-
Medical journals
- Career
EARLY DISCHARGE (48–72 HOURS) AFTER ACUTE ST-SEGMENT ELEVATION MYOCARDIAL INFARCTION: INTERIM RESULTS OF THE OPEN, RANDOMIZED, MONOCENTRIC STUDY
Authors: Kamil Novobílský; Radim Kryza; Petr Černý; Ivo Horák; Vladimír Kaučák; Jan Mrózek; Roman Štípal
Authors‘ workplace: Department of Cardiology, Municipal Hospital Ostrava, Czech Republic
Published in: Lékař a technika - Clinician and Technology No. 2, 2016, 46, 55-60
Category: Original research
Overview
Authors present the interim analysis of open, prospective, randomized study, comparing the strategy of early (48–72 hours) and standard (after 72 hours) discharge in low risk patients after myocardial infarction with ST-segment elevation (STEMI), treated with successful primary percutaneous coronary intervention (PCI).
91 patients (22. 5% of all STEMI patients admitted within the period between October 15, 2013 and October 6, 2015), who fulfilled given inclusion criteria of low risk, were randomly assigned to two groups in a 1 : 1 ratio.
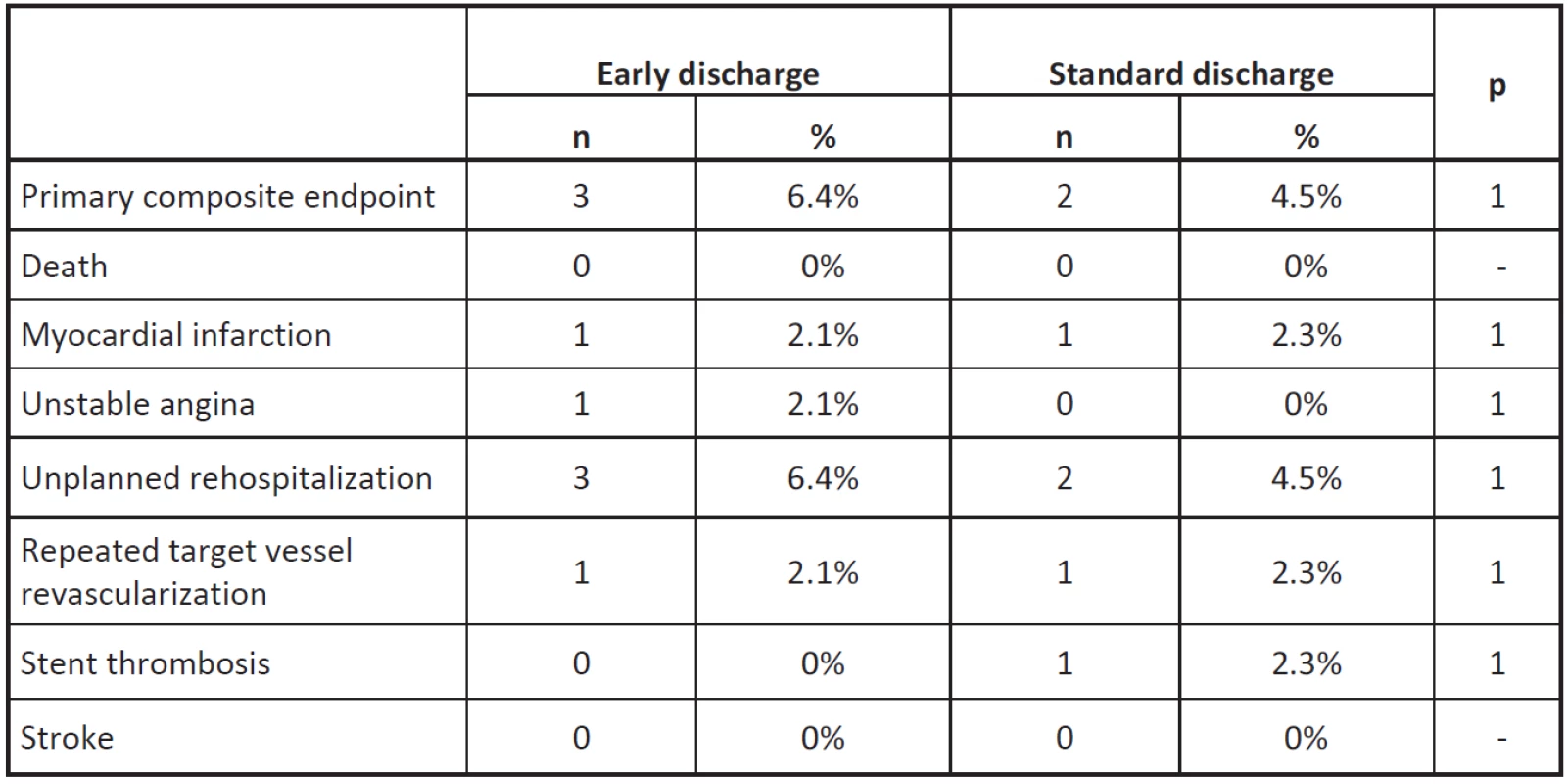
The primary end point was the composite of death, myocardial infarction (MI), unstable angina, stroke, unplanned rehospitalization, repeated target vessel revascularization, stent thrombosis within 90-day follow-up.
