-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
RADIATION MACULOPATHY AFTER ONE-DAY SESSION STEREOTACTIC RADIOSURGERY IN PATIENTS WITH CILIARY BODY AND CHOROIDAL MELANOMA
Authors: P. Zahorjanová 1; A. Furdová 2; I. Waczulíková 3; M. Šramka 4; G. Králik 5; M. Štubňa 1
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 1, p. 3-10
Category: Původní práce
doi: https://doi.org/10.31348/2019/1/1Summary
Introduction: Nowadays radiotherapy is the standard treatment care for patients with uveal melanoma. In Slovakia the only one option is a one-day session stereotactic radiosurgery at linear accelerator LINAC. Irradiation of surrounding tissues of the eye and orbit causes radiation complications. One of the most serious and vision-threatening is the radiation retinopathy, which divides into maculopathy and peripheric retinopathy. The clinical signs include microanerysms, teleangiectases, hard exsudates, cotton wool spots and macular edema, neovascularisation, and vitreous hemorrhage. Radiation macular edema can be classified by optical coherence tomography into cystoid or noncystoid edema. On fluorescein angiography macular edema is divided into non-ischemic and ischemic, while the latter means usually irreversible loss of the visual acuity. This paper is focused on risk factors of radiation retinopathy although it strongly influences functional result of radiotherapy and preservation of the visual acuity.
Purpose: By means of bivariate and multivariate analysis to determine the association of radiation dose and other variables with the development of radiation maculopathy.
Material and methods: The retrospective analysis of 168 patients with ciliary body or choroidal melanoma who performed one-day session stereotactic radiosurgery on a linear accelerator LINAC in a period 2007–2016.
Results: The prevalence of the radiation maculopathy was 29% with the median time from the irradiation to maculopathy 16 months. Median radiation dose on the macula was 37 Gy. Variables statistically significantly associated with the maculopathy were: radiation dose (p = 0.0016), postequatorial location of the tumor (p = 0.0271) and better visual acuity before treatment (p = 0.0007). The tumor touch of the macula was strongly associated with the visual acuity in the bivariate analysis (p = 0.0006), thus it could be omitted from the final model.
Discussion: The radiation dose on a macula is the key determinant for radiation-induced maculopathy, according to other authors and our study approvingly. Other variables were related to proximity of the tumor to the macula, so the radiation dose on the macula was higher indirectly. Better visual acuity before treatment as a risk factor for maculopathy can be a consequence of: a) earlier diagnostics of tumor with proximity to the posterior pole, b) lower enucleation rate; frequency of the enucleation was 1.6 higher in patients without maculopathy. Naturally, on enucleated eyes maculopathy was not diagnosed. Five patients underwent intravitreal application of the bevacizumab as a treatment of the radiation maculopathy, without improvement of the visual acuity.
Conclusion: Radiation complications can be vision and eye threatening. Radiation maculopathy is a consequence of higher radiation dose on the macula. The treatment modalities of radiation maculopathy are rather ineffective.
Keywords:
uveal melanoma – one-day session stereotactic radiosurgery – radiation maculopathy
INTRODUCTION
The current trend in the treatment of malignant melanoma of the uvea is radiotherapy, which by contrast with radical surgical treatment (enucleation) enables the preservation of the eyeball and sometimes even preservation of central visual acuity to a certain degree. With regard to the fact that the number of patients who suffer from this disease is relatively low (approximately 30-50 newly diagnosed cases per year in Slovakia), the treatment of this pathology is centralised. In Slovakia, the only possibility is stereotactic radiosurgery on a LINAC linear accelerator, which patients undergo at the Oncological Institute of St. Elizabeth in Bratislava, in co-operation with the Department of Ophthalmology at the Faculty of Medicine, Comenius University and Ružinov University Hospital, Bratislava [4, 5].
In connection with radiation therapy, we encounter adverse effects of irradiation on the surrounding tissues. Erythema to desquamation of the skin may appear on the eyelids following irradiation, and loss of the eyelashes and eyebrows may be either temporary or permanent. After higher doses of radiation, there is a danger of change of the position of the eyelids. Conjunctivitis and chemosis of the conjunctiva are acute consequences of radiation, while it is more difficult to manage chronic dry-eye syndrome following a loss of goblet cells. After radiotherapy a common manifestation is corneal erosion, while a worse complication is keratitis and the formation of ulcers.
