-
Medical journals
- Career
Reconstruction of recurrent ischiadic pressure ulcer using turnover hamstring muscle flap
Authors: F. Černoch; Z. Jelínková; Pavel Rotschein
Authors‘ workplace: Clinic of burns and reconstructive surgery, Faculty of Medicine, Masaryk University and University Hospital Brno, Czech Republic
Published in: Cesk Slov Neurol N 2019; 82(Supplementum 1): 15-18
Category: Original Paper
doi: https://doi.org/10.14735/amcsnn2019S15Overview
Aim: Our aim was to analyze the results of surgical reconstruction of recurrent ischiadic pressure ulcer using the turnover hamstring flap and to describe the re-use of turnover biceps femoris flap in recurrent ischiadic pressure ulcer.
Materials and methods: There were 16 patients included in our study (15 male, with the mean age of 47 years), who underwent reconstruction of recurrent ischiadic pressure ulcer between 1. 1. 2016 and 31. 5. 2018 using the turnover hamstring muscle flap in combination with fasciocutaneous posterior thigh flap. The recurrence and complications during the one-year follow-up were recorded.
Results: There was one recurrence (6.25%) and five complications (31.25%) during the one-year follow-up. All complications were healed conservatively (without surgery).
Conclusion: The recurrence of ischiadic pressure ulcer depends not only on the method of surgical reconstruction, but also on the general and nutritional state of the patient, compliance of the patient and other factors. The turnover hamstring muscle flap seems as a reasonable option for reconstruction of the recurrent ischiadic pressure ulcer.
Keywords:
pressure ulcers – ischiadic pressure ulcer – reconstruction – muscle flap
Introduction
Ischiadic pressure ulcers are caused by the continuous pressure of ischial tuberosity against the soft tissues resulting in local ischemia and tissue damage. They mainly occur in paraplegic wheelchair-bound patients and they significantly reduce their quality of life [1]. They may appear as a skin fistula with a pseudocyst cavity deep underneath which can reach to the ischial bone, rectum or vagina. Surgical procedure is indicated in the stage 3 and stage 4 of the pressure ulcer [2] and usually is divided into two separate surgeries. The first surgery includes radical necrectomy with capsulectomy of the pressure ulcer, removal of all the fistulas and resection of the lytic bone if present. The reconstruction surgery takes place later on after targeted antibiotics therapy and correction of the general and nutritional state of the patient [3]. Primary reconstruction of the defect usually involves fasciocutaneous dorsal thigh flap with medial or lateral pedicle or musculocutaneous flap using posterior muscles of the thigh or inferior part of gluteus maximus muscle [4]. The method of closure must be selected with respect to the size and depth of the ulcer and to the state of surrounding tissue to be tension free. Since the recurrence rate may reach up to 39% [5] the secondary reconstruction is a great challenge for the plastic surgeon. Our aim was to analyze the results of surgical reconstruction of recurrent ischiadic pressure ulcer using the turnover hamstring flap and to describe the re-use of turnover biceps femoris flap in recurrent ischiadic pressure ulcer.
Patients and Methods
We retrospectively analyzed the medical records of all the patients with recurrent ischiadic pressure ulcer treated at the University Hospital Brno from January 2016 to May 2018. The inclusion criteria were recurrent ischiadic pressure ulcer (on the right side, left side, or both), reconstruction of the defect with turnover muscle flap using muscles of the posterior thigh (hamstring muscle flap) and one-year follow-up. Collected data included demographics, location and side of the pressure ulcer, the length of hospital stay, anesthesiology procedure (general anesthesia, sedation or none), type of hamstring muscle flap used for reconstruction (biceps femoris, semitendinosus, semimembranosus), complications and a recurrence within the one-year follow-up.
Results
A total of 16 patients underwent reconstruction of recurrent ischiadic pressure ulcer using turnover hamstring muscle flap at our clinic between January 2016 and May 2018. Majority of patients (N = 15) were male. The mean age of the patients was 47 years (min. 26; max. 78 years). In 56.25% (N = 9) the pressure ulcer was localized on the left side of the body, in 37.5% (N = 6) on the right side and in 6.25% (N = 1) on both sides. The method of anesthesia was in 75% (N = 12) sedation, in 12.5% (N = 2) general anesthesia and in 12.5% (N = 2) no anesthesia. The mean hospital stay was 21 days (min. 9; max. 55). In 75% (N = 12) was used the biceps femoris muscle, in 6.25% (N = 1) the semitendinosus muscle, in 6.25% (N = 1) the semitendinosus and semimembranosus muscle and in 12.5% (N = 2) all posterior muscles of the thigh. The reconstruction was successful in 93.75% (N = 15) and there was only one patient with recurrence of the pressure ulcer during the one-year follow-up period making the recurrence rate 6.25% (N = 1). The complications rate within 30 days from surgery reached 31.25% (N = 5) and included four wound dehiscence and one hematoma. All complications were healed conservatively and required no further surgical procedures.
