-
Medical journals
- Career
Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
Authors: Š. Rusňák; L. Hecová
Authors‘ workplace: Přednosta: MUDr. Štěpán Rusňák, Ph. D., alej Svobody 60, 304 60 Plzeň ; Fakultní nemocnice Plzeň, Oční klinika
Published in: Čes. a slov. Oftal., 76, 2020, No. 1, p. 14-23
Category: Original Article
doi: https://doi.org/10.31348/2020/2Overview
Purpose: Penetrating eye trauma with an intraocular foreign body is very frequent, especially in men in their productive age. Pars plana vitrectomy would be the standard surgical method at our department. However, in indicated cases (metallic intraocular bodies in the posterior eye segment in young patients with well transparent ocular media without detached ZSM and without any evident vitreoretinal traction) transscleral extraction of the intraocular foreign body is performed using the exo magnet, eventually endo magnet with a minimal PPV without PVD induction under the visual control of endo-illumination.
Materials and Methods: Between June 2003 and June 2018, 66 eyes of 66 patients diagnosed with a penetrating eye trauma caused by an intraocular foreign body located in the posterior eye segment were treated. In 18 eyes (27,3 %) with a metallic foreign body in vitreous (body) or in retina, no PPV or a minimal PPV without PVD was used as a surgical method. In the remaining 48 eyes (72,7 %), a standard 20G, respectively 23G PPV method were used together with PVD induction and the foreign body extraction via endo or exo magnet.
Conclusions: As demonstrated by our survey/study, in the cases of a thoroughly considered indication an experimented vitreoretinal surgeon can perform a safe NCT transscleral extraction from the posterior eye segment via exo magnet, eventually endo magnet under the visual control of a contact display system with a minimal PPV. Thereby, the surgeon can enhance the patient´s chance to preserve their own lens and its accommodative abilities as well as reduce the risk of further surgical interventions of the afflicted eye.
Keywords:
penetrating eye trauma – metallic IOFB – exomagnet/endomagnet – transscleral extraction – minimal PPV – limited PPV – vitreoretinal traction
INTRODUCTION
Penetrating eye trauma with an intraocular foreign body constitutes 10 – 40 % [3,7,10,21] of all injuries to the eyeball. This type of injury primarily affects men of productive age [10,11]. Injuries usually occur in the workplace (54 – 72 %) or at home (30 %) [6]. The mechanism of injury is most often an impact of metal on metal (60 – 80 %) [6].
An intraocular foreign body always means a severe ocular trauma, and may lead to blindness or loss of the eyeball [4,20]. It may be localised in the anterior (anterior chamber, iris and lens) or posterior segment of the eye (vitreous body, retina, choroid), and may be diagnosed directly (biomicroscopically, by direct or indirect ophthalmoscope or perioperatively by surgical microscope) or, primarily in the case of poorly transparent ocular media, indirectly with the aid of imaging methods (ultrasound, UBM, X-ray image, computer tomography, in the case of unequivocally non-metallic foreign bodies also magnetic resonance) [13] (Fig. 1).
1. Metallic intraocular foreign body (IOFB) in CT image 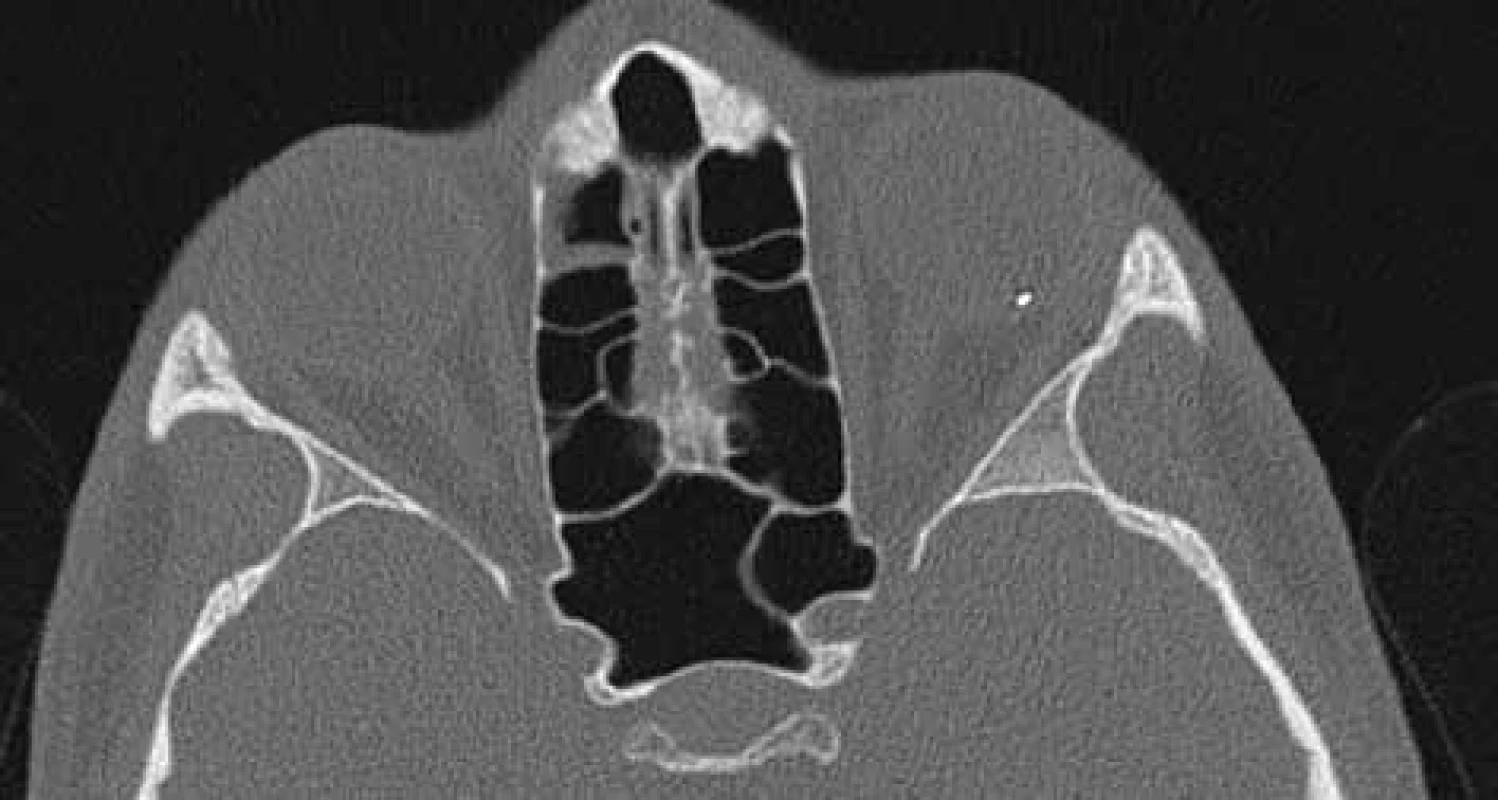