One of the most serious consequences of post-radiation complications on the anterior segment of the eye is neovascular glaucoma, which is also one of the main reasons for subsequent secondary enucleation. Radiation cataract can now be managed elegantly by means of a microsurgical solution. On the posterior segment of the eye, later complications of irradiation include radiation retinopathy and radiation optic neuropathy.
Radiation retinopathy is divided into maculopathy and peripheral retinopathy. It was first described in 1933. It is manifested clinically as microaneurysms, teleangiectasias, hard exudates, cotton wool spots and macular edema, neovascularisation and vitreous haemorrhage. After exposure to ionising radiation, first of all a loss of endothelial cells takes place, with a relative preservation of pericytes. There is a hypothesis that the different sensitivity of endothelial cells and pericytes may be connected with the exposure of the endothelial cells to a large amount of oxygen and iron in the blood, from which free radicals form and damage the cell membranes. In acellular capillaries, microaneurysms form. Ultimately retinal ischemia leads to the development of neovascularisations, and subsequently haemophthalmos, tractional retinal detachment and macular edema. On fluorescein angiography early changes are displayed as occlusion of capillaries with irregular dilations of capillaries and microaneurysms in their surrounding area [1].
On the basis of optical coherence tomography, radiation macular edema is divided into non-cystoid and cystoid, and also foveolar and extrafoveolar. According to the finding on fluorescein angiography it is divided into ischemic and non-ischemic. An early symptom of radiation maculopathy is non-ischemic macular edema, which can mutate into ischemic macular edema [6].
Various possibilities of treatment are used in the treatment of radiation retinopathy. At present this concerns especially intravitreal application of triamcinolone and bevacizumab, laser photocoagulation, and treatment in a hyperbaric chamber. After discovery of ischemic edema, however, an improvement of central visual acuity is improbable, regardless of what treatment the patient receives.
The aim of our study was to employ a bivariate and multivariate analysis in order to determine whether and to what extent the dose of radiation on the macula and selected patient characteristics are associated with the risk of onset of radiation maculopathy.