Discussion
Ischiadic pressure ulcer belongs among the most common pressure ulcers in paraplegic patients [6]. The continuous pressure of ischial tuberosity when seated is between 80 to 100 mmHg and causes difficulty in achieving successful reconstruction of the defect [5]. The reconstruction methods for primary or secondary closure usually follow the reconstruction ladder with choosing the easiest methods first saving the difficult ones for secondary reconstruction. The direct closure is not recommended at any time since the ischial bone presses right against the rigid non-vascularized scar and almost every time leads to recurrence [7]. Standard surgical procedure involves regional flaps consisting of fasciocutaneous, muscular or musculocutaneous tissue [8]. Fillet flaps following amputations of the limb are considered as a salvage option [9]. For reconstruction in the ischial region are usually used regional muscle and musculocutaneous flaps which are reliable for their excellent blood supply and durability [10].
At our clinic we mostly use muscles from the posterior thigh (hamstring muscles) or the inferior part of gluteus maximus to cover the bony prominence. On the top of the muscle we use the fasciocutaneous advancement flap. The gluteus maximus flap may not be enough to cover the entire exposed bone in some cases and it needs to be combined with other surgical technique or a different muscle flap must be chosen. The hamstring muscles can be used separately or as a block and they can be either used as V-Y advancement [11] or as a turnover muscle flap [7]. At our clinic when reconstructing large and deep ischiadic pressure ulcers we mostly use the turnover biceps femoris muscle flap. During the surgical procedure the fasciocutaneous posterior thigh flap is lifted, we localize the biceps femoris muscle, detach it from its tendon and dissect to the muscle the major pedicle, which is in literature described 5 cm from the ischial tuberosity [7]. Then we rotate the muscle to the cavity to cover the prominent bone.
The recurrence rate in the literature for reconstruction of pressure ulcers using regional flaps varies from 8.9 to 31% [12]. Among factors contributing to recurrence belong the localization of the pressure ulcer in the ischiatic area and body mass index of the patient [13]. During the one-year follow-up we registered in our study one recurrence which required surgery making the total recurrence rate at 6.25%. Complication rate in the literature varies from 7 to 31% [12] and remains high compared to other surgical procedures [14]. Complications include necrosis, dehiscence, infection, hematoma and others [12]. We registered four partial dehiscence of the wound (25%) and one hematoma (6.25%). All complications were healed conservatively without further surgical procedures.
The re-use of turnover biceps femoris muscle – case study
To illustrate the versatility of the turnover biceps femoris muscle flap we present a basic information from one case of a 42-year-old quadriplegic male with recurrent ischiadic pressure ulcer. Over the years the patient underwent several reconstructions of the ischiadic pressure ulcer including the turnover biceps femoris muscle flap. After admission to our department the standard treatment protocol was initiated including targeted antibiotics therapy, correction of the nutritional status of the patient and X-ray projection of the ischiadic bone, which showed no signs of osteomyelitis. The surgery was performed in prone position with conscious sedation. We used the previous scars to lift up the fasciocutaneous posterior thigh flap and we identified the rotated biceps femoris, which was insufficient to cover the ischiadic bone. After dissection of the biceps femoris muscle (Fig. 1) we sutured the muscle over the ischial tuberosity, but it wasn’t enough to close the defect. Therefore, we identified the semitendinosus muscle (Fig. 2), detached it from its tendon and after the dissection we turned the caudal portion of the muscle over the cranial part and we covered the entire ischiadic defect (Fig. 3). Both rotated muscles were sutured without tension. After that we used the advancement fasciocutaneous flap to create another layer on the top of the muscles and we sutured the skin using the vertical mattress stitches and surgical staples (Fig. 4).
1. Biceps femoris muscle after dissection.
Obr. 1. Musculus biceps femoris po disekci.