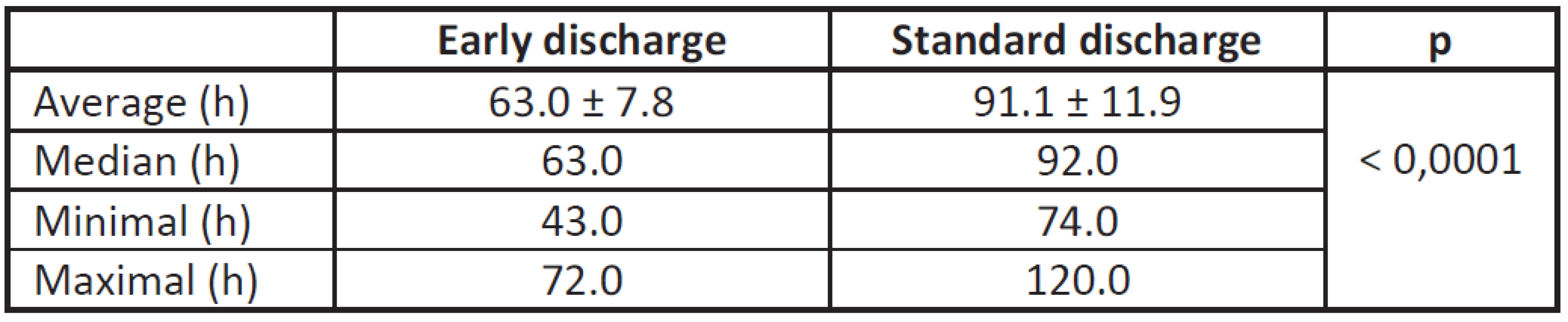
The length of stay was significantly shorter in the intervention group (63.0 ± 7.8 h vs. 91.1 ± 11.9 h, p < 0.0001).
The primary end point at 3 months occurred in 3 patients assigned to intervention group as compared to 2 patients assigned to control group (6.4% vs. 4.5%, p = 1.0 for non-inferiority). There were no significant differences in the incidence rates of individual components of the primary end point at 90 days.
Presented interim data of the study support the claim that early discharge (48–72 hours) in selected patients after STEMI, treated with successful primary PCI, is possible and safe, with the results comparable to the later discharge, realized in compliance with current guidelines and present everyday clinical practice.Keywords:
myocardial infarction with ST-segment elevation, primary percutaneous coronary intervention, low risk, early discharge, feasibility, safetyIntroduction
The length of hospital stay in patients with diagnosis of myocardial infarction with ST-segment elevation, has been shortened substantially within past 50 years [1]. Reduction of health cost associated with this strategy was proven also [2–4].
The current Guidelines of European Society of Cardiology, released in 2012, state, that in the selected patients after myocardial infarction with ST-segment elevation, the early discharge (after approximately 72 h) may be considered (class of recommendation IIb, level of evidence B), if adequate follow-up is arranged [5]. The data reflecting such an approach in clinical practice are limited.
Our first experience with the strategy of length of hospital stay shorter than current guidelines recom-mend, was described previously [6].
The aim of this study is to prove that early discharge (within 72 hours) in patients with low risk of follow-up complications after STEMI, treated with primary PCI, is feasible and safe, and that early discharge is "non-inferior" in comparison with the group of patients discharged in a standard way, accordingly with present, local practice and physician´s decision (usually 4th - 7th day), thus it is not associated with higher incidence of complications in the 90th day after myocardial infarction. (ClinicalTrials.gov – identifier NCT02023983).
Methods
This is the interim analysis of prospectively designed, open, randomized, monocentric study of patients with STEMI, treated with successful primary PCI.
Inclusion criteria, defining the eligibility of subjects for enrollment to the study, are listed in Table 1, plan of the study is shown in the Figure 1. Patients with comorbidities, requiring additional evaluation within primary hospitalization, were excluded. The par-ticipants were randomly assigned to two groups in a 1 : 1 ratio.
