-
Medical journals
- Career
Distraction osteogenesis in the head and neck region
Authors: Koudstaal Maarten Jan 1; Rupreht Joseph 2; Van Der Wal Karel G. H. 1
Authors‘ workplace: Department of Oral and Maxillofacial Surgery Craniofacial Center, Sophia Children’s Hospital, Erasmus University Medical Center Rotterdam 1; Department of Anesthesiology Craniofacial Center, Sophia Children’s Hospital, Erasmus University Medical Center Rotterdam 2
Published in: Anest. intenziv. Med., 19, 2008, č. 3, s. 139-142
Category: Anaesthesiology - Review Article
Overview
Distraction osteogenesis is a treatment often used in orthopedics and plastic surgery, but more frequently so in maxillofacial surgery. There is a variety of distractors available for use on the different parts of the maxillofacial skeleton. The aim of this article is to give publicity to distraction osteogenesis in the field of oral and maxillofacial surgery and to the different types of intra - and extraoral distractors frequently used in the head and neck region. The application of such distractors for several months while the patient carries on everyday life is potentially hazardous in case of an emergency. The anesthesiological aspects of these devices will be discussed in order to minimize the risks in cases of acute medical interventions.
Keywords:
distraction osteogenesis – maxillofacial surgery – anesthesiological aspects – emergency medicineIntroduction
Distraction osteogenesis (DO) was first described by Codivilla in 1905 [1]. The first publication on the use of DO in a group of patients was written by the orthopedic surgeon Ilizarov in 1990 [2]. The theory of DO consists of the administration of gradual forces on a bone segment after it has been osteomized. These forces are exercised by means of a distractor. A distractor is a device that is in contact with both bony segments and is equipped with a mechanism that can drive the two bony segments apart by means of an activation part. Between the two bony segments new trabecular bone growth occurs that is subsequently turned into bone with a normal mineralized architecture. The end result of the treatment is lengthening of the osteomized bone. When the desired lengthening has been reached the distractor is kept in situ for 6–12 weeks to allow the new bone to adjust to the new stable situation.
DO is used in orthopedic surgery, plastic surgery, and in oral and maxillofacial surgery. For DO there are different indications. For the regular movement of bone parts a normal osteotomy will suffice. However, when the bone has to be moved over a greater distance, distraction will sometimes be the solution. In these situations the bone is gradually moved and this allows also the soft tissues (ligaments, vessels, nerves, muscles, and sometimes the scar tissues) to stretch gradually, the so-called “histiogenesis”. If there is a shortage of bone in case of a normal osteotomy, the situation can be resolved by using an autologous bone transplant. DO has the advantage that there is no need for a donor site to increase the amount of bone.
There are several different distractors for the use on different areas of the facial skeleton. They vary in function, size, and the site where they are used.
The aim of this article is to increase the knowledge on DO in the head and neck region and the various different distraction devices. The specific indications and therapies for the individual cases will not be discussed.
Attention will be given to the fact that these distractors remain in situ for several months while the patient carries on everyday life. This leads to a risk when the patient has to be treated for an emergency, for example in case of an accident, a facial abscess or bleeding in the mouth. The general practitioner or the anesthesiologist is then confronted with an unfamiliar situation. The anesthesiological considerations on distractors in the head and neck region will be discussed.
The distractors
DO is used in the field of oral and maxillofacial surgery to lengthen or to move a bone over a certain distance, which would not be possible with a regular osteotomy. Many different distractors are available for a range of different treatment modalities. Depending on the intended result distractors can be placed intra - and extraorally. The authors realize it is impossible to discuss every available distractor, but the most widely used types of distractors and their normal anatomic locations will be reviewed.
Extraoral distractors are connected to the bone segments transcutaneously or through the opening of the mouth. In most cases the actual moving parts of the distractors are located externally and are connected to the bone with transcutaneous pins (Fig. 1). These distractors are used to lengthen the mandible in cases of hypoplasia. The advantage of these devices is the fact that they are easily placed, activated, aimed, and removed. The disadvantage is the unaesthetic scar the transcutaneous pins will cause during the distraction.
Image 1. An example of a standard extraoral distractor for lengthening the mandible 
A second type of extraoral distractor is the Rigid External Distractor (RED). The RED is used to move the maxilla at the LeFort I, II, and III level. These devices are fixed to the bone of the skull with a facial frame and pins. Through a titanium frame that is located in front of the patient’s face, the device has a connection with the bone segments that need to be displaced (Fig. 2).
Image 2. The Rigid External Distactor (RED) system in situ on a patient with a bilateral cleft-lip-alveolus and palate for advancing the hypoplastic maxilla 
Along with the extraoral devices, intraoral devices are also used. They are designed for a variety of therapies ranging from lengthening the mandible, widening the maxilla, or heightening the alveolar process of the mandible or maxilla for dental implant placement. The advantages of the internal device is that there is no extraoral scarring and no need for placement on the outside of the head of the patient, thereby making them more comfortable in daily life. The disadvantages are that they are more troublesome to place, aim, and remove.
