-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Pachychoroid disease of the macula
Authors: A. Stepanov; J. Studnička; M. Středová; N. Jirásková
Authors place of work: Univerzita Karlova, Lékařská fakulta v Hradci Králové, katedra očního lékařství ; Fakultní nemocnice Hradec Králové, Oční klinika přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 1, p. 3-8
Category: Původní práce
Summary
Progress in optical coherent tomography (OCT) has recently provided new insights into variety of chorioretinal disorders. The use of EDI (Enhanced Depth Imaging) during OCT examinations and as well as OCT angiography provides a more accurate analysis of the choroid both quantitatively and qualitatively. „Pachychoroid“ (greek pachy- [παχύ] - thick) is defined as an abnormal and sustained increase in choroidal thickness ≥ 300 μm, which is mainly due to dilated choroidal vessels in the Haller’s layer and other structural changes in physiological choroidal architecture. Central serous chorioretinopathy is one of many macular diseases associated with „pachychoroid“. Another diseases that belong to the group of macular pachychoroid disorders are: pachychoroid pigment epitelopathy, pachychoroid neovasculopathy, polypoid choroidal vasculopathy. In this paper we summarize the current view on pachychoroid macular diseases and describe characteristics that are observed in multimodal imaging analysis of choroidal changes.
Key words:
optical koherence tomography, OCT, pachychoroid, EDI scanINTRODUCTION
Rapid advances in imaging methods of the posterior segment of the eye have brought new insights into the etiology and pathogenesis of chorioretinal disorders. An illustrative example of this trend is the development of optical coherence tomography (OCT). Since the first mention of examination of the retina using the OCT method in 1991 [17], further development has led to a marked improvement in the resolution of images and also to better quality imaging of the structure of the retina [1, 8, 15].
Spaide et al. in 2008 presented the OCT module EDI (Enhanced Depth Imaging), with improved display of the depth of the incision (fig. 1) [35], which enabled more precise structural and functional analysis of the retina and choroid [4].
Fig. 1. The EDI module (Cirrus Zeiss HD-OCT) is marked with the red arrow. 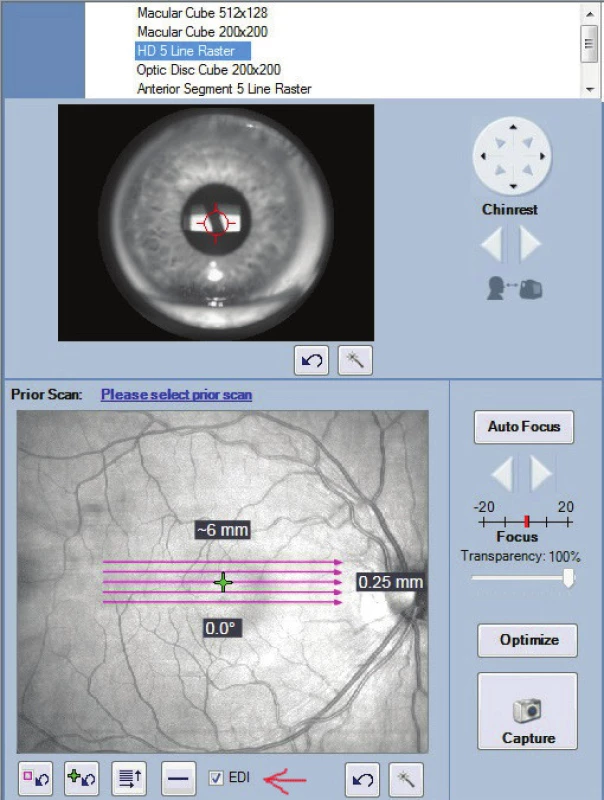
A current modern examination method is optical coherence tomographic angiography (OCTA), which enables imaging of both retinal and choroidal vascularisation without the use of a contrast substance, with the aid of non-invasive 3D imaging of blood flow [5].