A metallic intraocular foreign body can be removed from the posterior segment of the eye by a number of methods – transscleral extraction by exo magnet or extraction by endo magnet with partial or complete PPV. With regard to the risk of progression of severe postoperative complications (above all the risk of vitreoretinal traction with the potential progression of tractional retinal detachment and the risk of endophthalmitis) [6,12], and in the case of transscleral extraction or extraction by endo magnet with partial PPV, at present the preferred method is extraction by endo magnet with full PPV. However, even the method of PPV brings with it a range of potential complications – above all the progression of early cataract and maculopathy [2,5], or postoperative retinal detachment [17]. Especially in younger patients, this can lead to a loss of central visual acuity and accommodative capacities at a young age.
For this reason, in the case of metallic intraocular foreign bodies in the posterior segment of the eye in young patients with no or minimal injury to the lens, who had with a well transparent vitreous body without signs of retinal traction and were without a detached posterior vitreous membrane, at our centre we perform transscleral extraction of the intraocular foreign body by exo magnet. In cases in which it is not possible to use an exo magnet safely, we use the technique of extraction of the foreign body by an endo magnet with minimal or no PPV, under visual control with the aid of a contact display system (AVI, Advanced Visual Instruments).
METHOD
We retrospectively processed data on patients who were treated at our centre between June 2003 and June 2018, with a diagnosis of penetrating eye trauma with an intraocular foreign body localised in the posterior segment of the eye. According to the type of surgical procedure, we divided the patients into 2 groups: group 1 comprises patients in whom the intraocular foreign body (hereinafter IOFB) was removed with the aid of transscleral extraction by exo magnet or endo magnet, with minimal PPV and without PVD, group two consists of patients in whom complete PPV with PVD was performed. In both groups we observed the baseline and resulting best corrected visual acuity (BCVA), the ocular trauma score (OTS), the incidence of early and late postoperative complications and the type of subsequent surgical procedures.
Before the actual surgical procedure, in the case of group 1 we first of all verified the ferromagnetic properties of the foreign bodies – under visual control under a microscope we applied a pencil exo magnet and observed the reaction of the intraocular body to the presence of the magnet.
Before transscleral extraction of the IOFB with an exo magnet, we first of all determined the current position of the intraocular foreign body with the aid of an indirect ophthalmoscope (Fig. 2). The quadrant for extraction of the foreign body was selected with regard to the entry wound, and above all to the current position of the intraocular foreign body. A peritomy of the bulbar conjunctiva was performed, and subsequently a 1.5 mm – 3 mm long sclerotomy located 4.5 mm from the limbus. The pencil exo magnet was applied to the sclerotomy, and under visual control by indirect ophthalmoscope the foreign body was slowly extracted to the tip of the exo magnet (Fig. 3). Eventually, the intraocular foreign body was carefully vacuumed by sclerotomy under visual control under a surgical microscope.
