-
Medical journals
- Career
Ciliary body melanoma treatment by stereotactic radiosurgery
Authors: A. Furdová 1; J. Juhas 1; M. Šramka 2; G. Králik 3
Authors‘ workplace: Klinika oftalmológie LF UK a UNB, Nemocnica Ružinov, Bratislava, prednosta doc. MUDr. Krásnik Vladimír, PhD. 1; Klinika stereotaktickej rádiochirurgie OÚSA a VŠZaSP, Bratislava, prednosta prof. MUDr. Šramka Miron, DrSc. 2; Ústav klinickej fyziky SZU a OÚSA, Bratislava, prednosta doc. RNDr. Králik Gabriel, PhD. 3
Published in: Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 204-210
Category: Original Article
Overview
Introduction:
Malignant melanoma of the ciliary body (corpus ciliare) represents 10 to 15 percent of tumors of the uveal tract. The aim of the work is to evaluate the effectiveness of stereotactic radiosurgery performed on LINAC linear accelerator and the occurrence of postoperative complications.Material and methods:
Retrospective analysis of patients with ciliary body melanoma treated with stereotactic radiosurgery on linear accelerator in the period 1/2011 to 12/2016 in Slovakia.Results:
From 1/2011 to 12/2016 a group of 27 patients with melanoma of the ciliary body underwent one day session stereotactic radiosurgery irradiation on linear accelerator (SRCH). Primary enucleation was indicated in 10 (37 %) patients. A group of 17 (63 %) patients were treated with stereotactic radiosurgery. In a group of 17 patients indicated for SRCH, 7 (41 %) were diagnosed in T1 stage, 8 (47 %) in T2 stage. In 2 (12 %) patients who refused primary enucleation, palliative irradiation was indicated in T3 stage, and later metastases appeared in liver and systemic chemotherapy was indicated.
The therapeutic dose in all patients was TD 35 Gy, TD max 42 Gy. The mean age of patients at the time of irradiation was 60.8, the youngest patient was 40 and the oldest was 80 years old. The follow-up period was 12 months to 5 years.Conclusion:
Currently, in Slovakia, the only irradiation possibility to treat ciliary body melanoma is stereotactic radiosurgery. In our group of 17 patients, this method appears to be effective in the treatment of T1 to T2 stage. The results are comparable to brachytherapy and proton beam irradiation therapy.Key words:
corpus ciliare, uveal melanoma, linear accelerator, stereotactic radiosurgeryINTRODUCTION
Malignant melanoma of the ciliary body (corpus ciliare) represents 10 to 15 percent of all tumours of the uveal tract (2, 4). These tumours are often asymptomatic, and as a result may reach larger dimensions before they generate clinical symptoms in the patient (5, 10). The symptoms that may appear in the patient include changes in the visual field and deterioration of vision (10). One of the most significant symptoms is dilation of the episcleral vessels (sentinel vessels) in the quadrant of the tumour's growth (5, 10). The tumour frequently infiltrates the iris or sclera. Through its growth it presses upon the lens and causes a sectoral cataract, in some cases as far as luxation of the lens (3-5, 9, 10). Tumours are usually pigmented, in rarer cases non-pigmented. They most frequently grow nodularly, in isolated cases diffusely, when they are also referred to as ring melanoma and are linked with a worse prognosis (5). The TNM classification is the basis in the recording also of intraocular tumours. According to the American Joint Committee on Cancer from 2010, stage T1 corresponds to a tumour from the corpus ciliare not exceeding a base of 10 mm and a height of 2.5 mm. In stage T2 the tumour does not exceed a base of 16 mm and a height of 10 mm. In stage T3 we observe a spread into the anterior chamber, and in stage T4 also extrabulbarly (3). In diagnosis we rely on examination by a slit lamp. Due to its position, transscleral illumination using a Lange lamp is also necessary. On principle ultrasound diagnosis is performed in the A and B system, examination by ultrabiomicroscopy is optimal also with regard to long-term observation of patients. Anterior segment OCT (optical coherence tomography) and FAG (fluorescence angiography) of the anterior segment are significant in diagnosis, especially in the case of tumours ensuing from the iris and infiltrating the chamber angle and corpus ciliare. We can also implement puncture of the anterior segment of the eye for cytological, special biochemical and immunological examination. The dimensions and shape can be displayed by means of MR (magnetic resonance) and CT (computer tomography). We determine the definitive diagnosis on the basis of the imaging examinations in correlation with the clinical picture.
One of the possibilities for the therapy of tumours of the corpus ciliare is stereotactic radiosurgery. This consists in the application of photon beams from an external irradiator into the tumour from a number of directions, with the aim of attaining the highest dose of radiation in the place of the tumour and the lowest dose in the surrounding tissues. Tumours indicated for therapy have an elevation of up to 7 mm, in some cases these are tumours for which the patient refused another method of therapy (3, 4, 11). Patients who have a radiosurgical procedure planned undergo fixation of all the rectus muscles of the eye by means of sutures one day before irradiation. On the day of irradiation, a stereotactic frame is fitted onto the patients. Patients with a fitted stereotactic frame undergo CT and MR examination, by means of which the tumour is precisely measured. There then follows planning of the distribution of the dose of radiation in such a manner that the tumour is blasted with a dose of min. 35 Gy and the surrounding structures receive as little as possible. After the compilation of an individual irradiation plan, the patient is irradiated with a single dose of 35 Gy.