Fig. 1. Tumour deposit – melanoma of the choroidea in stage T1 – indicated in proximity of macula before stereotactic irradiation in 2013 – red arrow. 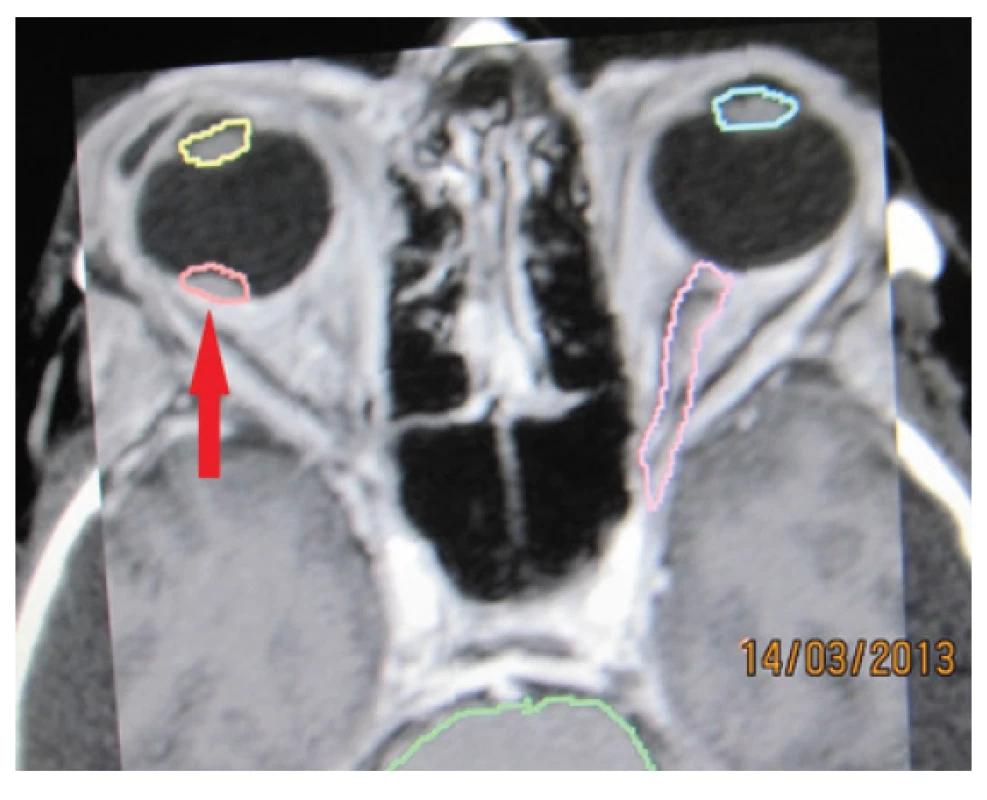
Fig. 2. Stereotactic plan of irradiation of deposit in 2013 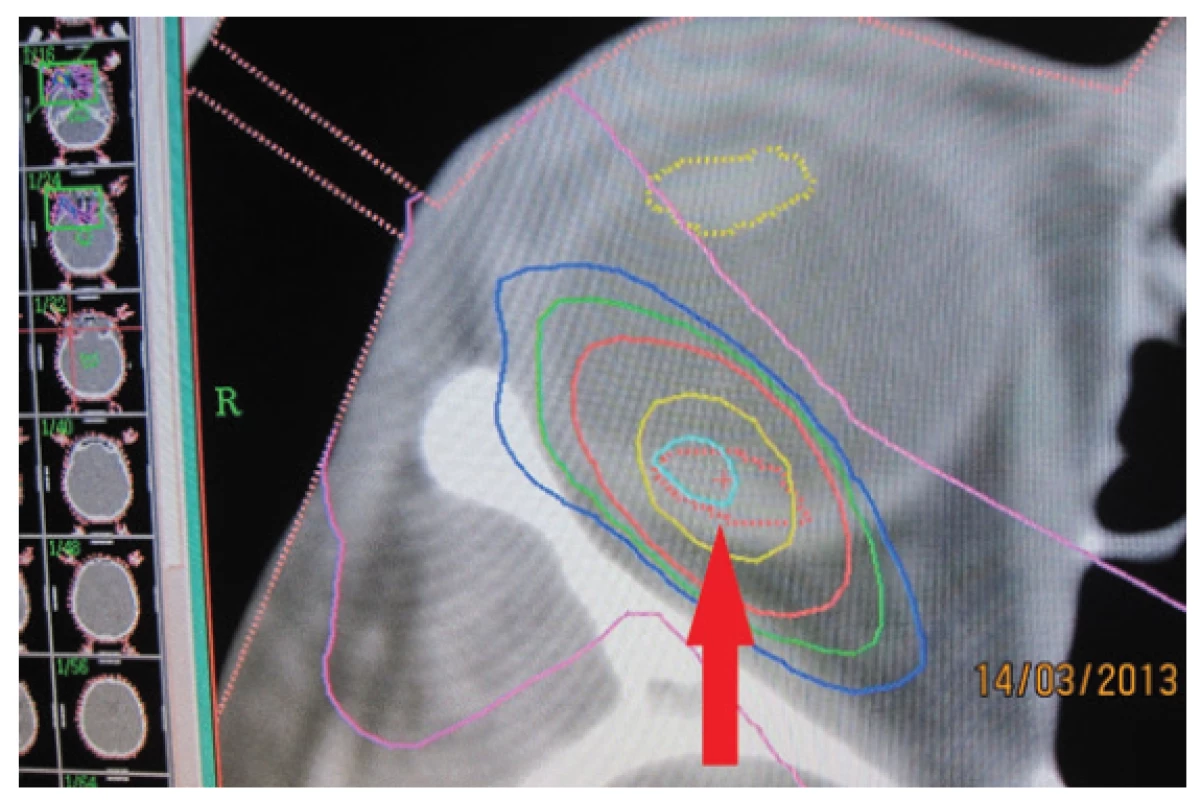
Fig. 3. Fluorescein angiography of tumour deposit 4 years later in 2017 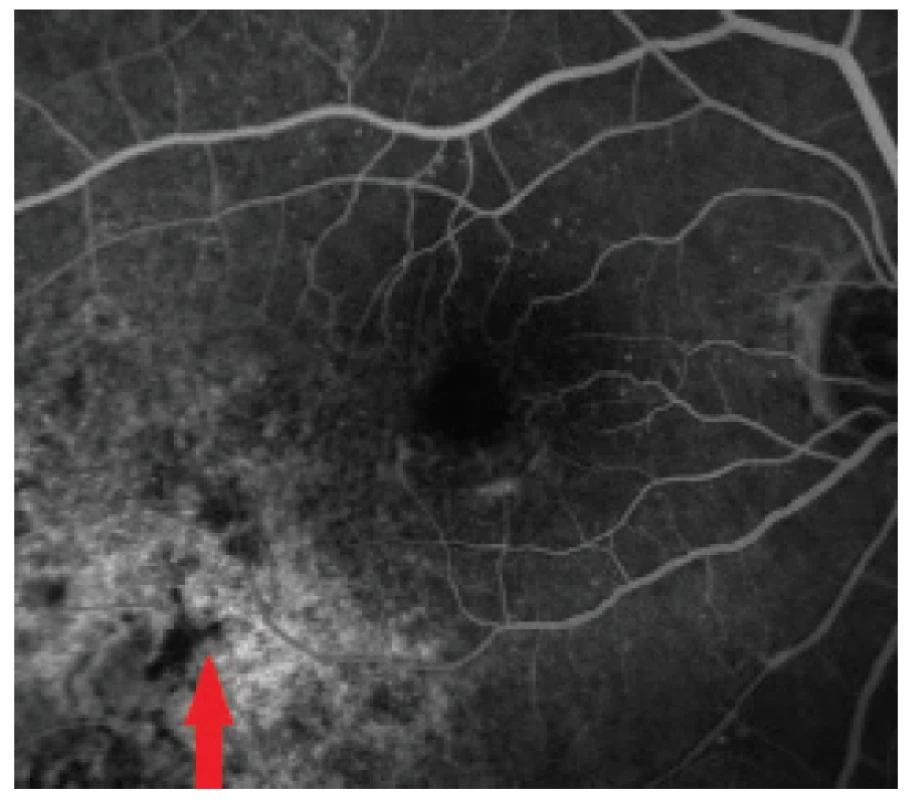
MATERIAL AND METHOD
We analysed a cohort of 168 patients with malignant melanoma of the corpus ciliare and choroidea, who underwent stereotactic radiosurgery on a LINAC linear accelerator at the Oncological Institute of St. Elizabeth in Bratislava in co-operation with the Department of Ophthalmology at the Faculty of Medicine, Comenius University and Ružinov University Hospital in Bratislava during the period of 2007-2016. The dose of radiation to the area of the tumour was 35.0 to 62.06 Gy, median 40.13 Gy. Radiation maculopathy was diagnosed on the basis of the finding on optical coherence tomography. The data was retrospectively evaluated in January 2018, thus the observation period was 13-122 months.
RESULTS
In the cohort of 168 patients, radiation maculopathy occurred in 49 patients (29%), of whom in 41 patients (84%) this was linked to tumours with post-equatorial localisation.
The time interval of the development of maculopathy following irradiation was 1 to 62 months, median 16 months. The median value of the dosage of irradiation of the macula in patients with subsequent development of maculopathy was 37 Gy. We evaluated the relationship of the individual parameters to the onset of maculopathy with the aid of a bivariate and multivariate analysis.
During the observation period, 28 patients (17%) underwent enucleation. The most frequent cause was dolorous neovascular glaucoma, in 23 patients (82% of enucleated). Enucleation was necessary in 4 eyes (14%) due to progression of the local finding, in which in all patients this concerned large tumours with a volume of more than 1 cm3. In 1 patient (4%), enucleation was performed due to the patient's decision, resulting from fear of the pathology. The time interval from irradiation to enucleation was 1 to 99 months, on average 26 months, median 21.5 months.
Bivariate analysis