The primary end point is the composite of death, myocardial infarction, unstable angina, stroke, unplan-ned rehospitalization, repeated target vessel revas-cularization and stent thrombosis within 90‑day follow-up.
No patient was transported back to referring hospital; the stress test before discharge was not routinely performed. Clinical control of patients, randomized to intervention group, was performed in outpatient clinic no later than 4 days after discharge. All patients, involved in analysis, completed 90-day follow-up.
1. Inclusion criteria. 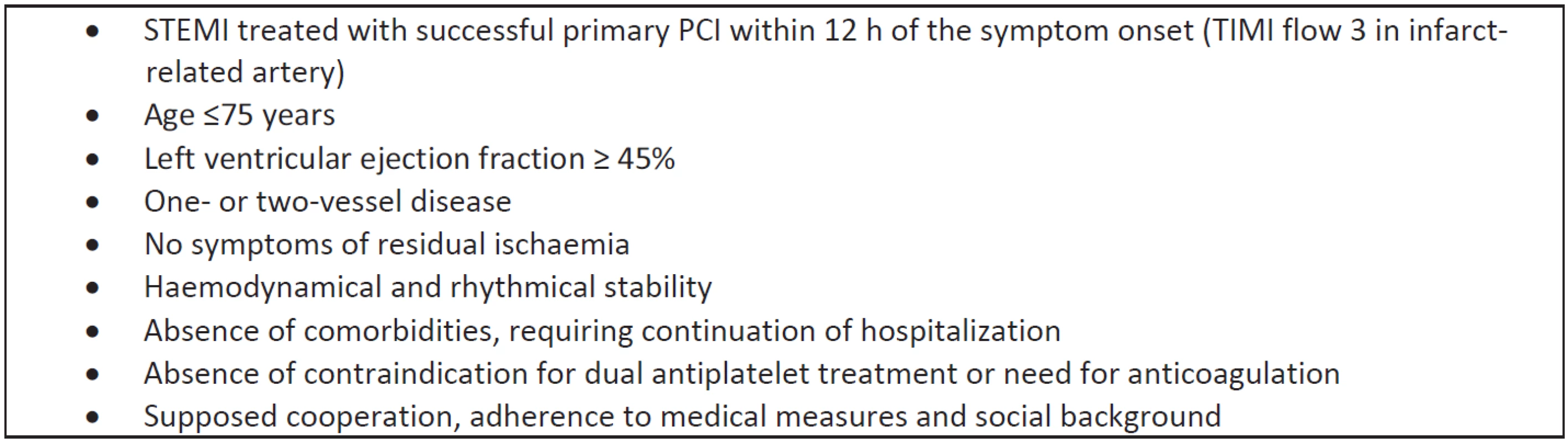
TIMI - thrombolysis in myocardial infarction. Statistical analysis
Statistical analysis was performed with SPSS Statistics software package, version 22 (IBM Corporation, Armonk, NY, USA). For comparison of qualitative variables between two groups Fischer’s exact test was used. For comparison of quantitative variables we used Student’s t-test (age, BMI), respectively Mann-Whitney U test (length of stay, left ventricular ejection fraction). Normality of data was assessed with Shapiro-Wilk test. Values of p < 0.05 were considered as statistically significant.
Results
409 consecutive patients with diagnosis of STEMI, treated with primary PCI, were admitted to our center within the period between October 15, 2013 and October 6, 2015.
91 (22.5%) of them fulfilled inclusion criteria, were recruited for study and randomized to two groups. Their baseline characteristics are shown in Table 2, except body-mass index the both cohorts were similar.
2. Baseline clinical characteristics of the analyzed cohorts. 
TIA – transient ischemic attack, GP IIbIIIa inhibitors - glycoprotein IIbIIIa inhibitors, EF – ejection fraction Inferior localization of MI clearly dominated. Radial approach as well as the use of drug eluting stents were preferred, aspiration thrombectomy was used in less than half of cases, glycoprotein IIbIIIa inhibitors were administrated in 17% and 4.5% respectively.
The length of stay was significantly (p < 0.0001) shorter in the intervention group (Tab. 3, Fig 2).
Fig 2: Quartile box chart – distribution of length of stay in compared groups. 
The primary end point at 3 months occurred in 3 patients assigned to intervention group as com-pared to 2 patients assigned to control group (6.4% vs. 4.5%, p = 1.0 for non-inferiority).
There were no significant differences in the incidence rates of individual components of the primary end point at 90 days between the group with early discharge and control cohort.