2. Semitendinosus muscle dissected and rotated.
Obr. 2. Disekovaný a rotovaný semitendinózní sval.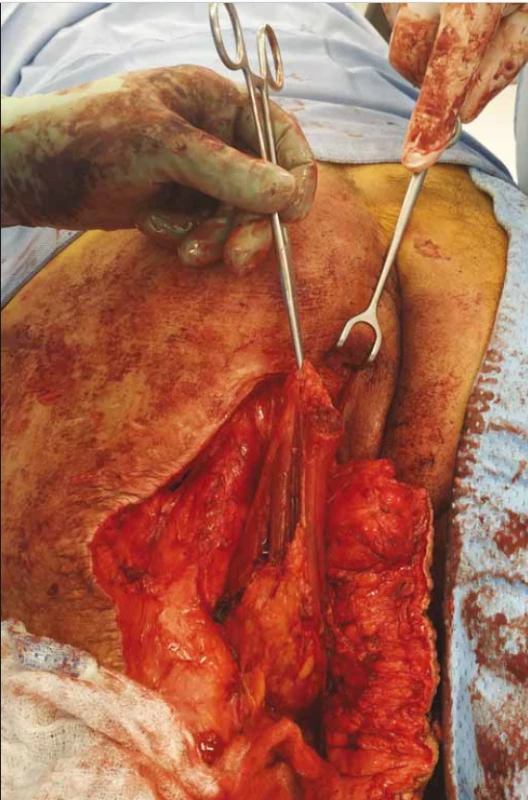
3. Biceps femoris muscle and semitendinosus muscle sutured into the defect.
Obr. 3. Musculus biceps femoris a semitendinózní sval všití do defektu.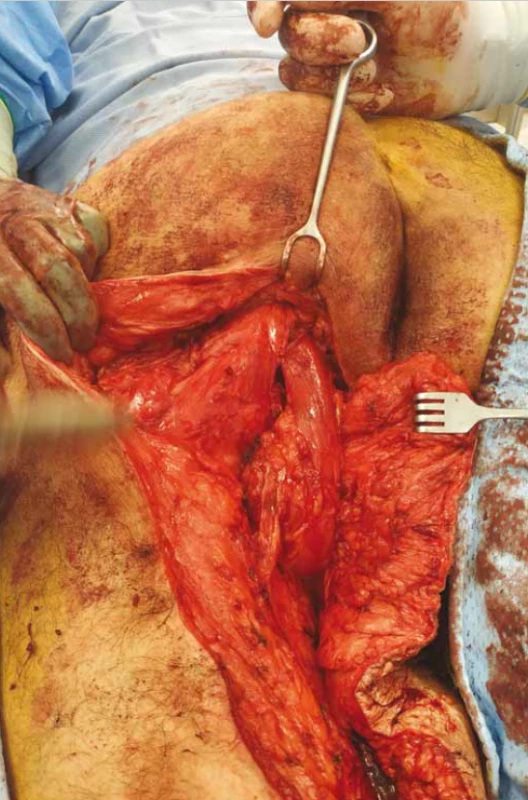
4. Defect covered by fasciocutaneous flap.
Obr. 4. Defekt uzavřen fasciokutánním lalokem.
Conclusion
A recurrent ischiadic pressure ulcer places heavy burden on patients and represent a great challenge for plastic surgeons. The results of our study show the advantages and versatile use of turnover hamstring muscle flap in combination with fasciocutaneous posterior thigh flap. This technique provides enough durable and very well vascularized tissue over the bone prominence and has a preventive effect on the recurrence. In case of failure it can be reused as described in our case report. The recurrence rate of the turnover hamstring muscle flap in our study was low at 6.25% during the one-year follow-up. We believe that the low incidence complication is influenced also by very well-arranged care for patients at our department.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 30. 6. 2019
Accepted for print: 4. 7. 2019
Pavel Rotschein, MD
Clinic of burns and reconstructive surgery
Jihlavská 20
625 00 Brno
Czech Republic
e-mail: rotschein.pavel@fnbrno.cz
Sources
1. Bluestein D, Javaheri A. Pressure ulcers: prevention, evaluation, and management. Am Fam Physician 2008; 78(10): 1186–1194.
2. Edsberg LE, Black JM, Goldberg M et al. Revised national pressure ulcer advisory panel pressure injury staging system. J Wound Ostomy Continence Nurs 2016; 43(6): 585–597. doi: 10.1097/ WON.0000000000000281.
3. Lewandowicz E, Witmanowski H, Sobieszek D. Selection of surgical technique in treatment of pressure sores. Post Dermatol Alergol 2011; 28(1): 23–29.