2. Determination of current position of intraocular foreign body by indirect ophthalmoscope 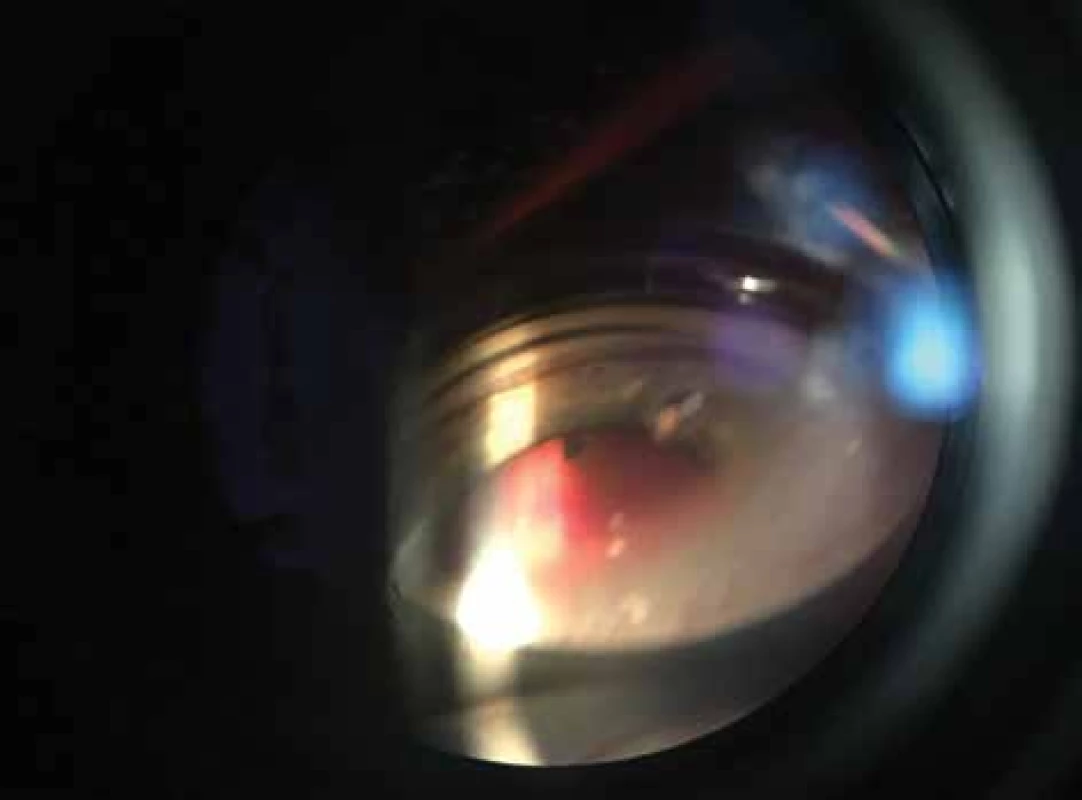
3. Extraction of IOFB to tip of exo magnet 
In the case of extraction of the IOFB by endo magnet, we inserted two 23G or 20G ports. One port serves for the light source, the second port is an endo magnet inserted into the eye, with the aid of which the IOFG is slowly extracted from the vitreous body under visual control under a surgical microscope. The same port may also serve for the insertion of an endo laser for laser treatment of the place of impact, or a vitrectom for the performance of minimal PPV in the area of the tunnel.
In all patients from group 1, thorough repositioning of the vitreous fibres was conducted at the end of the procedure, the sclerotomy was closed by a suture, and subsequently external cryoretinopexy of the area of the sclerotomy was performed. All the procedures were performed by 2 experienced vitreroretinal surgeons, after the patients had received detailed instructions and signed an informed consent form.
RESULTS
Between June 2003 and June 2018 we treated 66 eyes of 66 patients at our centre, with a diagnosis of penetrating eye trauma with an intraocular foreign body localised in the posterior segment of the eye. These were exclusively men aged between 18 and 70 years (mean 32.4 years, median 35.5 years).
In a total of 18 cases (27.3 %) (group 1) with a metallic foreign object in the vitreous body or in the retina with will transparent ocular media, without signs of haemorrhage into the vitreous body or with minimal haemophthalmos, without a detached posterior vitreous membrane and without significant affliction of the retina, we decided to use a surgical technique without PPV, or with minimal PPV without PVD. This was a group of men aged between 18 and 70 years (mean 35.1 years, median 32 years). The entry wound was located in the pars plana region (6 eyes), in the cornea (11 eyes), in one case it concerned a combined sclerocorneal wound. In 14 of these cases (77.8 %), this concerned an occupational injury. Baseline best corrected central visual acuity was 0.008 – 1.0 (mean 0.7, median 0.9). The ocular trauma score (OTS) in these patients was 3 (5 eyes, 27.8 %) and 4 (13 eyes 72.2 %) (Table 1).
1. Group of patients, characteristics of injury and surgical procedure 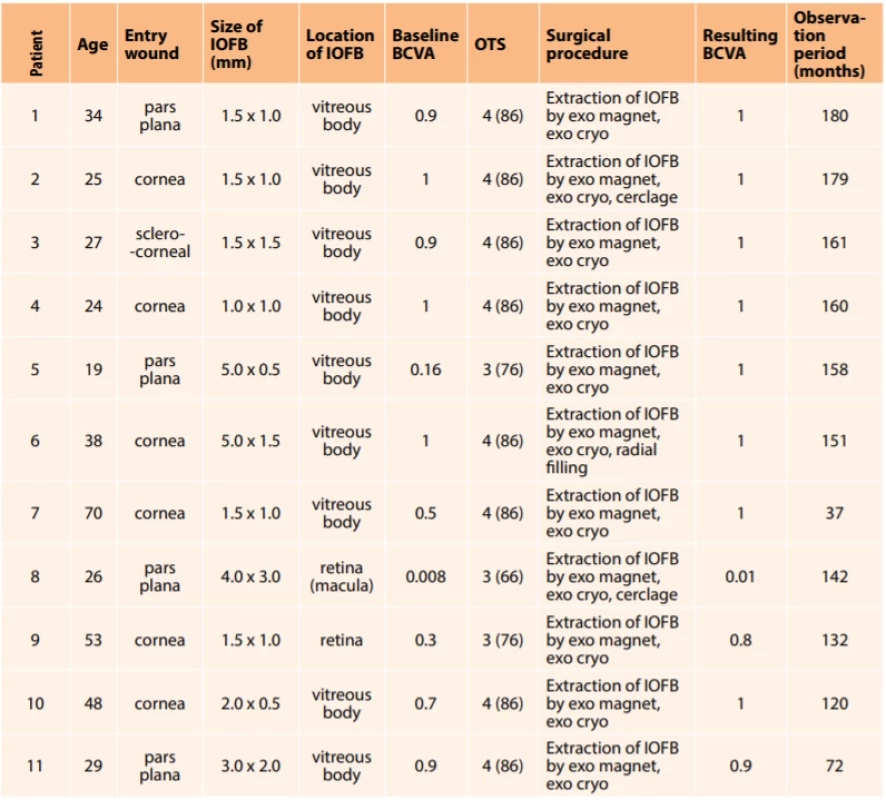
2. Group of patients, characteristics of injury and surgical procedure 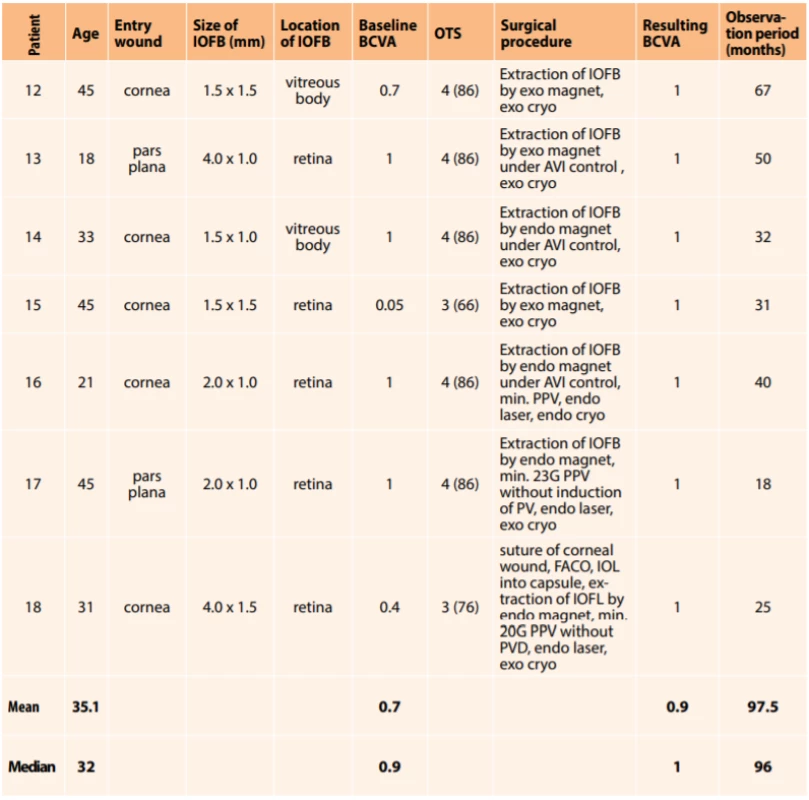