Neither death nor stroke occurred in either group in this period.
Discussion
Numerous references to the issue of early discharge after STEMI are available, but their overview indicates that methodology of these works widely varies (3–63% of probands fulfilled criteria for early discharge!).
At present, the low risk STEMI population is relatively well defined [7–11]. Several risk scores were created to identify the patients with low risk of subsequent complications [9–11]. De Luca et al. in their study developed practical score (Zwolle Risk Score for STEMI) for risk stratification in low risk patients with STEMI, treated with primary PCI [9]. Age, anterior infarction, Killip class, ischemic time, postprocedural TIMI flow in infarct-related artery and multi-vessel disease were defined as independent predictors of 30-day mortality. Score ≤3 designates low-risk patients.
Current guidelines for early discharge are based just on limited data derived from randomized trials.
In the small, pilot SAFE-DEPART study, Kotowycz et al. randomized 54 low risk patients with STEMI (Zwolle score ≤3), treated with primary (or rescue) PCI, to the early discharge (48–72 h) or discharge at the discretion of treating physician (control group) [12]. The primary outcomes of this study were to demonstrate feasibility and safety of such an approach. In the intervention group 74% of patients were discharged within 72 h, length of stay in hospital was short in all study patients (median 55 h). No death occurred in either group and no significant difference in the rate of rehospitalization between both groups was observed. There were no significant differences in compliance, quality of life or smoking cessation.
Noman et al. in retrospective analysis collected data of 2448 STEMI patients treated with primary PCI and surviving to hospital discharge [13]. Patients with TIMI 3 flow in infarct-related artery and without haemodynamic or arrhythmic comp-lications were considered for early discharge at the discretion of the attending physician: a total of 1542 patients (63%) were discharged within 2 days of admission (early discharge group) and remaining 37% after 2 days (late discharge). The 30-day post-discharge mortality rate was 0.71% in the early group and 1.66% in the late group. During a mean follow-up of 584 days, mortality was 4.3% and 12.3% respectively. The authors conclude that in unselected cohort of consecutive ‘‘real-world’’ STEMI patients those with low risk of subsequent complications (almost two thirds!) can be safely discharged within 2 days following primary PCI.
Recently, Azzalini et al. in EDAMI trial [14] in the cohort of 100 low-risk (Zwolle risk score ≤ 3) patients with STEMI compared the group with early discharge (≤ 72 hours) and the group with a conventional discharge strategy. The primary end point was defined as following: the feasibility of the early discharge strategy (EDS): (1) ≥ 70% of EDS patients discharged ≤ 72 h, (2) ≥ 70% visited by a nurse ≤ 7 days after discharge, (3) ≥ 70% with ≥ 3 visits by the nurse and (4) ≥ 70% visited by a cardiologist ≤ 3 months. Length of stay was shorter in early discharge strategy (70.1 vs. 111.8 h, p < 0.001). Early discharge feasibility was: (1) 72.2%; (2) 81.5%; (3) 76.9%; (4) 72.2%. No adverse events or differences in intervention goals and quality of life were registered between groups.
Our interim analysis indicates, that early dis-charge after STEMI, treated with primary PCI is feasible and safe, without higher risk of subsequent complications. It is fair to add, that the shorter hospital stay is associated with limited time for proper patient rehabilitation, education or titration of medication. It is therefore entirely appropriate to carry out early clinical post-discharge control and arrange subsequent regular care. In accordance with Azzalini et al. we consider reasonable the discharge not earlier than after 48 hours.
Conclusions
Presented interim data of the monocentric, open, randomized study support the claim that early discharge (48–72 hours) in selected, low risk patients after STEMI, treated with successful primary PCI, is possible and safe, with the results comparable to the later discharge, realized in compliance with current guidelines and present everyday clinical practice. According to this analysis, this strategy applies to at least 22.5% of all STEMI patients. Final results of the trial will be available in 2017.
Acknowledgement
The authors declare that there are no known conflicts of interest associated with the publication of the article, there has been no financial support for the work on the article and all the work was do-ne in accordance with the ethical standards. Hereby we kindly thank Mgr. Jana Zapletalová, Dr., Department of Medical Biophysics, Faculty of Medicine and Dentistry, Palacky University Olomouc, for her help with statistical analysis.
Kamil Novobílský
Kardiologie
Městská nemocnice Ostrava
Nemocniční 20
728 80 Ostrava 1
E-mail: k.novobilsky@mnof.cz
Phone: +420 59 619 4279
Sources
Berger, A.K., Duval, S., Jacobs Jr., D.R., et al. Relation of length of hospital stay in acute myocardial infarction to post-discharge mortality. American Journal of Cardiology, 2008, vol. 101, p. 428–434.
