-
Medical journals
- Career
Indikace a výsledky ukončení těhotenství před 24. týdnem těhotenství – série případů
Authors: Sukran Doğru 1; Fatih Akkuş 1; A. A. Atci 1; A. C. Erdoğan 2; A. Acar 2
Authors‘ workplace: Department of Obstetrics and Gynecology, Division of Perinatology, Necmettin Erbakan University Medical School of Meram, Konya, Turkey 1; Department of Obstetrics and Gynecology, Necmettin Erbakan University Medical School of Meram, Konya, Turkey 2
Published in: Ceska Gynekol 2023; 88(6): 428-434
Category: Original Article
doi: https://doi.org/10.48095/cccg2023428Overview
Cíl: Cílem této studie bylo zhodnotit indikace ukončení těhotenství (TOP – termination of pregnancy) a porodnické výsledky před 24. gestačním týdnem. Materiály a metody: Jedná se o retrospektivní studii, která zahrnuje ukončení těhotenství prováděné u jednočetných těhotenství v období od prosince 2021 do prosince 2022 na perinatologické klinice Lékařské fakulty Necmettin Erbakan University Meram. Podle důvodů TOP byly všechny pacientky rozděleny do tří skupin: mateřské, fetální a porodnické důvody. Ve všech případech byl hodnocen způsob ukončení a výsledky. Výsledky: Do studie bylo zahrnuto celkem 210 pacientek. Pokud jde o indikace ukončení léčby, mělo 18 (8,5 %) pacientek mateřské příčiny, 127 (60,5 %) fetální příčiny a 65 (31 %) porodnické příčiny. Mateřské příčiny byly významně vyšší v I. trimestru a fetální příčiny ve II. trimestru (p = 0,001). V mateřské skupině bylo použito 77,8 % dilatace a kyretáže, 70,1 % misoprostolu a 29,9 % misoprostolu + Foleyho katétr ve fetální skupině a 66,2 % misoprostolu v porodnické skupině (p = 0,0001). Délka hospitalizace a rekurentní revizní kyretáž nebyly mezi fetální, mateřskou a porodnickou skupinou statisticky rozdílné (p = 0,099; p = 0,8). Výsledky: U komplikovaných těhotenství z fetálních, mateřských nebo porodnických důvodů by měla být nabídnuta možnost ukončení. Týden ukončení těhotenství a indikace ovlivňují morbiditu.
Introduction
Termination of pregnancy (TOP) is performed in many countries worldwide due to patient demand, fetal anomalies, and obstetric and maternal diseases. The decision to terminate a pregnancy is influenced by several factors, including national law and religion as well as personal factors, especially those of the personnel involved in the procedures. In some countries, termination can be done at later gestational weeks. It depends on that country‘s abortion law or institution‘s experience with termination [1]. According to our country‘s laws, terminations to be made for maternal and fetal obstetric reasons in advanced gestational weeks are made by the decision of the board formed by the physicians (official gazette, 1983) [2]. The increase in fetal anomaly diagnosis due to the development of prenatal screening tests and imaging methods has increased the termination rates due to fetal reasons. The fact that the fetus has multiple problems is the main reason why the families want to terminate the pregnancy [3]. Families are offered termination options for pregnancies that threaten the mother‘s life. Although the frequency of pregnancy termination due to maternal disease appears to be low, clinicians face difficulties in treating expectant mothers who refuse to terminate their pregnancies. It is known that maternal terminations are mostly recommended in the early weeks of pregnancy [4,5]. Cesarean scar pregnancy (CSP) is associated with high morbidity early in pregnancy and even maternal mortality. Preterm premature rupture of membranes (PPROM) at or before the limit of viability complicates 0.1% of pregnancies. When PPROM happens before the viability limit, there is a very low chance that the baby will live (less than 5–28%). This poses significant risks to the mother (postpartum hemorrhage, chorioamnionitis, and sepsis) [6].
The vast majority of pregnancy terminations occurred during the 1st trimester, with 78 percent occurring at ≤ 9 weeks and 92 percent occurring at ≤ 13 weeks of gestation. At later gestational ages of 14 to 20 weeks, 6.9% of abortions were carried out, and 1% occurred at 21 weeks or later [7]. Many methods are used for pregnancy termination. Surgical or medical methods can be used in 1st and 2nd trimester terminations. All options aim to reduce the time between termination induction and abortion and maternal morbidity. Compared with 1st trimester TOP, 2nd trimester TOP accounts for 10–15% of all TOPs but is associated with higher maternal complications [8]. Unfortunately, there are very few studies in which termination indications and the morbidity and mortality of termination results are given together. This study aimed to assess termination indications and obstetric outcomes before the 24th gestational week.
