-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Congenital central toxoplasmic chorioretinitis - case study
Authors: K. Maršolková 1; J. Timkovič 1,2; V. Lesková 3; J. Němčanský 1,2; H. Wiedermannová 3,4
Authors place of work: Oční klinika, Fakultní nemocnice Ostrava 1; Katedra kraniofaciálních oborů, Lékařská fakulta, Ostravská univerzita 2; Oddělení neonatologie, Fakultní nemocnice Ostrava 3; Katedra dětského lékařství a neonatologie, Lékařská fakulta, Ostravská univerzita Oční klinika, Fakultní nemocnice Ostrava, 17. listopadu 1790/5, 708 00, Ostrava, přednosta: MUDr. Jan Němčanský, PhD. 4
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 3, p. 114-118
Category: Kazuistika
doi: https://doi.org/10.31348/2018/1/6-3-2018Summary
Congenital toxoplasmosis is a globally spread infectious disease caused by transplacental transmission of an intracellular parasitic protozoan Toxoplasma gondii. The infection can cause serious multi-organ complications, and in the case of vertical transmission, can lead up to fetal death – depending on the stage of pregnancy at the time of infection and the overall condition of the mother’s immune system. Chorioretinitis, hydrocephalus and intracranial calcifications are a typical triad of symptoms associated with the disease. Toxoplasmic chorioretinitis in particular is the most common ocular manifestation. If the central retina is affected, it can cause a severe impairment of central visual acuity or lead up to blindness in the child. Prenatal screening of this disease is presently voluntary in the Czech Republic.
This article reports on a case study of a toxoplasmic chorioretinitis in a newborn child observed from the active stage and the development of the affected retina over time. Further is also reported on the diagnostics and the treatment of multi-organ complications which occurred in this patient. Ophthalmologic examination was performed after diagnosis of hydrocephalus, which revealed severe changes of retina. Hydrocephalus was then properly treated. An overview of the diagnostic and therapeutic methods and the screening options available in the Czech Republic compare with other countries is also presented in the report.
Key words:
congenital toxoplasmosis, chorioretinitis, multi-organ complications, screening, hydrocephalusIntroduction
Congenital toxoplasmosis occurs following primary infection of the mother during pregnancy by the intracellular parasite Toxoplasma gondii and subsequent transplacental transmission of the parasite to the foetus. The incidence is within the range of 1 to 10 out of 10 000 live born children in Europe and the USA (1, 12, 13, 15), in the Czech Republic it is around 0.2/10 000 (23).
The incidence of serious symptoms is indirectly proportionate to the probability of infection of the mother during the whole of pregnancy (1, 13). This means that the probability of infection by Toxoplasma increases with gestation age, although this is also dependent on the general condition of the mother's immune system. The most serious complications of the disease are miscarriage, death of the foetus or neurosensory disorders of the newborn infant, but their incidence is most frequent in the first trimester, when the risk of infection is between 10 and 25% (1, 12). In the second trimester, although the risk of infection increases to 30-45%, the severity of the symptoms decreases (1, 12). The most frequently described manifestations are acute infections such as encephalitis, pneumonia, hepatosplenomegaly or lymphadenopathy. Despite the fact that the probability of infection of the foetus during the third trimester is as high as 60-80%, virtually no clinical manifestation of the disease need be evident, or only non-specific symptoms may be manifested. Nevertheless, the disease may be manifested in the later life of the child (1, 6, 12, 13).
Toxoplasmic chorioretinitis is the most common ocular complication of the general pathology. It appears in 70-90% of patients with the congenital form of the disease, and less often as a complication of acquired primary infection (13). Other described ocular symptoms of congenital toxoplasmosis are microphthalmia, congenital cataract, glaucoma or strabismus (5, 10, 12, 13, 14, 19).
The first doctor in the Czech Republic to observe and describe toxoplasmic uveitis and chorioretinitis in the literature was Josef Janků, whose publications were later quoted also in the foreign literature (7, 8, 9).
The aim of the presented study is to describe the clinical course of the pathology in a newborn infant with congenital form of toxoplasmosis, manifesting itself in affliction of both eyes and the central nervous system (CNS).
