-
Medical journals
- Career
Forefoot Navicular Bone Fractures - Short Communication and Case Report
Authors: Martin Sedlář; Jozef Kraus; Petr Dytrych; Věra Kratochvílová
Authors‘ workplace: I. chirurgická klinika – břišní, hrudní a úrazová chirurgie 1. lékařská fakulta Univerzity Karlovy v Praze a Všeobecná fakultní nemocnice v Praze
Published in: Úraz chir. 26., 2018, č.3
Overview
Fractures of the navicular bone are relatively uncommon injuries to the forefoot, but are accompanied by a high frequency of post-traumatic complications. The authors present a short review of the problem of navicular fractures and demonstrate their own case report of this less common fracture.
Keywords:
Navicular fractures – operative treatment – short term results
Introduction
Fractures of the navicular bone are relatively uncommon injuries to the forefoot, but are accompanied by a high frequency of post-traumatic complications. Common complications include the no-unions, avascular necroses and especially post-traumatic arthrosis leading to limitation of the forefoot mobility [8].
The navicular bone is the basic bone of the medial pillar of the forefoot, and any damage to the talonavicular joint leads to a significant reduction in mobility in all subtallar segments of the foot [1]. It is a part of the Chopart’s joint, which is formed in the tibial part by the talonavicular slit and in the fibular part by the calcaneocuboid joint. Chopart‘s joint is reinforced by longitudinally pathed ligaments. From dorsal part by ligamentum talonaviculare dorsale and lig. bifurcatum, in the plantar direction then by calcaneonavicular and calcaneocuboid ligament.
Movements in the lower metatarsal joint they are combined around the inclined axis of the foot. Around this axis, the tarsus as a whole performs two movements, namely:
- a) foot inversion, which is a combination of plantar flexion with supination and adduction;
- b) foot eversion where dorsal flexion is associated with abduction and pronation.
The vascularization of the navicular bone is limited due to its large cartilage areas, resulting often in avascular necrosis or the joint after a trauma. From the dorsal side, the navicular bone is supplied by the art. dorsalis pedis, in plantar direction then by art. tibialis posterior. The tuberosity area is supplied only by the links of both arteries and represents a site of the most common healing disorder. This is especially true in elderly patients. This area is also vulnerable by repeated stress and a region of stress-induced fractures.
Etiology
Traumatic fractures of navicular bone occur with high-energy axial violence. Falls from a hight, motorcycle accidents, high speed bicycle injuries, falls from a snowboard. It is the body of the bone that is usually affected by these accidents. In violent plantar flexion, the force is transferred to the m. tibialis posterior tendon and the avulsion fractures occur. Violent eversion causes the navicular bone tuberosity fractures.
Stress-induced fractures occur in the case of chronically repetitive minor loads, in long-distance runners, basketball players and surprisingly dancers.
Classification
Acute navicular bonde fractures are divided into 3 types:
- Avulsion fractures
- Tuberosity fractures
- Fractures of the body
Body fractures are classified based on the direction of the fracture line, the degree of comminution and the dislocation of fragments according to DeLee [1].