As regards the age of the patients, those aged younger than 60 years had a 1.8 times higher risk of the onset of maculopathy in comparison with patients aged over 60 years (OR=1.776). This difference was not statistically significant (p=0.1202). In patients with melanoma in the right eye, the risk of development of maculopathy was 1.6 times higher than in patients with melanoma in the left eye, also on the basis of a bivariate analysis this relationship was not significant (p = 0.1783). The relatively low p value points to an uneven division of this characteristic between patients with and without maculopathy, and for this reason we included it in the multivariate analysis. In patients with tumours localised in the choroidea, the risk of maculopathy was 2.7 times higher than in patients with tumours localised in the corpus ciliare. This difference was demonstrated to be statistically insignificant, but the relatively low p value points to a possible relationship (p=0.1293). In the case of tumours with post-equatorial localisation, the risk of maculopathy was 1.6 times higher in comparison with tumours with pre-equatorial localisation, in which this difference was statistically insignificant (p=0.3234). Upon a division of tumours into those without contact with the macula, those touching the macula and those covering the macula, the highest risk of maculopathy was associated with tumours touching the macula. This risk was not significant (p=0.1201). Upon an evaluation of the volume of the tumour, patients with a lower median value of the tumour volume before irradiation had a statistically higher risk of occurrence of maculopathy (p=0.0423). Upon an evaluation of the dose of irradiation of the macula, there was no statistically significant difference between patients in whom maculopathy had developed in comparison with patients without maculopathy. The p value did not reach the level of statistical significance (p=0.1147), but in the bivariate analysis the influence of the dose may have been suppressed by the presence of other characteristics currently associated with maculopathy and with the dose – in other words by characteristics with an uneven distribution of the dose such as localisation with regard to the equator. We also determined that patients with a better value of corrected central visual acuity before irradiation had a higher risk of developing maculopathy – the median of central visual acuity in the patients without subsequent development of maculopathy was 20/40. The characteristics and outputs of the bivariate analysis are presented in Table 1.