According to histopathological subdivisions, the choroid forms the posterior part of the uveal tract, has an average thickness of 150 μm in its anterior section and 220 μm in the region of the posterior pole. It is composed of five layers: the Bruch's membrane (lamina basalis), choriocapillaris – capillaries with fine fenestrations that are supplied with nutrition by the external layers of the retina, the Sattler's layer – which is composed of medium sized capillaries of the choroid, the Haller's layer – composed of large capillaries of the choroid, and the suprachoroidal lamina (lamina fusca) (fig. 2).
Fig. 2. The anatomy of the choroid. Layers of choriocapilaris, Sattler's and Haller's layers are marked with arrows. 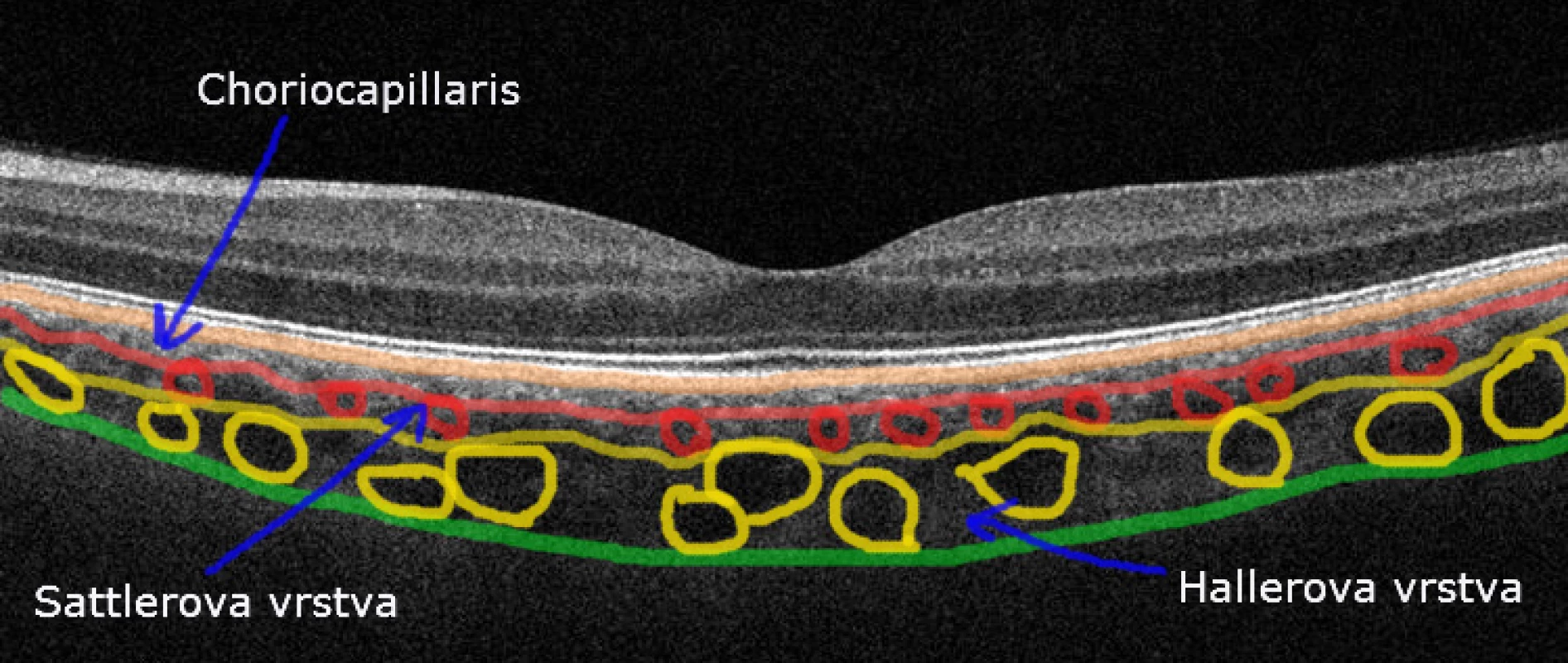
The term "Pachychoroid" (Greek pachy- [παχύ]: thick) was first used by Warrow et al. in 2013 [37]. It is defined as an abnormal and sustained increase in choroidal thickness ≥ 300 μm [32], which is mainly due to dilated choroidal vessels in the Haller’s layer, with its subsequent hyperpermeability. It has been demonstrated that choroidal thickness decreases with an increase in the age of the patient and the axial length of the eye [16, 23]. Temporary increase in choroidal thickness is generally linked with acute stages of severe posterior uveitis, for example Vogt-Koyanagi-Harada syndrome [24], multifocal choroiditis [34] and multiple white dot syndrome [2]. In the case of pachychoroid disease of the macula, this concerns a sustained increase in choroidal thickness. It is assumed that “pachychoroid” disease has an autosomally dominant type of heredity [7, 21, 39]. Depending on the further effect of various exogenous and/or endogenous factors, pachychoroid disease of the macula may occur.
