-
Medical journals
- Career
SUBACUTE ARTERIAL BLEEDING AFTER SIMULTANEOUS MASTOPEXY AND BREAST AUGMENTATION WITH IMPLANTS: CASE REPORT
Authors: S. Vikšraitis 1; E. Zacharevskij 1,2,3; G. Baranauskas 3
Authors‘ workplace: SV Plastic Surgery Center, Kaunas, Lithuania 1; Lithuanian University of Health Sciences Hospital, Plastic and Reconstructive Surgery Department, Kaunas, Lithuania 2; Lithuanian University of Health Sciences, Medical Academy, Kaunas, Lithuania 3
Published in: ACTA CHIRURGIAE PLASTICAE, 59, 2, 2017, pp. 92-96
INTRODUCTION
Breast augmentation surgery with implants is performed when breasts are small, underdeveloped or wilted after breastfeeding, or for shape improvement in case of asymmetries, in order to increase self-confidence1. Breast shape, size, and appearance is influenced by many factors, the most important of them being age, heredity, weight changes, pregnancy, sun exposure, physical activity, and congenital disease. Breast implants are also used to restore the breast after mastectomy, sex reassignment surgery, etc. Like any other operation, this procedure also has its general risks. However, some complications like bleeding to the lodge of the implant after surgery, infection, fluid accumulation around the implant, capsular contracture, implant rotation, and implant rupture are specific to this procedure2,3. In this case, subacute spontaneous arterial bleeding occurred. This type of postoperative complication is very rare because after almost 40 years from the first publication of spontaneous bleeding after breast augmentation with implants4, not more than 20 clinical cases have been presented5. This case report presents a description of a subacute hematoma after breast augmentation with silicone implants, which occurred 5 weeks after the surgery.
CASE REPORT
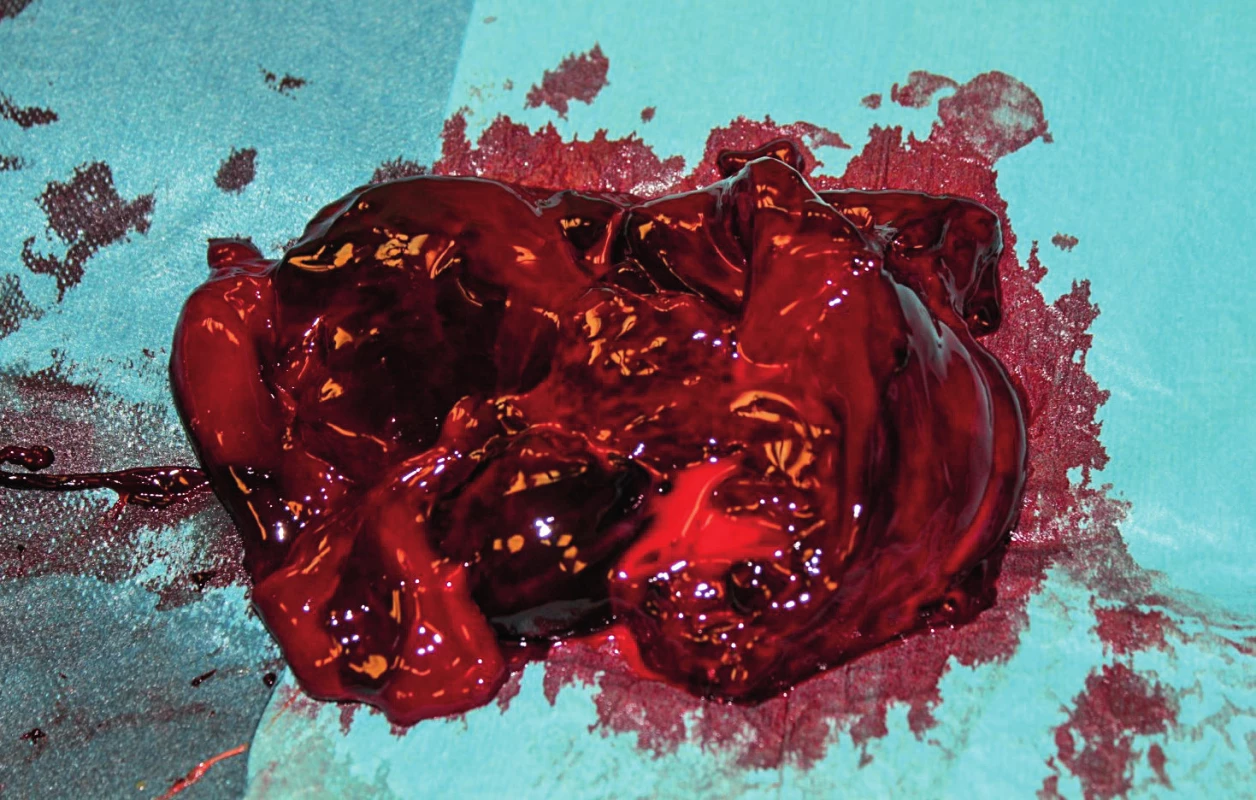
A 27-year-old woman applied for a breast reshaping surgery for aesthetic purposes. There were no other complaints in her medical history. The patient underwent simultaneous mastopexy according to classical Lejour vertical scar technique and breast augmentation surgery using round silicone (Allergan) TSF – 415 mL implants under the pectoral muscle and a breast lift under general anesthesia (Fig. 1). During the operation proper hemostasis was achieved using electrocoagulation. Drains