Case report
A boy was born from the mother's second pregnancy in the 38th week of gestation, screening of the mother for Streptococcus agalactiae was negative. A physiological prenatal course was documented up to the 26th week of gestation, when the last ultrasound examination of the foetus was conducted, after which the mother refused further recommended examinations. Birth took place spontaneously, outside a healthcare facility, in the presence of a midwife. The boy was born head first, the birth was accompanied by the discharge of slightly cloudy amniotic fluid. Anamnestically, immediately after birth there were present respiratory problems of the newborn which receded following artificial respiration, and subsequently the child ventilated regularly. A birth weight of 3245 g and a length of 50 cm was determined. Immediately after birth the infant's head was conspicuously large, otherwise the child was without striking features (Fig. 1). On the following day the mother visited a clinic for risk newborns, where the circumference of the infant's head was determined to be 38.5 cm (the physiological norm according to the growth curve for the given age is 32.5 to 37.5 cm) (14). Following ultrasonographic (USG) examination of the head, which demonstrated signs of hydrocephalus (Fig. 2), the boy was immediately sent and admitted to an intensive care unit at the Department of Neonatology at the University Hospital Ostrava.
Fig. 1. Hydrocephalus of inflammatory (toxoplasmic) etiology – upon visual inspection evident larger head circumference (38.5 cm). 
Fig. 2. Ultrasonographic finding of asymmetry and dilation of lateral brain ventricles – bilateral frontally present hyperechogenicity and evident signs of previous ventriculitis 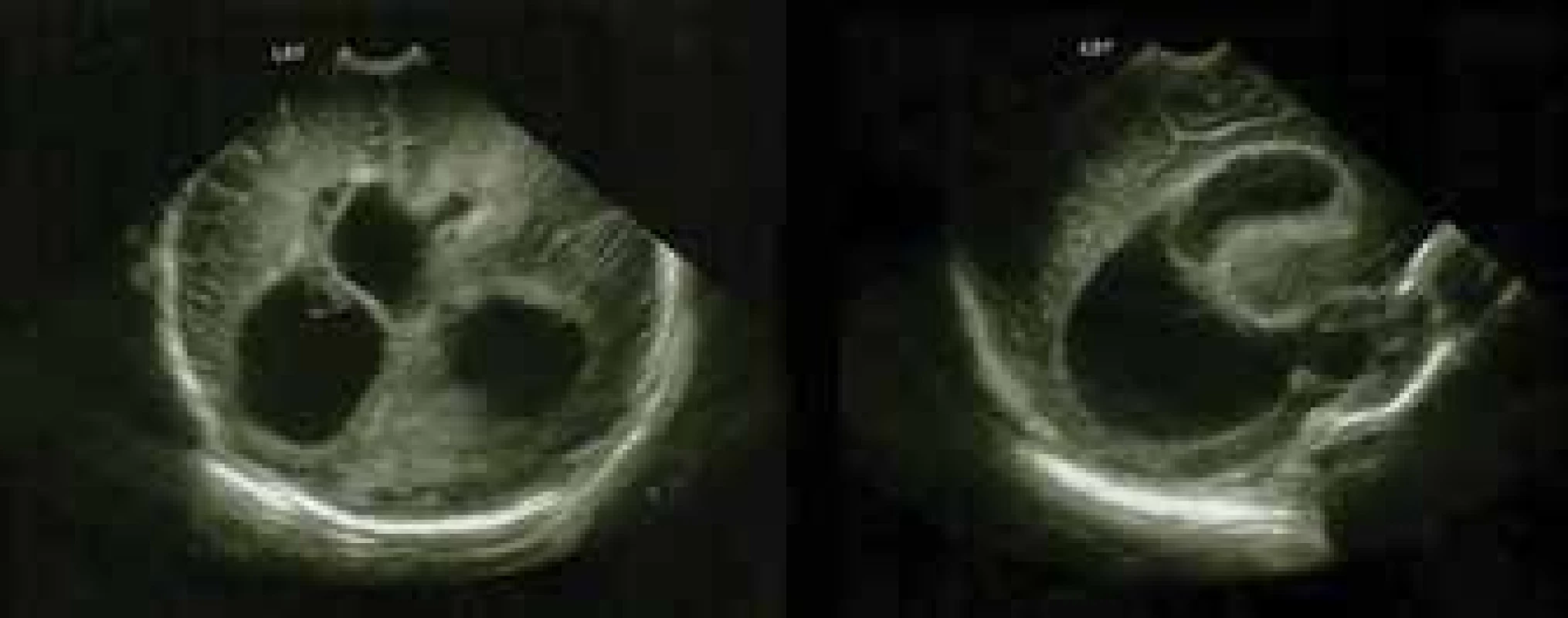
At the initial examination the boy was cardiopulmonary stable, spontaneously ventilating, and other than the larger circumference of his head the general physical finding was without remarkable features. The finding of dilation of the brain ventricles upon magnetic resonance imaging (MRI) confirmed suspicion of hydrocephalus. In addition to obstructive hydrocephalus, the images from magnetic resonance also