Tab. 1. Bivariate analysis 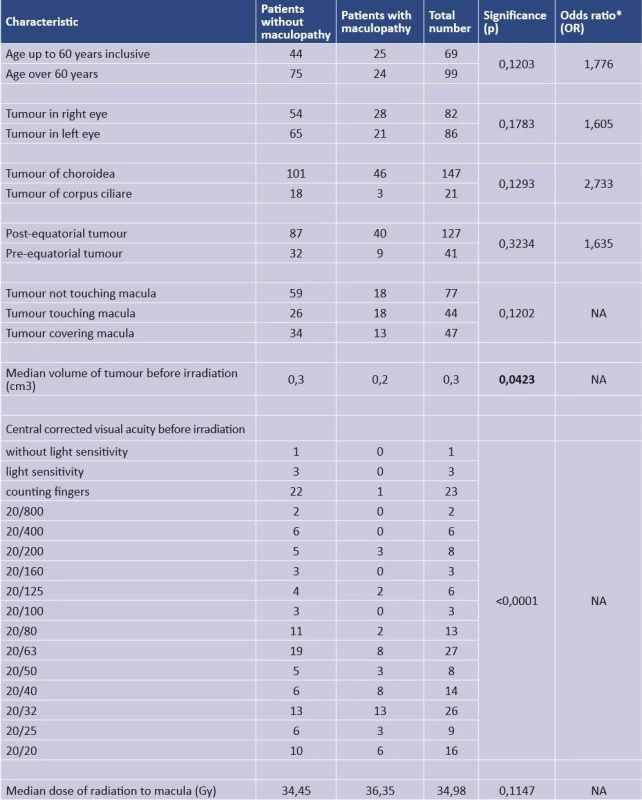
Numerical characteristics are presented as medians and categorical characteristics are presented as absolute numbers. OR* - odds ratio of onset of maculopathy in patients in upper row category to odds of onset of maculopathy in patients in lower row category of given explanatory variable. E.g. for age OR = (25/44) : (24/75) = 1.776.
Used abbreviations: OR - odds ratio; NA - not applicable.Tab. 2. Multivariate analysis 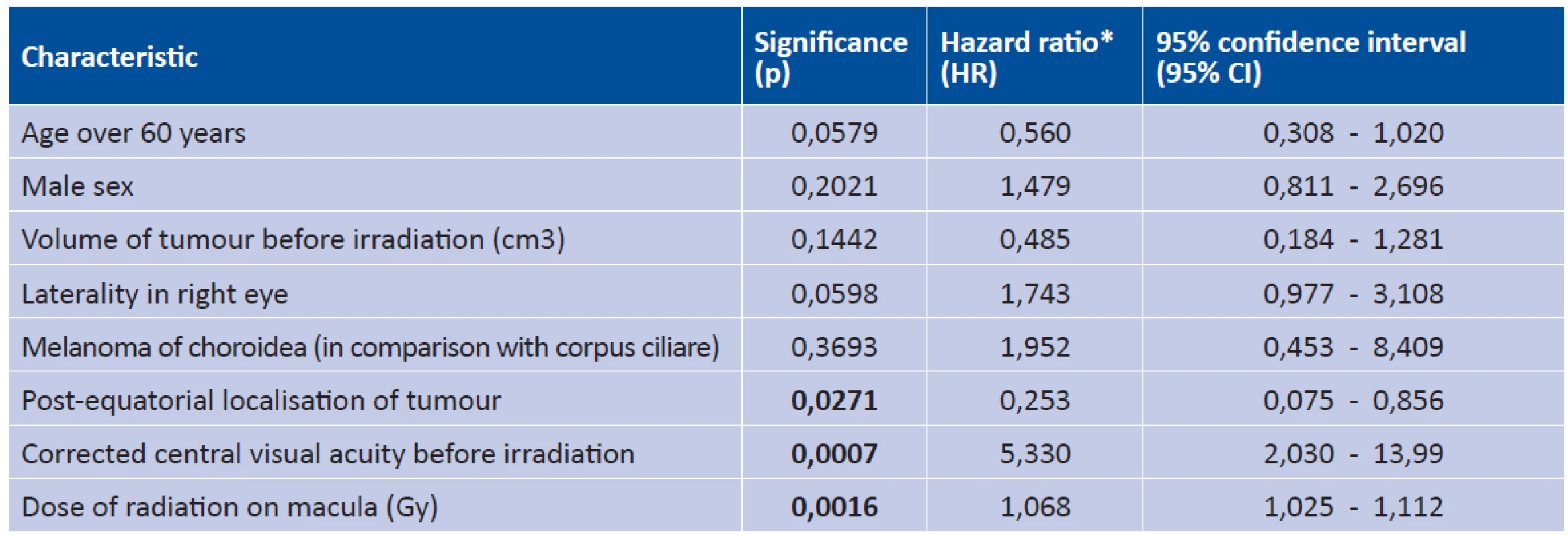
Test statistics of model and χ2 = 26.05 and corresponding attained level of significance of model p = 0.001.