The clinical unit of pachychoroid disease of the macula incorporates four different disorders, which are essentially individual stages of the same pathology:
- Pachychoroid pigment epitheliopathy (PPE);
- Central serous chorioretinopathy (CSC);
- Pachychoroid neovasculopathy (PNV);
- Polypoid choroidal vasculopathy (PCV).
With the progression of the pathology, a gradual transition to a further stage of the disorder takes place [6]. Their fundamental common features are: increase in thickness of the choroid, pathologically dilated vessels of the Haller's layer, thinning of the Sattler's layer and the layer of the choriocapillaris [6].
Pachychoroid pigment epitheliopathy
Pachychoroid pigment epitheliopathy was described by Warrow et al. in 2013 [37]. This unit can be considered a forme fruste or pre-stage of CSC. In addition to the above-mentioned common “pachychoroid” phenotype, PPE is typified by changes of the pigment sketch of the retina (fig. 3A) and other abnormalities of the retinal pigment epithelium (RPE) (fig. 3D), for example multiple small ablations thereof. Subretinal fluid and drusens are not evident. The choroid is typically thickened in the places of changes of the RPE, its larger thickness is conditioned by dilated choroidal vessels of the Haller's layer, with excessive thinning of the layer of the choriocapillaris and the Sattler's layer. These dilated vessels are located in close proximity to the complex of the RPE – Bruch's membrane, and thus mechanically contribute to the onset of pigment epitheliopathy. On ICGA (indocyanine green angiography) choroidal hyperpermeability is evident, which is manifested by hyperfluorescence correlating with the regions of breach of the RPE. Autofluorescence of the fundus is displayed as areas without sharp definition, of increased and reduced autofluorescence (obr. 3B). Pachychoroid pigment epitheliopathy may occur in isolated form or may be found also in the other eyes of patients affected by disorders of the “pachychoroid” spectrum, mainly in the case of CSC, in which we may find signs of PPE in as many as 61% of cases [9, 10].Fig. 3. The fundus of the eye of the patient with pachychoroid pigment epitheliopathy. A – changes of the retinal pigment drawing on color photography. B – areas of increased or decreased fundus autofluorescence. C – areas of hyperfluorescence correlated with destruction of RPE on FAG. D – RPE abnormalities on OCT. 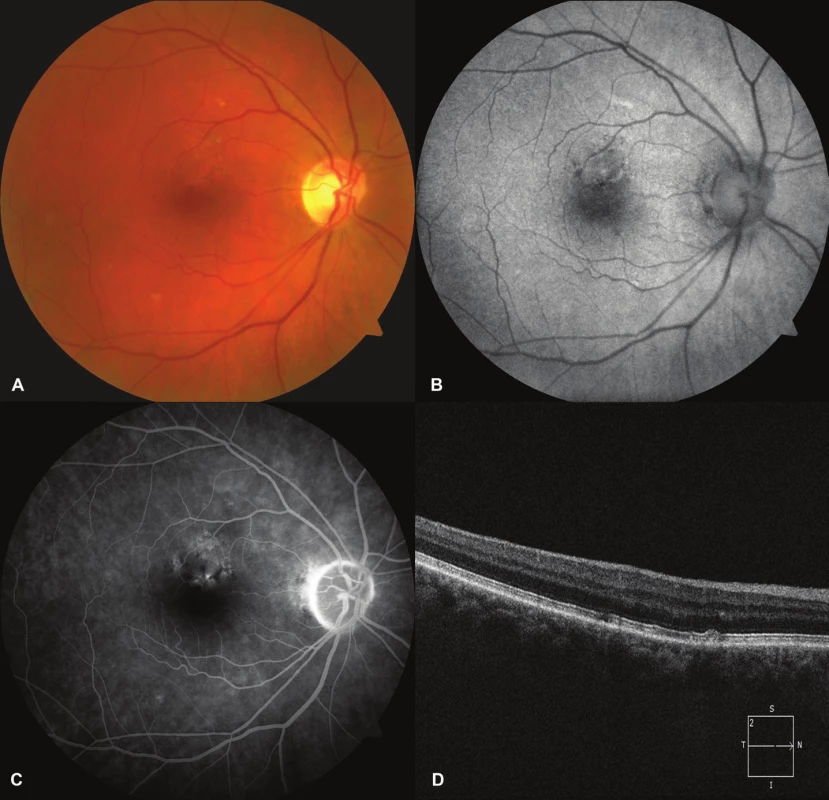
Central serous chorioretinopathy