showed the presence of extensive postischemic and haemorrhaged deposits in both hemispheres of the brain, as a consequence of hypoxic state (Fig. 3). Upon the instructions of a neurosurgeon the boy was referred for external ventricular drainage, which was subsequently due to malfunction replaced by Ommaya reservoirs with parieto-occipital insertion. Blood samples were taken for serological examination of the TORCH panel (Toxoplasma gondii, rubeola, cytomegalovirus, Herpes simplex).
Fig. 3. MRI examination of CNS – extensive ischemic-pseudocystic changes of both brain hemispheres, husky parenchyma on left and bilaterally evident periventricular haemorrhage. 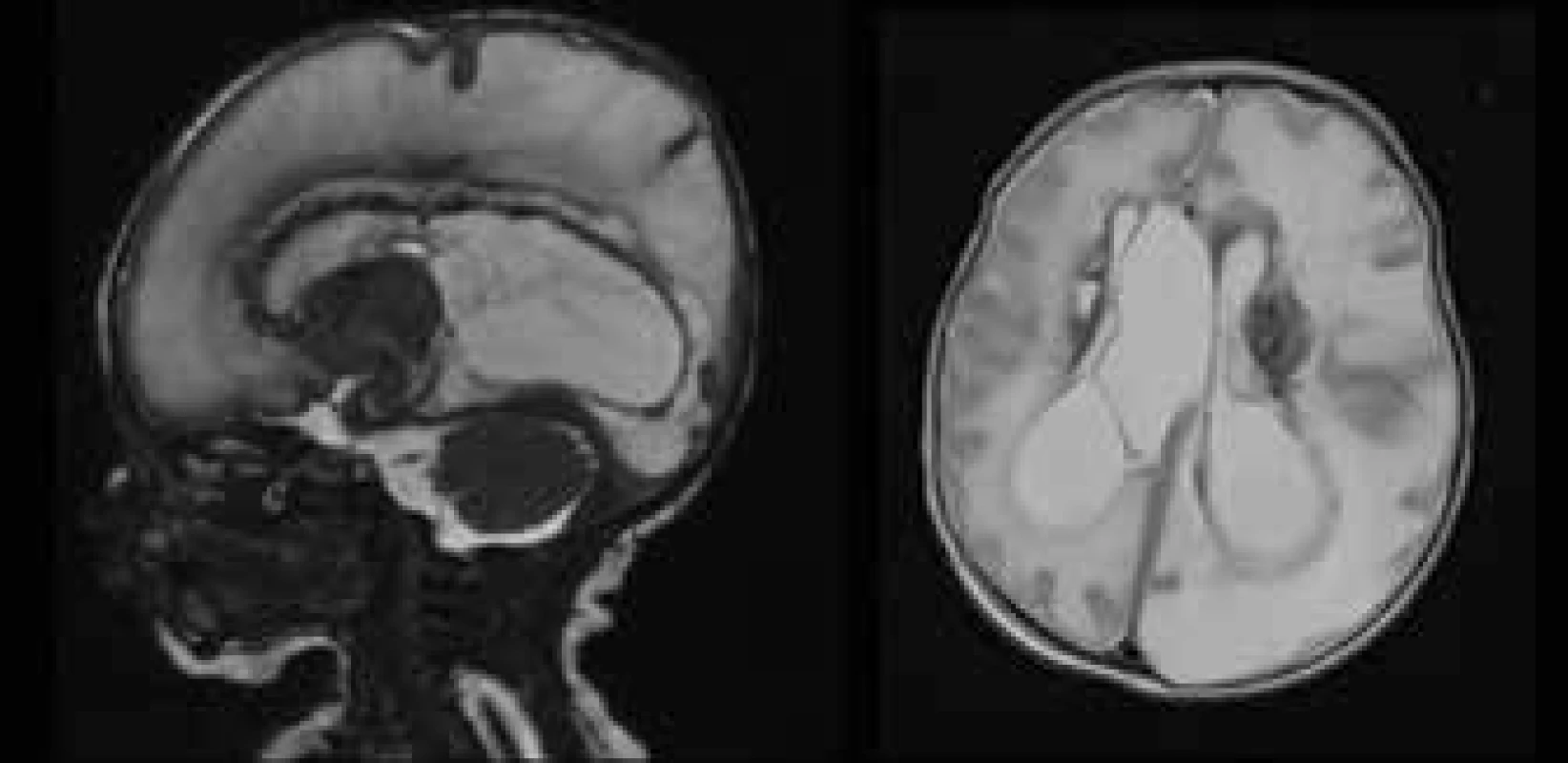
Within the framework of an interdisciplinary examination, the first ophthalmological examination was conducted on the boy in the 40th week after conception. The finding on the anterior segment was physiological. An examination of the ocular fundus in artificial mydriasis detected the presence of active chorioretinal inflammatory deposits of whitish colour in the central retinal landscape in both eyes, with a size of three times the diameter of the optic disc (DD), afflicting the fovea. At the edge of the inflammatory deposit there was an evident circular edema, in the left eye the nasal and upper edge of the deposit was slightly pigmented. The other retinas were without coarse deposit changes (Fig. 4a). Suspicion of chorioretinitis of toxoplasmic etiology was stated.
Fig. 4. Central toxoplasmic chorioretinitis – retinal finding in boy with congenital toxoplasmosis infection in both eyes. In the images two weeks after the birth of the infant (fig. 4a) deposits of active toxoplasmic chorioretinitis are identified, affecting the region of the macula. The retinal finding at an interval of 4 weeks after the commencement of general therapy shows subsiding inflammatory activity and incipient retinal scarring (fig. 4b) and advanced chorioretinal deposits of toxoplasmic etiology in the stage of atrophic scar with pigmented edges, functionally characterised by irreversible affliction of central visual acuity in the child (fig. 4c). Images obtained using digital imaging system RetCam, 3rd generation. 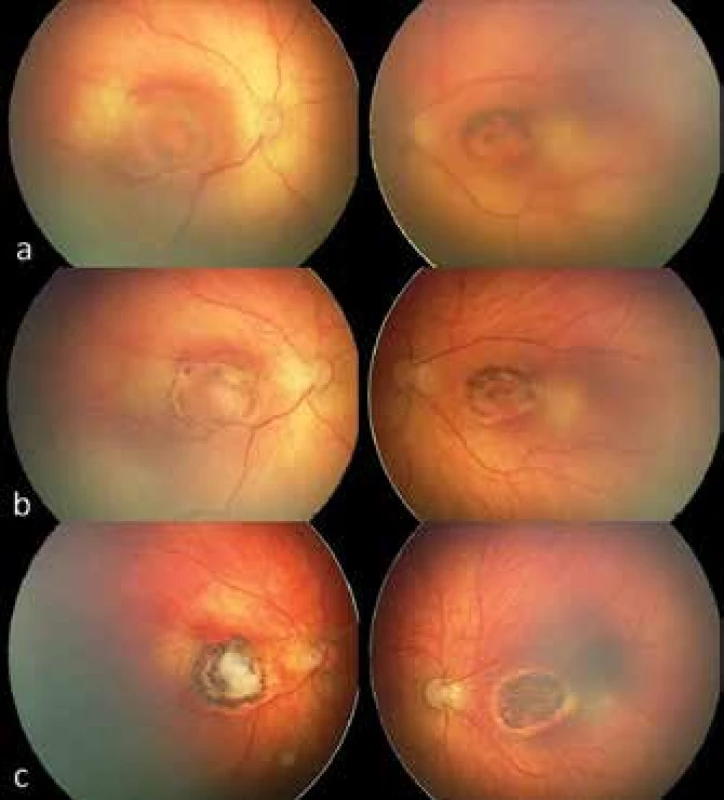
