-
Medical journals
- Career
Ophthalmic manifestations of acute leukaemias
Authors: S. Němčanská 1,2; A. Stepanov 3,4; J. Němčanský 1,2
Authors‘ workplace: Fakultní nemocnice Ostrava, Oční klinika, přednosta MUDr. Jan Němčanský, Ph. D. 1; Ostravská univerzita v Ostravě, Lékařská fakulta, Katedra kraniofaciálních oborů, vedoucí katedry: prof. MUDr. Pavel Komínek, Ph. D., MBA 2; Univerzita Karlova, Lékařská fakulta v Hradci Králové, Katedra očního lékařství, vedoucí katedry: prof. MUDr. Naďa Jirásková, Ph. D., FEBO 3; Fakultní nemocnice Hradec Králové, Oční klinika, přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO 4
Published in: Čes. a slov. Oftal., 74, 2018, No. 3, p. 98-101
Category: Original Article
doi: https://doi.org/10.31348/2018/1/3-3-2018Overview
Background and aims:
To determine the incidence of ocular pathological findings in a group of patients with acute leukemia. To define the predictive value of the presence of the ocular pathological findings.
Materials and methods:
Retrospective evaluation of a group of 67 patients with acute leukemia (age 1–75 years) examined at the Ophthalmology Clinic, Faculty Hospital Ostrava, from 2005 to 2014.
Results:
Ocular pathological findings were found in 13 patients of the group (19.4 %) - 7 patients with acute myeloid leukemia (10.9 %) and 6 patients with acute lymphoblastic leukemia (8.5 %). 10 patients died due to of the underlying disease. Ocular pathological findings were found in 6 of them (60 %). A higher prognostic value was found in a group of patients with AML.
Conclusion:
Ophthalmology examination is a necessary part of the examination of patients with acute leukemia. This prognostic benefit is particularly significant in patients with AML.
Key words:
acute myeloid leukemia, fundus leucaemicus, Roth's spot, ophthalmology examination
Introduction
Acute leukaemias are neoplastic pathologies of haematopoiesis caused by a malignant transformation of haematopoietic stem cells. As a consequence of this, two cell populations exist alongside one another in the patient. One originates from normal stem cells, the other from leukaemic stem cells. These tumour cells infiltrate bone marrow, peripheral blood and the haematopoietic organs, and lead to a suppression of normal haematopoiesis. According to which developmental range the malignant process affects, we divide acute leukaemias into two groups: acute myeloid leukaemias (AML) and acute lymphoblastic leukaemias (ALL) (1, 9).
Statistical data from the Institute of Health Information and Statistics (IHIS) from 2015 presents the incidence of all leukaemic pathologies in the Czech Republic at 14.9 per 100 000 men versus 10.8 per 100 000 women (12). The incidence is highest in the age group of children aged 0-4 years (2.1 males and 3.0 females per 100 000), the second peak of incidence of this pathology is in the age group over 70 years (66.9 men and 34.8 women per 100 000) (12). Acute myeloid leukaemias occur more frequently in adult age, and we observe an increase in incidence in patients over 65 years of age (12, 18, 19).
In the case of acute leukaemias, the diagnosis is determined on the basis of a laboratory finding and biopsy of bone marrow. In the blood count we always find a certain degree of anaemia and thrombocytopenia, and the total number of leukocytes may be increased, reduced or within the norm. Important for diagnosis is a laboratory finding of blasts in blood and a cytological examination of bone marrow, which demonstrates the infiltration of leukaemic cells (1, 9).
The therapy consists in the application of combined chemotherapy according to the relevant protocol, with the aim of liquidating the maximum possible quantity of pathologically altered bone marrow. An integral component of the treatment is transplantation of bone marrow and adjuvant therapy. Immunosuppression and bone marrow suppression is induced, which is desirable in the first phase of the therapy and represents a prognostically favourable sign.
