-
Medical journals
- Career
BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
Authors: V. Radošová; I. Krejčířová; R. Autrata; B. Žajdlíková
Authors‘ workplace: Dětská oční klinika, Lékařská fakulta Masarykovy univerzity a Fakultní nemocnice Brno, Přednosta: prof. MUDr. Rudolf Autrata, CSc., MBA
Published in: Čes. a slov. Oftal., 75, 2019, No. 2, p. 86-90
Category: Case Report
doi: https://doi.org/10.31348/2019/2/5Overview
An optic disc pit is a rare congenital anomaly of the optic nerve disc. It occurs rarely, and in case of its bilateral occurance, it can be caused by an autosomal dominant inheritance pattern. Ophthalmoscopically, the disc pit appears as an ovoid depression of the optic nerve disc. When identified unilaterally, the optic nerve disc is usually larger than the disc of the other healthy eye. Optic disc pits can be located anywhere in optic disc. Moreover, when located in the temporal margin, they can be accompanied by a maculopathy. The latest therapeutic possibilities include the retinal laser photocoagulation and pars plana vitrectomy, however the prognosis quoad visum neverthelles remains poor.
This report deals with bilateral occurance of the optic disc pit in case of 9-year-old asymptomatic patient. The patient had been transferred to our ophthalmology department with suspected retinal detachment. Following the examination, the optic disc pit was diagnosed. The patient remains subject to further observation, however, owing to his current satisfactory vision without the need for a surgical intervention.
Keywords:
optic disc pit – congenital anomaly – maculopathy
INTRODUCTION
Optic disc pit (ODP) is a congenital anomaly of the optic nerve, first described at the end of the 19th century [12]. The pathogenesis is unclear, some sources consider this anomaly a variant of colobomas of the optic nerve [3]. Histologically it concerns herniation of dysplastic retinal tissue into the disc of the optic nerve via the lamina cribrosa, through into the subarachnoid space. This produces an anomaly of communication between the intraocular and extraocular area [11].
The condition occurs with an incidence of 1 : 11 000, without preference for either sex [7]. Typically the affliction is unilateral with sporadic occurrence, in 10-15% of cases it occurs bilaterally, and in these cases may concern autosomal dominant type of heredity [7, 13]. It has a characteristic appearance of oval depression of the optic disc, the affected disc is usually larger [2], the colour mostly whitish-grey, but may also be yellow and black. It is most often localised inferotemporally, though localisation is possible also centrally in the place of excavation of the optic nerve, or anywhere within the region of the disc of the optic nerve (DON) [13]. In more than half of all cases, optic nerve pit has an associated cilioretinal artery outgoing from its base [2].
ODP is usually asymptomatic, and is generally diagnosed by chance. However, a complication may be maculopathy, with associated deterioration of vision. Maculopathy occurs in 25-75% of patients with congenital anomaly of the disc with temporal localisation. It is usually manifested in the third and fourth decade of life, but incidence has also been described in childhood age [3]. In the case of occurrence in childhood, spontaneous regression takes place in 25% of cases, probably because of the difference in vitreopapillary traction in comparison with the adult population [2]. However, with regard to visual acuity (VA) the majority of affected patients have a poor prognosis, with a progressive deterioration of best corrected visual acuity (BCVA) [2].
The precise pathogenesis of maculopathy remains unclear, and opinions on the origin of the intra-retinal and sub-retinal fluid differ. The potential sources considered are the vitreal fluid, cerebrospinal fluid, seepage from capillaries from the base of the pit and from the orbital fascia, surrounded by the dura [2, 5, 14, 15]. Maculopathy has the character of retinoschisis, with presence of macular edema, sometimes with progression to cystoid degeneration, and in 25% of patients macular hole and retinal detachment may develop [1].