Hazard ratio* - for categorical explanatory variables, the value of the ratio represents independent hazard (risk) of occurrence of maculopathy in patients in the stated category in comparison with the risk of maculopathy in patients in the referential (additional) category, on the precondition that the other characteristics are equal. Similarly in numerical characteristics, each increase by a unit in the given scale multiplies the hazard by the stated factor of HR. The combined effect of multiple explanatory variables is then the sum of the individual contributions.
Used abbreviations: HR - hazard ratio; NA - not applicableMultivariate analysis
Multivariate modelling demonstrated a highly significant influence of the dose of irradiation on the development of maculopathy (p=0.0016; Fig. 4). The model was adjusted for age (p=0.0578), laterality (p=0.0597), post-equatorial localisation of tumour (p=0.0271) and initial corrected central visual acuity (p=0.0007). In the final model we did not consider the characteristic of the edge of the tumour touching the macula, due to collinearity with central visual acuity (p=0.0006). The results of the multivariate analysis are presented in Table 2.
Fig. 4 presents the Kaplan-Meier curve of survival in patients without maculopathy stratified according to dose on the macula. The curves are adjusted to the characteristics of the patients stated in Table 2. Statistical significance of Cox model of proportionate risk: P = 0.00103 and statistical significance of influence of dose on macula: p = 0.0016.
Fig. 4. Kaplan-Meier curve of survival without maculopathy stratified according to dose on macula. The curves are adjusted to the characteristics of the patients stated in table 2. Statistical significance of Cox model of proportionate risk: p = 0.00103 and statistical significance of influence of dose on macula: p = 0.0016 
Treatment of radiation maculopathy
In 5 patients the treatment for maculopathy was bevacizumab administered intravitreally, 1x to 8x. None of the patients attained an improvement of central visual acuity after the intravitreal administration of bevacizumab.
DISCUSSION
On the basis of the information in the literature, a key risk factor for the development of radiation maculopathy is the dose of irradiation of the macula. At a dose of less than 45 Gy the development of radiation maculopathy is improbable, since other risk factors such as diabetes mellitus and concurrent treatment by chemotherapy, which in addition to the risk of development of retinopathy also influence its severity, are not present. The peak of incidence is 2-3 years after the irradiation treatment [11]. In our cohort the median value of the dose of irradiation of the macula in patients with subsequent development of maculopathy was lower, specifically 37 Gy.
In the cohort of patients after treatment by brachytherapy described by Summamen et al., radiation maculopathy appeared in 20 out of 85 eyes (24%), from 0.4 to 4.3 years after irradiation (median 1.8 years). The incidence of maculopathy was associated with the distance of the tumour from the fovea. A distance of the posterior edge of the tumour from the macula of more than 1.5 mm (1 dioptre) significantly reduced the risk of occurrence of maculopathy (p = 0.030 according to the Mantel-Cox test). The size of the tumour was not demonstrated to be a risk factor for the occurrence of maculopathy [13].
Stack et al. analysed the incidence of post-radiation complications in 92 patients following irradiation of malignant melanoma of the uvea by brachytherapy with the use of I125. Radiation retinopathy was the most commonly occurring complication, in which this concerned maculopathy in 23% of patients, and peripheral retinopathy in 17%. Irradiation of the macula with a dose of more than 90 Gy subsequently led to the development of retinopathy in 63% of patients (p<0.01). Thickness of the tumour of more than 4 mm was demonstrated to be a risk factor for the occurrence of maculopathy (p=0.003) [12].