Non-specific general symptoms of the pathology are fever or subfebrile temperature, weariness, loss of appetite, weight loss, and pain in the neck, joints and bones. Suppression of normal haematopoiesis leads to anaemia, fatigue, paleness of the skin and mucous membranes, breathlessness, headaches, dizziness, heart palpitations and also thrombocytopenia with haemorrhage manifestations into the mucous membranes and skin in the form of petechiae or haematomas. Ocular manifestations of acute leukaemias are present in up to 50-70% of patients (3, 4, 15). We can divide them into 2 groups: direct manifestations of the pathology and changes as a consequence of systemic affliction in the case of acute leukaemia.
Direct manifestations of the pathology
Primary leukaemic infiltration of the ocular tissues is relatively rare (5, 8). It concerns infiltration of abundantly vascularised tissues of the choroid and retina. Manifestations of infiltration of the choroid, which is most frequently afflicted, are best identified by ultrasonography as its diffuse thickening (3, 4, 11). We also include here primary infiltration of the orbit. This is more common in the case of ALL, and is generally linked with painful, rapidly developing protrusion of the eyeball, edema of the eyelids and chemosis of the conjunctiva (10). Infiltration of the iris tissue causes diffuse thickening in connection with the closure of the crypts, or nodular thickening of the iris with formation of nodules at the edge of the pupil (3, 4, 10). In the case of more extensive infiltration of the iris tissue, leukaemic cells penetrate into the anterior chamber, where they form a pseudohypopyon (6, 10). Infiltration of the chamber angle may be manifested in an increase of intraocular pressure, with the