As early as in 1866 Albrecht von Graefe first described a disorder of the macula with recurring detachment of the neuroretina, which he named “central recurring retinitis” [36]. In 1967 Gass presented a classic description of the pathogenesis and clinical course of this pathology, and named it idiopathic central serous choroidopathy [13]. At present we use the term central serous chorioretinopathy. This concerns the best known idiopathic recurring disorder of the macula, which is characterised by serous detachment of the neuroretina with or without ablation of the RPE [18, 26]. The pathology is easily diagnosed and forms the second stage of pachychoroid disease of the macula [6]. Exudation beneath the retina occurs as a result of increased hydrostatic pressure and permeability of the choroid, disorder of the Bruch's membrane and abnormalities of the RPE. Predisposing factors include type A personality, hypochondria, hysteria, use of corticoids (Cushing's syndrome), pregnancy, systemic hypertension, Japanese or South Asian race, SLE and psychopharmacological medication. Men are affected in 72-88% of cases of the pathology [33].
A typical finding is a rounded transparent deposit in the macula and discoid yellowish precipitates, which are evident thanks to the presence of a larger quantity of xanthophyll pigment (fig. 4A) [19]. Upon a longer course of the disease, we may find zones of thinning of the RPE and pigment abnormalities. During the course of the ablation of the neuroretina a range of changes take place, which are connected with a disorder of the metabolism in the retina. Cells of the RPE which have lost contact with the outer segments of the photoreceptors in the area of ablation do not have the capacity of phagocytosis. A progressive elongation of the photoreceptors takes place, with an accumulation of pathological material in the neuroretina [25]. On OCT we find ablation of the neuroretina (fig. 4B), which is sometimes complicated by ablation of the RPE. We may also find hyperreflective points on the lower edge of the ablation, which have stained hyperautofluorescence on autofluorescence of the fundus [27, 31]. Upon a longer duration of ablation of the neuroretina, apoptosis of the photoreceptors occurs, with an irreversible deterioration of visual acuity [28]. The subretinal fluid in the early stage of CSC is usually non-reflective, but in certain cases may be slightly hyperreflective as a result of the formation of fibrin [33]. Fibrin reaction usually disappears without consequences, with a subsequent deterioration of visual acuity.
#485077
Fluorescence angiography demonstrates one or more points of grading hyperfluorescence (fig. 4C-D), in certain cases of the character of a “factory chimney”, in which the colouring rises upwards beneath the neurosensory retina, at other times as a progressively enlarging “ink stain”. On ICGA we see deposits of choroidal vascular hyperpermeability especially in the middle phases of angiography [3, 6, 29].