1. DeLee’s Navicular Bone Fractures (Source. Moore Derek. Tarsal navicular Fractures: https://www.orthobullets.com/foot-and-ankle/7033/ tarsal-navicular-fractures) 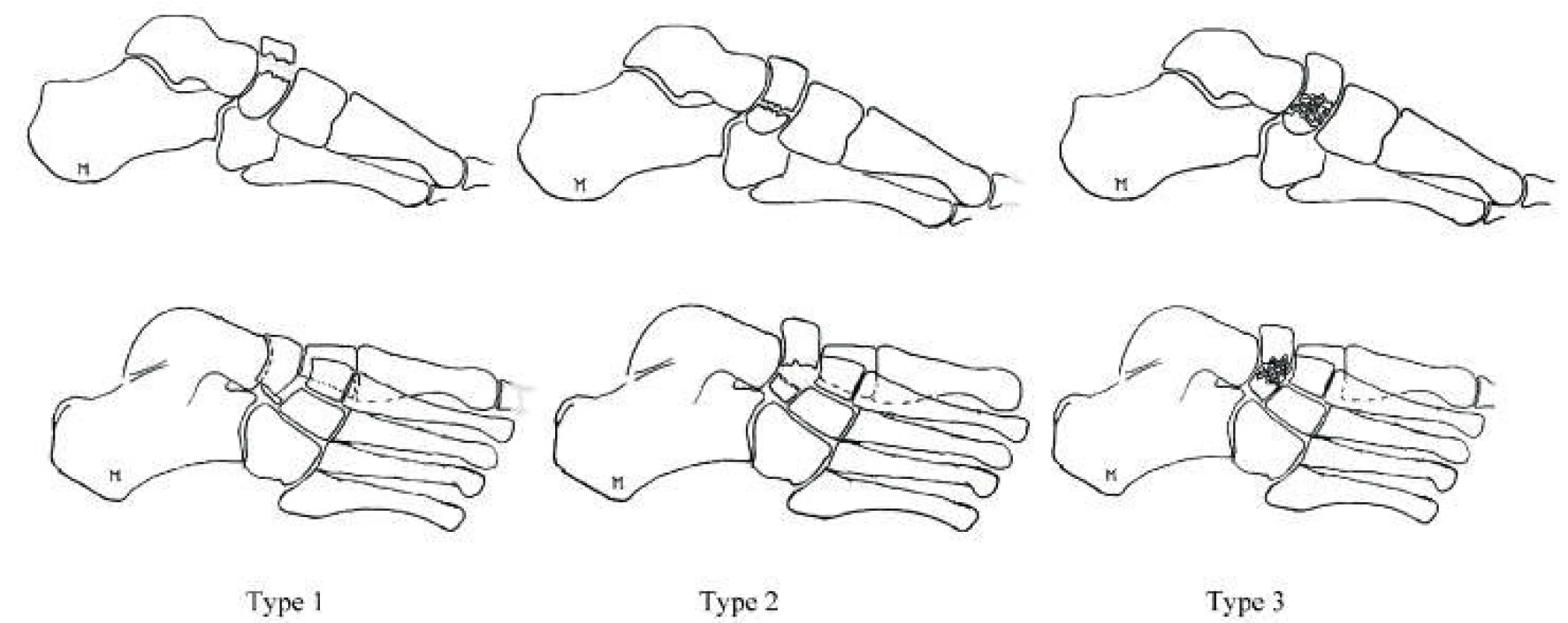
Diagnostics
The usual clinical manifestations of fracture include pain, swelling, limitation of locomotion. Due to the solid fibrous bed, at this localization, compartment syndrome may develop. However, symptoms of stress-induced fracture may be limited only to mild discomfort in the forefoot, with no concomitant clinical signs. They should be considered in the indication of paraclinical examinations, when even native X-ray in the early phase may not detect a fracture.
Selecting from the imaging methods, we typically indicate an anteroposterior, lateral, and oblique X-ray images, and a comparative image with suspected avulsion, and in the case of a growing skeleton. The comparative image can also identify accessory navicular bone occurring bilaterally. CT examination, including 3D reconstructions, is primarily suitable in high-energy injuries, where we expect associated injuries of the forefoot and when a stress-induced fracture is suspected. MRI is also justified in stress-induced fractures and in associated ligament injuries, particularly for damage to the musculus tibialis posterior tendon. This examination also reliably identifies the accessory os naviculare.
Arthroscopy as a diagnostic and therapeutic method is used to visualize the damage and repair of the involvement of the tendon of musculus tibialis posterior.
Treatment
The strategy of treating navicular bone fractures depends on many factors. It derives from the condition of soft tissues, fracture type, the presence of other injuries and the general condition of the patient. Conservative treatment is reserved for avulsion fractures with a small, little dislocated fragment (3 mm tolerance) and for stress-induced fractures. The treatment consists in gypsum immobilization under the knee or walker boot orthosis, stick support, load-free limb locomotion for 6 to 8 weeks. A series of X-ray checks, analgesia, and prevention of thromboembolic disease are required.