Lumbar puncture was performed with a negative finding of cultivation demonstration of pathogen. Elevation of inflammatory markers was evident in the boy's blood samples (C reactive protein). In the serological examination a finding of positivity of IgG antibodies against Toxoplasma gondii was described with low avidity (179.63 IU/ml), in which the value of IgA and IgM antibodies in serum was borderline. Congenital infection was confirmed also with the aid of the polymerase chain reaction (PCR) technique. General therapy was applied with pyrimethamine in a dose of 1 mg/kg/day and sulfadiazine of 100 mg/kg/day. The general therapy was supplemented by calcium folinate in a dose of 10 mg per day, with the aim of limiting the negative toxic effect of anti-toxoplasmosis medication.
An ophthalmological examination at an interval of four weeks after the commencement of general therapy demonstrated bilaterally subsiding inflammatory activity and edema, and continuing pigmentation on the edge of the deposits (Fig. 4b). General therapy was configured and directed by infectious disease specialists, from an ophthalmological perspective a conservative procedure was chosen and a schedule of regular eye examinations with photo-documentation was set. During the next few weeks the chorioretinal atrophic deposits were scarred centrally, and the edges of the lesions were bilaterally circularly pigmented, now without the presence of edema or other signs of inflammatory activity. The peripheral retina was without new deposit changes (Fig. 4c). At all ophthalmological examinations the anterior segment of the eye was without manifest pathology.
From a neurological perspective, central hypertonic syndrome was diagnosed in the child. Due to the risk of development of spasticity, intensive rehabilitation was commenced. The finding was gradually stabilised on USG, and after almost two months of hospitalisation the child was discharged into outpatient care in a stabilised condition, now without signs of intracranial hypertension. General medication was configured according to a protocol (4), in which after 3 months pyrimethamine and sulfadiazine are always replaced for a month by spiramycin in a dose of 100 mg/kg/day, alternating until the child reaches the age of one year. Upon discharge a regular schedule of paediatric, neurological, neurosurgical and ophthalmological examinations was set.