Materials and methods
This is a retrospective study that includes terminations performed in singleton pregnancies between December 2021 and December 2022 in the Perinatology Clinic of Necmettin Erbakan University (NEU) Meram Medical Faculty. Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as revised in 2013). This study was approved by the NEU ethics committee [Decree no: 2021/3338 (63249) ]. Demographic data, termination indications, and termination results of all patients included in the study were obtained from electronic file records. Pregnancies that were evaluated as having a dead fetus or twins in an ultrasound examination were excluded from the study. All patients were divided into three groups:
- maternal;
- fetal;
- obstetric reasons for termination.
Maternal chronic diseases (e. g., heart diseases), uncontrollable medical dis – eases (e. g., hypertension, thyroid, and diabetes that cannot be controlled by treatment), and teratogenic drug intakes were considered for maternal causes. The board evaluated the situation after consultation with the relevant branch physician in pregnancy terminations due to maternal illness. Chromosomal and structural anomalies constituted the fetal causes. After evaluation by at least two perinatologists and related branch physicians (such as pediatric cardiology and neurology) for fetuses diagnosed with a fetal anomaly, families were recommended TOP. The genetic examination was recommended for all patients diagnosed with a fetal anomaly, and only the results of those who accepted were evaluated. Chorionic villus bio psy (CVS) (especially in the 1st trimester), amniocentesis (AS) (especially in the 2nd trimester), or post-curative genetic examination were performed per gestation weeks. PPROM and CSPs that might advance to placenta accreta spectrum (patient was informed and the patient and family‘s wishes were taken into account) formed the obstetric causes in the study. For terminations after the 10th gestational week, approval was obtained from the triple-committee, one perinatologist, and two obstetricians and gynecologists. Since the viability limit is accepted as the 24th gestational week in our clinic, pregnancy terminations above this week are not performed. Feticide isn’t performed in our clinic. To assess the termination results, the study group was divided into two groups during the 1st trimester (4–136) and after the weeks (14–24) by subgroup analysis.
For termination, dilatation and curettage (D&C), misoprostol and misoprostol + Foley catheter (no. 26 was passed through the cervical canal, inflated to 30 cc, and cervical traction was applied) were applied to pregnancies between 4 and 24 weeks (mifepristone is unavailable in our country). These choices were made by considering the obstetric histories, weeks of gestation, and International Federation of Gynecology and Obstetrics (FIGO) 2017 recommendations of the patients [9]. Misoprostol dosing in TOP cases is highly dependent on the gestational age of the pregnancy. A successful termination was defined as fetal termination within 48 hours. If not, a catheter is added. Vacuum curettage was performed for the remaining tissues under anesthesia, accompanied by ultrasonography, in cases with abortions between 10–24 weeks. Dilatation evacuation (D&E) procedure was performed after cervical dilatation occurred in cases without expulsion of the fetus and appendages. If there was no cervical dilatation or if the patient‘s bleeding could not be stopped despite all these attempts, a hysterotomy was performed. All patients received 2 g of cefazolin before the procedure. Preoperative hemoglobin, postoperative hemoglobin values, blood transfusion, second revision curettage status, hysterotomy rates, and hospital stay were recorded for all patients.
Statistics
IBM SPSS.22 statistical package program was used in all analyses. Distribution of all data from normality was evaluated with Kolmogorov-Smirnov, Shapiro-Wilk Test and histograms. In descriptive statistics, mean + SD and median (min–max) were given together. Non-parametric tests were required for all of our data. Median (min–max) values were given in the descriptive statistics of continuous variables, and frequency (N) and percent (%) values were given in the definition of categorical variables. Relationships between categorical variables were analyzed by Chi-square analysis and significance was given as Pearson Chi-Square or Fisher‘s Exact Test. Parameters were compared in three groups according to termination etiologies using the Kruskal-Wallis Test. Bonferroni corrected Mann-Whitney U-test was used for pairwise comparison of groups according to etiology. First and 2nd trimester maternal morbidities were evaluated with the Mann-Whitney U-test. The statistical significance level was taken as P < 0.05.