were removed next day after the operation with minimum serohemorrhagic fluid volumes. The subsequent postoperative period was also uneventful. The patient was discharged from the clinic on the second day after the surgery. Five weeks after the operation the patient arrived to the clinic because of tenderness and swelling of the right breast. The patient stated that she had not sustained any traumas. During clinical examination, the upper right breast area was found to be significantly swollen and firm (Fig. 2). Ultrasound examination showed a 2.5 cm heterogeneous strip of fluid accumulated around the implant (Fig. 3). The implant was intact. Complete blood count showed an increased amount of leukocytes, and red blood cells and hemoglobin were at the lower limit of the normal level. No coagulopathies were found. The patient was taken to the operating room where she underwent revision surgery. The purpose was to remove the fluid and to find and stop the cause of its accumulation. During the operation (Fig. 4), a blood clot of 650 mL was removed (Fig. 5). Bleeding from one of the internal mammary artery branches in the implant pocket between the rib cage and the pectoral muscle lower pole was detected and stopped. After the revision, the implant was returned to the lodge. Vacuum drainage was used for one day only. One year after the surgery, there was no recurrence of bleeding, and there was no clinical evidence of the implant capsule contracture formation found either. (Fig. 6).
1. Patient before the operation 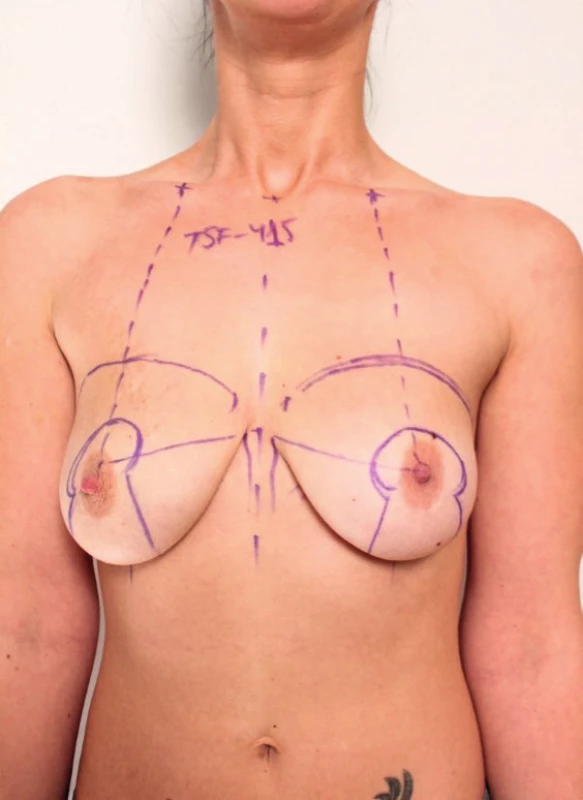
2. Hematoma of the right breast showing gross enlargement. Preoperative view 
3. Ultrasound evaluation showing liquid accumulation 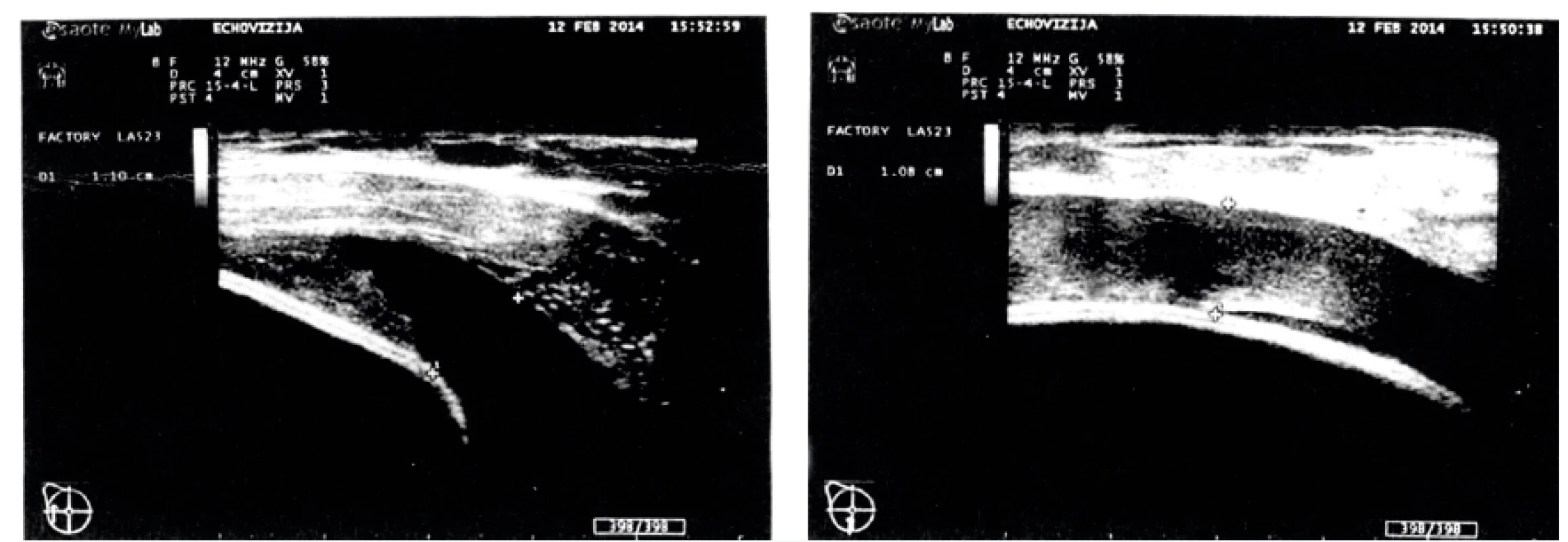
6. Patient 2 weeks (a) and twelve months (b) after a revision surgery 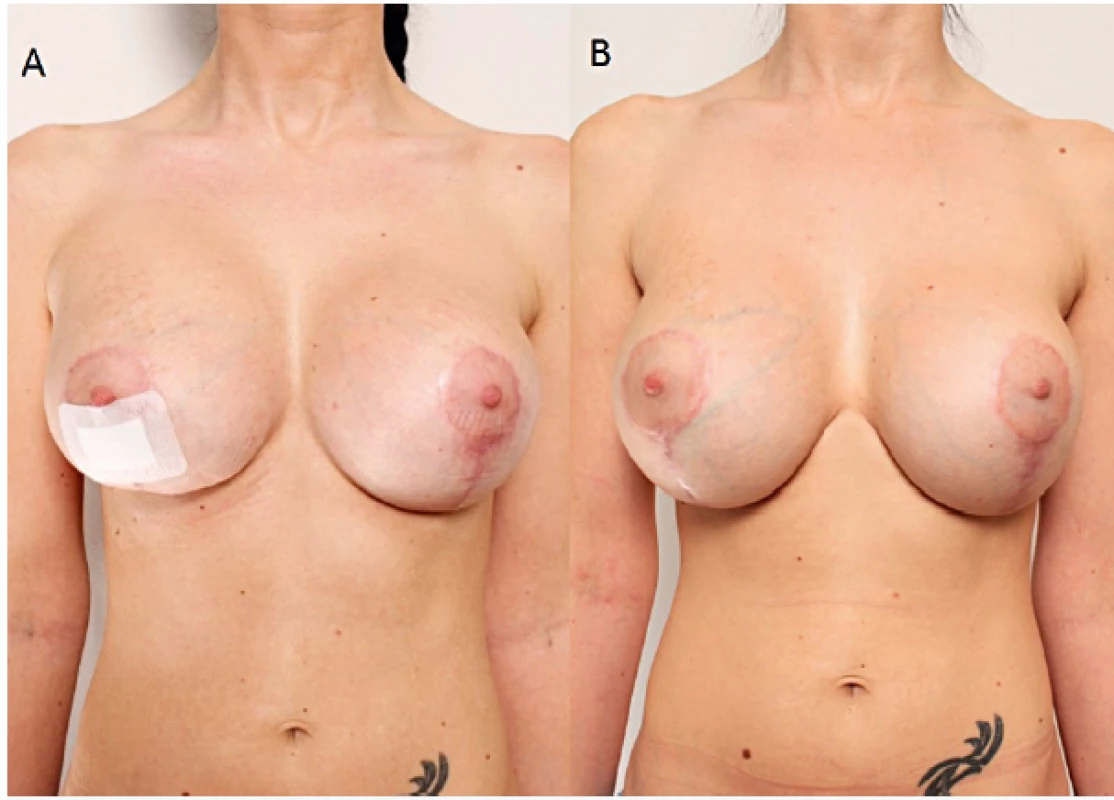
DISCUSSION
Breast augmentation with implants may lead to early or late complications, bleeding being one of the early complications6,7. Bleeding control is number one priority for any surgeon. Hematoma as a complication of breast enhancement with implants usually occurs within three days after the surgery8, and its incidence is 2% to 10.3% of all breast augmentation operations4, 9–12. We presented a case of a subacute hematoma appearing five weeks after the