Note: BCVA = Best Corrected Visual Acuity In 14 cases the method of transscleral extraction of a foreign body from the vitreous body using an exo magnet was used, in 1 patient the foreign body was extracted from the vitreous body with an endo magnet under AVI control without PPV, in 2 cases extraction of a foreign body from the retina with an endo magnet was performed, with limited vitrectomy around the base of the body and endo laser treatment of the place of impact, and in 1 patient this procedure was extended with suturing of the corneal wound and phacoemulsification with implantation of an IOL into the capsule. In 2 cases 360° cerclage was performed, in 1 case a radial filling was sewn in. At the end of the surgical procedure, cryoretinopexy was performed on all patients in the area of the sclerotomy, or on the retina in the place of impact of the foreign body. The surgical procedure was performed 0 – 10 days after the primary injury (mean 3.5 days, median 1.5 days). In all patients, broad-spectrum antibiotics were administered intravenously for a period of 7 – 10 days (Fig. 4, 5, 6 and 7).
4. Patient no. 16 – intraocular finding before procedure and development of scar after extraction of IOFB and endo laser treatment 
5. Patient no. 16 – OCT finding before extraction of IOFB and after healing 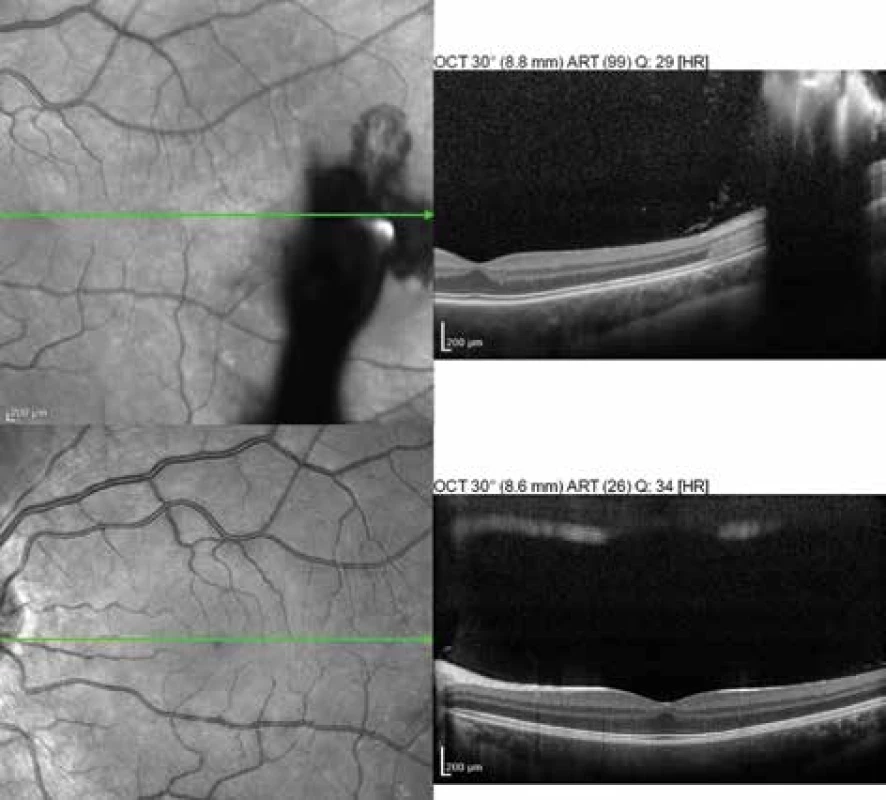
6. Patient no. 13 – finding before procedure and development of scar after extraction of IOFB and external cryoretinopexy 
7. Patient no. 13 – finding 40 weeks after procedure 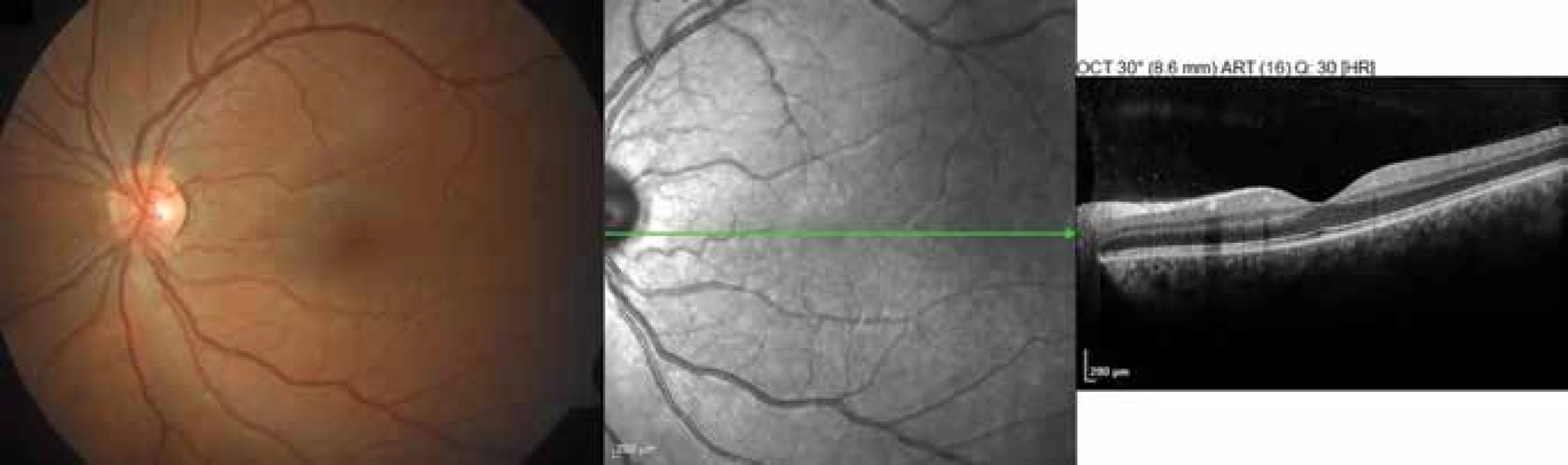
BCVA at the last follow-up examination was within the range of 0.01 – 1.0 (mean 0.93, median 1.0).
In 2 patients sporadic partial haemophthalmos was present at the baseline examination, which was gradually spontaneously reabsorbed.
In 8 patients a traumatic cataract was determined at the baseline examination – in 1 case the condition of the lens required a surgical solution (phacoemulsification and implantation of IOL into the capsule) together with extraction of the IOFB by endo magnet, in 1 case traumatic cataract surgery was performed 14 months after the injury. In the remaining 6 patients, the traumatic cataract is minimal and does not influence central visual acuity (in all cases the last BCVA is 1.0). During the course of the observation period (37 – 179 months) the cataract did not progress significantly.
We recorded a postoperative complication in 1 patient with an IOFB originally localised in the macular region, in the form of tractional maculopathy with BCVA of 0.008. A tractotomy of the vitreoretinal band was performed 3 months after the injury, postoperative BCVA initially improved to 0.2, but a progressive decrease of BCVA to 0.01 was observed as a consequence of the progression of chorioretinal atrophy in the place of impact of the IOFB.