At further ophthalmological examinations, no changes of the retinal finding or reactivation on the edges of the deposit were determined, although at an examination at the age of nine months, upon visual inspection, wandering to nystagmoid movements of the eyeballs were identified. The boy fixed only briefly on light, and upon an examination of the anterior chamber the red reflex was impaired by a perceptible whitish reflection of the central atrophic deposit of the retina. The size of the deposits continues to be without development over time, their edges remain pronouncedly hyperpigmented with an atrophic centre (Fig. 4c). With regard to the bilateral severe visual affliction and the development of oculugyric nystagmus, visual stimulation was recommended to the parents. At the last neurological examinations the boy was receiving general therapy for repeated epileptic fits of a myoclonic character. The boy remains in multi-disciplinary care, and the development of his general condition and local ocular finding is being thoroughly monitored and documented.
Discussion
Infection with the parasite Toxoplasma gondii is very widespread within today's population. Its incidence is estimated at around 25-30% worldwide, but may differ markedly between individual continents or states (15, 17). Differences are also described between different communities within a single region (1, 15, 19). Differences in incidence are contributed to, in addition to the social conditions of the population in the given region, also by the varying virulence of individual serotypes. Serological type II is widespread mainly in Europe and North America, and is less virulent. In contrast with this, highly virulent atypical serotypes I and III, occurring mainly in Central and South America, are associated with a higher incidence of intraocular complications, even upon infection of an immunocompetent patient postnatally (1, 10, 15, 24).
