-
Medical journals
- Career
Extension of the Therapeutic Time Window for Intravenous Thrombolysis Should Not Lead to Prolongation of Door-to-Needle Time
Authors: D. Sanak 1; R. Herzig 1; P. Hubacek 2; M. Král 1; T. Veverka 1; J. Zapletalová 3; D. Skoloudik 1; A. Bártková 1; I. Vlachová 1; P. Kaňovský 1
Authors‘ workplace: Comprehensive Stroke Centre, Department of Neurology, Palacký University Hospital, Olomouc 1; Emergency Department, Palacký University Hospital, Olomouc 2; Department of Biometry and Statistics, Palacký University Medical School, Olomouc 3
Published in: Cesk Slov Neurol N 2011; 74/107(6): 685-688
Category: Short Communication
Overview
Background:
The results of the ECASS III trial and the January 2009 update of the ESO guidelines have permitted extension of the therapeutic time window for intravenous thrombolysis (IVT) from 3 to 4.5 hours after stroke onset. Although the “time is brain” rule remains valid, prolongation of the door-to-needle time (DNT) interval may occur. Our aim was to compare DNT before and after extension of the therapeutic window.Methods:
Sex and age, initial stroke severity (assessed using NIHSS), DNT, and pre-treatment blood pressure (PBP) were observed in two groups of consecutive stroke patients treated within a window of 3 hours (Group 1 – year 2008) and 4.5-hours (Group 2 – year 2009).Results:
The sets consisted of 50 (Group 1) patients (27 males, mean age 69.3 ±10.8 years) and 52 (Group 2) patients (31 males, mean age 68 ±9.2 years). No differences were found in sex and age, initial NIHSS, DNT (p = 0.695) and PBP. No association was found between DNT and either stroke severity or age in the two groups.Conclusion:
In our centre, DNT interval was not prolonged after the extension of IVT therapeutic time window in the year 2009 and was not dependent on stroke severity or patient age.Key words:
ischemic stroke – intravenous thrombolysis – door-to-needle timeIntroduction
The results of the ECASS III trial [1] and the January 2009 update of the European Stroke Organization (ESO) guidelines [2] allowed the extension of the therapeutic time window for intravenous thrombolysis (IVT) from 3 to 4.5 hours after stroke onset. Nevertheless, this substantial prolongation of time window should not lead to the extension of the door-to-needle time (DNT) in respect of the still-valid “time is brain” concept. A meta-analysis of six randomized studies with IVT administered within 6 hours of stroke onset showed that the earlier IVT was performed, the better was the outcome [3].
The aim was to compare DNT before and after the official extension of the IVT therapeutic window.
Subject and methods
In a retrospective single-centre study, the sample group consisted of 102 acute IS patients treated with IVT in the years 2008 and 2009 at our stroke centre, which has a catchment area with a total of approximately 700 thousand people [4]. IVT was performed within 3 hours in the year 2008 [5], and was prolonged to 4.5 hours at the beginning of the year 2009 in accordance with revised ESO guidelines [2].
All patients were admitted to the emergency department (ED) of our hospital and routine data gathered on entrance: blood pressure, electrocardiogram, and blood samples (standard coagulation panel, blood count and serum glycaemia). Clinical status was evaluated using the National Institutes of Health Stroke Scale (NIHSS) assessed by a certified neurologist. A brain-imaging examination followed immediately. All patients then underwent standard IVT directly at ED.
For the purposes of this analysis, patients were divided into two groups: Group 1 (year 2008; patients treated within 3 hours of stroke onset); and Group 2 (year 2009; patients treated within 4.5 hours of stroke onset). Sex and age, initial stroke severity, DNT and onset-to-arrival (OAT) intervals, admission and pre-treatment systolic blood pressure (SBP) were recorded in both groups. The relationship between the DNT and the OAT was analyzed to assess any possible negative correlation that might lead to undesirable prolongation of DNT in the case of very early patient arrival to the hospital.
SPSS software, version 15.0 (SPSS Inc., Chicago, USA) was used for the statistical analysis. The chi-square test was used for group comparison between the sexes. The Mann-Whitney test was used for group comparison (between the years 2008 and 2009) of baseline NIHSS, pre-treatment SBP, DNT and OAT intervals. Spearman‘s correlation analysis was used for the assessment of the relationship between DNT, age and initial stroke severity and also for the assessment of the relationship between DNT and the OAT intervals. Student‘s t-test was used for the comparison of age and admission SBP in the two groups.