In our cohort the dose of irradiation of the macula was a similarly statistically significant variable associated with maculopathy. Post-equatorial localisation of the tumour and touching of the macula with the edge of the tumour is associated with the proximity of the macula, and therefore indirectly also with a higher dose of irradiation of the macula.
An interesting factor is the association between maculopathy and better initial corrected central visual acuity, in which the bivariate analysis showed maculopathy to be statistically significantly associated also with a lower median of the volume of the tumour before irradiation. This may be caused by: a) earlier diagnosis of tumours localised on the posterior pole - they have a lower median volume and after irradiation a higher risk of maculopathy, b) lower risk of enucleation in patients with smaller tumours and better central visual acuity (in patients without maculopathy, enucleation was 1.6 times more frequent). If a patient has a lower risk of enucleation, he or she also has a higher chance of developing later post-radiation compilations such as maculopathy and optic neuropathy, which would naturally not have occurred in the patient if he or she had had to undergo enucleation.
We explain the higher incidence of maculopathy in the right eye by means of the larger median volume of the tumours in the right eye, which was 0.3 cm3, whereas the median of the tumours in the left eye was 0.26 cm3. As regards the distance of the tumours from the macula, out of the total number of 82 tumours in the right eye, 59 were with post-equatorial localisation (72%), in the left eye out of a total of 86 tumours, 68 had post-equatorial localisation (79%). The difference in prevalence of maculopathy between the right and left eye is therefore not associated with the distance from the macula.
Bevacizumab in a dose of 1.25 mg intravitreally is used for the treatment of age-related macular degeneration, diabetic retinopathy and retinal vein occlusion. It is a humanised monoclonal antibody against vascular endothelial growth factor (VEGF). It is assumed that its blocked reduces vascular permeability and prevents abnormal vascularisation. After intravitreal administration of bevacizumab, central visual acuity may improve in patients with radiation retinopathy, although in the majority of cases this improvement is only temporary. Central visual acuity usually returns to the same level as before the administration of the injection within 1 year of application [3].
Intravitreal administration of triamcinolone acetate in a dose of 4 mg is used in the treatment of macular edema caused by various pathologies. The mechanism of its effect is not well clarified, it is assumed that it has an influence on restoring the inner blood retinal barrier by means of modulating cytokines and regulating the permeability of capillaries. However, this treatment may be complicated by steroid glaucoma [11].
In certain indications, laser photocoagulation has also retained its place in the treatment of radiation retinopathy. It has been demonstrated that panretinal laser photocoagulation is effective in the treatment of proliferative retinopathy. Focal laser photocoagulation was previously used in the treatment of macular edema, in which it led to a regression of edema in some patients. However, two years after treatment there is no longer any difference in central visual acuity between the patients treated with laser photocoagulation and those who were not treated [7].
With regard to the fact that the present possibilities of treatment of radiation retinopathy are not very successful, some authorities are focusing on its prevention. Oliver et al. tested the effect of 1000 CSt silicone oil, 5000 CSt silicone oil, perfluorocarbon and heavy oils as protection against the effect of I125 on cadaverous eyes. The strongest protective effect was achieved by 1000 CSt silicone oil, which had a 55% greater effect in comparison with the vitreous body in preventing the spread of radiation. Pars plana vitrectomy with tamponade using 1000 CSt silicone oil in combination with brachytherapy may be an effective method of treatment, and is being applied in a number of centres [9].
In our cohort, bevacizumab as treatment for radiation maculopathy was applied to 5 patients, with the result that central visual acuity did not improve in a single case. Ischemic edema evidently developed in the macula, upon which treatment by bevacizumab is ineffective, as are the other currently available options.
The aim of every treatment of uveal melanoma is to prevent metastatic spreading [10, 2]. Monitoring of small pigment lesions - nevi, and monitoring of their potential transformation into melanoma is of great significance in clinical practice. In practice ophthalmologists use display methods such as optical coherence tomography in order to assess the dynamics of changes in the deposit [8].