There are different distractors that are located on the palate for widening the maxilla. The Hyrax expander is the oldest and most widely used tooth-borne device that is placed by the orthodontist. There are also several bone-borne devices that are placed by the surgeon during the operation. Some are fixed to the palate with screws. The Transpalatal Distractor (TPD) was developed in 1999 and is placed on the palate by screw fixation [3]. The Rotterdam Palatal Distractor (RPD), a bone-borne device without screw fixation was engineered in 2004 (Fig. 3).
Image 3. The Rotterdam Palatal Distractor (RPD), a bone-borne distractor for widening the narrow maxilla 
There is also a range of devices available for widening the narrow mandible. One of these is also a kind of tooth-borne Hyrax expander that is placed lingually. The different bone-borne distractors are all bucally positioned with the activation part on the inside of the lower lip. To illustrate an example the Trans Mandibular Distractor is chosen (TMD) (Fig. 4).
Image 4. Trans Mandibular Distractor (TMD), a bone-borne distractor for widening the narrow mandible 
There are several standard and custom build distractors available for lengthening the different regions of the mandible. These are placed submucosally and only their activation part sticks out in the oral orifice through the mucosa. (Fig. 5a and 5b). These types of distractors are used in cases of uni - or bilateral mandibular hypoplasia.
Image 5. 5a and 5b. Submucosally positioned intraoral distractor 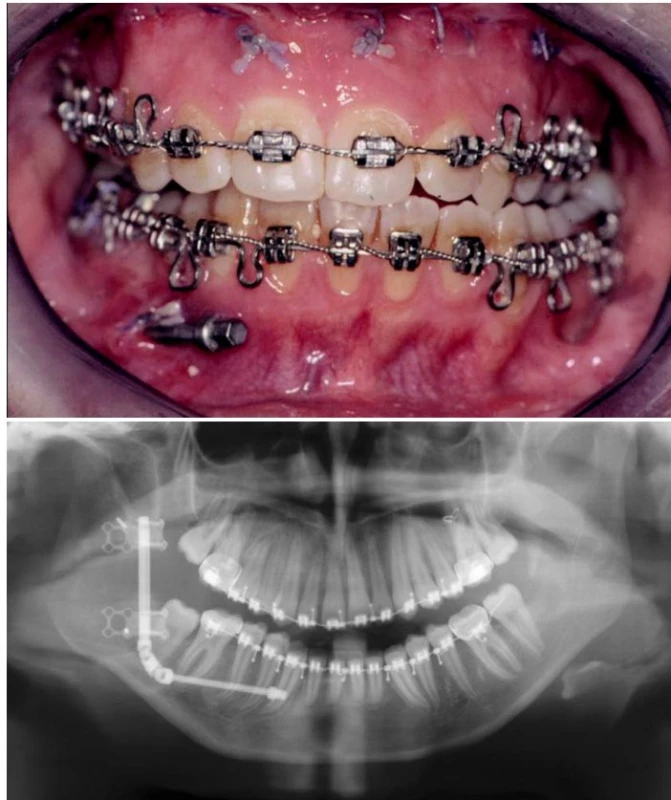
To complete our list of mandibular distractors the custom-build devices for lengthening the mandible in the sagittal direction in newborns should be mentioned. The indication for this therapy is a compromised airway in children with extreme micrognathia. An example is the Treacher Collins syndrome, an autosomal dominant deformity. The malformation is mainly limited to the face and is usually bilateral and symmetric. There is an underdevelopment of the mandible (micrognathia) which can lead to breathing and feeding difficulties. By moving the frontal part of the mandible anteriorly, the base of the tongue is also moved forward and this facilitates the breathing. In most of these cases, the tracheostoma can be removed and/or the hospital stay at the intensive care with or without ventilation can be shortened (Fig. 6).
Image 6. Specific intraoral distractor on a patient with the Treacher Collins syndrome 
In the area of implantology, distractors are used to solve the problem of the shortage of bone in the alveolar process of the maxilla or mandible. An advantage of this therapy is the presence of histiogenesis. The distraction is directed in a vertical dimension thereby heightening the level of the alveolar process to facilitate the placement of dental implants.
Anesthesiological aspects
Some intra - and extraoral distractors can complicate access to the larynx and trachea. In one of our elective surgery cases, the intubation was difficult due to the fact that the distractor on the palate of the patient was obstructing the insertion of the laryngoscope. We advice the anesthesiologists to check the access of the larynx before administering the hypnotic and relaxant and also before the extubation at the end of the procedure. When reintubation is expected to be very difficult one should consider delaying the extubation and should follow the guidelines for rigid intermaxillary fixation.