surgery. Hematomas occurring after breast augmentation are classified into three groups: acute hematomas appear from 3 to 7 days after the surgery, subacute hematomas occur from 7 days up to 3 to 5 months after augmentation, and late hematomas appear 3–5 months or more after mammoplasty15. The cause of acute hematoma after breast augmentation with implants may be inadequate hemostasis during surgery or a congenital, acquired or drug-caused coagulation disorder. Trauma is also one of the factors. The first reported case of a late hematoma was published in 1979 by Georgiade et al.4. Hematoma appeared 2.5 years after the surgery. Authors suggested that the cause of bleeding was a large dose of corticosteroids used in the saline implant. In 2002, Hsiao et al. reported two cases on late hematomas10. The first one occurred two years after the surgery, and the second one – a year postoperatively. In both cases, saline-filled, textured silicone prostheses without corticosteroids were used. The cause of the bleeding was only identified in the second patient – neovascularization on the inner surface of the capsule was found. It is thought that mechanical friction between the textured surface of the implant and the high vascular capsule may result in an intracapsular hematoma. In 2009, McArdle and Layt described a case of a late hematoma, which occurred 12 months postoperatively13. Gel-filled implants were used in this patient. Operative examination showed no signs of bleeding. Supposedly, the subsequent traumatization of the new neovascularized capsule might have been the cause of the late hematoma9. In 2014, Peters et al. hypothesized after examining 5 patients with a late unilateral hematoma that bleeding was associated with microfractures in the implant capsule14. The histological analysis of the capsules showed that there was episodic bleeding and reorganization of the hematoma, and the vascular spasm of the damaged vessel was impossible because of the rigidity of the capsule. Late hematomas after breast augmentation with implants also occur because of a sudden rupture of the implant and the capsule, usually – due to the effect of an external force. An increasing chronic hematoma may appear when chronic inflammatory processes are active, the friction force between the surface of the implant and capsule