Table 1. Characteristics of patients and indications for termination of pregnancy. Tab. 1. Charakteristika pacientek a indikace k ukončení těhotenství. 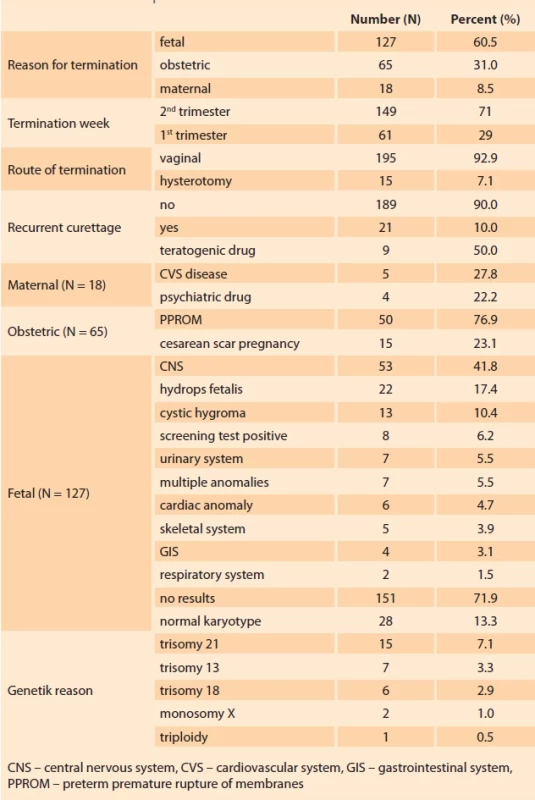
Table 2. Comparison of fetal, maternal, and obstetric indications for termination of pregnancy in 1st and 2nd trimesters. Tab. 2. Srovnání fetálních, mateřských a porodnických indikací k ukončení těhotenství v I. a II. trimestru. 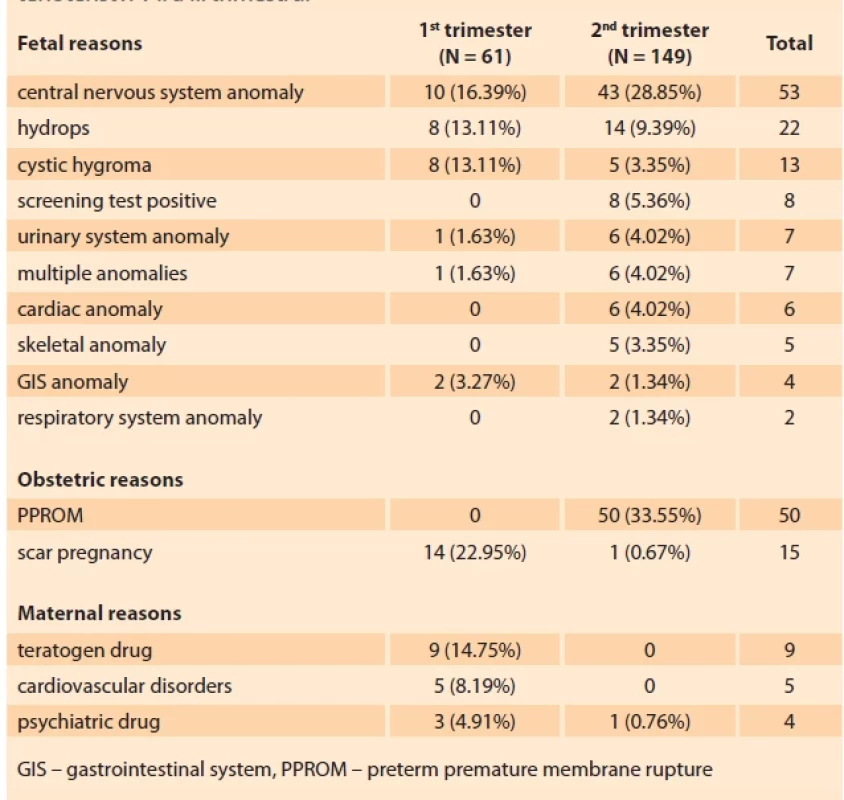
Results
A total of 210 patients were included in the study. The mean age of the pregnant women participating in the study was 29 (18–48). The mean termination week for the pregnant women was 15 (4–24). Out of the pregnant women who underwent termination, 29% (N = 61) were in the 1st trimester, and 71% (N = 149) were between 14 and 24 weeks gestation. Considering termination indications, 8.5% (N = 18) of patients had maternal causes, 60.5% (N = 127) had fetal causes, and 31% (N = 65) had obstetric causes. A vaginal termination was used in 92.9% (N = 195) of the cases. A central nervous system (CNS) anomaly was found to be higher in the fetal group (25.2%). Trisomy 21 was more common in the genetic test group (7.1%). PPROM was high among the obstetric reasons (23.8%), and teratogenic drug (6.2%) use was observed more frequently due to maternal reasons (Tab. 1).