Monitoring by an ophthalmologist is subsequently conducted at 2-weekly intervals, 3 months after the procedure we conduct an MRI examination. Continuous observation of patients after irradiation is permanent, and requires monitoring of intraocular pressure values, regular observation with the aid of ultrasound and MR examination at 1-yearly intervals. Observation of the occurrence of potential metastases is conducted at 6-monthly intervals in the first 5 years after irradiation, and later at 1-yearly intervals for the remainder of life.
MATERIAL AND METHOD
Retrospective analysis of patients with melanoma of the corpus ciliare treated by stereotactic radiosurgery on a LINAC linear accelerator during the period from 1/2011 to 12/2016 in Slovakia.
RESULTS
At the Department of Ophthalmology at the Faculty of Medicine, Comenius University and University Hospital Bratislava, during the observed period we diagnosed and indicated treatment for a total of 27 patients with melanoma of the corpus ciliare. The average age of the patients was 72 years, in which the youngest patient was 40 and the oldest 80 years.
In the cohort of 27 patients, the primary indication was enucleation for 10 patients (37%); treatment by stereotactic radiosurgery was indicated for 17 patients (63%) (graph 1). In the group of patients who were indicated for primary enucleation, the average age was 75 years; in the patients treated with stereotactic radiosurgery the average age was 60.8 years.
1. Indication for treatment in patients with melanoma of the corpus ciliare 
Indication for treatment by stereotactic radiosurgery was conditional also upon the result of examination by PET/CT (positron emission tomography), in order to exclude the presence of metastases at the time of diagnosis of the tumour.
For one patient we indicated stereotactic radiosurgical treatment on the basis of progression of the deposit also in the region of the iris and anterior chamber, which we documented also with the aid of fluorescence angiography (FAG) (fig. 1).
1. Macro photo of anterior segment with melanoma growing into the anterior chamber (A, B); fluorescence angiography of the same patient (C, D) – the tumour is before the planned irradiation on a linear accelerator. 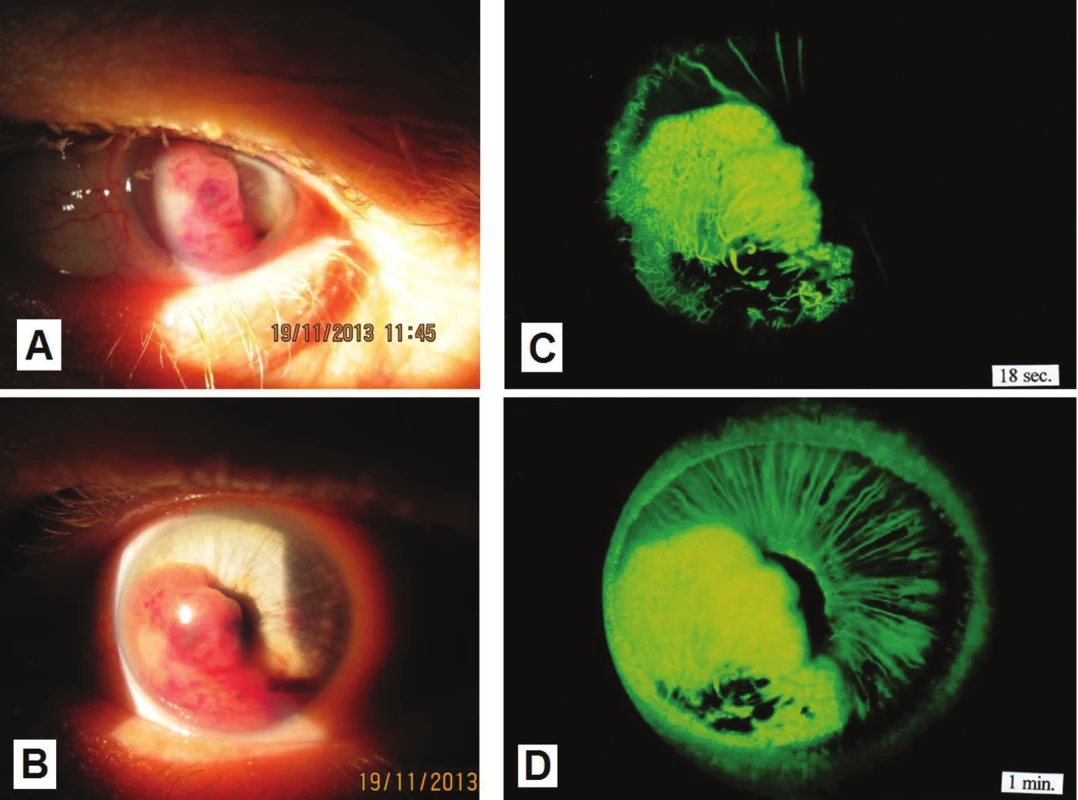
Thanks for photographs C and D to the authors: Dr. Streicher and Dr. Špirková from Bojníce In the group of 17 patients indicated for stereotaxis, 7 patients (41%) were diagnosed with a tumour in stage T1, 8 cases (47%) concerned stage T2. In 2 patients (12%), who refused primary enucleation, palliative irradiation by stereotactic radiosurgery was indicated on a linear accelerator in stage T3 – later remote metastases were discovered in the liver of these patients, and general chemotherapy was indicated. The therapeutic dose was TD 35 Gy for all patients, TD max 42 Gy (graph 2).
