2019 - Supplementum 1Multidisciplinary approach in surgical pressure ulcer therapy after spinal cord injury
Multidisciplinární přístup v chirurgické léčbě dekubitů u pacientů s míšní lézí
Chirurgická léčba rozsáhlých dekubitů u pacientů s traumatickou míšní lézí stále představuje velkou výzvu a často opomíjenou kapitolu, s níž je celá řada odborností denně konfrontována. Léčba pacientů často vyžaduje multidisciplinární spolupráci napříč nejen chirurgickými obory. Právě úzká spolupráce s výživovým specialistou, mikrobiologem a pracovníky z chirurgických oborů je mnohdy jedinou možností k úspěšné terapii. Cílem příspěvku je ve stručnosti shrnout základní parametry multidisciplinární spolupráce při léčbě rozsáhlých dekubitů u pacientů s míšní lézí. Výše zmíněný přehled v krátkosti demonstrujeme na sérii kazuistik z naší každodenní praxe. V diskuzi se zabýváme rolí jednotlivých chirurgických specializací, významem nutriční podpory a řešením infekčních komplikací.
Klíčová slova:
dekubity – míšní poranění – infekce – multidisciplinární spolupráce
Authors: P. Šín 1,2; J. Holoubek 1,2; A. Hokynková 1,2; B. Lipový 1,2
Authors place of work: Department of Burns and Plastic Surgery, University Hospital Brno, Czech Republic 1; Faculty of Medicine, Masaryk University, Brno, Czech Republic 2
Published in the journal: Cesk Slov Neurol N 2019; 82(Supplementum 1): 52-55
Category: Původní práce
doi: https://doi.org/10.14735/amcsnn2019S52Summary
Surgical treatment of extensive pressure ulcers in patients with spinal cord injury still represent a major challenge and often neglected part of care with which many experts is confronted daily. Treatment of these patients often requires extensive multidisciplinary approach across, not only, surgical disciplines. Close cooperation with a nutritionist, microbiologist and other surgical specialists is often the only way to successfully manage the problem. The aim of this publication is to briefly summarize the basic parameters in multidisciplinary collaboration in the treatment of large pressure ulcers in patients with spinal cord lesions. We then briefly demonstrate the above mentioned issues on a series of case reports resulting from our daily practice and then discuss the role of individual surgical specializations, the importance of nutritional support and the solution of infectious complications.
Keywords:
pressure ulcers – infection – spinal cord injury – multidisciplinary approach
Introduction
Pressure ulcers after spinal cord injury (SCI) represent a difficult problem leading to repeated hospitalizations, multiple operations and potentially devastating complications. This problem presents a challenge for patients, nurses and doctors [1]. Patients with SCI and its associated comorbidities are among the highest risk population for developing pressure ulcers. The incidence of pressure ulcers in the SCI population is 25 – 66% [2,3].
In this publication we describe the need for extensive multidisciplinary approach in surgical treatment of pressure ulcers in SCI patients. In the individual chapters we describe the importance of nutritional support, microbiological surveillance and interdisciplinary cooperation within the surgical closure of the defect. We then demonstrate the discussed topics with several examples based on our clinical practice.
Case series
Case report 1
A 68-year-old paraplegic patient was admitted to our clinic in septic condition with an extensive pressure ulcer in the sacral region (Fig. 1). Multiple necrectomy of the whole region was performed and intensive antibiotic therapy was introduced (further adjusted according to the results of cultivation and antibiotic sensitivity). Due to repeated contamination of the wound with stools (within closed distance of anus) and mainly the presence of the posterior wall of the rectum just below the bottom of the defect, it was decided that a sigmoidostomy would be created by a general surgeon. The condition was further complicated by the development of the ileus state, with the necessity of surgical revision due to rotation and malposition of intestinal loops. Derotation, desuflasion and re-suture were performed during revision surgery. Following the surgery, the post-operative period was uneventful. The closure of the pressure ulcer in such a stressful situation and under these conditions would be a high risk, especially in cases of wound healing in fields that have been re-operated several times. By this point, the patient was in malnutrition, hypoproteinemia and all his reserves were exhausted. Therefore, a conservative approach and intensive correction of all macro - and micronutrients was priority. Surgical closure of the wound was postponed for several weeks after the patient’s complete realimentation. The final wound closure was performed one month later. The entire defect was covered by a large fasciocutaneous flap from the left half of the sacral/ gluteal region (Fig. 2). The whole hospitalization period was managed under precise microbiological surveillance and targeted antibiotic therapy.