Surgical treatment is preferred for dislocated fractures of the bone body, intraarticular fractures with articular surface incongruity [2, 5, 7, 9]. The treatment consists in extirpation of free fragments, in avulsion fractures with a fragment of up to 2 mm or open reposition and osteosynthesis by Kirschner wires, screws or miniature plates [3] with reconstruction of the medial pillar of the forefoot. According to the region of the fracture, dorsomedial or dorsolateral approach is chosen. The external fixateur is the method of choice to maintain the median pillar length, in polytrauma, developed compartment syndrome combined with the fasciotomy [4] and as the first step of phase surgery in complex injuries. In addition to the nature of the fracture, the overall condition of the patient and possible factors affecting healing, such as diabetes mellitus, soft tissue trophics in chronic venous insufficiency, anticipated angiopathy in strong smokers, quality of locomotion before injury and patient compliance during postoperative period, etc., should be taken into account in the indication of surgical treatment.
Postoperative complications have to be anticipated in both treatment strategies. These include limited locomotion, algic forefoot syndrome, post-traumatic arthrosis, avascular necrosis, or non-union.
Arthrodesis is indicated in case of progressive algic syndrome in bone healing disorders and progression of post-traumatic arthrosis [2, 8].
Case reports
A 27-year-old man, without compromising comorbidities, a physically hard-working individual was admitted to our clinic 24 hours upon falling down the stairs. The mechanism of injury was a violent plantar flexion with a type III luxation fracture.