is high, manifestations of coagulopathies are seen, there is a probability of capillary damage because of the rigidity of the capsule, or steroids are used. Nasr et al. reported a case of a subacute hematoma that developed three weeks after the augmentation mammoplasty15. In this case, mild physical stress was sufficient to trigger bleeding from a branch of the internal mammary artery because it was eroded by the friction between the implant and the vessel. In our case, the cause that triggered bleeding was unknown. The patient denied trauma, use of anticoagulants or a history of any coagulopathies. Classical Lejour vertical scar technique for the breast lifting affects skin, subcutaneous fat and glandular tissues16, but there is no influence to the pectoral muscle and its vascularization. In our case no suspension sutures were performed to the muscle underneath. Damaged bleeding artery was found in the implant pocket under the muscle in the border where the lower internal pectoral muscle pole attaches to the ribs and sternum. If the artery was on tension even a slight displacement of the implant in condition of a scar formation could have made damage. Also this theory makes sense with big and high profile silicone implants because of the mechanical tension to the muscle and other tissues. We believe that the treatment tactics for acute and subacute hematomas after breast augmentation with implants should be revision surgery – an inframammary incision with subsequent evacuation of the hematoma, followed by identification and elimination of the source of bleeding. A bacterial culture test is useful for prophylactic antibiotic therapy after surgery. Drainage to reduce the risk for complications should be carried out17. As for late hematoma, the procedure is the same, except for the histological examination of the capsule tissue; replacement of the implant is questionable.
CONCLUSIONS
Subacute hematoma after breast augmentation with implants is an extremely rare complication in esthetic surgery. The technique used for breast augmentation and mastopexy could be one of the reasons for bleeding. History of trauma or use of specific pharmaceuticals also could not be ruled out. However, most of the times the etiology of bleeding is unknown. This type of complication requires surgical treatment. We recommend that each case of late and subacute hematomas after breast augmentation with implants should be described and published for a scientific evaluation of this complication.