2. TNM stage in patients with melanoma of the corpus ciliare indicated for stereotaxis 
The observation period was 12 months to 5 years.
Of secondary complications following irradiation, secondary glaucoma occurred in 8 cases at a time interval of 12 to 24 months after irradiation.
Post-radiation cataract began to develop in all of the patients within a period of 12 to 24 months after irradiation, while secondary glaucoma was recorded in 8 cases. Secondary enucleation due to post-radiation complications was indicated in 3 patients (17.64%), in which malignant melanoma ensuing from the corpus ciliare was histopathologically confirmed.
In the patients after stereotaxis we recorded one case of death which was unconnected with the basic pathology (the patient had determined metastases in the inguinal region).
CASE REPORT 1
The patient, a 65 year old man, reported to the emergency eye clinic at Ružinov hospital in May 2012 following a blow from a conifer branch to the right eye. He had never undergone an ocular examination before. Best corrected visual acuity was 0.1, intraocular pressure within the norm. In addition to the finding in the anterior segment following the trauma, in mydriasis the attending physician noticed a pigmented formation behind the iris. In June 2012 an MR examination was conducted, which confirmed a finding of a solid tumour mass in the region of the corpus ciliare of the nasal quadrant of the right eye, with infiltration in a “forward” direction and infiltration of the chamber angle (fig. 2, 3).
2. MRI image of patient with sketched tumour in the region of the corpus ciliare with outgrowth in a “forward” direction and into the chamber angle (A), and sketching of the tumour of the corpus ciliare (red colour) and lens (green colour) in the planning scheme for radiosurgical irradiation on a linear accelerator (B) 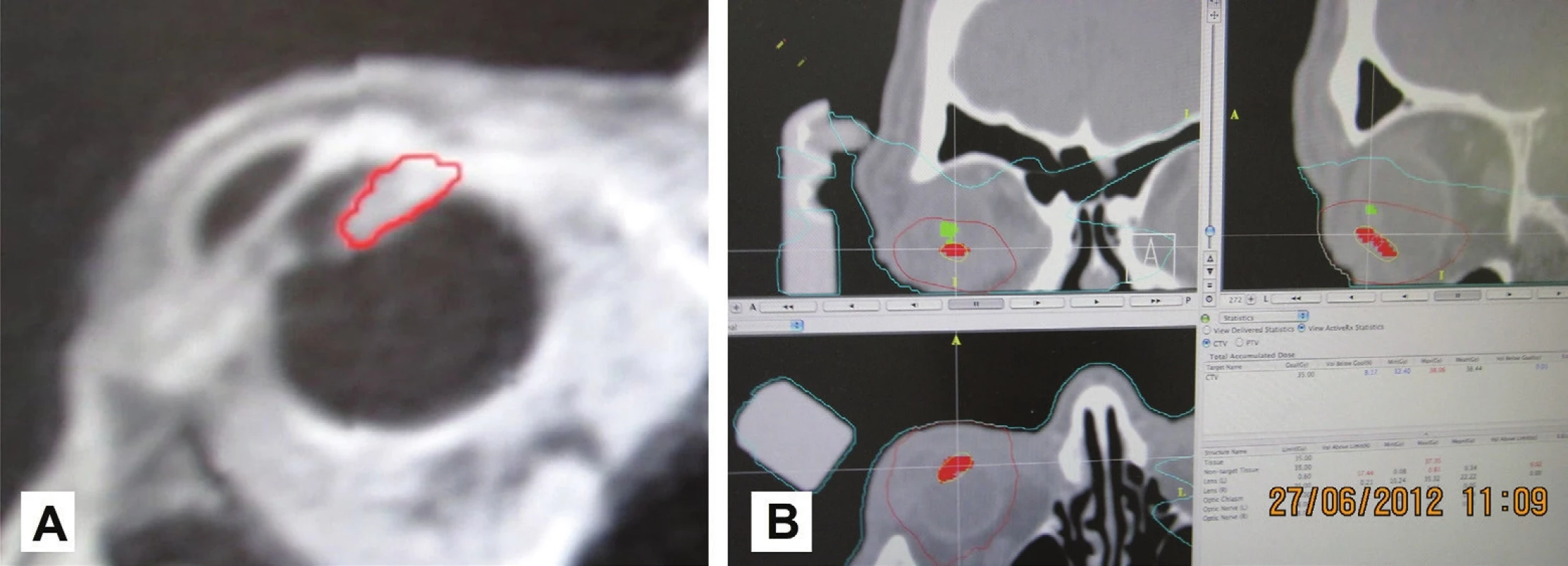
3. Macro photo of anterior segment of eye of patient in 2012 (A), 2013 (B) and 2014 © 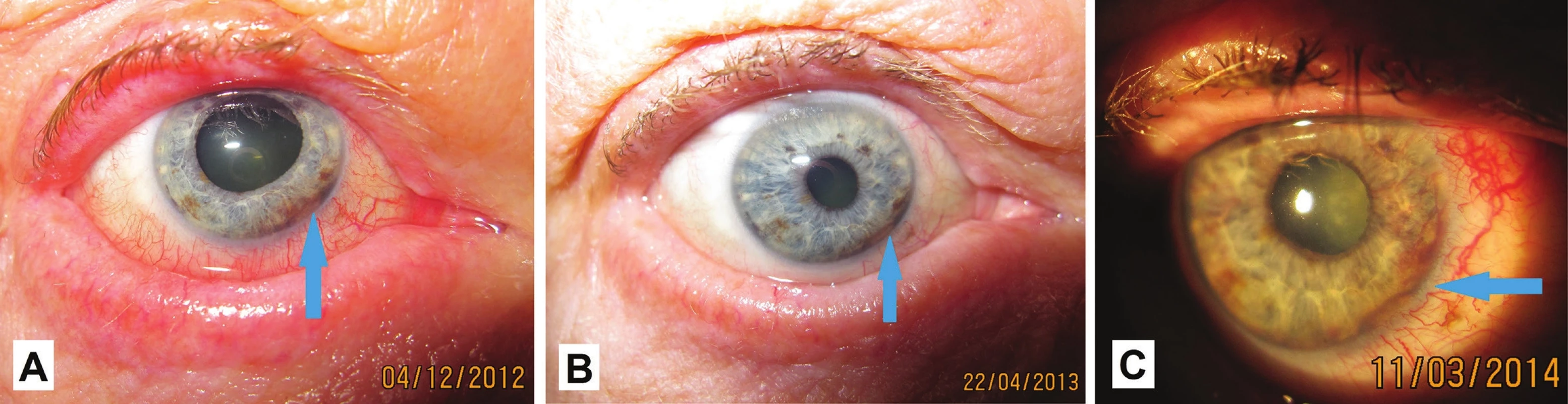
The patient was indicated for stereotactic radiosurgery. The size of the calculated volume of the tumour was 0.2 cm3. TD applied was 35 Gy, the maximum dose was 37 Gy.