Another recorded postoperative complication was decentration of an IOL – the condition required surgical repositioning of the IOL 25 months after the injury.
In group 1 therefore 3 patients (16.7 %) underwent a further surgical procedure after extraction of the IOFB (cataract surgery, repositioning of IOL, tractotomy of vitreoretinal tractional band by vitrectom), in the remaining 15 patients (83.7 %) the condition did not require and further surgical procedure during the observation period (mean 97.5 months, median 96 months).
Group 2 comprises 48 eyes (72.7 %) of 48 patients aged between 21 and 77 years (mean 44.3 years, median 43.5 years), who were operated on with the aid of a standard 20G or 23G PPV technique, with induction of PVD and extraction of the intraocular foreign body by an endo magnet or exo magnet. Baseline BCVA was very diverse, from unclear light projection to 1.0 (mean 0.33, median 0.05). The entry wound was scleral in 15 patients, in the cornea in 24 patients, and sclerocorneal in 9 patients. Extraction of the IOFB was performed 0 – 13 days (mean 3.25 days, median 3 days) after the injury. In 8 cases, cerclage was performed together with the procedure. In 30 patients lensectomy was performed without implantation of an IOL, in 1 case phacoemulsification was performed with implantation of an IOL. In 12 cases an antibiotic was applied into the vitreous cavity due to signs of incipient endophthalmitis. In 37 eyes silicone oil was implanted into the eye, in 8 cases gas. Resulting BCVA is within the range of amaurosis to 1.0 (mean 0.28, median 0.06).
In 11 patients (21.9 %), the condition after the extraction of the IOFB did not require a further surgical procedure, 14 eyes (29.2 %) underwent 1 surgical procedure during the observation period, 10 eyes (20.8 %) underwent 2 surgical procedures, in 8 cases (16.7 %) 3 further surgical procedures were performed, in 3 eyes (6.3 %) it was necessary to perform 4 subsequent surgical procedures and in 2 eyes (4.2 %) the condition required a further 5 operations. In 15 aphakic patients, secondary implantation of an IOL was performed (of which in 9 cases anterior chamber), in 9 patients phacoemulsification was performed with implantation of a posterior chamber IOL. In 16 cases (33.3 %) tractional or rhegmatogenous retinal detachment was determined and operated on, in which 5 of these cases were recurring. In 3 patients a secondary epiretinal membrane developed, which required a surgical solution.