Infection of the foetus takes place via vertical transmission of the parasite upon primary infection of the mother (most frequently alimentary) during or up to six months before the beginning of pregnancy. Secondary infection with subsequent foetal transmission has been described, but in our conditions is extremely rare (6). The penetration of tachyzoites of the parasite into the amniotic fluid and subsequently into the foetal space depends upon the immune control of the placental transmission, although the entire mechanism and the factors influencing it have not yet been entirely clarified (17).
Toxoplasmic chorioretinitis is the most common ocular complication causing deterioration of central visual acuity to complete loss of vision. The parasite invades the retinal cells, in which it may persist in the cystic stage for periods of varying length. At the moment when the microorganisms are activated and begin to reproduce intracellularly, manifestations of chorioretinitis may appear, and this may occur up to several decades following congenital infection (3, 18, 24).
For confirmation of diagnosis, a serological examination of a blood sample of the patient is required, which demonstrates positivity of IgG and IgM antibodies against Toxoplasma. In case of necessity, for the purpose of a definitive decision it is possible to conduct a molecular examination of the amniotic fluid using the PCR technique (2, 3, 6, 13, 17, 25). It is then necessary to commence general therapy of the mother immediately (thus during pregnancy) and subsequently also of the newborn infant. Timely determination of the diagnosis and commencement of treatment influences the severity of the course of the infection and the development of later complications. General therapy is applied as standard in a triple combination of pyrimethamine, sulfadiazine and folic acid. This is administered in order to limit the toxic side effects of anti-toxoplasmosis therapy, since pyrimethamine causes a suppression of haematopoiesis in bone marrow. The therapy may be supplemented with corticosteroids. This triple combination is always replaced after 3 months by spiramycin, and the therapy continues for up to one year (4, 13, 11, 25). A further described possibility of general therapy is a quadruple combination with cotrimoxazol and clindamycin, which has fewer adverse effects, in addition to which more rapid regression of the deposits of the pathology on the retina has been described in comparison with the classic triple combination (10, 18).
Recently, the possibility of intravitreal administration of therapy has frequently been discussed. A range of cases of regression of an active deposit of toxoplasmic chorioretinis have been described, as well as an improvement of central visual acuity in adult patients following intravitreal administration of clindamycin in combination with dexamethasone (26). The authors of a study investigating the possibilities of intravitreal therapy of toxoplasmic chorioretinitis as alternatives to the classic combination of pharmaceuticals have described a beneficial effect and improvement of central visual acuity by at minimum two rows of ETDRS (early treatment diabetic retinopathy study) optotype. Following intravitreal administration of the combination of pharmaceuticals trimethoprim/sulfamethoxazole/dexamethasone they recorded a rapid regression of retinal deposits (22). All of these options would represent a good alternative for patients with adverse effects or allergy to general therapy, which could substantially reduce the time of administration of general therapy and thereby improve patient compliance.
In the case of the development of later complications in the form of choroidal neovascular membranes, other therapeutic procedures are available such as laser photocoagulation of the retina or photodynamic therapy (11, 16). A good effect has also been described following intravitreal application of anti-VEGF preparations, probably because VEGF (vascular endothelial growth factor) plays a role here not only in the process of neoangiogenesis and therefore in the formation of a neovascualr membrane, but also as an proinflammatory mediator (11). An improvement of the retinal finding was achieved following the application of bevacizumab (Avastin – this concerns off-label therapy in the Czech Republic) (16), ranibizumab (20) or aflibercept (this concerns a pilot study) (11).
Other ocular complications which have been described in the literature include vitritis, epiretinal membrane, subretinal collection of fluid to development of serous retinal detachment (19, 26).