Soft tissues were not compromised, compartement syndrome was not present. The extremity was with mild edema, not presenting any neurovascular deficit. Initially, standard X-ray projections were performed, followed by CT examination with 3D reconstructions on their basis. With regard to the good condition of soft tissues and minimum swelling, an urgent open reposition and osteosynthesis were indicated. The surgery was performed within 2 hours of admission.
From the anteromedial approach, without the use of turnstile, open reposition, osteosynthesis by Kirschner wires with reconstruction of the medial pillar, adaptation suture of talonavicular ligament was performed and supplemented by fasciotomy as prevention of development of the compartment syndrome. Osteosynthesis with a minimum of metallic material was chosen on the assumption of soft tissue healing failure and good stability following reposition.
Peroperatively and postoperatively administered antibiotics – vulmizoline in the preventive protocol, fraxiparin in the dose related to the weight of the patient administered throughout the fixation, single-dose administration of dexona peroperatively. The wound healed per primam. A limb-free walker boot was applied for 6 weeks, then rehabilitation for 2 weeks, which was terminated at the patient‘s request. The patient was financially motivated and after 8 weeks ended treatment and sick leave.
2. Post-injury input X-ray image (Source: Sedlář Archive) 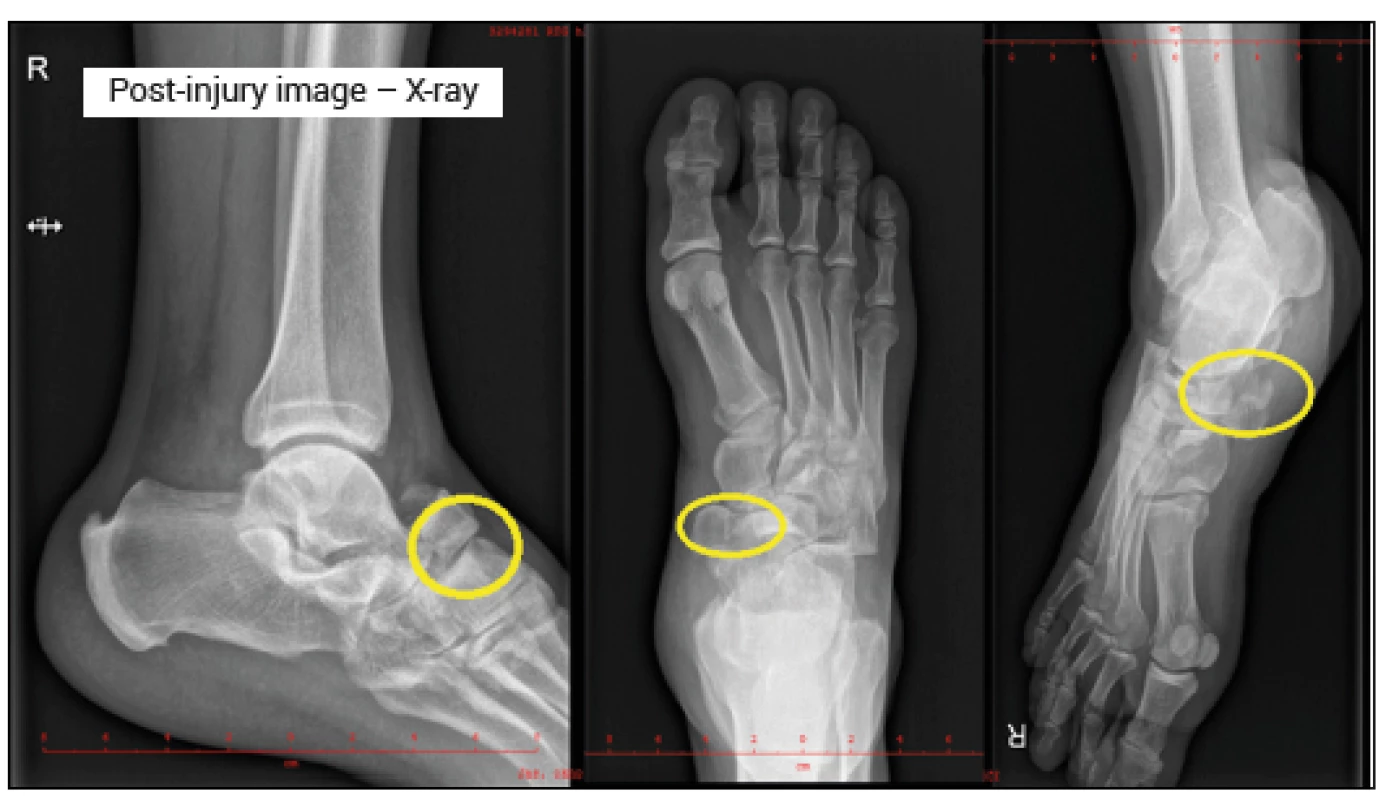
3. Completed CT with reconstruction (Sedlář Archive) 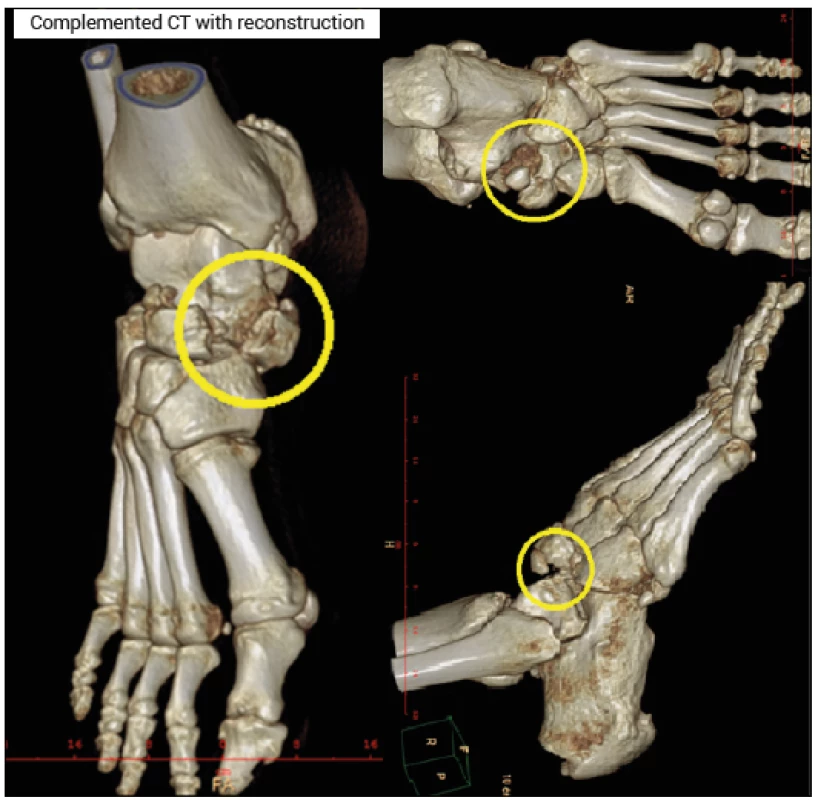
Resultant condition
Functionally: a good gait stereotype (video by the author), despite the limitation of sub-talo locomotion of a minor degree of severity - plantar flexion - 10 degrees, extension - 15 degrees, pronosupination - 15 degrees. The patient returned to the profession of the construction worker and refused the proposed extraction of metallic material. In the last X-ray check, the fracture was consolidated, the metallic material in situ, with no signs of development of aseptic necrosis in this early period.