Diagnosis of ODP incorporates standard ophthalmoscopic examination, in perimetric examination of the visual field we find an expansion of the blind spot and relative central scotoma. In the precise characterisation of changes on the retina, an irreplaceable role is played by optical coherence tomography (OCT) [4]. Also worthy of mention is electroretinographic examination (ERG) in the diagnosis and observation of changes in patients with associated maculopathy. Svěrák et al. recorded a significant reduction in the amplitudes of oscillation potentials, and a reduction of the potentials of b wave in standard reactions, and also recorded a correlation between the decrease of amplitude and the age of the patients, or the duration of the pathology [19].
In the past, therapy incorporated conservative treatment with a debatable effect, while the current standard of treatment is laser coagulation and pars plana vitrectomy with gas tamponade [4]. In the case of laser coagulation the success rate is only 50%, which is also due to the impossibility of closing the formed cavity by laser upon retinoschisis [2]. Upon progression of the pathology and transition into the stage of chronicity however, the prognosis is unfavourable and the options for therapy limited.
CASE REPORT
The subject of the case report is a 9-year-old boy, who was observed by the district ophthalmologist for almost one year due to low myopia and astigmatism. A regular check-up in August 2018 by chance detected suspect bilateral retinal detachment by ophthalmoscopy. The patient was referred for a specialist examination and proposal of a further procedure at the Children’s Ophthalmology Clinic at the University Hospital in Brno.
Subjectively the patient was without complaints, the personal history without any remarkable features, the parents negated any injury or infection, and the patient did not regularly use any medications. VA with own correction was unimpaired (RE s -1.25 dsf 4/4; LE s -0.50 ax 70 4/4). Intraocular pressure was within the norm (RE 16, LE 14 mmHg). Objective position of the eyeballs was parallel, motility without restriction, finding on the anterior segment biomicroscopically physiological. In artificial mydriasis opththamoscopically there dominated a finding on the papillas of the optic nerve – a bilaterally oval yellowish depression, with its maximum temporally (fig. 1, 2), in the right eye a depression reaching into the nasal region of the disc of the optic nerve. On the right eye the central landscape was intact, in the left eye on the edge of the papilla superotemporally connected extensive area of elevation of neuroretina, reaching into the region of the macula, the other finding up to the periphery of the retina was without a further pathological finding. Examination with the aid of the Amsler grid bilaterally without metamorphopsia. For a more detailed examination, spectral HD-OCT (Zeiss Cirrus) was performed. On linear vertical and horizontal transpapillary scans we observed a finding of bilateral deep ODP covered with hyperreflective tissue (fig. 3, 4). In the right eye nasally peripapillary image of schisis-like retinopathy, with separation of internal and central retinal layers. On the linear horizontal trans-foveolar scan of the right eye the macula was with physiological contours of the inner as well as outer layers of retina. In the left eye on linear horizontal trans-retinal scans superotemporally from the papilla there was apparent high serous ablation of the neuroretina of more than 800 µm, with accumulation of fluid sub-retinally, to a lesser degree there was also evident accumulation of fluid intra-retinally (fig. 5). A linear horizontal transfoveolar scan on the left eye documented an image of low schisis-like maculopathy with separation in the region of the central retinal layers (fig. 6), the outer retinal layers appeared without change of linearity or continuity.