Results
Group 1 numbered 50 and Group 2 numbered 52, all of them acute ischemic stroke patients; demographic and baseline characteristics are shown in Table 1. No significant differences between the groups were found in sex (p = 0.567) and age (p = 0.184) distribution, initial NIHSS value (p = 0.867), in DNT (p = 0.695), and OAT (p = 0.350) intervals (Table 1). There was a significant difference in the admission SBP between the groups (p = 0.001), but no difference was found in the pre-treatment SBP (Table 1). No interdependence was found between DNT and either initial stroke severity (r = 0.218; r = 0.161) or age (r = 0.0017; r = 0.055) in the two groups. No significant interdependence was found between DNT and OAT in Group 1 (r = –0.206; p = 0.152) (Fig. 1). In Group 2, a slight significant positive correlation was found between DNT and OAT (r = 0.282; p = 0.042) (Fig. 2). Nine (17.3%) patients were treated within 3 hours in the year 2009 (Table 1). Mean DNT was 47.4 ±7.5 min with a median of 45 min in these patients; it did not differ from DNT in either group. In the year 2008, four patients (8%) had DNT >60 min with a mean DNT of 68 ±6.2 min and eight patients (15.3%) had a mean DNT of 73 ±5.4 min in the year 2009.
Fig. 1. Relationship between door-to-needle time and onset-to-arrival time in Group 1. DNT – door-to-needle time, OAT – onset-to-arrival time 
Fig. 2. Relationship between door-to-needle time and the onset-to-arrival time in Group 2. DNT – door-to-needle time, OAT – onset-to-arrival time 
1. Patient demographics and baseline characteristics. 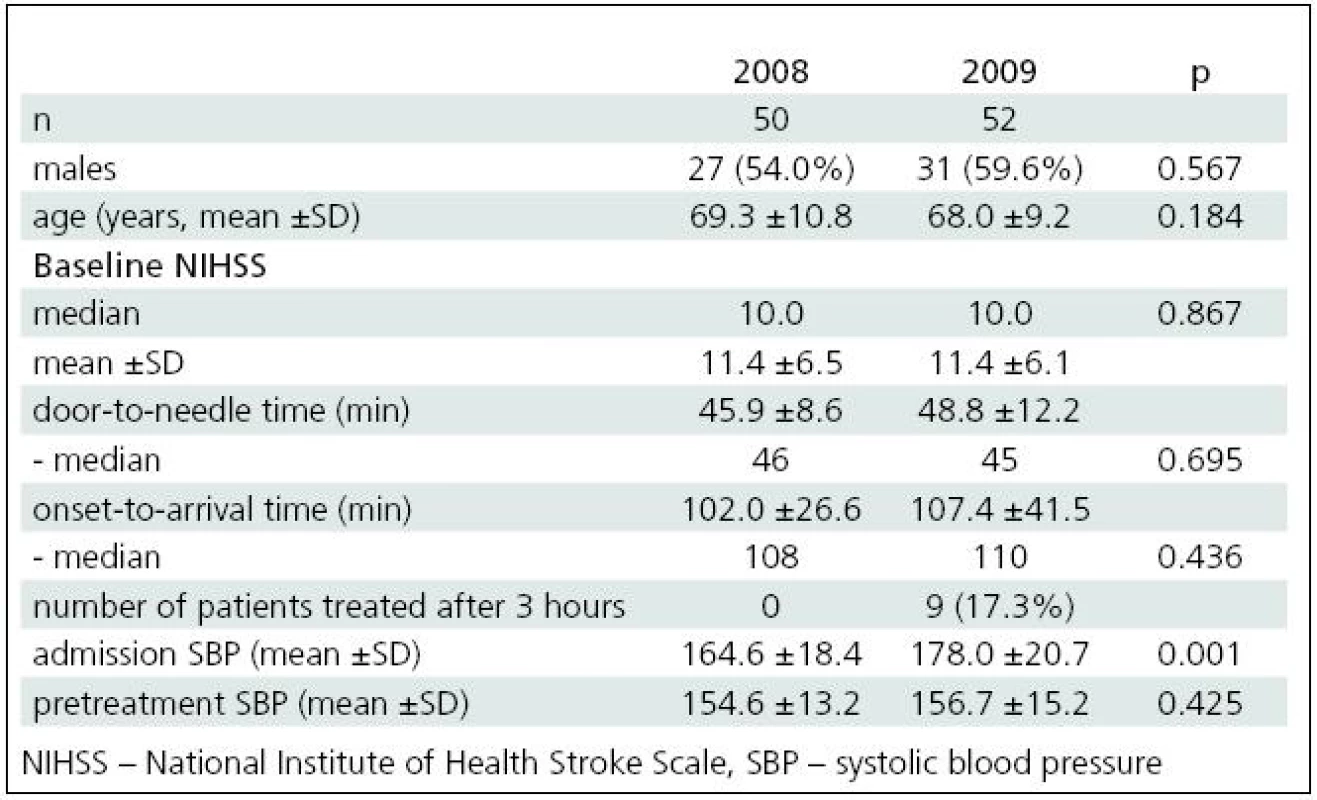
Discussion
The results of the study showed no significant change in DNT after the extension of therapeutic time window for IVT at the beginning of the year 2009. Although the “time is brain” dogma remains valid, one may expect a tendency to prolong DNT after the extension of the therapeutic time window for IVT. Paradoxically, earlier patient hospital arrival may be associated with delayed t-PA administration [6] and could be a potential reason for DNT prolongation. Longer pre-hospital journeys from more distant places, which the extended window now allows, may also contribute to this prolongation. During such longer pre-hospital transportation, patients may develop greater clinical and circulation instability. In some cases, the clinical worsening manifests as, for example, vomiting, which may require longer stabilization before brain imaging. In contrast, a more urgent approach may be expected in younger patients and in patients with severe strokes [7]. Nevertheless, no relationship was observed between DNT and either age or initial stroke severity in this study.