4. Post-surgery X-ray Images (Sedlář Archive) 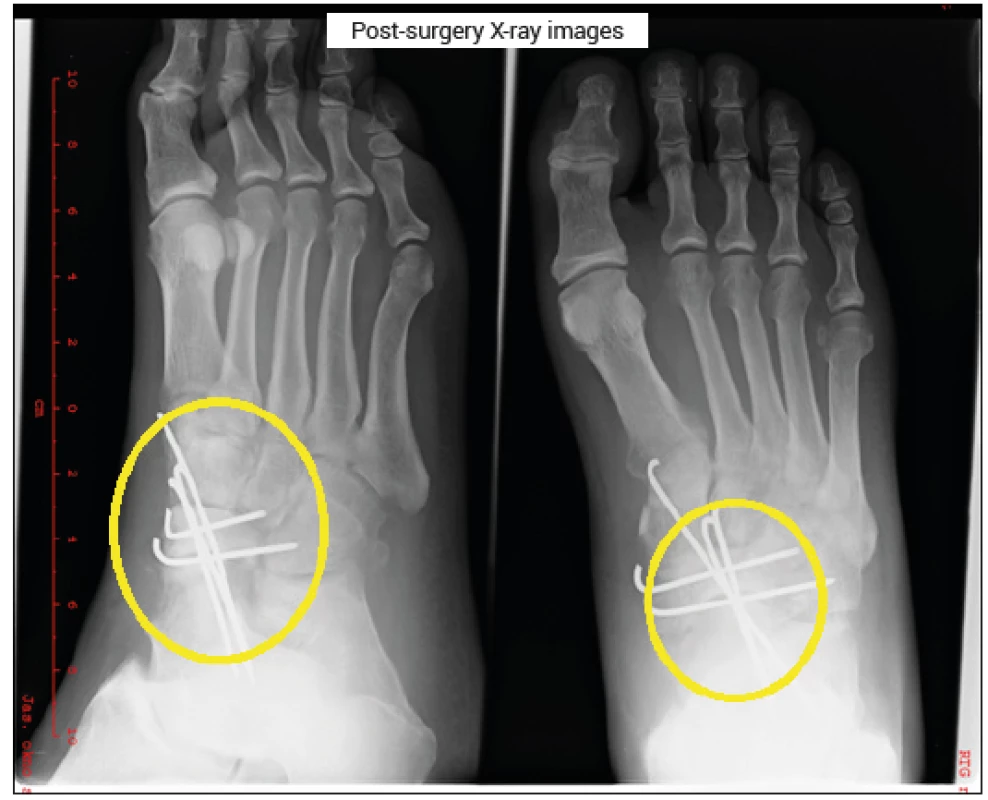
The patient did not attend to further follow-up checks, according to the information provided by his wife, who is an employee of our hospital, he continues to work as a construction worker.