1. Photograph of fundus of right eye, ODP 
2. Photograph of fundus of left eye, ODP with serous ablation of neuroretina superotemporally 
3. HD-OCT: Linear horizontal transpapillary scan of right eye, extensive ODP covered by hyperreflective tissue. Nasally image of schisis-like retinopathy, with separation of individual retinal layers 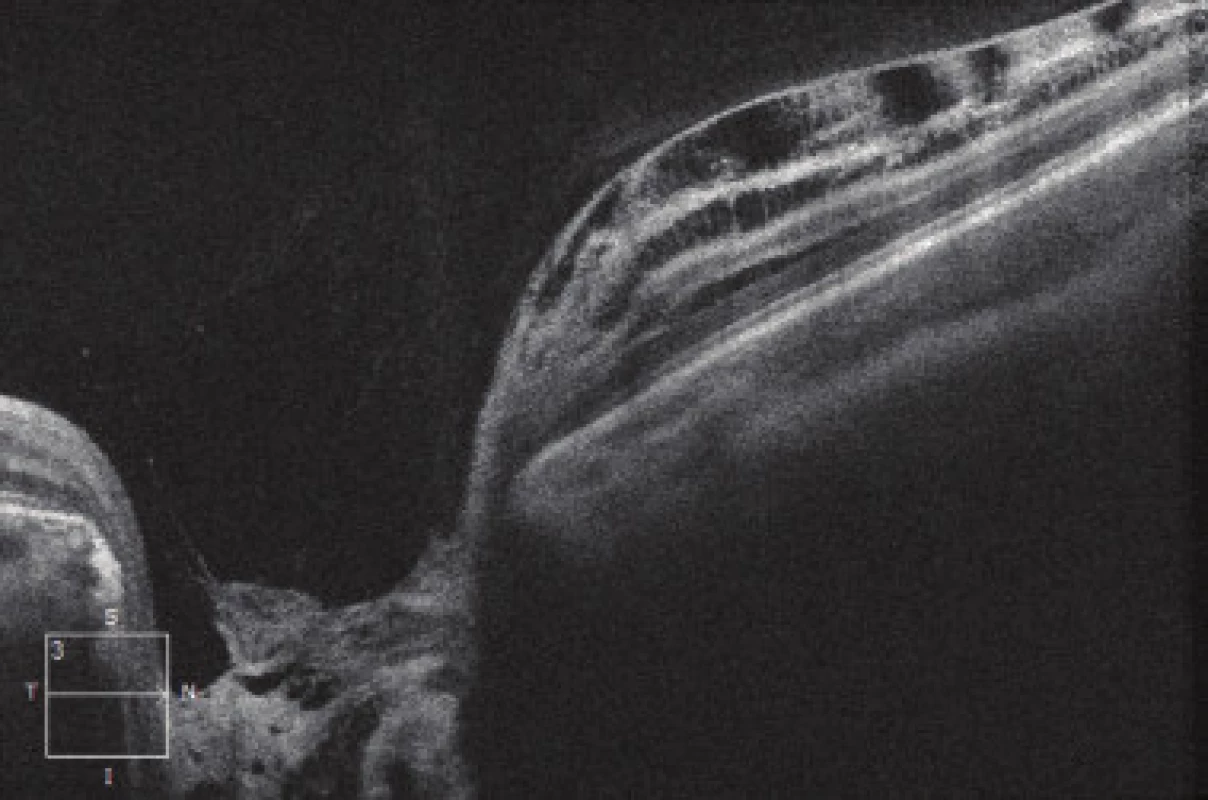
4. HD-OCT: Linear vertical transpapillary scan of left eye, extensive ODP covered by medium reflective tissue. At the upper edge connecting