With regard to the very diverse finding in group 2, we divided the patients into subgroups on the basis of a calculation of OTS – OTS 1 was determined in 5 patients (10.4 %), OTS 2 in 16 patients (33.3 %), OTS 3 in 14 patients (29.2 %) and OTS 4 in 13 patients (27.1 %).
We compared the postoperative results of the patients from groups 1 and 2 with analogous baseline parameters, i.e. OTS 3 and OTS 4 (Table 2).
3. Division of groups 1 and 2 into subgroups according to Ocular Trauma Score (OTS) and comparison of results 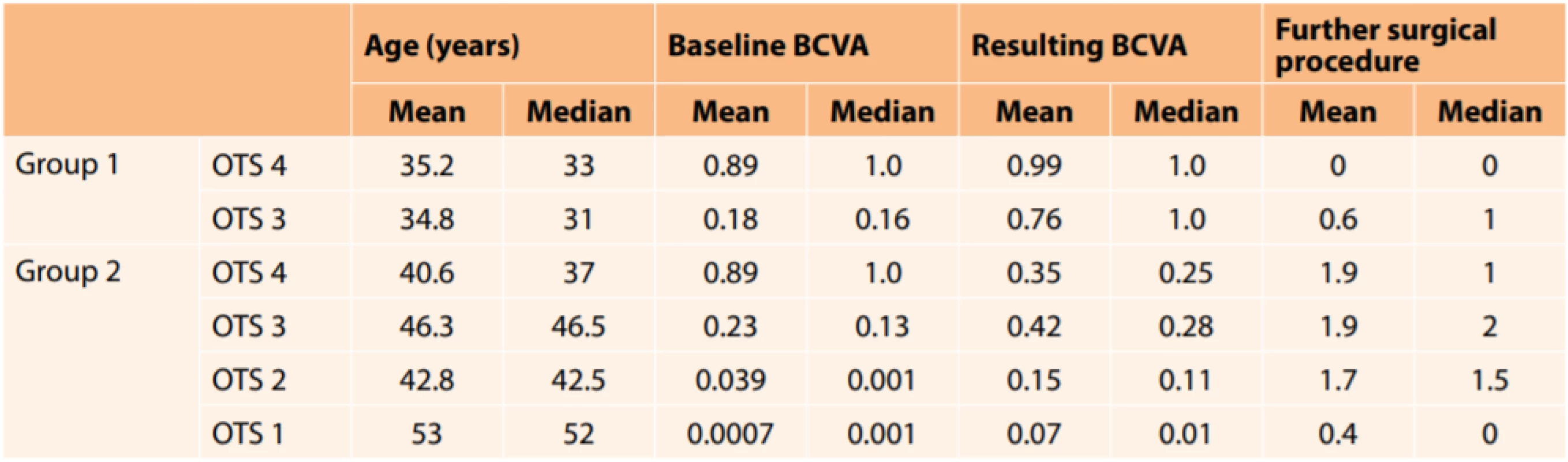
Note: BCVA = Best Corrected Visual Acuity In patients with OTS 3 in group 1, resulting BCVA was within the range of 0.01 to 1.0 (mean 0.762, median 1.0). In 1 case, within the framework of the primary procedure, phacoemulsification with implantation of an IOL into the capsule was performed, and in 1 eye cerclage was performed. In a total of 3 patients the condition required 1 further surgical procedure (tractotomy of VR tractional band by vitrectom, traumatic cataract surgery, repositioning of IOL). In group 2 with the same OTS, resulting BCVA was within the range of certa to 1.0 (mean 0.42, median 0.28). In this group, silicone oil was implanted within the framework of the primary procedure in 13 cases, the postoperative finding enabled aspiration of the silicone oil in 12 cases, in 1 case continuous tamponade of the SO is required. In 2 eyes cerclage was performed. Furthermore in group 2, within the framework of the primary procedure, lensectomy without implantation of an IOL was performed in 7 cases, and in 1 eye phacoemulsification with implantation of an IOL (suspension) was performed, secondary implantation of an IOL was performed in 4 eyes (in 3 cases an anterior chamber IOL was implanted), and phacoemulsification with implantation of an IOL in the second time was performed in 3 cases. In 6 eyes tractional retinal detachment occurred, in 2 cases this was recurring, and in 1 eye peeling of the epiretinal membrane was performed.
In patients with OTS 4 in group 1, resulting BCVA was within the range of 0.9 to 1.0 (mean 0.99, median 1.0). Within the framework of the primary procedure, cerclage was performed on 1 eye, and a radial filling was sewn in on 1 eye. The postoperative development did not require a further surgical procedure on any of the eyes. In group 2 with the same OTS, resulting BCVA was within the range of 0.02 to 1.0 (mean 0.35, median 0.25). Within the framework of the primary procedure, expansive gas was implanted in 7 eyes and silicone oil in 5 eyes, and the postoperative finding enabled aspiration of the silicone oil in 3 cases. Cerclage was performed on 1 eye. In addition, within the framework of the primary procedure, lensectomy without implantation of an IOL was performed in 6 cases, secondary implantation of an IOL was performed in 5 eyes (in 4 cases an anterior chamber IOL was implanted, in 1 case a posterior chamber IOL into the capsule), and phacoemulsification with implantation of an IOL in the second time was performed in 3 cases. Within the framework of a further surgical procedure, lensectomy was performed without implantation of an IOL in 1 eye, and in 4 eyes phacoemulsification with implantation of a posterior chamber IOL was performed. In 6 eyes tractional retinal detachment occurred, in 1 case recurring.