We continued to monitor the patient at regular intervals at our ophthalmology outpatient department. At a follow-up examination in April 2013, increased intraocular pressure was recorded (40 Torr). After the application of local anti-glaucomatous therapy, correction and long-term stabilisation of the condition was attained. An MR examination in October 2014 showed the tumour now in subtotal regression (fig. 4, 5).
4. Macro photo of anterior segment of eye of same patient in 2015 – progression of cataract (A), accentuation of neovascularisation of isis (B) 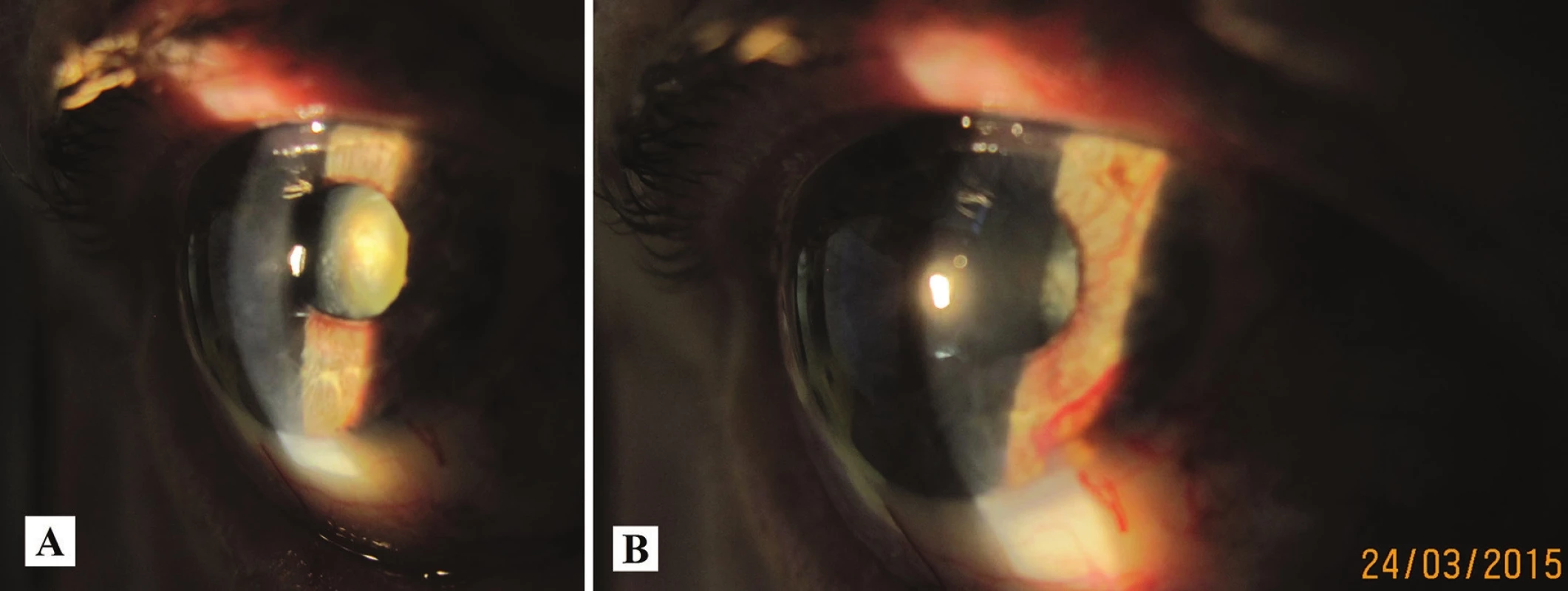
5. Comparison of MR images of patients in 2012 before irradiation (A) and in 2015, i.e. 3 years after irradiation there is visible reduction of the volume of the tumour (B) 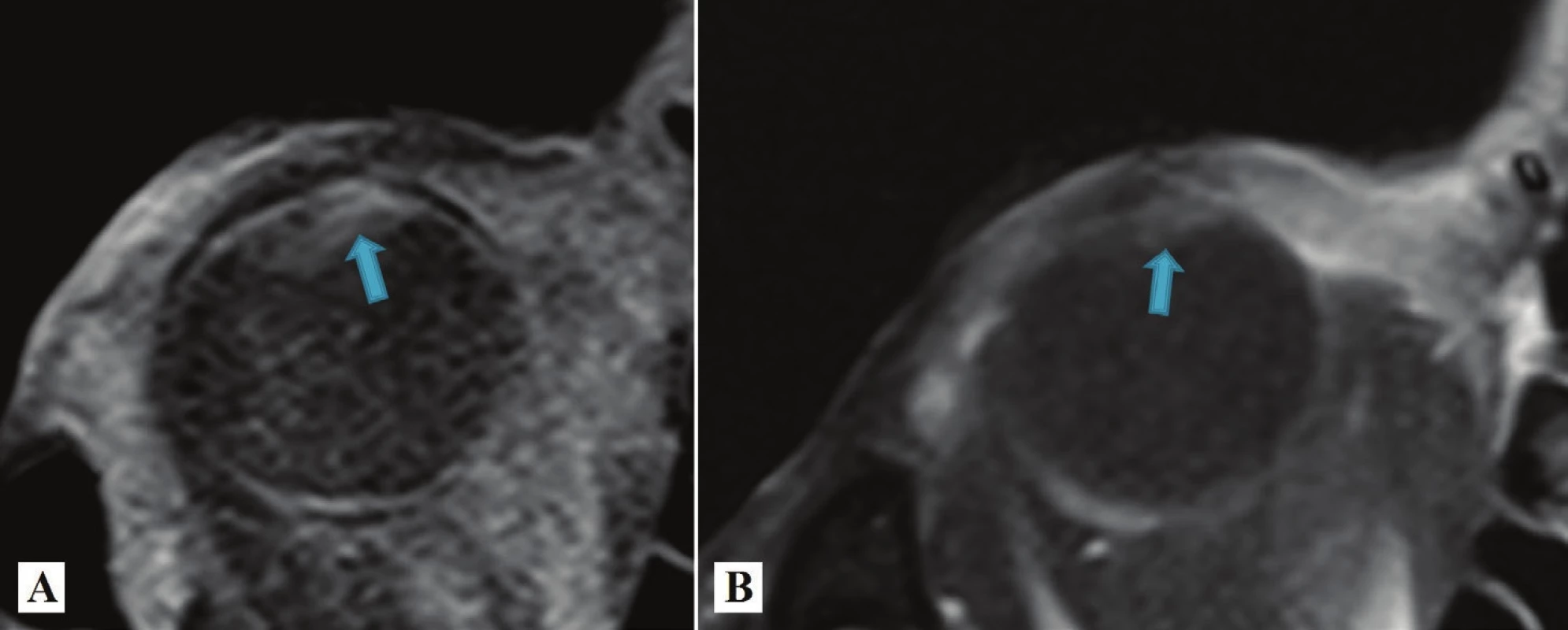
At the last follow-up examination in 2017, corrected visual acuity was light perception, increased values of intraocular pressure persisted up to 35 Torr despite the application of anti-glaucomatous therapy, but the patient felt no pain. Outpatient monitoring is continuing, screening of metastases negative.