serous ablation of the neuroretina, with accumulation of fluid sub-retinally 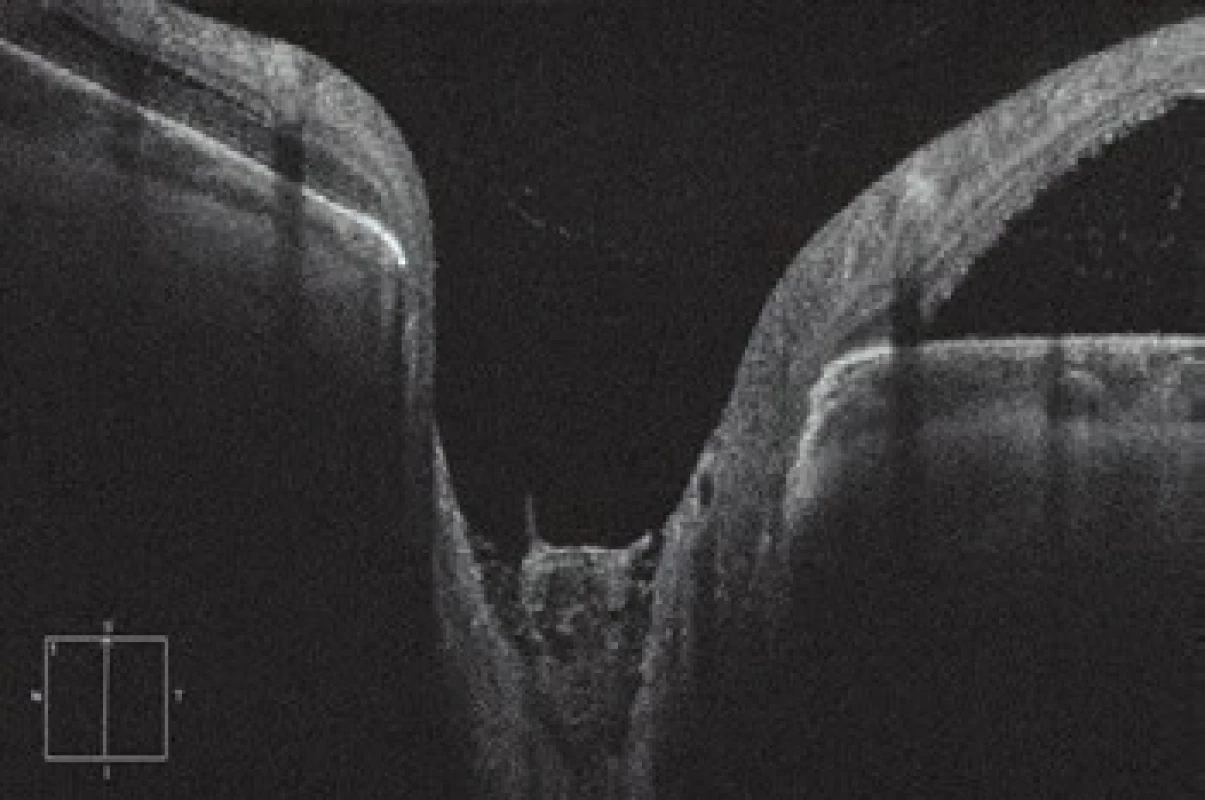
5. HD-OCT: Linear horizontal trans-retinal scan of left eye conducted in superotemporal peripapillary region, with evident extensive area of high serous ablation of neuroretina with accumulation of fluid sub-retinally, in temporal regions again evident schisis of retinal layers 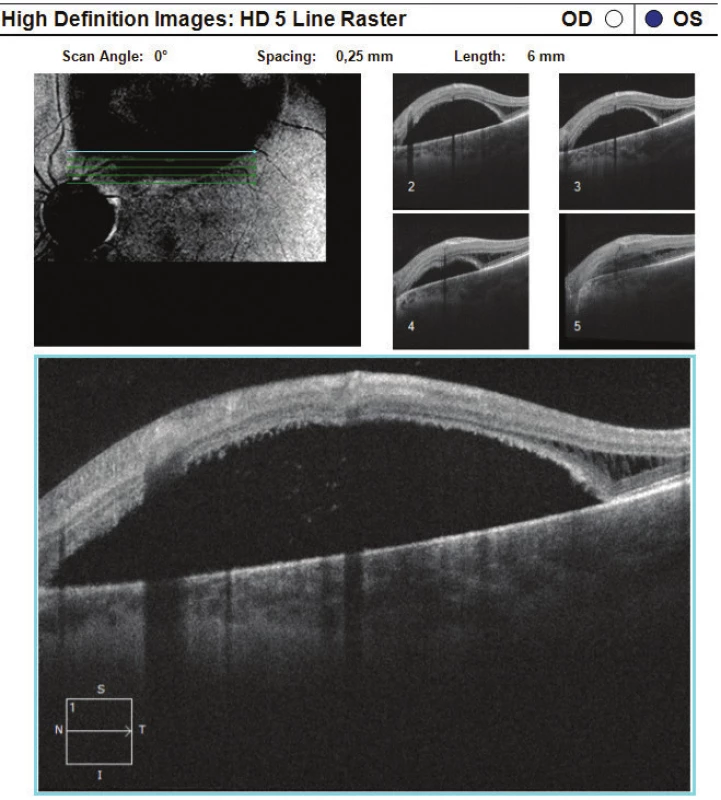
6. HD-OCT: Linear horizontal transfoveolar scan of left eye with image of