development of secondary glaucoma. A further location of primary leukaemic infiltration is the optic nerve (4, 6). Leukaemic infiltrates in the retina and subretinal space have the form of whitish deposits (Fig. 2). Perivascular leukaemic infiltrates form greyish-white streaks.
1. Fundus leucaemicus: intraretinal haemorrhage, soft exudates and Roth's spots 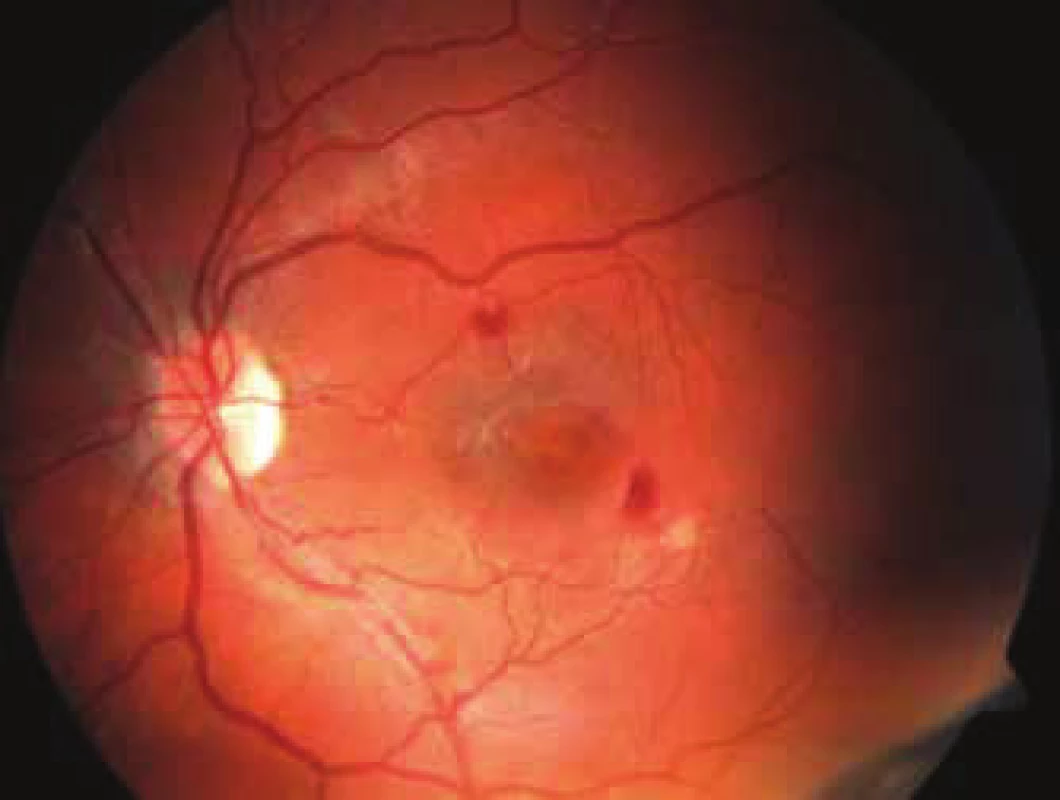
2. Leukaemic infiltrates of retina 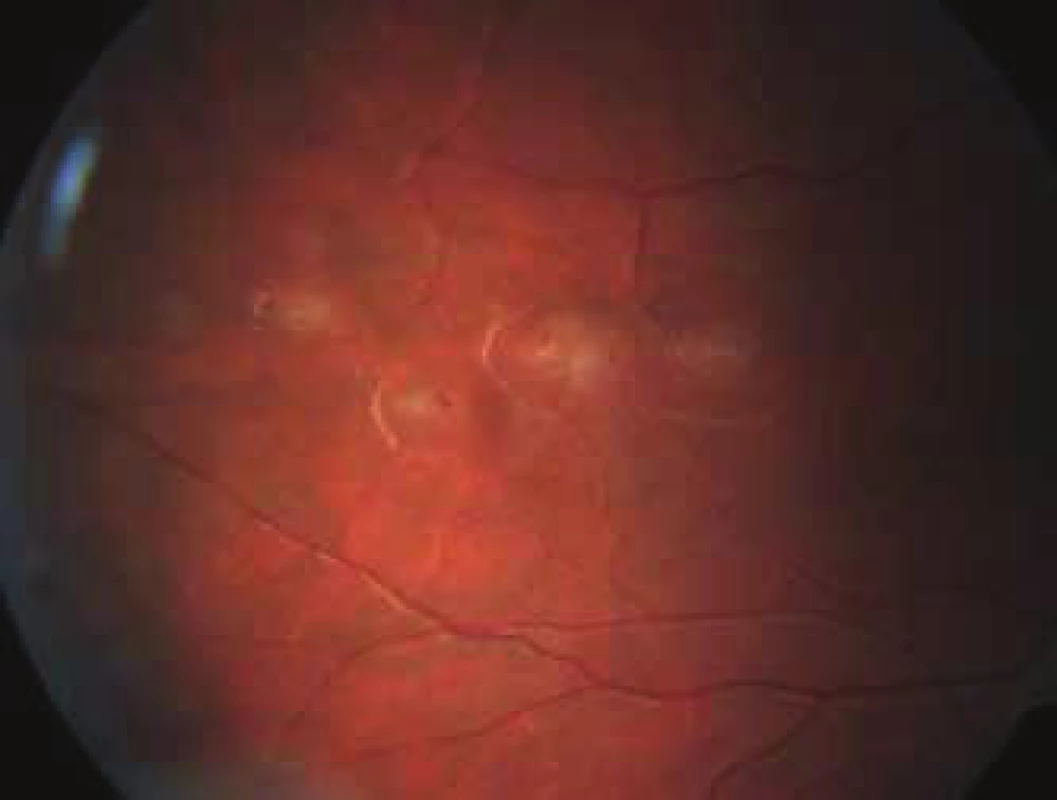
Manifestations of leukaemic affliction of the retina are often asymptomatic. More rarely they cause deterioration of vision in patients unilaterally or bilaterally, especially upon affliction of the macula. They may also be the first sign of the pathology or the first sign of a relapse. They are considered a prognostically unfavourable factor, linked with a shorter survival time (6, 15, 17). In leukaemia patients it may be difficult to differentiate whether this concerns inflammatory or leukaemic infiltration of the ocular tissues. Classic signs of inflammation are often lacking, which is due to immunosuppression of the patient (2). Avascular tissues of the lens and vitreous body are not generally primarily afflicted.
Manifestations of the pathology as a consequence of systemic affliction upon acute leukaemia
These ocular changes appear more frequently. In the pathogenesis a role is played by anaemia, thrombocytopenia, leukocytosis and immunosuppression. A further developing factor is aggressive chemotherapy (2). The most common finding is “leukaemic retinopathy” or fundus leucaemicus: intraretinal and subhyaloid haemorrhages, hard and soft exudates and retinal haemorrhages with central pallor termed Roth's spots (Fig. 1). Signs of occlusion of the retinal blood vessels may be present.