CASE REPORT 2
A 71 year old man was monitored at our department due to diabetic retinopathy. In 2014 deterioration of vision was determined, with a prescription for glasses, best corrected visual acuity was 0.8, intraocular pressure within the norm. The patient was sent for an USG examination, suspect TU I dx. was determined, originating from the region of the corpus ciliare. MR examination confirmed a tumour growing intrabulbarly from the medial wall, with infiltration in a “backward” direction, base 10 mm x 14 mm, projecting 7 mm into the vitreous body. Stereotactic radiosurgery performed, the size of the calculated volume of the tumour was 0.4 cm3, TD was applied in dose of 35 Gy, maximum dose was 38 Gy (fig. 6). Outpatient monitoring of the patient continues, screening of metastases negative. 24 months after the procedure secondary glaucoma was determined, the patient was treated in outpatient care, deterioration of CVA – light perception with localisation. Enucleation was indicated upon the patient's request (fig. 7). A histological examination confirmed malignant melanoma fusocellular type B.
6. Sketching of tumour deposit originating from the region of the corpus ciliare with outgrowth in a “backward” direction into the region of the choroidea – tumour in red colour, lens in yellow colour (A), MR imaging of eye with tumour (B) 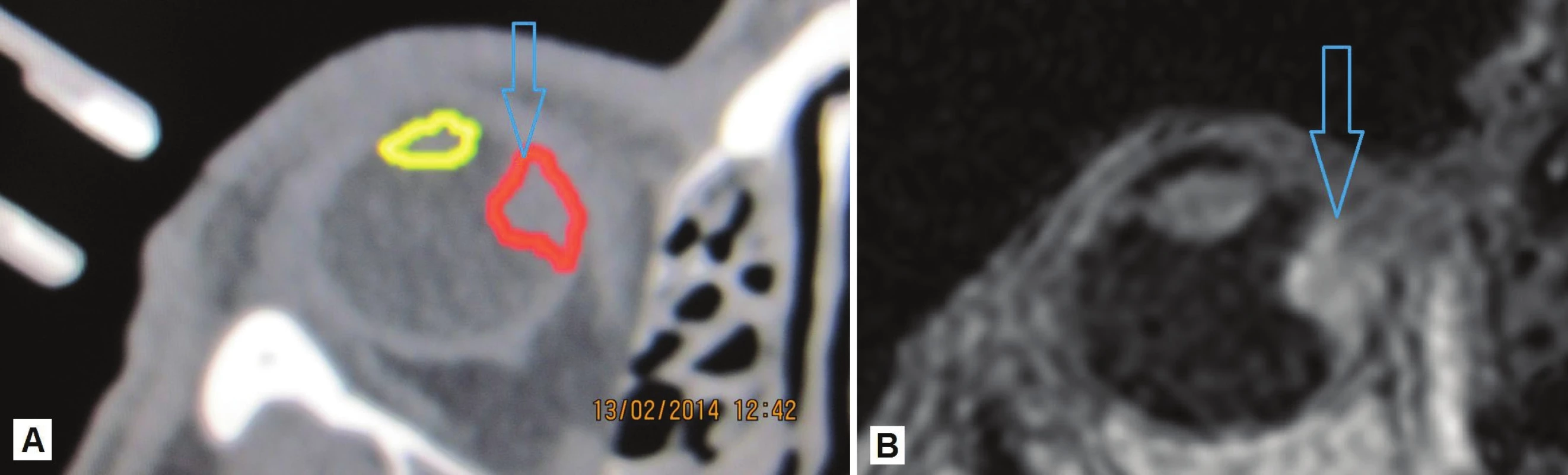
7. Macro photo of enucleated eyeball (A), detail of pronounced pigmented malignant melanoma in cross-section (B) 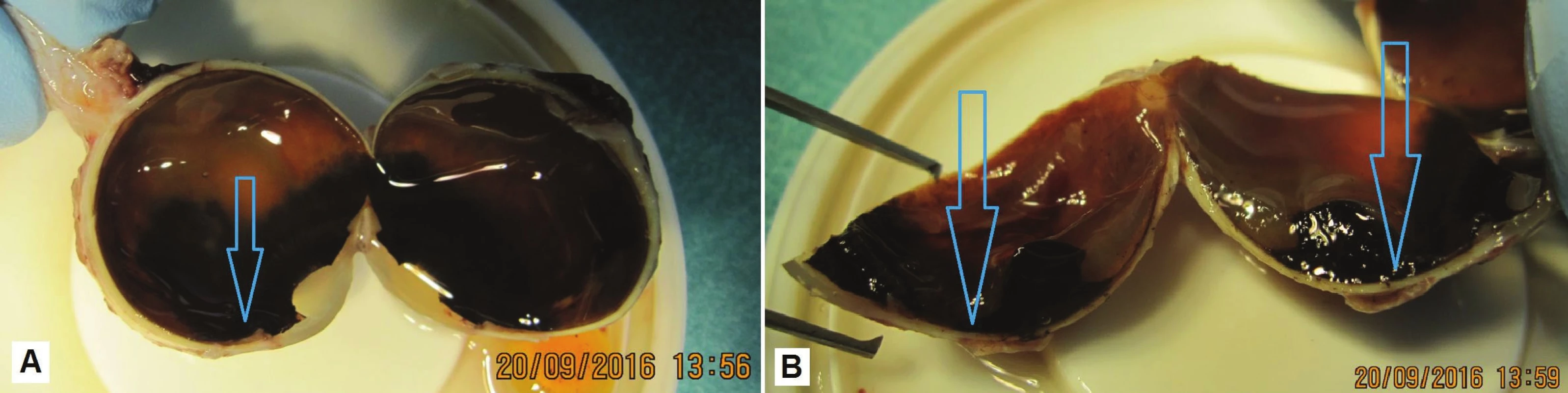
DISCUSSION
Melanomas rarely originate in the corpus ciliare in comparison with the posterior uvea. Malignant melanomas of the corpus ciliare are often not recognised for a long time, and have complex clinical manifestations, which are not easily diagnosed and influence the prognosis of the pathology if diagnosed in an advanced stage (15). Small tumours as a rule do not cause the patients any complaints, and therefore as a rule their diagnosis is late, or they are identified by chance at an ophthalmological examination. At present there are a number of therapeutic options for treatment. Small, medium sized and also large tumours are suitable for treatment by stereotactic radiosurgery. The first Gamma knife was presented in the 1960s by Lars Leksell, a Swedish neurosurgeon, in co-operation with the radiobiologist Borje Larsson. As a rule this form of therapy takes place as fractionated or single-treatment radiation of a precisely defined value into a stereotactically localised volume of tumour tissue (6).