schisis-like maculopathy, with separation in the region of central retinal layers 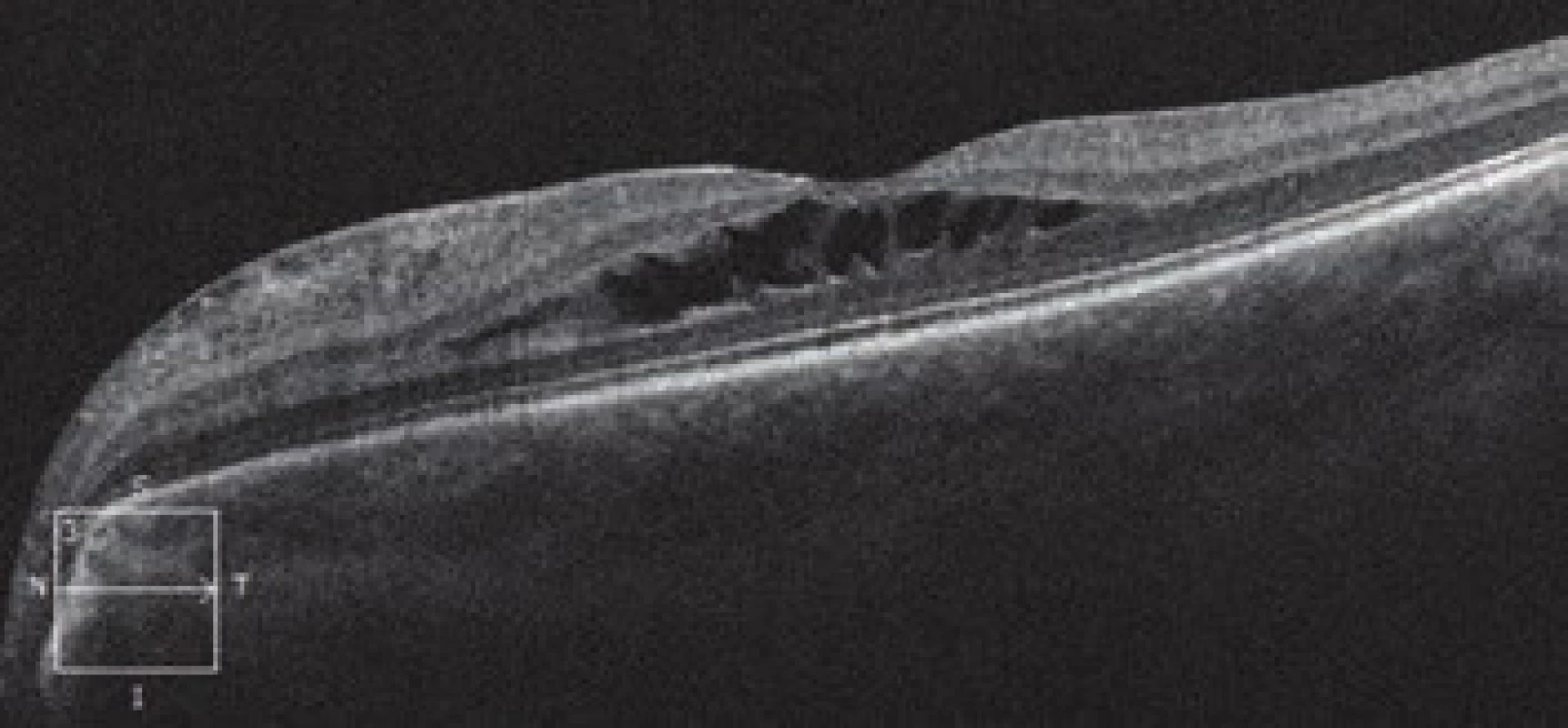
On the basis of the examination, the diagnosis was comprehensively concluded as bilateral optic disc pit, in the right eye with peripapillary retinoschisis, in the left eye with maculopathy of the character of retinoschisis. With regard to the patient’s unimpaired VA, no surgical solution of the given condition was indicated, the boy was left without local or general therapy in regular observation.