Ocular complications of immunosuppression
Ocular complications of long-term immunosuppression, total body irradiation, aggressive chemotherapy treatment and last but not least also recurring malignancy are evident above all on the anterior segment, and include manifestations such as keratoconjunctivitis sicca, pseudomembranous conjunctivitis, bacterial and viral conjunctivitis, sterile or infectious corneal ulcer and development of cataract. On the posterior segment of the eye, manifestations of immunosuppression and haematological imbalances are less common, but very serious and sight-threatening. These are in particular opportunistic infections of the eye, most frequently cytomegaloviral chorioretinitis (7, 16). Patients with acute leukaemia undergoing intensive chemotherapy are also the highest-risk group for the incidence of invasive mycotic infections generated both by yeast fungi and fibrous fungi.
Cohort and method
The study evaluated medical records of 67 patients with a diagnosis of acute lymphoblastoma or myeloid leukaemia examined in the period from January 2005 to June 2014 at the Department of Ophthalmology at the University Hospital Ostrava, at a time when the patients were hospitalised at the Department of Haematooncology or the Department of Paediatric Haematooncology of the University Hospital Ostrava.
In the majority of cases, the ocular examination was conducted by indirect or direct ophthalmoscope in inpatient care, due to the alteration of the overall condition of the patient, which did not enable transport to an ocular outpatient clinic and examination on a slit lamp. In one case an ocular examination was conducted at an ocular emergency department, and on the basis of a pathological ocular finding a diagnosis of acute leukaemia was determined. In one case a patient was examined when already in the stage of remission. We focused on age, sex, incidence and nature of the ocular affliction, and the mortality of patients in the acute phase of the pathology. Patients with AML are sent as a standard procedure from the University Hospital Ostrava for induction therapy at the Department of Haematooncology in Brno and Olomouc, therefore their data is not complete. In the case of child patients, treatment is often conducted at the University Hospital Motol in Prague, especially if bone marrow transplant is indicated. The data was statistically evaluated with the aid of the software IBM SPSS Statistics version 22. All the statistical tests were conducted as bilateral on a level of significance of 0.05.
Results
In our cohort, out of a total of 67 patients, 55 patients (82.1%) had ALL and 12 patients (17.9%) had AML (graph 1). The cohort was composed of 41 men (61.2%) and 26 women (38.8%). Further epidemiological parameters are stated in table 1. There were 9 adult patients (13.4%) with an average age of 54.7 years (18-75 years). There were 58 child patients (86.6%), with an average age of 7.5 years (1-17 years). Ocular manifestations of leukaemia were described in 13 patients (retinal haemorrhage in 6 cases, 2x suffusion of conjunctiva, 3x congestion on the disc of the optic nerve as a consequence of intracranial hypertension, 1x unilateral protrusion of eyeball from infiltration of the retrobulbar space, 1x bilateral anterior iritis, 1x central retinal vein occlusion) (table 2, graph 2). During the observation 10 patients died as a consequence of the basic pathology. Ocular manifestations were diagnosed in 6 of these patients (i.e. 60% of deceased patients).