More complicated are the emergency cases when ventilation of the patient with the facial mask may prove impossible or when intubation or placement of a laryngeal mask is difficult or not feasible. The situation certainly becomes very dangerous when facial trauma occurs to patients wearing distractors. When distractors inhibit proper oxygenation, the distractors should be removed immediately and all parts of the device carefully collected.
When it is not possible to quickly remove the distractor, the alternatives for intubation are fiberscopic intubation or the use of the light wand (“Trachlight”). One should be prepared to perform an emergency tracheotomy. Such emergencies may seem rare but there are potentially life threatening. This is why they deserve the attention of emergency medical personnel and anesthesiologists.
Discussion
In the field of the oral and maxillofacial surgery, distraction osteogenesis is increasingly used in recent years. For several indication areas, where there used to be no treatment, or the treatment consisted of extensive surgery or transplantation of autologous bone, distraction is currently used. For all these different indications, there is a variety of distractors available and every year new devices are developed.
Most of these distractors barely interfere with the patient’s day-to-day activities. Some types, however, do interfere with the patient’s life for several months. In addition, the presence of the distractor itself might bear a risk for the patient. If these patients are in need of emergency medical assistance during this period and the patient needs intubation, the device itself can lead to unexpected and unwelcome surprises for the treating physicians. In the searched literature (Pubmed, Cochrane library), no studies were found that discuss this risk. In most situations the distractors do not interfere with the access of the airway. A number of distractors, however, do pose a risk in cases of an emergency intubation. Especially the RED (see Fig. 2) and the mandibular distractors in the newborns (see Fig. 6) lead to reasonable impairment of the accessibility of the mouth and oropharynx. In these cases the distractor most likely needs to be removed to make access and intubation possible. It is therefore necessary that the patient and their families are properly informed about what to do in case of emergency, and especially about how to remove the device. Some of the other devices can inhibit the use of the laryngoscope, especially the ones that are positioned in the palate. The intra - and extraoral distractors that are used to lengthen the mandible, in combination with the performed osteotomy lead to a compromised mouth opening. This impairment will no longer be present after the administration of muscle relaxants.
It should also be noted that many of the patients on whom distraction osteogenesis is performed suffer from craniofacial anomalies which are often accompanied by impaired mouth opening. Intubation of such patients is complicated even more by the presence of a distractor.
Conclusion
Distraction osteogenesis is a therapy used in the oral and maxillofacial surgery for correction of anomalies of the craniofacial skeleton. In addition to the advantages of DO, this treatment also induces several risks. The patient carries the device for several months, and might be in need of elective or emergency medical treatment, for example in cases of a trauma, an abscess, or bleeding. In some cases the distractors should be removed to make intubation possible. When removal of the distractor is impossible while the patient is in respiratory distress, an emergency tracheotomy must be performed. Well-informed medical personnel, familiar with the presence and the potential risks of the distractors, will be able to handle such acute medical care scenarios better.
Došlo 20. 11. 2007.
Přijato 6. 1. 2008.
Address of correspondence:
Maarten J. Koudstaal
Department of Oral and Maxillofacial Surgery
Erasmus University Medical Center Rotterdam
Gravendijkwal 230, 3015 CE Rotterdam
The Netherlands
e-mail: m.koudstaal@erasmusmc.nl
Sources
1. Codivilla, A. On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. Am. J. Orthop. Surg., 1905, 2, p. 353.
2. Ilizarov, G. A. Clinical applications of the tension-stress effect for limb lengthening. Clin. Orthop., 1990, 250, p. 8–26.
3. Mommaerts, M. Y. Transpalatal distraction as a method of maxillary expansion. Brit. J. Oral. Maxillofac. Surg., 1999, 37, p. 268–272.
Labels
Anaesthesiology, Resuscitation and Inten Intensive Care Medicine
Article was published inAnaesthesiology and Intensive Care Medicine

2008 Issue 3-
All articles in this issue
- Selektivní intubace dětí tracheální rourkou UniventR
- Distraction osteogenesis in the head and neck region
- Hemoragicko-traumatický šok po teroristickém útoku – léčba v Polní nemocnici Armády České republiky ROLE II+, Kábul
- Možnosti prevence nozokomiální pneumonie ventilovaných nemocných – aktuální stav
- Možnosti antikoagulačního zajištění metod mimotělní náhrady funkce ledvin u kriticky nemocných
- O výzkumné činnosti v oboru anesteziologie a resuscitace v druhé polovině dvacátého století
- Anaesthesiology and Intensive Care Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Hemoragicko-traumatický šok po teroristickém útoku – léčba v Polní nemocnici Armády České republiky ROLE II+, Kábul
- Selektivní intubace dětí tracheální rourkou UniventR
- Možnosti prevence nozokomiální pneumonie ventilovaných nemocných – aktuální stav
- O výzkumné činnosti v oboru anesteziologie a resuscitace v druhé polovině dvacátého století
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