CONCLUSION
Post-radiation complications can complicate the results of treatment of uveal melanoma using radiation, by means of a deterioration of central visual acuity and sometimes also the necessity of secondary enucleation. Radiation maculopathy ranks among the later sight-threatening complications. The dose of radiation of the macula is the most significant risk factor for its development. No effective treatment currently exists. After treatment of uveal melanoma by radiation, it is necessary to ensure long-term active monitoring care by an ophthalmologist, not only to monitor the tumour itself, but also for the purpose of diagnosis and treatment of potential post-radiation complications.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received by the Editorial Department on: 8 August 2018
Accepted for printing on: 22 January 2019
MUDr. Pavlína Zahorjanová
Department of Ophthalmology of the University Hospital with the Outpatient Clinic in Žilina, V. Spanyola 43, 012 07 Žilina
Zdroje
1. Archer, B.D., Amoaku, W.M., Gardiner, T.A.: Radiation retinopathy – clinical, histopathological, ultrastructural and experimental correlations. Eye, 5; 1991 : 239-51.
2. Damato, B.: Ocular treatment of choroidal melanoma in relation to the prevention of metastatic death - A personal view. Prog Retin Eye Res [online]. Mar 2018 [cit. 21. 8.2018]. Dostupné na https://www.ncbi.nlm.nih.gov/pubmed/29571968.
3. Finger, P.T.: Radiation retinopathy is treatable with anti-vascular endothelial growth factor bevacizumab (Avastin). Int J Radiat Oncol Biol Phys, 70(4); 2008 : 974-7.
4. Furdová, A., Šramka, M., Waczulíková, I., et al.: Stereotaktická rádiochirurgia (LINAC) uveálnych melanómov; postradiačné komplikácie. Cesk slov oftalmol, 71(3); 2015 : 134-42.
5. Furdová, A., Šramka, M.: Uveal malignant melanoma and stereotactic radiosurgery. Saarbrucken, LAP LAMBERT Academic Publishing, 2014, 181 p.
6. Horgan, N., Shields, C.L., Mashayekhi, A., et al.: Classification and treatment of radiation maculopathy. Curr Opin Ophthalmol, 21(3); 2010 : 233-8.
7. Hykin, P.G., Shields, C.L., Shields, J.A., et al.: The efficacy of focal laser therapy in radiation-induced macular edema. Ophthalmology, 105(8); 1998 : 1425-9.
8. Neroev, V.V., Saakyan, S.V., Myakoshina, E.B., et al.: Role of optical coherence tomography angiography in diagnostics of early choroidal melanoma and circumscribed choroidal hemangioma. Vestn Oftalmol, 134(3); 2018 : 4–18.
9. Oliver, S.C., Leu, M.Y., DeMarco, J.J., et al.: Attenuation of iodine 125 radiation with vitreous substitutes in the treatment of uveal melanoma. Arch Ophthalmol, 128(7); 2010 : 888-93.
10. Shields, C.L., Mashayekhi, A., Shields, J.A.: By Sleight of Hand, Prognosis Determined-Even for Small Choroidal Melanoma. JAMA Ophthalmol, 136(5); 2018 : 488–9.
11. Singh, A.D., Damato, B.: Clinical Ophthalmic Oncology. In: Basis Principles and Diagnostic Techniques. Berlin, Springer, 2014, 99-109 p.
12. Stack, E., Elder, M., Abdelaal, A., et al.: New Zealand experience of I125 brachytherapy of uveal melanoma. Clin Exp Ophthalmol, 33(5); 2005 : 490-4.
13. Summanen, P., Immonen, I., Kivelä, T., et al.: Radiation related complications after ruthenium plaque radiotherapy of uveal melanoma. Br J Ophthalmol, 80; 1996 : 732-739.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 1- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- Usage of shear wave elastography for diagnosis of changes of oculomotor muscles in endocrine orbitopathy
- Treatment of idiopathic choroidal neovascular membrane with ranibizumab - our experience
- RADIATION MACULOPATHY AFTER ONE-DAY SESSION STEREOTACTIC RADIOSURGERY IN PATIENTS WITH CILIARY BODY AND CHOROIDAL MELANOMA
- Effective Tissue Layer Separation of Donor Cornea for DMEK by Fluid Injection Between Descemet
- Primary orbital teratoma – case study
- Late postoperative capsular bag distension syndrome
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Late postoperative capsular bag distension syndrome
- Primary orbital teratoma – case study
- Treatment of idiopathic choroidal neovascular membrane with ranibizumab - our experience
- RADIATION MACULOPATHY AFTER ONE-DAY SESSION STEREOTACTIC RADIOSURGERY IN PATIENTS WITH CILIARY BODY AND CHOROIDAL MELANOMA
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