When the 1st trimester indications were evaluated, 22.95% (N = 14) of the cases were terminated due to CSP. In the 1st trimester, 16.39% (N = 10) of cases were terminated due to a CNS anomaly and 14.75% (N = 9) from maternal teratogenic drug use. Pregnancy was terminated in the 2nd trimester as a result of a 33.55% (N = 50) PPROM and a 28.85% (N = 43) CNS anomaly (Tab. 2). When TOP patients were evaluated in the 1st and 2nd trimesters, hysterotomy was performed in 9.4% (N=14) patients in the 2nd trimester, and 1.6% (N=1) of patients in the 1st trimester (P = 0.048). D&C was used to terminate the pregnancy in the 1st trimester, and misoprostol and misoprostol plus a Foley catheter were used to terminate the pregnancy in the 2nd trimester (P = 0.0001). The length of hospital stay was statistically different in the 1st and 2nd trimester terminations [2.95 ± 2.16 (days, mean ± SD) vs 3.70 ± 2.31 (days, mean ± SD) (P = 0.002) ]. The number of patients who received a blood transfusion after the procedure was 3.3% (N = 2) in the 1st trimester and 13.4% (N = 20) in the 2nd trimester (P = 0.03). While the number of patients who underwent recurrent revision curettage was only 3.3% (N = 2) in the 1st trimester, it was 12.8% (N = 12) in the 2nd trimester (P = 0.038) (Tab. 3).
The termination week in the maternal group was significantly lower than in the fetal and obstetric groups [8 (range 4–15), 16 (range 10–24), and 16 (range 4–21), respectively, P = 0.001]. Considering the post-procedure hemoglobins in terminations made for fetal, maternal, and obstetric reasons, the decrease in hemoglobin in the obstetric group was statistically significant (P = 0.003). When the methods of termination were evaluated, 77.8% of women underwent a D&C, 70.1% of women underwent a misoprostol procedure, and 29.9% of women underwent a misoprostol procedure plus a Foley catheter (P = 0.0001) (Tab. 4).
Discussion
In this study, fetal, maternal, and obstetric causes of TOP were 60.5%, 8.5%, and 31%, respectively. The majority of fetal causes were structural fetal anomalies; the majority of maternal causes were teratogenic drug use; and PPROM was the most common reason for obstetric termination. Higher rates of post-procedure Hb decrease, blood transfusion, hospital stay, recurrent curettage, and hysterotomy were observed in 2nd trimester terminations. This study is one of the few studies that evaluates pregnancy terminations and outcomes along with their indications.
Although international termination reports are limited, there are a few studies investigating social, fetal, and maternal causes. The retrospective study examining the 5-year termination results revealed that 61.2% were due to social, 25.3% fetal, 16% maternal risks, and 6.3% maternal medical risks (cardiac, renal, and thyroid diseases) [5,10]. Vaknin et al. concluded that fetal structural anomalies were more common in late trimester terminations and genetic anomalies were more common in early week terminations. They reported that CNS anomalies among fetal causes accounted for one-quarter of the cases, and CVS anomaly rates were higher in the late termination group than in the literature [11]. In this study, while the rate of CNS anomaly was 25.2% in the group with fetal cause, the rate of cardiac anomaly was 2.9%. In our study, hydrops and cystic hygroma were more common in 1st trimester cases, while CNS anomalies and cardiac anomalies were more common in the 2nd trimester. In a study examining 144 cases of terminations performed in Israel, it was found that the most common indication for termination was fetal structural anomalies. The fetal CNS (29%) and fetal cardiac anomalies (26%) are the most common anomalies [12]. Examining maternal causes, an Australian study cites psychiatric disorders, malignancies, and heart conditions as the most common maternal indications for termination of pregnancy between 5 and 23 weeks of gestation. The World Health Organization recommends TOP to be recommended for cases who develop severe preeclampsia before the 23rd gestational week [13]. Maternal reasons for termination were found to be 10% in one study and 5% in another [6,14]. Teratogenic drug use was the most common maternal cause in our series. The low rates of maternal causes of TOP suggest that women use adequate contraception in the presence of the disease and that contraception is important [15,16]. In this study, when obstetric reasons were examined, the fact that pregnancy-related termination with CSP was 7.1% of the total indications revealed that the couples did not want a possible CSP. CSP are associated with high morbidity early in pregnancy (e. g., hemorrhage, uterine rupture, placenta accreta spectrum [PAS]) and even maternal mortality [17]. PPROM before or at the limit of viability complicates 0.1 to 0.7 percent of pregnancies. Counseling the patient with PPROM before or at the limit of viability about pregnancy complications and pediatric outcome is challenging. Chorioamnionitis complicates approximately 30 to 40 percent of PPROM cases before or at the limit of viability. Infection and abruption are potentially life-threatening maternal complications [18]. These results support that PPROM in the 2nd trimester is the cause of termination in our case series.