Discussion
Isolated dislocated navicular bone fractures of the forefoot are not frequent injuries and the results of their treatment are not optimal according to literature [8]. Despite the relatively low incidence of this type of injury encountered by traumatic surgeons, and, according to our experience, also scarce literary data, an immediate stabilization is necessary either within the external phase fixator procedure or the primary definite osteosynthesis by optimal prevention of soft-tissue complications, compartment syndrome and post-trauma arthrosis. The requirement for reconstruction of the articular surface and restoration of the stability of the medial pillar during definitive synthesis is crucial for the function of the foot. Indications of surgical treatment are given by the nature of the fracture [2, 5, 7, 9], condition of the soft tissue, comorbidities and estimated patient compliance. The patient must be informed of the limits of treatment and in case of occurrence of a non-union or progression of post-traumatic arthrosis with algic syndrome arthrodesis is indicated. Another reported complication – post-traumatic necrosis of the navicular bone with collapsed central pillar is also an indication for replacement of the navicular bone by autologous graft and arthrodesis. Infectious complications are described more frequently in plate osteosynthesis [3]. When Kirschner wires are used, their migration occurs and synthesis fails; in the case of percutaneous insertion, pin infection develops.
Conclusion
Fractures of the navicular bone are not a common injury to the locomotor system and the knowledge of the management of these fractures allow the trauma surgeon to select optimum reatment and minimize post-traumatic complications [6]. A research of injuries to the forefoot at the interval of the past 10 years at our clinic is being prepared by the authors.
LIST OF ABBREVIATIONS AND ACRONYMS
CT computed tomography
LIG. ligamentum
MRI magnetic resonance imaging
p.p.i. proton-pump-inhibitors
RTG X-ray
TEN thromboembolic disorder
tib. tibialis
MUDr. Martin Sedlář, Ph.D.
Sources
- ČIHÁK, R. Anatomie 1, 2. vyd. Praha : Avicenum, 2011. 552 s. ISBN 978-80-247-3817-8.
- DiGiovanni, CW. Fractures of the navicular. Foot Ankle Clin. 2004, 9, 25–63. ISSN 1558-1934
- Evans, J., Beingessner, DM., Agel, J. et al. Minifragment plate fixation of high-energy navicular body fractures. Foot Ankle Int. 2011, 32, 485–492. ISSN 1558-1934
- Koslowsky, TC., Mader, K., Siedek. M. et al. Minimal invasive treatment of a comminuted os naviculare body fracture using external fixation with limited open approach. J Trauma. 2008, 65, 58–61. ISSN 2163-0763
- MOORE, D. Tarsal Navicular Fractures. Orthobullets. [cit. 2018-07-02]. https://www.orthobullets.com/foot-and-ankle/7033/tarsal-navicular-fractures. ISSN 1526-3231
- Penner, MJ. Late reconstruction after navicular fracture. Foot Ankle Clin. 2006, 11, 105–119. ISSN 1558-1934
- Ramadorai, MU., Beuchel, MW., Sangeorzan, BJ. Fractures and Dislocations of the Tarsal Navicular. J Am Acad Orthop Surg. 2016, 24, 379–389. ISSN 1067-151X
- Rosenbaum, AJ., DiPreta, JA., Tartaglione, J. et al. Acute Fractures of the Tarsal Navicular: A Critical Analysis Review. JBJS Rev. 2015, 31, 1–7. ISSN 2329-9185
- Schmid, T., Krause, F., Gebel, P. et al. Operative Treatment of Acute Fractures of the Tarsal Navicular Body: Midterm Results With a New Classification. Foot Ankle
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2018 Issue 3-
All articles in this issue
- Current approach to the management of forearm and elbow dislocation in children
- Medial malleolar fractures
- Examples of use of outpatient negative pressure therapy in chronic wound healing – a set of case reports
- Forefoot Navicular Bone Fractures - Short Communication and Case Report
- Assessment of the injuring effect of loose objects in a vehicle in a traffic accident
- Effect of earlier load on healing of calcaneus fractures after stable osteosynthesis
- Trauma Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Current approach to the management of forearm and elbow dislocation in children
- Forefoot Navicular Bone Fractures - Short Communication and Case Report
- Effect of earlier load on healing of calcaneus fractures after stable osteosynthesis
- Examples of use of outpatient negative pressure therapy in chronic wound healing – a set of case reports
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