1. Comparison of patients with diagnosis of AML and ALL. 
2. Percentage representation of ocular symptoms 
1. Epidemiological parameters of patients 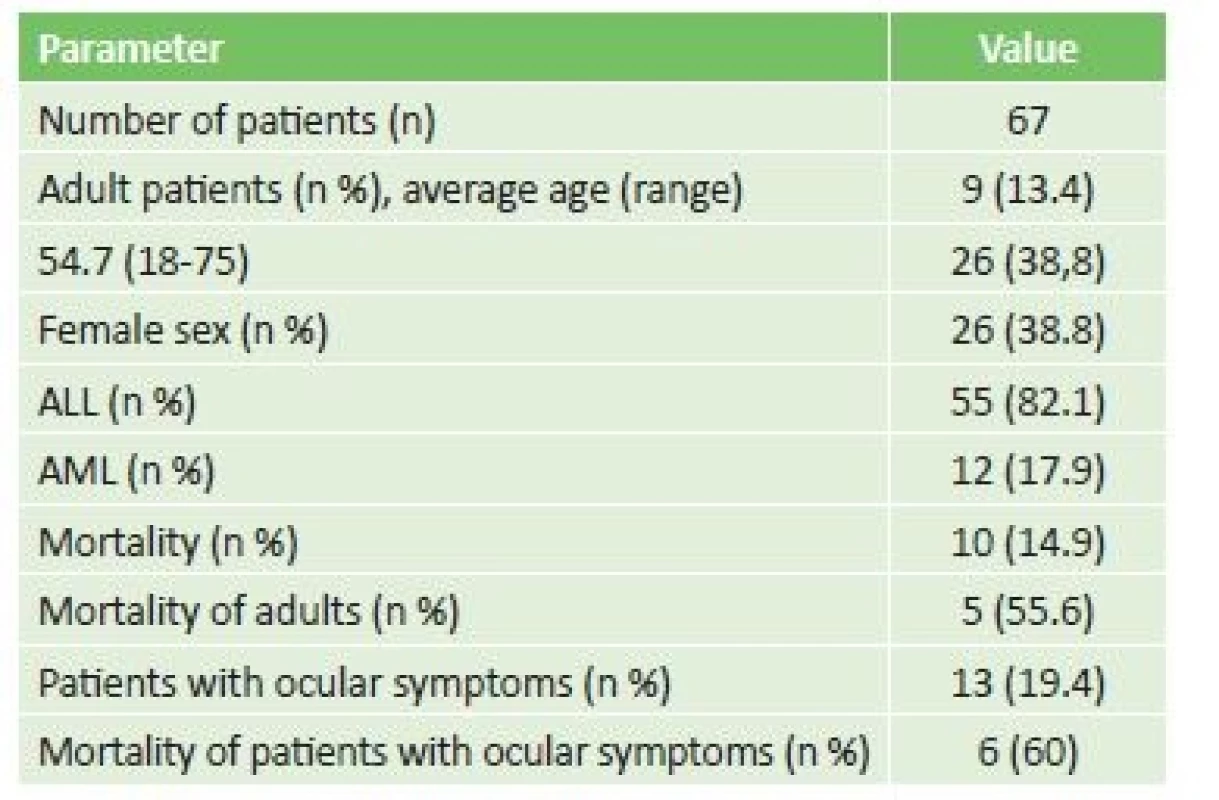
2. Acute ocular symptoms in patients with leukaemia in our cohort. 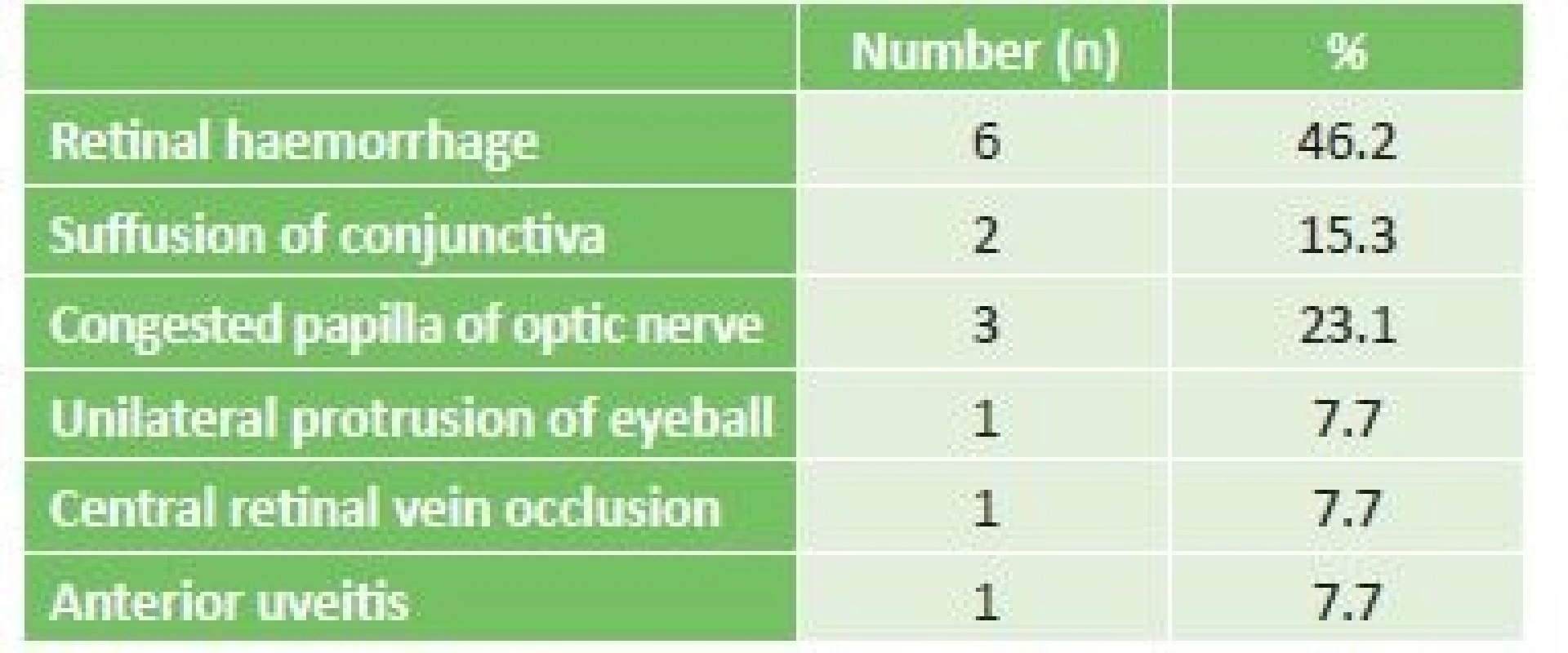
Discussion
In our cohort an ocular finding was identified in 19.4% of all examined patients (in child patients in 12.1%, in adults in 66.7%). We explain the high representation of ocular symptoms in adult patients by means of the higher number of patients aged over 65 years. In these patients the haematooncologist did not indicate radical therapy due to comorbidity and advanced age. These factors also link to the worse prognosis of these patients. Reddy et al. in their study state the incidence of ocular symptoms in 35.4%, but include patients with both acute and chronic leukaemias, and at the same time they had a higher proportion of adults and patients with AML than in our cohort (14). In child patients they state the incidence of ocular symptoms in 16.5%, in adult patients in 49.1% (14).
Ohkoshi et al. recorded a pathological ocular finding in 28 out of 63 child patients with acute leukaemia, of whom 6 patients (9.5%) were in the early stage and 22 patients (34.9%) upon relapse or development of affliction of the central nervous system (CNS) (13). In our cohort early ocular symptoms were identified in 3 child patients (5.1%), in relapse and affliction of the CNS in 4 cases (6.9%) of all child patients. A reduction of the incidence of relapse of the CNS took place after the introduction of prophylactic administration of methotrexate or intrathecal chemotherapy, as well as prophylactic radiotherapy of the neurocranium into the protocols of therapy for ALL. In our child patients with ALL, prophylaxis with methotrexate was performed in 46 cases, combined prophylaxis with methotrexate and radiotherapy of the neurocranium in 5 cases, and radiotherapy of the neurocranium alone in 2 cases. Only in one child prophylaxis of the CNS was not performed. In our view this explains the lower incidence of ocular findings in patients with a relapse of the pathology in comparison with the study by Ohkoshi.