In this study, 24 weeks was determined as the termination limit and vaginal termination was applied first. Only 15 patients underwent hysterotomy. No hysterectomy was performed in any of the patients. We used misoprostol or D&C in 1st trimester patients, which we think is safe in this patient group [19–21]. In our clinic, we offer the option of termination using combined methods according to the literature. Due to patient diversity, it is impossible to apply a single method as a termination option. It seems safe to use mechanical dilators and uterotonic drugs at the same time, but if uterine rupture is a significant concern, it might be preferred to avoid doing that. It has been reported that misoprostol and the Foley catheter are safe in 2nd trimester pregnancy terminations. In the same study, it was shown that the use of misoprostol and a catheter shortened the termination time by 4 h [22]. It is known that 2nd trimester terminations have 3–5 times higher morbidity and mortality than 1st trimester terminations [23]. The method to be chosen affects this situation. In selecting the method, we consider the patient‘s age, obstetric history, previous surgical history, general health status, and patient request. In this study, hospital stays were long, blood transfusion rates were high, postoperative hemoglobin rates were low, and recurrent revision curettage rates were high in 2nd trimester cases. The history of the previous cesarean section did not change maternal morbidity in this case series. In the study by Garofalo et al., they compared the complications of the 1st trimester and 2nd trimester, demonstrating that the risk is high in terminations performed in the 2nd trimester, although there is no risk factor. They reported that unsuccessful intervention was due to inexperienced surgeons, uterine anomalies, advanced maternal and gestational age, and the number of previous surgeries [8,24]. Another study, following 