Pachychoroid neovasculopathy
This unit was described by Freund et al. in 2015 [11]. Pachychoroid neovasculopathy is considered to be a late complication of PPE and CSC in patients who probably carry a genetic risk of choroidal neovascularisation [30]. A typical sign is the development of an occult choroidal neovascular membrane (CNV). Increased thickness of the choroid and the absence of drusens differentiates PNV from ARMD and other degenerative disorders which have a predisposition to the occurrence of CNV (fig. 5A, 5B) [14]. According to current opinion, the cause of occurrence of CNV is long-term pressure on the Bruch's membrane and subsequent ischaemia of the choriocapillaris and Sattler's layer, which generates an impulse for the proliferation of vessels of the Haller's layer. The vascular complex of CNV known as the “tangled network” beneath irregular ablation of the RPE is well displayed on OCTA [12, 26, 30]. A common secondary finding is focal dilation of the vessels of the choroid directly beneath CNV. It is assumed that not only the increase of the overall thickness of the choroid, but also the finding of dilated vessels plays a role in the pathogenesis of PNV [30].
Fig. 4. Pachychoroid neovasculopathy. A – ablation of the neuroretina, hard exudates and hemorrhage due to occult occult CNV in PNV. B – OCT finding, serous ablation of the neuroretina, hyper-reflective CNV and ablation of RPE. 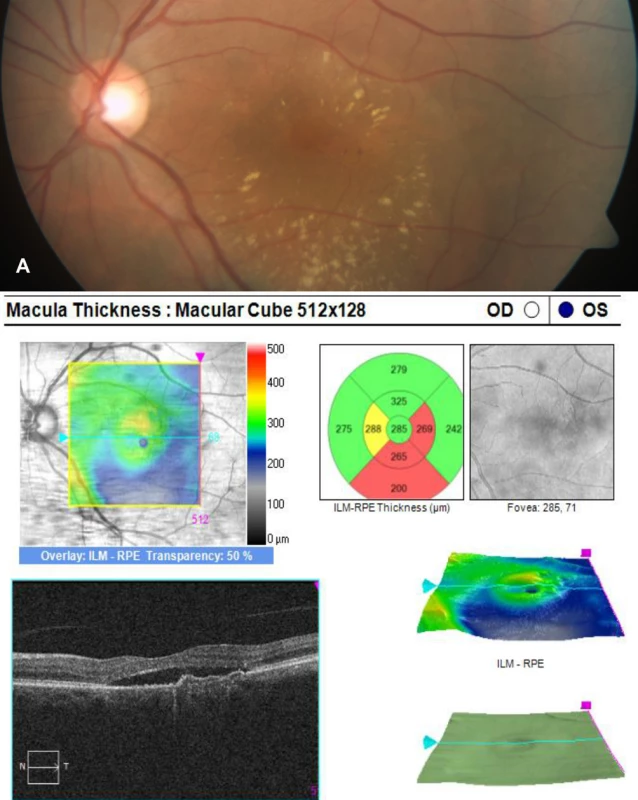
With regard to the fact that PPE and CSC have a similar etiology, cases of the occurrence of PNV are documented in patients with PPE, as well as without previous signs of CSC [30].
Polypoid choroidal vasculopathy
Polypoid choroidal vasculopathy was described by Yannuzzi et al. as a proliferation of the choroidal capillaries beneath the RPE and the development of aneurysms in the form of polyps on the tip of the capillary proliferation, with subsequent serous infiltration and haemorrhage [38]. This represents the last, most advanced stage of the spectrum of pachychoroid disease of the macula, which can be displayed with the aid of ICGA (obr. 6C) [20, 22].
PCV has a predilection for incidence in people of Asian or African race, but may also affect individuals of the white race. Clinically PCV is characterised by projecting orange-red deposits, often with polypoid ablation of the RPE, which can be found upon examination of the ocular fundus with the aid of ophthalmoscopy and biomicroscopy.