Conclusion
From the perspective of the prognosis of the course of leukaemia, ophthalmological examination is of an unequivocal benefit. Despite this fact this examination is not conducted routinely. In the case of subjectively stated ocular complaints, if the presence of ocular symptoms are detected macroscopically upon physical examination, or as an examination for the exclusion of congestion on the ocular fundus before lumbar puncture, the haematologist sends the patient for an ophthalmological examination. Nowadays, modern therapeutic options increase the probability of longer survival for patients with acute leukaemia, nevertheless interdisciplinary co-operation is still necessary in order to ensure the determination of a timely and correct diagnosis. An important role is played also by eye examinations, which record the course of the pathology.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Korespondující autor: MUDr. Alexandr Stepanov, Ph.D., FEBO
Oční klinika FNHK
Hradec Králové, Sokolská 581, 500 05
Sources
1. Bureš, J.: Základy vnitřního lékařství. 1. vyd. Praha, Galén, 2003, s. 416-421.
2. Gordon, K., Rugo, H., Duncan, J. et al.: Ocular Manifestations of Leukemia. Ophthalmology, 108; 2001 : 2293-2300.
3. Hejcmanová, D., Jebavá, R., Hak, J. et al.: Izolovaná leukemická infiltrace duhovky. Čes a slov Oftal, 49(6); 1993 : 374-379.
4. Hejcmanová, D., Langrová, H., Jebavá, R. et al.: Unusual ocular findings in children’s acute leukemia cases. Acta medica, 40; 1997 : 51-56.
5. Jackson, N., Reddy, S.C., Hishamuddin, M. et al.: Retinal findings in adult leukaemia: correlation with leukocytosis. Clin Lab Haem, 18; 1996 : 105-109
6. Kanski, JJ.: Clinical ophthalmology. 5th ed. Edinburgh, Butterworth-Heinemann, 2003, p. 485-486.
7. Kanvinde, S., Bhargava P., Patwardhan S.: Cytomegalovirus Infection as a Cause of Cytopenia After Chemotherapy for Hematological Malignancies. Indian Pediatrics, 50; 2013 : 197-201.
8. Karas, M.: Akutní myeloidní leukemie u nemocných nad 60 let, možnosti její léčby a potenciální role alogenní transplantace krvetvorných buněk. Onkologie, 5(2); 2011 : 91-95.
9. Klener, P.: Vnitřní lékařství. 2. vyd. Praha, Galén, 2001, s. 360-365.
10. Kuchynka, P.: Oční lékařství. 1.vyd. Praha, Grada, 2007, s. 733-734.
11. Miyamoto, K., Kashii, S., Honda, Y. et al.: Serous retinal detachment caused by leukaemic choroidal infiltration during complete remission. Br J Ophthalmol, 84; 2000 : 1318-19.
12. Novotvary ČR [online]. Praha: Ústav zdravotnických informací a statistiky ČR, 1988-2015. Dostupné z: www.uzis.cz/katalog/zdravotnicka-statistika/novotvary
13. Ohkoshi, K., Tsiaras, W.G.: Prognostic importance of ophthalmic manifestations in childhood leukaemia. Br J Ophthalmol, 76(11); 1992 : 651-655.
14. Reddy, S.C., Jackson, N., Menon, B.S.: Ocular Involvement in Leukemia - A Study of 288 Cases. Ophthalmologica, 217; 2003 : 441-445.
15. Rozsíval, P.: Oční lékařství. 1. vyd., Praha, Karolinum, 2006, s. 323-324.
16. Říhová, E.: Uveitidy. 1. vyd., Praha, Grada, 2009, s. 107.
17. Sharma, T., Grewal, J., Gupta, S.: Ophthalmic manifestations of acute leukaemias: the ophthalmologist's role. Eye, 18(7); 2004 : 663-672.
18. Specchia, G., Albano, F., Guerriero, S. et al.: Retinal Abnormalities in Newly Diagnosed Adult Acute Myeloid Leukemia, Acta Haematol, 105; 2001 : 197-203
19. Starý, J.: Akutní leukémie u dětí. Onkologie, 4(2); 2010 : 120-124.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 3-
All articles in this issue
- Ophthalmological finding in a patient with lowe syndrome
- Marshall and stickler syndrome in one family
- Congenital central toxoplasmic chorioretinitis - case study
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Conjuctival lesions - the relationship of papillomas and squamous cell carcinoma to HPV infection
- Ophthalmic manifestations of acute leukaemias
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ophthalmic manifestations of acute leukaemias
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Congenital central toxoplasmic chorioretinitis - case study
- Marshall and stickler syndrome in one family
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