Conflict of interest: The authors have no conflicts of interest to declare.
Funding: No funding has been received for this report.
Ethical standard: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The patient gave her informed consent prior to her inclusion in this case report. Any details that might disclose the identity of the patient under study were excluded.
Acknowledgments: The authors thank lecturer Irmantas Ramanauskas from Lithuanian University of Health Sciences Department of Languages and Education for his English proofreading.
Author’s contribution: All authors participated in the research, and have reviewed and agree with the content of the article.
Corresponding author:
Ernest Zacharevskij, M.D.
SV Plastic Surgery Center
Savanorių Ave.75, LT-44208 Kaunas
Lithuania
E-mail: ernest.zacharevskij@gmail.com
Sources
1. Ramachandran K. Breast augmentation. Indian J Plast Surg. 2008 Oct;41(Suppl):S41-7.
2. Gabriel SE, Woods JE, O‘Fallon WM, Beard CM, Kurland LT, Melton LJ 3rd. Complications leading to surgery after breast implantation. N Engl J Med. 1997 Mar 6;336(10):677-82.
3. Erian A, Shiffman MA. Complications of breast augmentation. In: Shiffman MA, Di Giuseppe A (Eds.) Body Contouring, Springer, New York, 2010, p. 93-117.
4. Georgiade NG, Serafin D, Barwick W. Late development of hematoma around a breast implant, necessitating removal. Plast Reconstr Surg. 1979 Nov;64(5):708-10.
5. Seth AK, Kim JY. Acute symptomatic hematoma with defined etiology seven years after breast reconstruction: A case report and literature review. Can J Plast Surg. 2010 Summer;18(2):e27-9.
6. Veiga DF, Filho JV, Schnaider CS, Archangelo I Jr. Late hematoma after aesthetic breast augmentation with textured silicone prosthesis: a case report. Aesthetic Plast Surg. 2005 Sep-Oct;29(5):431-3; discussion 434.
7. Marques AF, Brenda E, Saldiva PH, Andrews JM. Capsular hematoma as a late complication in breast reconstruction with silicone gel prostheses. Plast Reconstr Surg. 1992 Mar;89(3):543-5.
8. Brickman M, Parsa NN, Parsa FD. Late hematoma after breast implantation. Aesthetic Plast Surg. 2004 Mar-Apr;28(2):80-2. Epub 2004 Jun 1.