In histopathological examination of these lesions, choroidal capillary proliferation beneath the RPE was found, as well as the occurrence of aneurysms in the form of polyps on the endings of the capillary proliferations (fig. 6A). These polypoid structures cause serous and haemorrhagic infiltration beneath the RPE and neuroretina (fig. 6B, 6D), and in some patients may lead to haemorrhagic ablation of the RPE.
Fig. 5. Polypoid choroidal vasculopathy. A – polypoid lesion in the nasal part of the macula is marked with the red arrow, color photo. B – high polypoidal elevation of the RPE with surrounding ablation of the neuroretina. C – hyperfluorescence of polyp on indocyanine green angiography. D – fluorescein angiography findings. 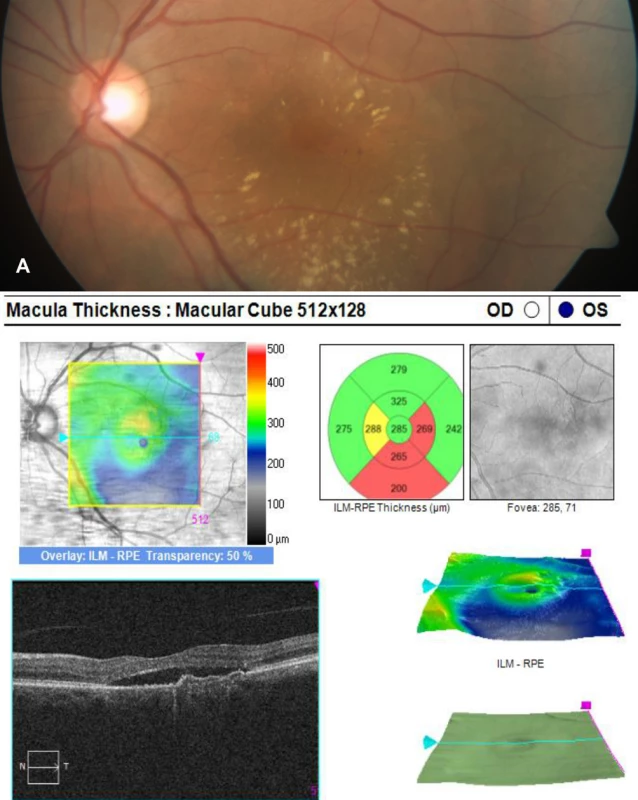
Conclusion
Use of the EDI module on classic OCT and modern methods of OCTA have provided a better understanding of the role of pathological changes of the choroid in CSC. Furthermore, they have helped define the term “pachychoroid” and detect pathologies linked with this finding. The spectrum of pachychoroid diseases is characterised by three common features: an increase in choroidal thickness ≥ 300 μm, dilation of the vessels of the Haller's layer and thinning of the layer of the choriocapillaris and the Sattler's layer.
These pathologies include CSC, upon which a role is played by choroidal congestion and hyperpermeability, with a subsequent occurrence of serous detachment of the neuroretina and RPE; PPE, which represents a forme fruste of CSC; PNV, which is characterised by the presence of occult CNV, and finally PCV, which is considered to be the most advanced form of pachychoroid disease of the macula.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
The study was presented in the form of a verbal communication at the annual congress of the Czech vitreoretinal society in Mikulov, 24.11.2017
Delivered to the editorial board 2.2.2018
Received for printing 14.3.2018
Dr. Alexandr Stepanov
Department of Ophthalmology, University Hospital Hradec Králové
Hradec Králové, Sokolská 581, 500 05
Zdroje
1. Alam, S., Zawadzki, RJ., Choi, S. et al.: Clinical application of rapid serial fourier-domain optical coherence tomography for macular imaging. Ophthalmology, 113(8); 2006 : 1425–31.
2. Aoyagi, R., Hayashi, T., Masai, A. et al.: Subfoveal choroidal thickness in multiple evanescent white dot syndrome. Clin Exp Optom, 95(2); 2012 : 212–7.