Fig. 1. Large and deep pressure ulcer in whole sacral region.
Obr. 1. Rozsáhlý dekubitus postihující prakticky celou oblast sakra a hýždí.
Fig. 2. Defect after closure with large transposition flap.
Obr. 2. Defekt po definitivním uzávěru transpozičním lalokem.
Case report 2
As our second case, we present a 43-year-old paraplegic man, who was admitted to our clinic with large infected pressure ulcers in the sacral and right trochanteric region (Fig. 3). Both defects were severely contaminated by multiresistant strains of Pseudomonas aeruginosa and Acinetobacter baumanii, which required prolonged and challenging antibiotic therapy with close cooperation with the Department of Clinical Microbiology. Preoperative examination and CT scans showed extensive osteomyelitis in the right proximal femur. In cooperation with an orthopedic surgeon, we performed radical resection of the proximal femur and subsequently radical necrectomy of both defects. At first, we decided to close the smaller and more superficial defect in the sacral region with a V-Y fasciocutaneous flap. In the trochanteric region, the defect was large and deep so we decided to apply NPWT (Negative Pressure Wound Therapy) for promoting granulation and remediation of infection. We sustained the vacuum assisted closure therapy for several weeks, together with intense nutrition support. Finally, after 1 month we could close the defect with a large transposition flap (Fig. 4). Further healing and the post-operative period were without any complication.
Fig. 3. Large trochanteric defect with luxated femur. Picture after osteotomy of proximal femur, including caput femoris.
Obr. 3. Rozsáhlý trochanterický dekubitus s dominující luxovanou kyčlí. Obrázek již po provedené osteotomii hlavy a proximální části femuru.
Fig. 4. Peroperation picture after elevation of large fasciocutaneous flap for closure of trochanteric defect.
Obr. 4. Peroperační snímek elevace fasciokutánního laloku k uzávěru trochanterického dekubitu.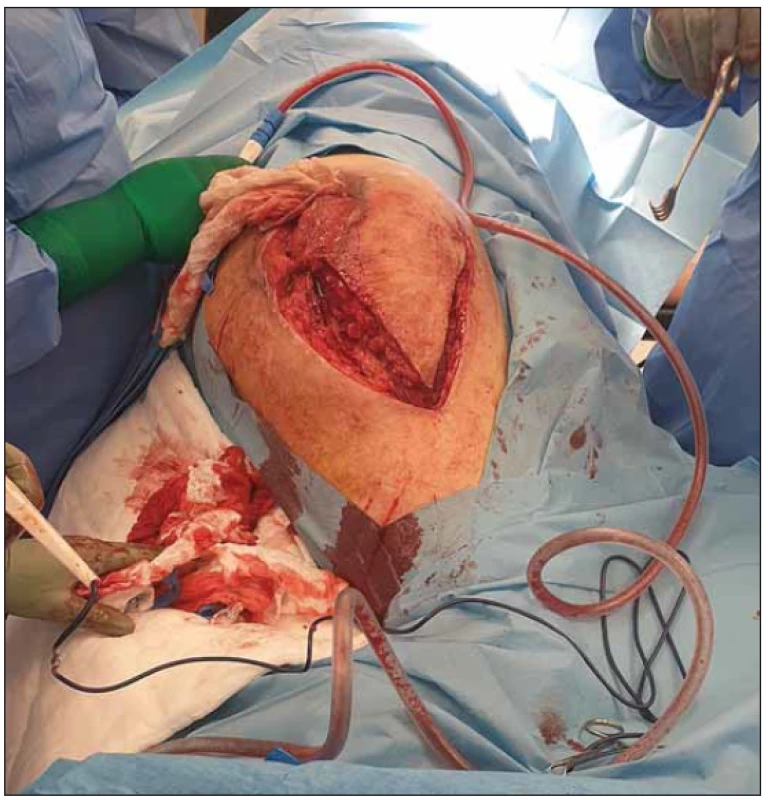
Discussion
University Hospital Brno provides one of four SCI in the Czech Republic. As a part of this service, a multidisciplinary surgical team was established for the surgical management of pressure ulcers arising in this patient group. Despite the growing possibilities of conservative therapy, the extensive pressure ulcers of grades III and IV can only be closed by surgical excision and reconstruction. Due to the fact that such an intervention is generally an elective surgical procedure, patient’s overall condition and chronic medical comorbidities (e. g. diabetes mellitus, hypertension, malnutrition, and anemia) have to be compensate by the multidisciplinary team before a patient is considered a good candidate for surgery [1]. If the ulcer or ulcers are in close proximity to the anus, clinical judgment should address the need for bowel diversion by colostomy. The presence of stool significantly compromises wound healing and makes its toilet virtually impossible. Furthermore, the close proximity of the rectum to the defect may complicate the surgical procedure and its possible perforation may result in fatal complications [4]. The same applies to the perineal region – the creation of a temporary or permanent urinary diversion should be considered here. The presence of an orthopedic surgeon is often required due to osteomyelitis, which will also have a significant impact on further surgical plans. Often, a radical osteotomy is required before final wound closure [5]. Only after proper radical surgical debridement, including of bone structures and conceiving