[2] Topol, E.J., Burek, K., O'Neill, W.W., et al. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. New England Journal of Medicine, 1988, vol. 318, p. 1083–1088.
[3] Newby, L.K., Eisenstein, E.J., Califf, R.M., et al. Cost effectiveness of early discharge after uncomplicated acute myocardial infarction, New England Journal of Medicine, 2000, vol. 342, p. 749–755.
[4] Grines, C.L., Marsalese D.L., Brodie, B., et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. PAMI-II Investigators. Primary Angioplasty in Myocardial Infarction, Journal of the American College of Cardiology, 1998, vol. 31, p. 967–972.
[5] Steg, P.G., S.K. James, S.K., D. Atar, D., et al. Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology, European Heart Journal, 2012, vol. 33, p. 2569–2619.
[6] Novobílský, K., Kryza. R., Černý, P., et al. Early discharge (within 72 h) in low risk patients after acute ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. Single centre experience, Cor et Vasa, 2015, vol. 57, p. e45–e49.
[7] Newby, L.K., Califf, R.M., Guerci, A., et al. Early discharge in the thrombolytic era: an analysis of criteria for uncomplicated infarction from the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO) trial, Journal of the American College of Cardiology, 1996, vol. 27, p. 625–632.
[8] van der Vugt, M.J., Boersma, H., Leenders, C.M., et al. Prospective study of early discharge after acute myocardial infarction (SHORT), European Heart Journal, 2000, vol. 21, p. 992–999.
[9] Addala, S., Grines, S.L., Dixon, S.R., et al. Predicting mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention (PAMI Risk Score), American Journal of Cardiology, 2004, vol. 93, p. 629–632.
[10] De Luca, G., H. Suryapranata, H., A.W. van't Hof, A.W., et al. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: implications for early discharge, Circulation, 2004, vol. 109, p. 2737–2743.
[11] Halkin, A., Singh, M., Nikolsky, E., et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score, Journal of the American College of Cardiology, 2005, vol. 45, p. 1397–1405.
[12] Kotowycz, M.A., Cosman, T.L., Tartaglia, C., et al. Safety and feasibility of early hospital discharge in ST-segment elevation myocardial infarction – a prospective and randomized trial in low-risk primary percutaneous coronary intervention patients (the Safe-Depart Trial), American Heart Journal, 2010, vol. 159, p. 117.e1–117.e6.
[13] Noman, A., Zaman, A.G., Schechter, C., et al. Early discharge after primary percutaneous coronary intervene-tion for ST-elevation myocardial infarction, European Heart Journal: Acute Cardiovascular Care, 2013, vol. 2, p. 262–269.
[14] Azzalini, L., Solé, E., Sans, J., et al. Feasibility and Safety of an Early Discharge Strategy after Low-Risk Acute Myocardial Infarction Treated with Primary Percutaneous Coronary Intervention: The EDAMI Pilot Trial, Cardiology, 2015, vol. 130, p. 120–129.
Labels
Biomedicine
Article was published inThe Clinician and Technology Journal

2016 Issue 2-
All articles in this issue
- CROSSOVER FROM AUTOMATED TO MANUAL TITRATION OF FiO2 IN THE NICU: IS THERE A TRANSITION LAG?
- DESIGN CONCEPTS FOR PREVENTING GAS BUBBLE INTERFERENCE IN MICROFLUIDIC DEVICES
- CELL-BASED SENSOR CHIP FOR NEUROTOXICITY MEASUREMENTS IN DRINKING WATER
- TESTING A SYSTEM FOR PREDICTING MICROSLEEP
- EARLY DISCHARGE (48–72 HOURS) AFTER ACUTE ST-SEGMENT ELEVATION MYOCARDIAL INFARCTION: INTERIM RESULTS OF THE OPEN, RANDOMIZED, MONOCENTRIC STUDY
- The Clinician and Technology Journal
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- EARLY DISCHARGE (48–72 HOURS) AFTER ACUTE ST-SEGMENT ELEVATION MYOCARDIAL INFARCTION: INTERIM RESULTS OF THE OPEN, RANDOMIZED, MONOCENTRIC STUDY
- CELL-BASED SENSOR CHIP FOR NEUROTOXICITY MEASUREMENTS IN DRINKING WATER
- TESTING A SYSTEM FOR PREDICTING MICROSLEEP
- DESIGN CONCEPTS FOR PREVENTING GAS BUBBLE INTERFERENCE IN MICROFLUIDIC DEVICES
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career