At a follow-up examination at the Children’s Ophthalmology Clinic conducted 4 months later, BCVA in RE was 4/4, BCVA LE 4/4, on the ocular fundus an image of ODP without progression. According to the follow-up and comparative HD-OCT in the right eye, stable finding with separation of retinal layers peripapillary in the nasal region, macula of physiological appearance without fluid, in left eye stationary extensive ablation of neuroretina in superotemporal retinal region connecting to DON, in macula schisis of retinal layers with slight regression of finding (fig. 7).
7. HD-OCT: Linear horizontal transfoveolar scan of left eye, follow-up examination after 4 months, image of stationary schisis-like maculopathy 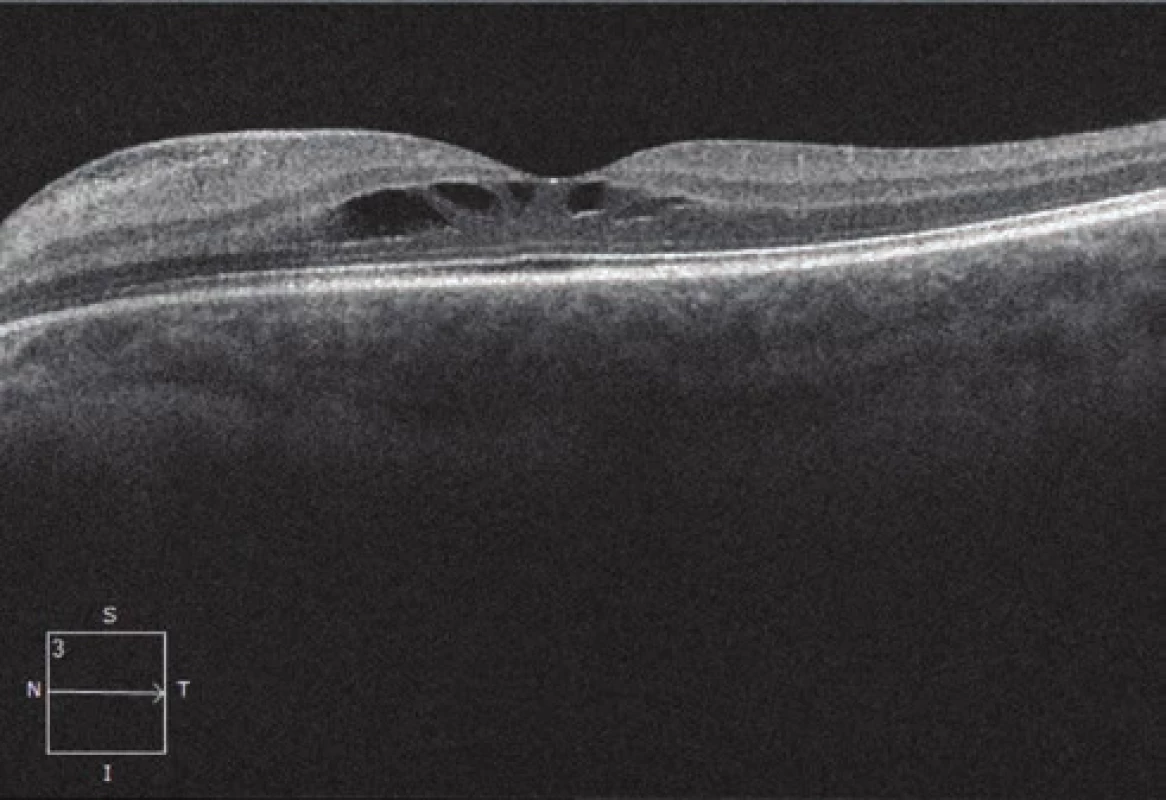
Outpatient check-ups were recommended every six months, upon any potential subjective worsening even earlier with regular OCT examination in order to compare and assess the development of the condition.