3. Arora, S., Pyare, R., Sridharan, P. et al.: Choroidal thickness evaluation of healthy eyes, central serous chorioretinopathy, and fellow eyes using spectral domain optical coherence tomography in Indian population. Indian J Ophthalmol, 64(10); 2016 : 747–751.
4. Azar, G., Wolff, B., Mauget-Faÿsse, M. et al.: Pachychoroid neovasculopathy: aspect on optical coherence tomography angiography. Acta Ophthalmol, 95(4); 2017 : 421-427.
5. Bonini Filho, MA., de Carlo, TE., Ferrara, D. et al.: Association of Choroidal Neovascularization and Central Serous Chorioretinopathy with Optical Coherence Tomography Angiography. JAMA Ophthalmol, 133; 2015 : 899–906.
6. Dansingani, KK., Balaratnasingam, C., Naysan, J. et al.: En face imaging of pachychoroid spectrum disorders with swept-source optical coherence tomography. Retina, 36(3); 2016 : 499–516.
7. de Jong, EK., Breukink, MB., Schellevis, RL. et al.: Chronic central serous chorioretinopathy is associated with genetic variants implicated in age-related macular degeneration. Ophthalmology, 122(3); 2015 : 562-70.
8. Drexler, W., Morgner, U., Ghanta, RK. et al.: Ultrahigh-resolution ophthalmic optical coherence tomography. Nat Med, 7(5); 2001 : 636.
9. Ersoz, MG., Karacorlu, M., Arf, S. et al.: Outer nuclear layer in pachychoroid pigment epitheliopathy. Retina, 2017: [Epub ahead of print]
10. Ersoz, MG., Karacorlu, M., Arf, S. et al.: Pachychoroid pigment epitheliopathy in fellow eyes of patients with unilateral central serous chorioretinopathy. Br J Ophthalmol, 2017: [Epub ahead of print]
11. Freund, KB., Pang, CE.: Pachychoroid Neovasculopathy. Retina, 35; 2015 : 1–9.
12. Fung, AT., Yannuzzi, LA., Freund, KB.: Type 1 (sub-retinal pigment epithelial) neovascularization in central serous chorioretinopathy masquerading as neovascular age-related macular degeneration. Retina, 32(9); 2012 : 1829–37.
13. Gass, JDM.: Pathogenesis of disciform detachment of the neuroepithelium. II. Idiopathic central serous choroidopathy. Am J Ophthalmol, 63; 1967 : 587–615.
14. Gemenetzi, M., De Salvo, G., Lotery, AJ.: Central serous chorioretinopathy: an update on pathogenesis and treatment. Eye, 24; 2010 : 1743–1756.
15. Gloesmann, M., Hermann, B., Schubert, C. et al.: Histologic correlation of pig retina radial stratification with ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci, 44(4); 2003 : 1696–703.
16. Goldenberg, D., Moisseiev, E., Goldstein, M. et al.: Enhanced depth imaging optical coherence tomography: choroidal thickness and correlations with age, refractive error, and axial length. Ophthalmic Surg Lasers Imaging, 43(4); 2012 : 296–301.
17. Huang, D., Swanson, EA., Lin, CP. et al.: Optical coherence tomography. Science, 254(5035); 1991 : 1178–81.
18. Chrapek, O., Řehák, J.: Léčba centrální serózní chorioretinopatie – naše zkušenosti. Čes. a slov. Oftal, 1; 2002 : 51-56
19. Ie, D., Yannuzi, LA., Spaide, RF. et al.: Subretinal exudative deposits in central serous chorioretinopathy. Br J Ophthalmol, 77; 1993 : 349–53.
20. Kawamura, A., Yuzawa, M., Mori, R. et al.: Indocyanine green angiographic and optical coherence tomographic findings support classification of polypoidal choroidal vasculopathy into two types. Acta Ophthalmol, 91(6); 2013: e474–e481.