a proper surgical field, the defect can be closed by a plastic surgeon. Surgical management of pressure ulcer closure involves a spectrum of options, from simple debridement with direct closure, to skin grafting, fasciocutaneous flaps, myocutaneous flaps or even free flaps [1]. The choice of flap reconstruction always depends on a number of factors such as anatomical location, reoperated terrain, general condition and surgeon‘s preference [4]. Considering the spectrum of patients with often neglected chronic wounds and a very poor overall condition, it is clear that the resulting surgical effect is burdened with a corresponding percentage of complications and recurrences. Scientific sources show different percentages of complications. For example, Sameem et al reports complications ranging from 9 – 20%, depending on the type of flap chosen. The most frequent complications in their study were flap necrosis (partial), wound dehiscence, infection and recurrence of pressure ulcer [6]. The ideal nutritional intake continues to be discussed to this day. Energy, protein, arginine, and micronutrients are all essential for proper wound healing. Proteins play the most important role in the healing process and are essential in the fibroblast proliferation process, angiogenesis, collagen synthesis and overall in tissue reparation [7], In 2009, National Pressure Ulcer Advisory Panel introduced general guidelines for the treatment and prevention of pressure ulcers, these were updated in 2014 [8]. For pressure ulcer stage III/ IV, recommended protein intake goes up to 2 g/ kg. The key role of protein intake is well demonstrated in a study presented by Crowe et al [9]. The group receiving higher protein (1.8 g protein per kg body weight) demonstrated nearly a two-fold greater rate of healing than those randomized to lower protein intake (1.2 g protein per kg body weight). The role of carbohydrates, fats and micronutrients is equally important. To prevent protein-energy malnutrition and improve wound healing, the diet should be adequate in energy in the form of carbohydrates, fat and protein. Infection of a pressure ulcer may result in soft tissue and bone infections: cellulitis, abscess formation, bursitis, and osteomyelitis of bone underlying the wound bed [10]. In SCI patients, it is one of the most common causes of bacteremia [11]. Control of wound colonization and infection should always be one of the biggest priorities in treatment protocol [1]. Precise microbiological surveillance should be strictly conducted in all patients, along with targeted antibiotic administration based on sensitivity. This is the only way to prevent an increase in antibiotic resistance and at the same time to successfully eradicate pathogens in an effort to prevent further dissemination [12].
Conclusion
Surgical treatment of pressure ulcers in patients after SCI is often a very complicated process involving many aspects of surgery. Today, correct and effective treatment is possible due to large collaboration in a multidisciplinary team. It is the presence of a diverse range of experts, not only from the surgical field, that has contributed to the development in this often neglected issue.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 30. 6. 2019
Accepted for print: 4. 7. 2019
Alica Hokynková, MD
Department of Burns and Plastic Surgery
University Hospital Brno
Jihlavská 20
625 00, Brno
Czech Republic
e-mail: alicah@post.cz
Zdroje
1. Kruger EA, Pires M, Ngann Y et al. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med 2013; 36(6): 572 – 585. doi: 10.1179/ 2045772313Y.0000000093.