With regard to the fact that general and local therapy is highly demanding in terms of organisation and very costly financially, in some European states mandatory regular prenatal screening for this pathology has now been introduced (Belgium, France, Austria, Slovakia, Slovenia) (23). Many studies from these countries document that from a long-term perspective, blanket screening of pregnant mothers can ensure timely detection of infection, after which it is possible to commence treatment of the mother immediately. The result is an alleviation of the consequences of infection of the afflicted newborn infant, and last but not least also a positive influence on the development of later complications of Toxoplasma infection (15, 21, 24, 25). All children with diagnosed congenital toxoplasmosis should be regularly actively monitored by an ophthalmologist up to adult age, since even in the case of timely commencement of treatment it is not possible to exclude later manifestation or reactivation of the disease (3, 24). At the same time it is demonstrated that the introduction of mandatory screening for Toxoplasma gondii infection would be suitable also for financial reasons (15).
Conclusion
A newborn infant with suspicion of congenital toxoplasmosis infection should be completely examined, from blood samples to display methods such as ultrasonography, computer tomography or magnetic resonance imaging. The child should also be examined by a specialist in the field of neurology, infectious diseases and ophthalmology, and in the case of confirmation of congenital toxoplasmosis or its ocular form, general therapy should be commenced immediately.
The diagnosis and therapy of this pathology is highly demanding, and for this reason attention should also be devoted to the methods of limiting the spread of infection. An effective means would be the introduction of mandatory screening for the infection during pregnancy. However, it is also the task of the healthcare personnel to inform pregnant women to avoid risk behaviour, and if possible to maintain a healthy lifestyle during pregnancy.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Kristýna Maršolková
Oční klinika, Fakultní nemocnice Ostrava, 17. listopadu 1790/5, 708 52, Ostrava
Zdroje
1. Bischoff, A.R., Friedrich, L., Cattan, J.M. et al.: Incidence of Symptomatic Congenital Toxoplasmosis During Ten Years in a Brazillian Hospital. Pediatr Infect Dis J, 35; 2016 : 1313-1316.
2. Boyer, K., Hill, D., Mui, E. et al.: Unrecognized Ingestion of Toxoplasma gondii Oocysts Leads to Congenital Toxoplasmosis and Causes Epidemics in North America. CID, 53; 2011 : 1081-1089.
3. Faucher, B., Garcia-Meric, P., Franck, J., et al.: Long-term ocular outcome in congenital toxoplasmosis: A prospective kohort of treated children. J Infect, 64; 2012 : 104-109.
4. Geleneky, M., Prášil, P., Kodym, P.: Doporučený postup pro diagnostiku a léčbu toxoplasmózy [online]. Schváleno výborem Společnosti infekčního lékařství ČLS JEP v červnu 2017, datum vydání 7. listopadu 2017. Dostupné na WWW: < https://www.infekce.cz/DoporToxo17.htm >.
5. Guha, R., Miley, L., Aspiri M. et al.: Congenital Toxoplasmosis. Pediatr Neurol, 70; 2017 : 81-82.
6. Handl, V.K., Klingelhöfer, D., Schlöffel, N. et al.: Kongenitale Toxoplasmose und Toxoplasma gondii. Zbl Arbeitsmed, 66; 2016 : 239-248.
7. In Pepose J.S., Holland, G.H., Wilhalmus, K.R.: Ocular Infection Immunity. Mosby, St.Lois, 1996, p. 1183-1224.8.
8. Janků, J.: Pathogenesa a patologická anatomie tak nazvaného vrozeného kolobomu žluté skvrny v oku normálně velikém a mikrophtalmickém s nálezem parasitů v sítnici.Cas Lek Ces, 62; 1923 : 1021-1027.
9. Janku J.: Die patogenese ung pathologishe Anatomie des sogenannten angeborenen Koloboms des gelben Fleckes im normal grossen sowie im mikrophthalmishen Auge mit Parasitenbefund in der Netzhaut. Cls Parasit, 6; 1959 : 9-16.
10. Kartasasmita, A., Muntur, W.P., Enus, S. et al.: Rapid resolution of toxoplasma chorioretinitis treatment using quadruple therapy. Clin Ophthalmol, 11; 2017 : 2133-2137.
11. Korol, A.R., Zborovska, O., Kustryn, T. et al.: Intravitreal aflibercept for choroidal neovascularization associated with chorioretinitis: a pilot study. Clin Ophthalmol, 11; 2017 : 1315-1320.