1st trimester vacuum aspiration, stated that while 0.007% of procedures were complicated by vaginal bleeding that required hospitalization, in a large cohort study of D&E up to 26 weeks of gestation, blood loss of more than 500 mL was encountered in 0.9% of cases [19]. When a pregnancy is terminated between 13 and 24 weeks of gestation, Bryant et al. searched the morbidity of the procedure by either inducing labor or by D&E. Twenty-four percent of women undergoing induction and three percent of women undergoing D&E experienced at least one complication [25].
The limitations of our study are the low number of cases, its retrospective nature, the lack of detailed comparison of termination options (since patient characteristics and options are not similar), and the inability to perform genetic screening in all cases with fetal anomalies.
Table 3. Comparison of clinical parameters and outcomes of termination of pregnancy in 1st and 2nd trimesters. Tab. 3. Srovnání klinických parametrů a výsledků ukončení těhotenství v I. a II. trimestru. 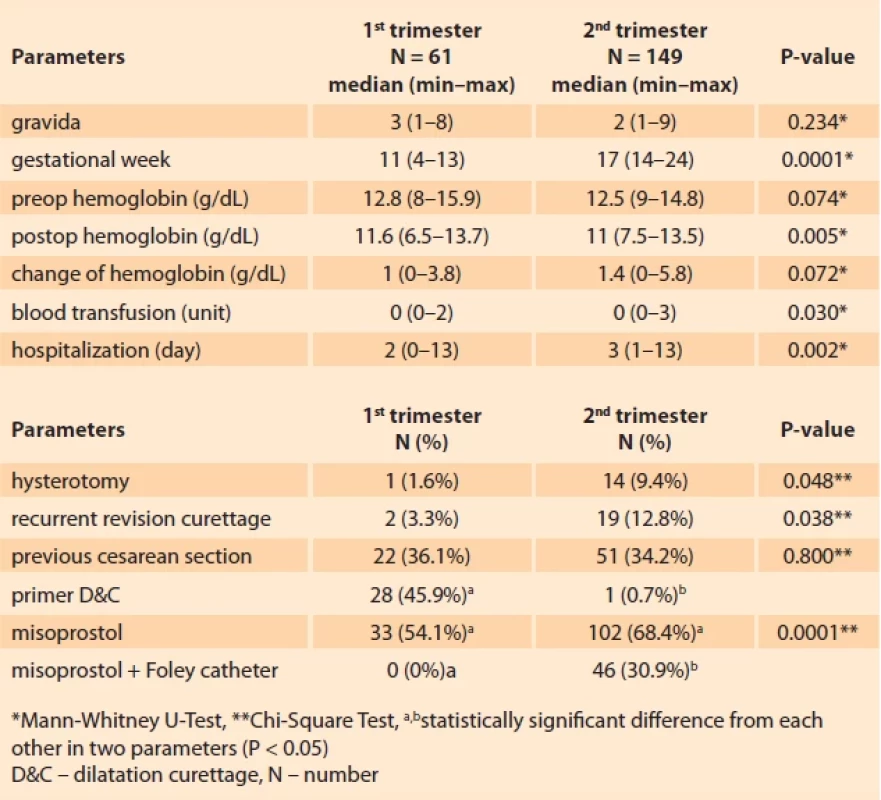
Table 4. Comparison of demographic and clinical parameters and outcomes of termination of pregnancy by fetal, obstetric, and maternal indications. Tab. 4. Porovnání demografi ckých a klinických parametrů a výsledků ukončení těhotenství podle fetálních, porodnických a mateřských indikací. 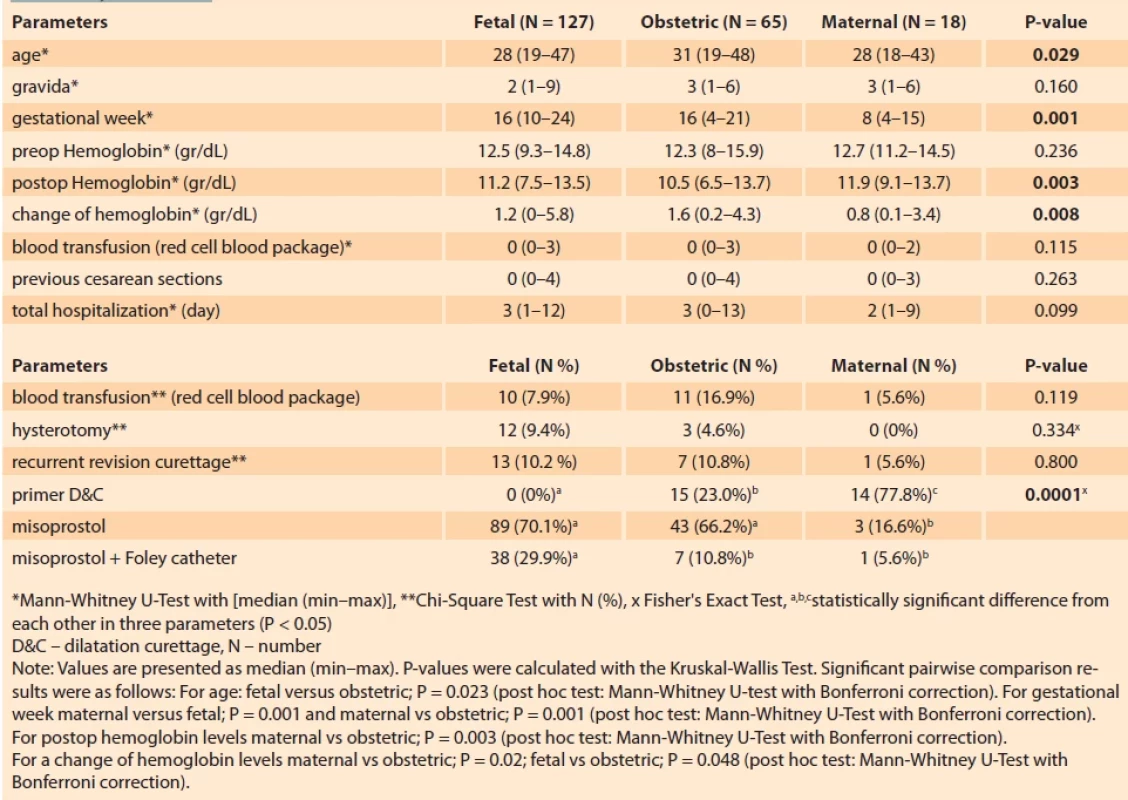
Conclusion
Termination options should be offered to all couples for problematic pregnancies due to fetal, maternal, or obstetric reasons. In this study, terminations due to fetal reasons were the most common situation. The gestational week and the indication for termination are associated with morbidity. Termination recommendation and termination process should be individualized according to the patient. The termination procedures used were successful in our series, except for the increase in 2nd trimester maternal morbidity.