DISCUSSION
ODP is one of the congenital anomalies of the optic nerve. It appears as standard as an isolated affliction of the optic nerve, but some variants of congenital anomalies of the optic nerve are associated with other affliction of organ systems (for example papillorenal syndrome or basal encephalocele) [9, 16]. Most commonly ODP is unilateral, asymptomatic, and as a result is generally detected by chance, with maximum incidence in the third and fourth decade of life [10]. It does not represent a stable pathology, but a condition which progresses over time, and is associated with a progressive decrease of VA, blurred vision, metamorphopsias and a shift of refraction toward hypermetropia [8].
In our case report we describe a case of an asymptomatic 9-year-old patient with bilateral occurrence of optic disc pit, together with retinopathy and unilateral maculopathy. In approximately ½ of patients with diagnosis of ODP in childhood age there is a deterioration of vision between the ages of 20 and 30, an earlier onset of complaints is rare [18]. The onset of subjective symptoms is linked with the degree of retinopathy and maculopathy. Although in ¼ of cases a spontaneous regression of the finding takes place, in the majority of the afflicted eyes the prognosis remains poor. A number of cases of spontaneous regression of maculopathy on a background of ODP has been described in the literature. Yuen and Kaye [20] describe the case of an 8-year-old patient in whom VA improved from light perception to 2/30. Schatz and McDonald [17] described the case of a 6-year-old child with almost complete retinal reattachment after 5 months. In these cases spontaneous regression of the changes took place, without the necessity for surgical treatment. Even despite the quantity of studies dealing with ODP and the therapies of associated retinopathy and maculopathy, to date there is no consensus on the best method of therapy in paediatric patients. The majority of vitreoretinal ophthalmologists recommend a combination of laser photocoagulation on the peripapillary region and vitrectomy [6, 7]. Above all in diagnosis in children, 3-6 month observation is essential before any surgical intervention [18].
CONCLUSION
ODP is a congenital abnormality, which though rare, may be encountered in outpatient eye clinics for adult patients and children. The challenge still remains to ensure long-term care for patients with maculopathy, the incidence of which is within the range of 25–75 %. No precise standards exist for the therapy of maculopathy, and the correct timing of treatment also remains a matter for discussion. The patient with bilateral ODP with unilateral maculopathy from our case report remains under regular observation, and with regard to his satisfactory VA has been left without indication for surgical intervention. In the case of progression of the finding with seepage of fluid into the macula, it is possible to expect a deterioration of vision. In such a case, surgical therapy will be chosen according to the latest medical observations.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received by the Editorial Department on: 31 January 2019
Accepted for printing on: 11 March 2019
MUDr. Veronika Radošová
Sources
1. Bonett, M.: Serous macular detachment associated with optic nerve pits. Graefes Arch. Clin Exp Ophthalmol, 229; 1991 : 526-532.
2. Brodsky, MC.: Congenital optic disk anomalies. In Hoyt, CS., Taylor, D, Pediatric Ophthalmology and Strabismus, fourth edition. China, Elsevier Saunders, 2013, p. 552-553.