4. Hokynková A, Šín P, Černoch F et al. Employment of flap surgery in pressure ulcers surgical treatment. Cesk Slov Neurol N 2017; 80/ 113 (Suppl 1): S41–S44. doi: 10.14735/ amcsnn2017s41.
5. Keys KA, Daniali LN, Warner KJ et al. Multivariate predictors of failure after flap coverage of pressure ulcers. Plast Reconstr Surg 2010; 125(6): 1725–1734. doi: 10.1097/ PRS.0b013e3181d51227.
6. Marchi M, Battaglia S, Marchese S et al. Surgical reconstructive procedures for treatment of ischial, sacral and trochanteric pressure ulcers. G Chir 2015; 36(3): 112–116.
7. Demirseren ME, Ceran C, Aksam B et al. Clinical experience with the combination of a biceps femoris muscle turnover flap and a posterior thigh fasciocutaneous hatchet flap for the reconstruction of ischial pressure ulcers. Ann Plast Surg 2016; 77(1): 93–96. doi: 10.1097/ SAP.0000000000000290.
8. Kuo PJ, Chew KY, Kuo YR et al. Comparison of outcomes of pressure sore reconstructions among perforator flaps, perforator-based rotation fasciocutaneous flaps, and musculocutaneous flaps. Microsurgery 2014; 34(7): 547–553. doi: 10.1002/ micr.22257.
9. Kempny T, Holoubek J, Abdelkarim A et al. Postamputation femur reconstruction with an autologous vascularized tibia bone graft. Microsurgery 2019; 39(5): 476–477. doi: 10.1002/ micr.30441.
10. Borgognone A, Anniboletti T, De Vita F et al. Ischiatic pressure sores: our experience in coupling a split-muscle flap and a fasciocutaneous flap in a criss-cross way. Spinal Cord 2010; 48(10): 770–773. doi: 10.1038/ sc.2010.25.
11. Albarah AM. De-epithelialized biceps femoris myocutaneous V-Y advancement flap for ischial bed sore reconstruction. J Plast Reconstr Surg 2012; 36(2): 181–186.
12. Sameem M, Au M, Wood T et al. A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg 2012; 130(1): e67–e77. doi: 10.1097/ PRS.0b013e318254b19f.
13. Antalová N, Pokorná A, Hokynková A et al. Factors influencing recurrence of the pressure ulcers after plastic surgery – retrospective analysis. Cesk Slov Neurol N 2018; 81/ 114 (Suppl 1): S23–S28. doi: 10.14735/ amcsnn2018s23.
14. Kuhfuss I, Cordi A. Reduction of “Dead Space” and “Shear” through flap adhesion may reduce short term complication rates in flap-based reconstruction for Stage IV pressure sores: a retrospective comparison cohort series. J Spine 2016; 5(4). doi: 10.4172/ 21657939.1000318.
Labels
Paediatric neurology Neurosurgery Neurology
Article was published inCzech and Slovak Neurology and Neurosurgery

2019 Issue Supplementum 1-
All articles in this issue
- The knowledge and practises of nurses in the prevention of medical devices related injuries in intensive care – questionnaire survey
- Effectiveness of comprehensive pain management in hard-to heal ulcers – a protocol of systematic review
- Negative wound pressure therapy in treatment of a pressure ulcer in paraplegics
- The use of negative pressure wound therapy for wound complication management after vascular procedures
- Mapping of pressure ulcers and non-healing wounds in medical curriculum
- Quality of life in patient with non-healing wounds
- Pain assessment of surgical wounds after angio-surgical interventions
- Effectiveness of hyperbaric oxygen therapy in non-healing ulcerations – meta-review
- Hyperbaric oxygen therapy in non-healing ulcerations – mechanisms of action, current european recommendations and case report
- Reconstruction of recurrent ischiadic pressure ulcer using turnover hamstring muscle flap
- Oxidative stress in wound healing – current knowledge
- Multidisciplinary approach in surgical pressure ulcer therapy after spinal cord injury
- Key factors for the development of pressure ulcers in surgical practice
- Pilot analysis of pressure ulcers – nationwide data from central adverse event reporting system
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Quality of life in patient with non-healing wounds
- The knowledge and practises of nurses in the prevention of medical devices related injuries in intensive care – questionnaire survey
- The use of negative pressure wound therapy for wound complication management after vascular procedures
- Negative wound pressure therapy in treatment of a pressure ulcer in paraplegics
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