12. Melamed, J., Eckert, G.U., Spadoni, V.S. et al.: Ocular manifestations of congenital toxoplasmosis. Eye, 24; 2010 : 528-534.
13. Modrzejewska, M., Patalan, J., Kulik, U. et al.: Ocular manifestation of congenital toxoplasmosis, clinical implication – case report. Ginekol Pol, 87; 2016 : 226-230.
14. Paulová M., Vignerová J., Riedlová J.: Individuální hodnocení růstu pomocí růstových grafů se zaměřením na děti do 2 let. Neonatologické listy 15; 2009 : 3-9.
15. Prusa, A-R., Kasper, D.C., Sawers, L. et al.: Congenital toxoplasmosis in Austria: Prenatal screening for prevention is cost-saving. PloS Negl Trop Dis. 2017, č. 11 [cit. 2017-04-21]. Dostupný na WWW: < http://doi.org/10.1371/journal.pntd.0005648 >.
16. Rishi P.,Venkataraman A., Rishi E.: Combination photodynamic therapy and bevacizumab for choroidal neovascularization associated with toxoplasmosis. Indian J Ophthalmol. 2011;59(1):62-64.
17. Robert-Gangneux, F., Dard M.-L.: Epidemiology of and Diagnostic Strategies for Toxoplasmosis. Clin Microbiol Rev. 2012 Apr; 25(2): 264–296.
18. Rothova, A., Meenken, C., Buitenhuis, H.J. et al.: Therapy for Ocular Toxoplasmosis. Am J Ophthalmol, 115; 1993 : 517-523.
19. Sahinoglu-Keskek, N., Unal F., Cevher, S. et al.: Cause of visual impairment in patiens with ocular toxoplasmosis. J Infect dev Ctries, 11; 2017 : 192-195.
20. Shah NJ, Shah UN.: Intravitreal ranibizumab for the treatment of choroidal neovascularization secondary to ocular toxoplasmosis. Indian J Ophthalmol. 2011;59(4):318-319.
21. Smit, S.A., Padalko, E., Acker, J.V. et al.: Public Health Impact of Congenital Toxoplasmosis and Cytomegalovirus Infection in Belgium, 2013: A Systematic Review and Data Synthesis. CID, 20; 2017 : 1-8.
22. Souza, C.E., Nascimento, H., Lima, A. et al.: Intravitreal Injection of Sulfametoxazole and Trimethoprim Associated with Dexamethasone as an Alternative Therapy for Ocular Toxoplasmosis. Ocul Immunol Inflamm, 00; 2017 : 1-4.
23. Surveillance Atlas of Infectious Diseases. Dataset provided by ECDC based on data - provided by WHO and Ministries of Health from the affected countries. Dostupné na WWW: < http://atlas.ecdc.europa.eu/public/index.aspx >.
24. Wallon, M., Garweg, J.G., Abrahamowicz, M. et al.: Ophthalmic Outcomes of Congenital Toxoplasmosis Followed Until Adolescence. Pediatrics, 133; 2014: e601-e608.
25.. Wallon, M., Peyron, F.: Congenital Toxoplasmosis: A Plea for a Neglected Disease. Pathogens, 7; 2018 : 25.
26. Zamora, Y.F., Arantes, T., Reis, F.A. et al.: Local treatment of toxoplasmic retinochoroiditis with intravitreal clindamycin and dexamethasone. Arq Bras Oftalmol, 78; 2015 : 216-219.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2018 Číslo 3- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- Ophthalmological finding in a patient with lowe syndrome
- Marshall and stickler syndrome in one family
- Congenital central toxoplasmic chorioretinitis - case study
- 24. výroční konference Eye Advance 2018
- Zemřela moje maminka, MUDr. Vlasta Doležalová, CSc.
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Conjuctival lesions - the relationship of papillomas and squamous cell carcinoma to HPV infection
- Ophthalmic manifestations of acute leukaemias
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Ophthalmic manifestations of acute leukaemias
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Congenital central toxoplasmic chorioretinitis - case study
- Marshall and stickler syndrome in one family
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