3. Brodsky, MC.: Congenital optic disk anomalies. Surv Ophthalmol, 39; 1994 : 89-112.
4. Ernest, J. et al: Makulární edémy. Praha, Mladá fronta, 2014, s. 229-233.
5. Gass, JD.: Serous detachment of the macula. Secondary to congenital pit of the optic nervehead. Am J Ophthalmol, 67; 1969 : 821-841.
6. Georgalas, I., Kouri, A. et al.: Optic disc pit maculopathy treated with vitrectomy, internal limiting membrane peeling, and air in a 5-year-old boy. Can J Ophthalmol., 45; 2010 : 189-191.
7. Georgalas, I., Ladas, I., Georgopoulos, G.: Optic disc pit: a review. Graefes arch Clin Exp Ophtalmol, 249; 2011 : 1113-1122.
8. Goktas, A., Goktas, S.: Common. embryological links to the optic pit and anterior segment structures. Optom Vis Sci; 87; 2010 : 585-7
9. Goldhammer, Y., Smith JL.: Optic nerve anomaliesin basal encephalocele. Arch Ophthalmol, 93; 1975 : 115-8.
10. Hirakata, A., Okada, AA. et al.: Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology; 112; 2005 : 1230–1235.
11. Jain, N., Johnson, MW.: Pathogenesis and treatment of macu opathy associated with cavitary optic disc anomalies. Am J Ophtalmol, 158; 2014 : 423-435.
12. Kalvodová, B., Říčařová, R., Kuthan, P. et al.: Vitrektomie u jamky terče zrakového nervu s makulopatií. Cesk Slov Oftalmol, 55; 1999 : 123-127.
13. Kranenburg, EW.: Crater-like holes in the optic disc and central serous retinopathy. Arch Ophthalmol, 64; 1960 : 912-924.
14. Krivoy, D., Gentile, R., Liebmann, JM. et al.: Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophtlhalmol, 114; 1996 : 165-170.
15. Sadun, AA., Khaderi, KH.: Optic disc anomalies, pits and associated serous macular detachment. In: Ryan, SJ., Schachat, AP., Wilkinson, CP.: Retina 5. UK, Elsevier Health Sciences, 2013, p. 1538-1588 .
16. Sanyuanusin, P., Schimmemnti, LA. et al.: Mutation of the PAX2 gene in a family with optic nerve colobomas, renal anomalies and vesicoureteral reflux. Nat Genet, 9; 1995 : 358–64.
17. Schatz, H., McDonald, R.: Treatment of sensory retinal detachment associated with optic nerve pit or coloboma. Ophthalmology, 95; 1988 : 178-186.
18. Sezin, AB., Almila, SS. et al.: Spontaneous Regression of Optic Disc Pit Maculopathy in a Six-Year-Old Child. Turk J Ophtlhalmol, 47; 2017 : 56-58.
19. Svěrák, J., Rencová E., Kvasnička J. et al.: Jamky terče a makulopatie. Elektroretinografická studie. Cesk Slov Oftalmol, 58; 2002 : 287-291.
20. Yuen, CHW., Kaye SB.: Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: A case report. J AAPOS, 6; 2002 : 330-331.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 2-
All articles in this issue
- Očná klinika Lekárskej fakulty Univerzity Komenského v Bratislave oslavuje 100-TÉ VÝROČIE činnosti – 1. časť
- Normal tension vs high tension glaucoma: an – overview
- Correction of myopia and myopic astigmatism by femtosecond laser in situ keratomileusis
- Effect of Botulinum toxin A application in neuro-ophtalmologic indications on Schirmer’s test and tears osmolarity.
- Peripheral exudative hemorrhagic chorioretinopathy
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Normal tension vs high tension glaucoma: an – overview
- BILATERAL OPTIC DISC PIT WITH MACULOPATHY – THE CASE REPORT
- Suprachoroideal haemorrhage in postoperative period of antiglaucoma surgery, case report
- Peripheral exudative hemorrhagic chorioretinopathy
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