Authorship:
SD: study design, patient management, and manuscript writing/editing
FA: data analysis, patient management
AAA: data analysis, patient management
ACE: data collection
AA: contributed to and approved of the final version of the manuscript
ORCID authors
Ş. Doğru 0000-0002-3383-2837
F. Akkuş 0000-0001-7037-9165
A. A. Atci 0000-0002-2637-3150
A. C. Erdoğan 0000-0001-5749-4134
A. Acar 0000-0002-9074-258X
Submitted/Doručeno: 20. 7. 2023
Accepted/Přijato: 28. 7. 2023Şükran Doğru, MD
Department of Obstetrics and Gynecology
Division of Perinatology
Necmettin Erbakan University Medical School
Yunus Emre, Akyokuş Street
42080 Meram/Konya
Turkey
Sukrandogru-2465@hotmail.com
Sources
1. Blondel B, Cuttini M, Hindori‐Mohangoo A et al. How do late terminations of pregnancy affect comparisons of stillbirth rates in Europe? Analyses of aggregated routine data from the Euro‐Peristat Project. BJOG 2018; 125 (2): 226–234. doi: 10.1111/1471-0528.14767.
2. Gürsoy A. Abortion in Turkey: a matter of state, family or individual decision. Soc Sci Med 1996; 42 (4): 531–542. doi: 10.1016/0277-95 36 (95) 00176-x.
3. Kose S, Altunyurt S, Yıldırım N et al. Termination of pregnancy for fetal abnormalities: main arguments and a decision‐tree model. Prenat Dia gn 2015; 35 (11): 1128–1136. doi: 10.1002/pd.4662.
4. Garne E, Loane M, Dolk H et al. Prenatal dia g – nosis of severe structural congenital malformations in Europe. Ultrasound Obstet Gynecology 2005; 25 (1): 6–11. doi: 10.1002/uog. 1784.
5. Monier I, Lelong N, Ancel PY A et al. Indications leading to termination of pregnancy between 22+0 and 31+6 weeks of gestational age in France: a population-based cohort study. Eur J Obst Gynecol Reprod Biol 2019; 233 : 12–18. doi: 10.1016/j.ejogrb.2018.11.021.
6. LeMoine F, Moore RC, Chapple A et al Neonatal survivability following previable PPROM after hospital readmission for intervention. AJP Rep 2020; 10 (4): e395–e402. doi: 10.1055/ s-0040-1721421.
7. Thompson KM, Sturrock HJ, Foster DG et al. Association of travel distance to nearest abortion facility with rates of abortion. JAMA Netw Open 2021; 4 (7): e2115530. doi: 10.1001/jamanetworkopen.2021.15530.
8. Garofalo G, Garofalo A, Sochirca O et al. Maternal outcomes in first and second trimester termination of pregnancy: which are the risk factors? J Perinat Med 2018; 46 (4): 373–378. doi: 10.1515/jpm-2017-0106.
9. Morris JL, Winikoff B, Dabash R et al. FIGO‘s updated recommendations for misoprostol used alone in gynecology and obstetrics. Int J Gynaecol Obstet 2017; 138 (3): 363–366. doi: 10.1002/ijgo.12181.
10. Choudhary N, Saha SC, Gopalan S. Abortion procedures in a tertiary care institution in India. Int J Gynaecol Obstet 2005; 91 (1): 81–86. doi: 10.1016/j.ijgo.2005.06.012.
11. Vaknin Z, Ben‐Ami I, Reish O et al. Fetal abnormalities leading to termination of singleton pregnancy: the 7‐year experience of a single medical center. Prenat Dia gn 2006; 26 (10): 938–943. doi: 10.1002/pd.1531.
12. Vaknin Z, Lahat Y, Barel O et al. Termination of pregnancy due to fetal abnormalities performed after 23 weeks’ gestation: analysis of indications in 144 cases from a single medical center. Fetal Dia gn Ther 2009; 25 (2): 291–296. doi: 10.1159/000229501.
13. van Eerden L, Zeeman GG, Page-Christiaens GC et al. Termination of pregnancy for maternal indications at the limits of fetal viability: a retrospective cohort study in the Dutch tertiary care centres. BMJ Open 2014; 4 (6): e005145. doi: 10.1136/bmjopen-2004-005145.
14. Ozyuncu O, Orgul G, Tanacan A et al. Retrospective analysis of indications for termination of pregnancy. J Obstet Gynaecol 2019; 39 (3): 355–358. doi: 10.1080/01443615.2018.1506 427.
15. Beksaç MS. Doğum Hekimliği – Meternal – Fetal Tıp’ta Etik ve Yasal Boyut. Ankara: Mebas Medikal Basin Yayin 2006 : 639–644.