Our finding of a slight significant positive correlation between DTN and OAT in the year 2009 might be explained by a higher number of clinically and haemodynamically unstable patients transferred from more distant places after the extension of the IVT therapeutic window. These patients required longer clinical stabilization before brain imaging. Vomiting and agitation, with insufficient cooperation leading to pharmacological sedation, all consumed time before imaging. Patients also required more aggressive treatment of arterial hypertension before the IVT administration. All of this supports significantly higher mean SBP on admission in the year 2009 (Table 1).
The relatively low number of patients treated with IVT beyond 3 hours in the year 2009 (Table 1) reflects the generally low number of potential candidates for treatment between 3 and 4.5 hours, as also recorded in the ECASS III trial, where 821 patients were enrolled over more than four years from 130 sites in 19 European countries [1].
In the authors’ opinion, every centre performing IVT within a prolonged time window should assess DNT and, in the event of its prolongation, take measures to shorten it, which may lead to improvement in the care of acute stroke. No significant change of DNT after extension of the IVT therapeutic window may be considered a marker for a well organized system of hospital IVT management. In our institution, a special education program was undertaken to avoid possible prolongation of DTN after the extension of therapeutic time window for IVT.
Two study limitations should be mentioned: single centre study design and a relatively low number of patients in the two groups drawn from the catchment area.
Conclusion
In this study, DNT interval was not prolonged after the extension of the IVT therapeutic time window at the beginning of the year 2009 and was not dependent on either initial stroke severity or patient age.
The study was partially supported by a grant from the Ministry of Education of the Czech Republic, ref. no. MSM6198959216.
Daniel Sanak, MD, PhD, FESO
Comprehensive Stroke Centre
Department of Neurology
Palacký University Hospital
I. P. Pavlova 6
775 20 Olomouc
e-mail: daniel.sanak@centrum.cz
Accepted for review: 1. 3. 2011
Accepted for publication: 10. 5. 2011
Sources
1. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D et al. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. N Engl J Med 2008; 359(13): 1317–1329.
2. Update Guidelines January 2009 New Elements. Dostupné z URL: http://www.eso-stroke.org/pdf/ESO_Extended_Thrombolysis_KSU.pdf.
3. Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004; 363(9411): 768–774.
4. Sanak D, Vlachova I, Hubacek P, Weinberg J, Bartkova A, Kral M et al. Single center or multicenter acute stroke care? A comparison of different systems among regions of Czech Republic. Int J Stroke 2008; 3 (Suppl 1): 307.
5. The European Stroke Organization (ESO) Executive Committee and the ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 2008; 25(5): 457–507.
6. Izenberg A, Silver F, Hill M, Kapral M, Casoubon LK, Fang J et al. Earlier hospital arrival in acute stroke is associated with delayed tPA administration. Neurology 2009; 11 (Suppl 3): 102.
7. Maestroni A, Mandelli C, Manganaro D, Zecca B, Rossi P, Monzani V et al. Factors influencing delay in presentation for acute stroke in an emergency department in Milan, Italy. Emerg Med J 2008; 25(6): 340–345.
Labels
Paediatric neurology Neurosurgery Neurology
Article was published inCzech and Slovak Neurology and Neurosurgery

2011 Issue 6-
All articles in this issue
- Surgical Treatment of Brachial Plexus Injury
- Questionnaires of Activities of Daily Living in Patients with Alzheimer Disease
- Parkinsonian Phenotypes – towards New Nosology of Atypical Parkinsonian Syndromes
- Updated Insight into the Pathophysiology of Migraine – an Update
- Motor Aspects of Speech Imparment in Parkinson‘s Disease and their Assessment
- Tractography in Neuronavigation during Intraaxial Brain Tumour Surgery Near Corticospinal Tract
- Amendment of the Czech Addenbrooke’s Cognitive Examination (ACE-CZ)
- Miller Fisher Syndrome – Four Case Reports and Review of Current Concept
- Parkinson’s Disease with a Phenotype of Progressive Supranuclear Palsy – a Case Report
- Cognitive and Emotional Changes Five Years after SAH – a Case Report
- Amisulpride in the Treatment of Schizophrenia
- The Reasons and the Process of Amendment of the Czech Addenbrooke’s Cognitive Examination (ACE-CZ)
- Postural Reflexes in Conditions of Visual Disturbance
- Extension of the Therapeutic Time Window for Intravenous Thrombolysis Should Not Lead to Prolongation of Door-to-Needle Time
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Miller Fisher Syndrome – Four Case Reports and Review of Current Concept
- Updated Insight into the Pathophysiology of Migraine – an Update
- Amendment of the Czech Addenbrooke’s Cognitive Examination (ACE-CZ)
- Surgical Treatment of Brachial Plexus Injury
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