2. Fuhler M, Garber S, Rintala D et al. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil 1993; 74(11): 1172 – 1177.
3. Regan M, Teasell R, Dalton L et al. A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Arch Phys Med Rehabil 2009; 90(2): 213 – 231. doi: 10.1016/ j.apmr.2008.08.212.
4. Rubayi S, Chandrasekhar B. Trunk, abdomen, and pressure sore reconstruction. Plast Reconstr Surg 2011; 128(3): 201e – 215e. doi: 10.1097/ PRS.0b013e31822214c1.
5. Thomson C, Choudry M, White C et al. Multi-disciplinary management of complex pressure sore reconstruction: 5-year review of experience in a spinal injuries centre. Ann R Coll Surg Engl 2017; 99(2): 169 – 174. doi: 10.1308/ rcsann.2016.0227.
6. Sameem M, Au M, Wood T et al. A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg 2012; 130(1): 67e – 77e. doi: 10.1097/ PRS.0b013e318254b19f.
7. Antalová N, Pokorná A, Hokynková A et al. Factors influencing recurrence of the pressure ulcers after plastic surgery – retrospective analysis. Cesk Slov Neurol N 2018; 81/ 114: S23. doi: 10.14735/ amcsnn2018S23.
8. Dunk A, Carville K. The international clinical practice guideline for prevention and treatment of pressure ulcers/ injuries. J Adv Nurs 2016; 72(2): 243 – 244. doi: 10.1111/ jan.12614.
9. Crowe T, Brockbank C. Nutrition therapy in the prevention and treatment of pressure ulcers. Wound Practice 2009; 17(2): 90 – 98.
10. Dana A, Bauman W. Bacteriology of pressure ulcers in individuals with spinal cord injury: what we know and what we should know. J Spinal Cord Med 2015; 38(2): 147 – 160. doi: 10.1179/ 2045772314Y.0000000234.
11. Wall B, Mangold T, Huch K et al. Bacteremia in the chronic spinal cord injury population: risk factors for mortality. J Spinal Cord Med 2003; 26(3): 248 – 253. doi: 10.1080/ 10790268.2003.11753692.
12. Salcido R, Popescu A, Potter A et al. Pressure ulcers and wound care. [online]. Available from URL: http: / / www.emedicine.medscape.com/ article/ 31984-overview.
Štítky
Dětská neurologie Neurochirurgie Neurologie
Článek vyšel v časopiseČeská a slovenská neurologie a neurochirurgie
Nejčtenější tento týden
2019 Číslo Supplementum 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Magnosolv a jeho využití v neurologii
- Zolpidem může mít širší spektrum účinků, než jsme se doposud domnívali, a mnohdy i překvapivé
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- Reconstruction of recurrent ischiadic pressure ulcer using turnover hamstring muscle flap
- The knowledge and practises of nurses in the prevention of medical devices related injuries in intensive care – questionnaire survey
- Effectiveness of comprehensive pain management in hard-to heal ulcers – a protocol of systematic review
- Negative wound pressure therapy in treatment of a pressure ulcer in paraplegics
- The use of negative pressure wound therapy for wound complication management after vascular procedures
- Mapping of pressure ulcers and non-healing wounds in medical curriculum
- Oxidative stress in wound healing – current knowledge
- Quality of life in patient with non-healing wounds
- Pain assessment of surgical wounds after angio-surgical interventions
- Effectiveness of hyperbaric oxygen therapy in non-healing ulcerations – meta-review
- Multidisciplinary approach in surgical pressure ulcer therapy after spinal cord injury
- Hyperbaric oxygen therapy in non-healing ulcerations – mechanisms of action, current european recommendations and case report
- Key factors for the development of pressure ulcers in surgical practice
- Pilot analysis of pressure ulcers – nationwide data from central adverse event reporting system
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Quality of life in patient with non-healing wounds
- The knowledge and practises of nurses in the prevention of medical devices related injuries in intensive care – questionnaire survey
- The use of negative pressure wound therapy for wound complication management after vascular procedures
- Negative wound pressure therapy in treatment of a pressure ulcer in paraplegics
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