In 2015 authors from the University of Los Angeles published a study of 37 patients (37 eyes) treated by brachytherapy for malignant melanoma of the choroidea and corpus ciliare, where they observed changes of best corrected visual acuity, contrast and colour sensitivity. They evaluated the results over the course of the 1st, 2nd and 3rd years. Average visual acuity before irradiation was 77 letters, in the first year 65 letters, in the second year 56 and in the third year 47 letters. At the conclusion they evaluated a significant deterioration of best corrected visual acuity, contrast and colour sensitivity in patients following brachytherapy (12).
In 2016 authors from the Cole Eye Institute in Cleveland published an interesting case report of a 44 year old man with an amelanotic ring melanoma of the corpus ciliare. A fine-needle biopsy confirmed malignant melanoma, and the patient underwent enucleation of the eye. The patient remains without signs of metastases for 9 years. A histopathological examination confirmed malignant melanoma incorporating the iris and corpus ciliare with 360 degree spread along the trabecular tissue. The tumour was composed of a mixture of fusocellular and epitheloid cells, with weak pigmentation (1).
In 2016 Weber et al. published a study in which they presented the results and toxicity of proton therapy of uveal melanomas. The study included the cases of 77 patients, of whom the corpus ciliare was afflicted in 35%. In the majority of patients (61%) this concerned a large tumour in stage T3/T4 according to the AJCC classification. After 5 and 10 years the authors of the study evaluated the level of control of the ocular tumour, the number of surviving patients without metastases, the overall survival of patients and the number of enucleations of the bulb in the observed cohort. Toxicity of proton therapy, requiring enucleation of the bulb, occurred only rarely (13).
In 2017 a team of doctors headed by the professor of radio-oncology Cengiz presented a study which evaluates the results of stereotactic radiosurgery and fractionated stereotactic radiosurgery in the treatment of uveal melanomas as a whole. In the study the authors determined that with a dose equal to or higher than 45 Gy divided into 3 fractions it is possible to attain a higher degree of control of the ocular tumour. Survival without the necessity of enucleation after 2 years reached the level of 73% in the entire observed group of 181 patients with uveal melanoma. After 5 years the total level of patient survival was 98%. According to the study, the dose of radiotherapy is therefore an exceptionally significant factor in the control of the tumour and prevention of loss of the eye (14).
In 2017 an American team from the Mayo Clinic evaluated a cohort of patients with uveal melanoma, who had undergone therapy by Gamma knife. Out of 11 patients with uveal melanoma, enucleation was necessary in 1 case (9%). Metastases did not appear in any of the patients. Complications of treatment by Leksell gamma knife within the group represented the occurrence of radiation retinopathy in 2 patients, papillotomy in 1 patient, the occurrence of cystoid macular edema also in 1 patient, vitreomacular traction in 1 patient and exudative retinal detachment in 1 patient (8). In our cohort we recorded secondary enucleation due to post-radiation complications in 3 patients (17.64%), in which malignant melanoma originating from the corpus ciliare was histopathologically confirmed in all.
An interesting case report was published by authors from The New York Eye and Ear Infirmary of Mount Sinai in New York. A 75 year old female patient with diagnosed 17-year pseudoexfoliative glaucoma, surgically treated by argon laser trabeculoplasty and trabeculectomy in the left eye, was diagnosed in the ipsilateral eye with melanoma of the corpus ciliare with visible extrascleral extension. The treatment involved the insertion of a 103Pd radioactive irradiator via functional trabeculectomy with removal 7 days later. The result was a successfully treated tumour without clinical evidence of damage to the filtration pad, with resulting stable intraocular pressure. Without further surgery for glaucoma, intraocular pressure remained well controlled upon local application of pharmaceuticals for a period of 6 years. Melanoma of the corpus ciliare with minimal extrascleral extension beneath a functional filtration pad can be treated with the aid of therapy by radioactive irradiators. In this case the authors were able to achieve a regression of the tumour with control of the glaucoma pathology (7).