21. Lehmann, M., Bousquet, E., Beydoun, T.: Pachychoroid: an inherited condition? Retina, 35(1); 2015 : 10-6.
22. Lin, WY., Yang, SC., Chen, SJ. et al.: Automatic segmentation of polypoidal choroidal vasculopathy from indocyanine green angiography using spatial and temporal patterns. Transl Vis Sci Technol, 4(2); 2015 : 7
23. Margolis, R., Spaide, RF.: A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol, 147(5); 2009 : 811–5.
24. Maruko, I., Iida, T., Sugano, Y. et al.: Subfoveal choroidal thickness after treatment of Vogt-Koyanagi-Harada disease. Retina, 31(3); 2011 : 510–7.
25. Matsumoto, H., Kishi, S., Otani, T. et al.: Elongation of photoreceptor outer segment in central serous chorioretinopathy. Am J Ophthalmol, 145; 2008 : 162–8.
26. Matušková, V.: Centrální serózní chorioretinopatie jako maskující syndrom choroidálního hemangiomu. Čes. a slov. Oftal, 72(6); 2016 : 209-214
27. Mrejen, S., Spaide, RF.: Optical coherence tomography: imaging of the choroid and beyond. Surv Ophthalmol, 58(5); 2013 : 387–429.
28. Ojima, A., Iida, T., Sekiryu, T. et al.: Photopigments in central serous chorioretinopathy. Am J Ophthalmol, 151; 2011 : 940–52.
29. Ooto, S., Kuroda, Y., Yoshimura, N.: Increased choroidal vascularity in central serous chorioretinopathy quantified using swept-source optical coherence tomography. Am J Ophthalmol, 169; 2016 : 199–207.
30. Pang, CE., Freund, KB.: Pachychoroid neovasculopathy. Retina, 35(1); 2015 : 1–9.
31. Pang, CE., Shah, VP., Sarraf, D. et al.: Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am J Ophthalmol, 158(2); 2014 : 362–371.e2.
32. Rosa, Dolz-Marco., Kunal, K., Dansingani, K.: The pachychoroid clinical spectrum. [online] Retina Today. May/June 2016. Dostupné na www: <http://retinatoday.com/2016/06/the-pachychoroid-clinical-spectrum/>.
33. Spaide, RF., Campeas, L., Haas, A. et al.: Central serous chorioretinopathy in younger and older adults. Ophthalmology, 103; 1996 : 2070–9.
34. Spaide, RF., Goldberg, N., Freund, KB.: Redefining multifocal choroiditis and panuveitis and punctate inner choroidopathy through multimodal imaging. Retina, 33(7); 2013 : 1315–24.
35. Spaide, RF., Koizumi, H., Pozzoni, MC.: Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol, 146(4); 2008 : 496–500.
36. Von Graefe, A.: Uebercentralerecidivierende retinitis. Graefes Arch Clin Exp Ophthalmol, 12; 1866 : 211–15.
37. Warrow, DJ., Hoang, QV., Freund, KB.: Pachychoroid pigment epitheliopathy. Retina, 33(8); 2013 : 1659–1672.
38. Yannuzzi, LA., Sorenson, J., Spaide, RF. et al.: Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina, 10(1); 1990 : 1-8.
39. Yoneyama, S., Sakurada, Y., Kikushima, W. et al.: Genetic factors associated with choroidal vascular hyperpermeability and subfoveal choroidal thickness polypoidal choroidal vasculopathy. Retina, 36(8); 2016 : 1535-41.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2018 Číslo 1- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Kontaktní dermatitida očních víček
-
Všechny články tohoto čísla
- Změna osmolarity slz po refrakčním zákroku
- Meningeómy zrakového nervu Očnice
- Pachychoroidní choroba makuly
- Implantácia intrastromálnych rohovkových segmentov s použitím femtosekundového lasera - naše skúsenosti
- Karcinóm z merkelových buniek mihalnice a očnice
- Použití ex-press® implantátu v chirurgii glaukomu - retrospektivní studie
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Pachychoroidní choroba makuly
- Meningeómy zrakového nervu Očnice
- Použití ex-press® implantátu v chirurgii glaukomu - retrospektivní studie
- Karcinóm z merkelových buniek mihalnice a očnice
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