16. Barrett HL, Lust K, Callaway LK et al. Termination of pregnancy for maternal medical indications: failings in delivery of contraceptive advice? Aust N Z J Obstet Gynaecol 2011; 51 (6): 532–535. doi: 10.1111/j.1479-828X.2011.013 71.x.
17. Calì G, Timor-Tritsch IE, Palacios-Jaraquemada J et al. Outcome of cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obstet Gynecol 2018; 51 (2): 169–175. doi: 10.1002/uog.17 568.
18. Abrahami Y, Saucedo M, Rigouzzo A et al. Maternal mortality in women with pre-viable premature rupture of membranes: an analysis from the French confidential enquiry into maternal deaths. Acta Obstet Gynecol Scand 2022; 101 (12): 1395–1402. doi: 10.1111/aogs.14 452.
19. Norwitz ER, Zelop CM, Miller DA et al. Evidence-based obstetrics and gynecology. Vol. Chapter 3. Oxford: John Wiley and Sons Ltd 2019.
20. Kulier R, Fekih A, Hofmeyr GJ et al. Surgical methods for first trimester termination of pregnancy. Cochrane Database Syst Rev 2001; 2001 (4): CD002900. doi: 10.1002/14651858.CD002900.
21. Tunçalp Ö, Gülmezoglu AM, Souza JP. Surgical procedures for evacuating incomplete miscarriage. Cochrane Database Syst Rev 2010; 2010 (9): CD001993. doi: 10.1002/14651858.CD001993.
22. Costescu D, Mui C. When there is only one patient: induction of labour for termination of pregnancy. Best Pract Res Clin Obstet Gynaecol 2022; 79 : 81–94. doi: 10.1016/ j.bpobgyn.2021.11.001.
23. Mazouni C, Provensal M, Porcu G et al. Termination of pregnancy in patients with previous cesarean section. Contraception 2006; 73 (3): 244–248. doi: 10.1016/j.contraception.2005.09. 007.
24. Kaunitz AM, Rovira EZ, Grimes DA et al. Abortions that fail. Obstet Gynecol 1985; 66 (4): 533–537.
25. Bryant AG, Grimes DA, Garrett JM et al. Second-trimester abortion for fetal anomalies or fetal death: labor induction compared with dilation and evacuation. Obstet Gynecol 2011; 117 (4): 788–792. doi: 10.1097/AOG.0b013e 31820c3d26.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicine
Article was published inCzech Gynaecology

2023 Issue 6-
All articles in this issue
- Je rozdíl mezi akutní appendicitou u těhotných a netěhotných žen?
- Jsou sérový neutrofilní delta index a systémový zánětlivý index užitečné jako prediktivní parametry preeklampsie a HELLP syndromu?
- Umělé ukončení těhotenství farmakologickou metodou (UUT-F) v I. trimestru – význam stanovení lidského choriového gonadotropinu a ultrazvukového vyšetření při diagnostice těhotenství a hodnocení výsledku UUT-F
- Indikace a výsledky ukončení těhotenství před 24. týdnem těhotenství – série případů
- Nový pohľad na diagnostiku a liečbu idiopatickej granulomatóznej mastitídy
- Ojedinělý případ živého abdominálního těhotenství u ženy s následnou graviditou v děloze
- Triandrická monogynická tetraploidia ako výsledok DNA analýzy parciálnej moly hydatidózy
- Výsledok pacientky s Herlyn-Werner-Wunderlichovým syndrómom liečenej balónikovou septostómiou – pred- a pooperačný ultrazvukový nález
- Metody a techniky ochrany reprodukce u pacientek s endometriózou
- Asistovaná aktivace oocytů
- Vliv stavu pánevního dna na výsledek operačního řešení sestupu pánevních orgánů
- Preeklampsie a diabetes mellitus
- Diagnostika komplikovaných gynekologických zánětů pomocí výpočetní tomografie – zkušenosti jednoho centra
- Emergentní hysterektomie pro spektrum placenta accreta – některé další techniky
- Diagnostika a léčba endometriózy: Doporučený postup Sekce pro léčbu endometriózy ČGPS ČLS JEP
- Czech Gynaecology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Diagnostika a léčba endometriózy: Doporučený postup Sekce pro léčbu endometriózy ČGPS ČLS JEP
- Preeklampsie a diabetes mellitus
- Asistovaná aktivace oocytů
- Je rozdíl mezi akutní appendicitou u těhotných a netěhotných žen?
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