DISCUSSION
Penetrating eye trauma with an intraocular foreign body in the region of the posterior segment of the eye is a serious condition, with the risk of permanent reduction of central visual acuity to blindness of the eye or loss of the eyeball. The severity of this type of trauma consists above all in the risk of progression of an infectious complication, toxic reaction to the foreign body, and the scope of the ocular lesion in the course of the intraocular trajectory of the foreign body [16]. The following have been defined as negative prognostic factors: size of intraocular foreign body larger than 5 mm2, presence of relative afferent pupillary defect (RAPD), prolapse of intraocular tissues, presence of retinal detachment or haemorrhage into the vitreous body upon initial examination, and baseline visual acuity worse than 0.1 [8,14,16].
The visual prognosis of injury to the eyeball may be predicted with the aid of the Ocular Trauma Score (OTS) described by Kuhn et al. in 2002 [9]. Calculation of the OTS is performed on the basis of the patient’s baseline Best Corrected Visual Acuity (BCVA) and the presence of 5 variables – rupture of eyeball, endophthalmitis, perforating injury, retinal detachment, RAPD. The resulting OTS score is stratified into 5 groups, which reflect the expected range of central visual acuity of the eye 6 months after injury (Tables 3 and 4).
4. Ocular Trauma Score (OTS) – reproduced according to Kuhn et al. [15] ![Ocular Trauma Score (OTS) – reproduced according to Kuhn et al. [15]](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image_pdf/a6e9e646967e41594098a9fb56ec1ad6.png)
Note: RAPD = Relative afferent pupillary defect 5. Calculation of expected resulting BCVA. Ocular Trauma Score (OTS) – reproduced according to Kuhn et al. [15] ![Calculation of expected resulting BCVA. Ocular Trauma Score (OTS) – reproduced according to Kuhn et al. [15]](https://www.prolekare.cz/media/cache/resolve/media_object_image_small/media/image_pdf/16eba37157dac051b7779b30f60de6cf.png)
Note: BCVA = Best Corrected Visual Acuity With regard to the most common mechanism of occurrence of penetrating eye trauma, i.e. impact of metal on metal, this injury primarily affects men of productive age. All 18 patients in our cohort were men, and in 14 patients this concerned an occupational injury.
Today the standard therapeutic procedure in the case of a penetrating eye trauma with a metallic foreign body inserted in the region of the posterior segment is pars plana vitrectomy. The main argument in favour of the PPV technique is reduction of the risk of retinal detachment thanks to the removal of the damaged vitreous body. However, in young phakic patients progression of a cataract is frequently observed following PPV [2], and here there is also an increased risk of induction of an iatrogenic retinal defect or even retinal detachment, the occurrence of cystoid macular edema, or the formation of epiretinal membranes [1,18]. In the case of transscleral extraction by exo magnet or endo magnet without PPV or with minimal PPV, however, there is an increased risk of vitreoretinal traction (as a consequence of adherences between the intraocular foreign body and the retina), with the potential progression of tractional retinal detachment or iatrogenic retinal cracks with subsequent rhegmatogenous retinal detachment, the risk of progression of proliferative vitreoretinopathy or haemophthalmos [12]. Furthermore, within the space of hours a fibrin capsule forms around the intraocular foreign body, which may prevent extraction of the foreign body by exo magnet [14]. A further potential risk of this technique is the presence of a metallic but non-magnetic intraocular foreign body [15], which cannot be extracted by a magnet. By contrast, thanks to comprehensive studies mapping the safety of intravitreal applications of various pharmaceuticals [19], it is known that even repeated simple vitreoretinal intervention into the eye without PVD usually remains asymptomatic, with a low risk of iatrogenic induction of tractional retinal detachment or other serious complication.
In 8 patients in our cohort, traumatic cataract was present upon the baseline examination – 1 case required a surgical solution of the cataract concurrently with extraction of the IOFB, in 1 case progression was determined during the observation period, which required a surgical solution 14 months after the trauma (phacoemulsification and implantation of a posterior chamber IOL). In the remaining 6 eyes, thanks to the minimally invasive procedure, the cataract did not progress even during the long observation period, and the patients retained their own lens with accommodative capacity.
In all patients in the cohort, the intraocular foreign body was small (maximum 5 mm in the largest dimension), which is one of the main positive prognostic factors [14].
In the great majority of cases, we chose a minimally invasive procedure for young patients with a well transparent lens, with preserved accommodative capacity. The exception was a 70 year old man, for whom we would indicate a PPV procedure as standard. However, the patient had well transparent ocular media, so far without a detached posterior vitreous membrane and minimal damage to the posterior segment. For personal and health reasons he preferred a minimally invasive surgical procedure. During the course of the observation period (37 months) until his death, we did not observe any progression of traumatic cataract or any other intraocular complication.
Another patient for whom we chose this procedure (without PPV) outside of our defined indication criteria was a young man with very low baseline BCVA (0.008, i.e. 0.4/50) as a consequence of impact of an IOFB into the macular region. We decided in favour of a minimally invasive procedure due to the intact lens and good condition of the vitreous body, without a detached PVM. It was in this patient that a complication occurred in the form of development of a vitreomacular tractional band with the risk of progression to tractional retinal detachment, and the condition required a surgical procedure. Again, with regard to the condition of the lens and the age of the patient, we chose a minimally invasive solution, and 4 months after the trauma we performed tractotomy of the vitreomacular tractional band by vitrectom without PPV. During the subsequent observation period (139 months) no further complications were recorded.