CONCLUSION
In Slovakia at present, the only possibility for treatment of tumours of the corpus ciliare is irradiation by means of stereotactic radiosurgery. In our cohort of patients this method is demonstrated to be effective in the treatment of melanomas of the corpus ciliare in stage T1 and T2. The results are comparable with treatment by means of brachytherapy and proton radiation.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Doc. Mgr. MUDr. Alena Furdová, PhD.,MPH, FEBO
Klinika oftalmológie LFUK a UNB,
nemocnica Ružinov
Ružinovská 6, 826 06 Bratislava
e-mail: alikafurdova@gmail.com
tel: pracovisko +421 248 234 607
Sources
1. Aziz, H. A. et al. Amelanotic Irido-Ciliary Ring Melanoma: A Clinicopathological Correlation. Ocular Oncology and Pathology. 2016-04, vol. 2, no. 3, p. 153–155. DOI: 10.1159/000441725.
2. Baráková, D. et al. Nádory oka. Praha : Grada Publishing, 2002. 152 p. ISBN: 80-247-0141-3.
3. Furdová, A.; Krásnik, V. Možnosti liečby vnútroočného malígneho melanómu. Bratislava : Univerzita Komenského, 2016. 135 p. URL <https://www.fmed.uniba.sk/fileadmin/lf/sluzby/akademicka_kniznica/PDF/Elektronicke_knihy_LF_UK/MOZNOSTI_LIECBY_VNUTROOCNEHO_MALIGNEHO_MELANOMU.pdf>. ISBN: 978-80-223-4073-1.
4. Furdová, A.; Oláh, Z. Nádory oka a okolitých štruktúr. Brno : Akademické nakladatelství CERM, 2010. 152 p. ISBN: 978-80-7204-689-8.
5. Furdova, A.; Sramka, M. Uveal malignant melanoma and stereotactic radiosurgery: Intraocular uveal melanoma and one-day session stereotactic radiosurgery at linear accelerator. Saarbrücken: LAP LAMBERT Academic Publishing, 2014-09-30. 188 p. ISBN: 978-3-659-61042-4.
6. Mclean, M. J.; Foster, W. D.; Zimmerman, L. E. Prognostic factors in small malignant melanomas of choroid and ciliary body. Archives of Ophthalmology (Chicago, Ill.: 1960). 1977-01, vol. 95, no. 1, p. 48–58. 00318.
7. Pathan, A. H. K. et al. Palladium-103 plaque radiation therapy for ciliary body melanoma through a functioning glaucoma filtering bleb. European Journal of Ophthalmology. 2017-09-23, p. 0. DOI: 10.5301/ejo.5001046.
8. Reynolds, M. M. et al. Gamma knife radiosurgery for the treatment of uveal melanoma and uveal metastases. International Journal of Retina and Vitreous. 2017-05-29, vol. 3. DOI: 10.1186/s40942-017-0070-2. URL <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5447304/>.
9. Salmon, J.; Bowling, B.: Kanski’s Clinical Ophthalmology E-Book: A Systematic Approach. Elsevier Health Sciences, 2015-03-24. 931 p. Google-Books-ID: D9GfBwAAQBAJ. ISBN: 978-0-7020-5574-4.
10. Shields, J. A.; Shields, C. L.: Intraocular Tumors: An Atlas and Textbook. Lippincott Williams & Wilkins, 2008. 598 p. Google-Books-ID: SXYXDY2DPtAC. ISBN: 978-0-7817-7580-9.
11. Svetlošáková, Z.; Krásnik, V.: Malígny melanóm uvey – diagnostika, liečba, prognóza. Onkológia. 2012, vol. 7, no. 1, p. 35–38.
12. Tsui, I. et al.: Visual Acuity, Contrast Sensitivity and Color Vision Three Years After Iodine-125 Brachytherapy for Choroidal and Ciliary Body Melanoma. The Open Ophthalmology Journal. 2015, vol. 9, p. 131–135. DOI: 10.2174/1874364101509010131.
13. Weber, B. et al.: Outcomes of Proton Beam Radiotherapy for Large Non-Peripapillary Choroidal and Ciliary Body Melanoma at TRIUMF and the BC Cancer Agency. Ocular Oncology and Pathology. 2015-09, vol. 2, no. 1, p. 29–35. DOI: 10.1159/000433546.
14. Yazici, G. et al.: Stereotactic Radiosurgery and Fractionated Stereotactic Radiation Therapy for the Treatment of Uveal Melanoma. International Journal of Radiation Oncology, Biology, Physics. 2017-05-01, vol. 98, no. 1, p. 152–158. DOI: 10.1016/j.ijrobp.2017.02.017.
15. ZHAO, M. et al.: Secondary glaucoma as initial manifestation of ring melanoma: a case report and review of literature. International Journal of Clinical and Experimental Pathology. 2014, vol. 7, no. 11, p. 8163–8169.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2017 Issue 5-6-
All articles in this issue
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career