9. van Rijssen AL, Wilmink H, van Wingerden JJ, van der Lei B. Amorous squeezing of the augmented breast may result in late capsular hematoma formation: A report of two cases (and a review of English-language literature on late hematoma formation in the augmented breast). Ann Plast Surg. 2008 Apr;60(4):375-8.
10. Hsiao HT, Tung KY, Lin CS. Late hematoma after aesthetic breast augmentation with saline-filled, textured silicone prosthesis. Aesthetic Plast Surg. 2002 Sep-Oct;26(5):368-71.
11. Daw JL, Lewis VL, Smith JW. Chronic expanding hematoma within a periprosthetic breast capsule. Plast Reconstr Surg. 1996 Jun;97(7):1469-72.
12. Görgü M, Aslan G, Tuncel A, Erdogan B. Late and long-standing capsular hematoma after aesthetic breast augmentation with a saline-filled silicone prosthesis: A case report. Aesthetic Plast Surg. 1999 Nov-Dec;23(6):443-4.
13. McArdle B, Layt C. A case of late unilateral hematoma and subsequent late seroma of the breast after bilateral breast augmentation. Aesthetic Plast Surg. 2009 Jul;33(4):669-70.
14. Peters W, Fornasier V, Howarth D. Late unilateral hematoma after breast augmentation. Plast Surg (Oakv). 2014 Spring;22(1):18-21.
15. Nasr MW, Stephan HA, Sleilati FH, Hokayem NE. Subacute hematoma after augmentation mammaplasty: case report. J Plast Reconstr Aesthet Surg. 2009 Dec;62(12):e611-2.
16. Spear SL, Davison SP, Ducic I. Superomedial pedicle reduction with short scar. Semin Plast Surg. 2004 Aug;18(3):203-10.
17. Gherardini G, Zaccheddu R, Milner SM, El-Shazlyl M, Liapakis I. Breast augmentation with silicone implants: the role of surgical drainage – report on 502 consecutive patients. Eur J Plast Surg. 2006;29(1):9-12.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2017 Issue 2-
All articles in this issue
- Editorial
- COMPLICATIONS OF LOWER EXTREMITY HEMATOMAS IN PATIENTS WITH PRE-INJURY WARFARINE USE
- SURGICAL CORRECTION OF LABIA MINORA HYPERTROPHY, A PERSONAL TECHNIQUE
- SUTURE VERSUS FIBRIN GLUE MICRONEURAL ANASTOMOSIS OF THE FEMORAL NERVE IN SPRAGUE DEWLY RAT MODEL. A COMPARATIVE EXPERIMENTAL ASSESSMENT OF THE CLINICAL, HISTOLOGICAL AND STATISTICAL FEATURES
- INTRAOPERATIVE FAT GRAFTING INTO THE PECTORALIS AND LATISSIMUS DORSI MUSCLES-NOVEL MODIFICATION OF AUTOLOGOUS BREAST RECONSTRUCTION WITH EXTENDED LATISSIMUS DORSI FLAP
- HAS A GLOMUS TUMOR ALWAYS A QUICK DIAGNOSIS?
- CURRENT CONCEPTS IN PERIPHERAL NERVE INJURY REPAIR
- SUBACUTE ARTERIAL BLEEDING AFTER SIMULTANEOUS MASTOPEXY AND BREAST AUGMENTATION WITH IMPLANTS: CASE REPORT
- AUTOLOGOUS FAT TRANSFER, BREAST LIPOMODELLING AND FAT TRANSFER TO THE FACE: CURRENT GOLD STANDARDS AND EMERGING NEW DATA
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- SURGICAL CORRECTION OF LABIA MINORA HYPERTROPHY, A PERSONAL TECHNIQUE
- INTRAOPERATIVE FAT GRAFTING INTO THE PECTORALIS AND LATISSIMUS DORSI MUSCLES-NOVEL MODIFICATION OF AUTOLOGOUS BREAST RECONSTRUCTION WITH EXTENDED LATISSIMUS DORSI FLAP
- COMPLICATIONS OF LOWER EXTREMITY HEMATOMAS IN PATIENTS WITH PRE-INJURY WARFARINE USE
- HAS A GLOMUS TUMOR ALWAYS A QUICK DIAGNOSIS?
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career