CONCLUSION
In the era of pars plana vitrectomy, extraction of an intraocular foreign body from the region of the posterior segment of the eye without PPV is considered a controversial approach, with a range of risks. However, as demonstrated by the cohort of patients at our centre, in the case of carefully considered indication and in the hands of an experienced vitreoretinal surgeon, it is possible to perform safe extraction of an IOFB from the posterior segment of the eye transsclerally with the aid of an exo magnet or endo magnet, under visual control by contact light and with minimal PPV. This increases the patient’s chance of preserving his/her own lens with accommodative capacities of the eye, and reducing the risk of the necessity of further surgical procedures on the affected eye.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company. The authors further declare that the study has not been submitted to any other journal or printed elsewhere, with the exception of congress abstracts and recommended procedures.
Sources
1. Al-Amro, SA., Khan, NM., Kangave, D.: Visual outcome and prognostic factors after vitrectomy for posterior segment foreignbodies. Eur J Ophthalmol, 10(4); 2000 : 304-311.
2. Blodi, BA., Paluska, SA.:Cataract after vitrectomy in young patients. Ophthalmology, 104(7); 1997 : 1092-1095.
3. Cillino, S., Casuccio, A., Di Pace, F. et al.: A five – year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmology, 8(1); 2008 : 6.
4. Ehlers, JP., Kunimoto, DY., Ittoop, S. et al.: Metallic intraocular foreign bodies: characteristics, interventions, and prognostic factors for visual outcome and globe survival. Am J Ophthalmol, 146(3); 2008 : 427-433.
5. Fabian, ID., Moisseiev, E., Moisseiev, J. et al.: Macular hole after vitrectomy for primary rhegmatogenous retinal detachment. Retina, 32(3); 2012 : 511-519.
6. Guevara-Villarreal, DA., Rodriguez-Valdés, PA.:Posterior segment intraocular foreign body: extraction surgical techniques, timing, and indications for vitrectomy. J Ophthalmol, 2016; 2016 : 2034509. doi: 10.1155/2016/2034509. eCollection 2016.
7. Jonas, JB., Knorr, HLJ., Budde WM: Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology, 107(5); 2000 : 823-828.
8. Karel, I., Diblík, P.: Management of posterior segment foreign bodies and long-term results. Eur J Ophthalmol, 5(2); 1995 : 113-8.
9. Kuhn, F., Maisiak, R., Mann, L. et al.: Theocular trauma score (OTS). Ophthalmology Clinics of North America, 15(2); 2002 : 163–165.
10. Li, L., Lu, H., Ma, K. et al.: Etiologic causes and epidemiological characteristics of patients with intraocular foreign bodies: retrospective analysis of 1340 cases over ten years. J Ophthalmol, 2018; 2018 : 6309638. doi: 10.1155/2018/6309638. E Collection 2016.
11. May, DR., Kuhn, FP., Morris, RE. et al.: The epidemiology of serious eye injuries from the United States Eye Injury Registry. Graefes Arch Clin Exp Ophthalmol, 238(2); 2000 : 153-157.
12. Mester, V., Kuhn, F.: Ferrous intraocular foreign bodies retained in the posterior segment: management options and results. Int Ophthalmol, 22(6); 1998 : 355-362.
13. Modjtahedi, BS., Rong, A., Bobinski, M. et al.: Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computad tomography, ultrasound and magnetic resonance imaging. Retina, 35(1); 2015 : 95-104.
14. Nicoara, SD., Irimescu, I., Calinici, T. et al.: Intraocular foreign bodies extracted by pars plana vitrectomy: clinical characteristics, management, outcomes and prognostic factors. BMC Ophthalmol, 15; 2015 : 151. doi: 10.1186/s12886-015-0128-6. E Collection 2015.
15. Panissod, PNMR.: study and magnetic properties of vanadium based alloys with transition metals. Journal of Physics F: Metal Physics, 4(3); 1974 : 484-496.
16. Parke 3rd, DW., Flynn Jr, HW., Fisher, YL.: Management of intraocular foreign bodies: a clinical flight plan. Can J Ophthalmol, 48(1); 2013 : 8-12.
17. Parke 3rd, DW., Pathengay, A., FlynnJr, HW. et al.: Risk factors for endophthalmitis and retinal detachment with retained intraocular foreign bodies. J Ophthalmol, 2012; 2012 : 758526. doi: 10.1155/2012/758526. E Collection 2012.
18. Weissgold, DJ., Kausha, P.: Late onset of rhegmatogenous retinal detachments after successful posterior segment intraocular foreign body removal. Br J Ophthalmol, 89(3), 2005 : 327–331.
19. Wu, L., Martínez-Castellanos, MA., Quiroz-Mercado, H. et al.: Pan American Collaborative Retina Group (PACORES): Twelve-month safety of intravitreal injections of bevacizumab (Avastin): results of the Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol, 246(1); 2008 : 81-87.
20. Yeh, S., Colyer, MH., Weichel, ED.:Current trends in the management of intraocular foreign bodies. Curr Opin Ophthal, 19(3); 2008 : 225-233.
21. Zhang, Y., Zhang, MN., Jiang, CH. et al.: Intraocular foreign bodies in China: clinical characteristics, prognostic factors, and visual outcomes in 1421 eyes. Am J Ophthalmol, 152(1); 2011 : 66-3.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2020 Issue 1-
All articles in this issue
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Current use of the automatic retinal oximetry. Review
- Importance of PET/CT examination in patients with malignant uveal melanoma
- Enucleation after Stereotactic Radiosurgery in Patients with Uveal Melanoma
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Importance of PET/CT examination in patients with malignant uveal melanoma
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

