-
Medical journals
- Career
Late postoperative capsular bag distension syndrome
Authors: M. Otrošinová; J. Novák
Authors‘ workplace: Nemocnice Pardubického kraje a. s., Pardubická nemocnice, Oční oddělení primář doc. MUDr. Jan Novák, CSc., FEBO
Published in: Čes. a slov. Oftal., 75, 2019, No. 1, p. 46-50
Category: Case Report
doi: https://doi.org/10.31348/2019/1/6Overview
Purpose: Capsular bag distension syndrome is to be seen as a relatively rare complication after cataract surgery.
Materials and Methods: We describe our experience of late-onset capsular bag distension syndrome with one case onset 4 years after cataract surgery. Nowadays diagnostic imaging methods were used. The literature was reviewed to summarize the diagnosis, classification, use of diagnostic aids, and the current treatments for the capsular bag distension syndrome. Visual acuity was assessed using the ETDRS (Early Treatment Diabetic Retinopathy Study) chart.
Discussion: A 72-year-old woman presented with decreased visual acuity and blurred vision 4 years after phacoemulsification with continuous curvilinear capsulorhexis (CCC) and in-the-bag IOL implantation. After the slit lamp examination, patient was investigated with Scheimpflug camera (OCULUS Pentacam HR) and anterior segment spectral domain OCT (Optovue, Avanti RTVue XR), which confirmed the diagnosis of capsular block syndrome. Aspiration of the turbid fluid behind the lens and capsular bag lavage resulted in resolution of her symptoms. Aspirated fluid was examined. We have observed no CBS recurrence.
Conclusion: CBS is the relatively rare complication of the standard cataract surgery, which can occur during surgery and in a postoperative period. CBS can be solved successfully after regular diagnosis using modern imaging methods.
Keywords:
capsular bag distension syndrome – capsular block syndrome OCT – CBS – Pentacam
INTRODUCTION
Capsular bag distension syndrome (CBDS), also known as capsular block syndrome, is described in the literature as a rare complication of cataract surgery. It occurs upon the use of the technique of continual curvilinear capsulorhexis with implantation of a posterior chamber artificial intraocular lens.
Circular adhesion occurs between the edge of the curvilinear capsulorhexis and the anterior surface of the artificial intraocular lens or nucleus.
CASE REPORT
In March 2016, a 72-year-old woman was examined at our centre, who was complaining of a deterioration of visual acuity and blurred vision in the right eye. Upon arrival best corrected visual acuity (BCVA) was 0.32. A dramatic deterioration had occurred above all during the course of the last month. The patient had not observed any complaints with vision in her left eye, in which she had also undergone surgery.
In her anamnesis the patient had undergone cataract surgery at a private centre in February 2012, with implantation of a posterior chamber artificial intraocular lens into the capsule, and in December 2012 she had undergone a trabeculectomy at our centre, with functional filtration bleb, both procedures in the right eye. After surgery the patient had not experienced any complaints, in the available records postoperative uncorrected visual acuity (UCVA) was 1.00. The patient was treated internally only for arterial hypertension.
On a slit lamp there was a finding of a pacific anterior segment, fibrotically altered edge of anterior curvilinear capsulorhexis and circular adherence between the edge of the capsulorhexis and the anterior surface of the IOL. The edge of the anterior curvilinear capsulorhexis was smaller than the optical part of the implanted lens, and circularly covered its edges. The lens was centred in the capsule without shifting on a front-to-back axis. Behind the IOL it was possible to document a distended posterior capsule, and the space between the posterior surface of the IOL and posterior capsule was homogeneously filled with a milky white turbid fluid (Fig. 1). We did not observe any abnormalities of the cornea, iris-corneal angle, depth of the anterior chamber or content thereof. Intraocular pressure was 15 mmHg.
1. Anterior segment without signs of inflammation, distended space between the posterior surface of IOL and posterior capsule filled with milky white turbid fluid. Fibrotically altered anterior capsule closely adhering to the anterior surface of IOL. 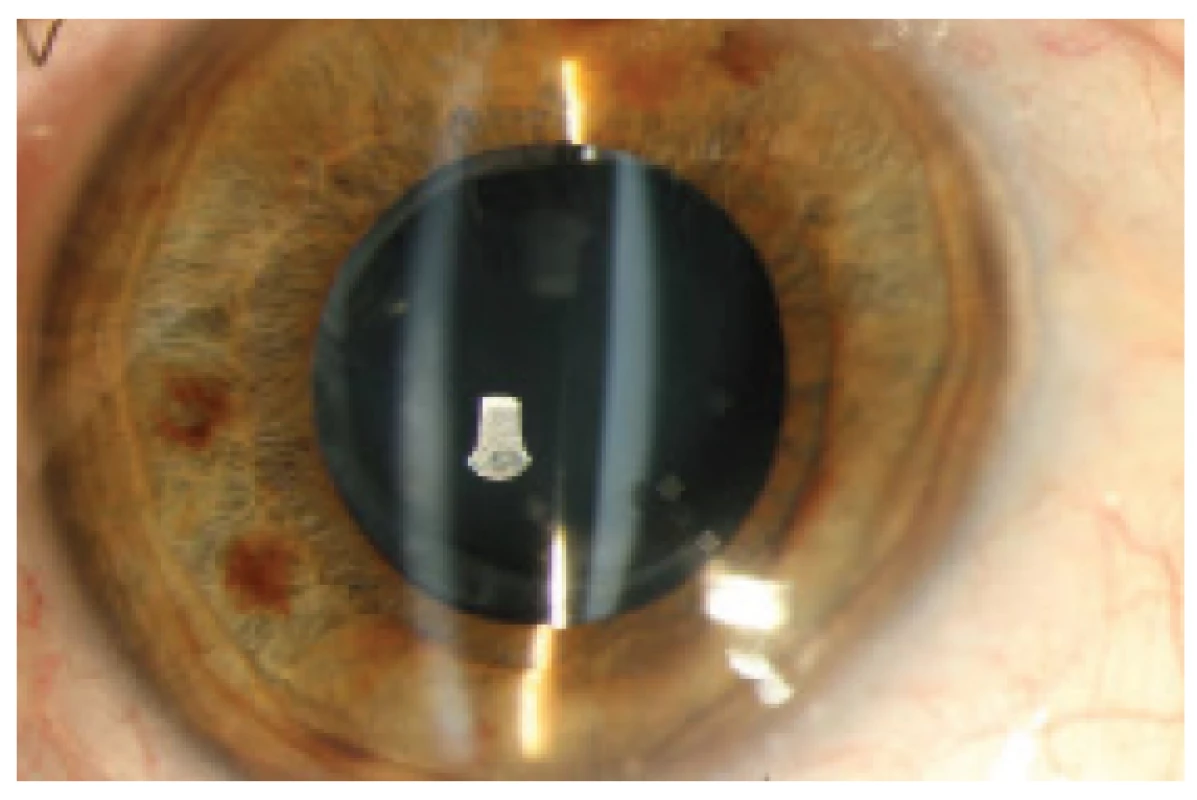
The quality of the examination of the vitreous body and retina was not optimal due to the blurred image. Nevertheless, no signs of inflammation or vitreoretinal pathology were determined.
On the basis of the examination we determined a suspected diagnosis of late postoperative posterior capsular bag distension syndrome. In order to confirm the set diagnosis we chose further examination methods – anterior segment OCT (Optovue, Avanti RTVue XR) without mydriasis (Fig. 2) and Scheimpflug camera (OCULUS Pentacam HR) in maximum mydriasis (Fig. 3).
2. Anterior-segment OCT demonstrates capsular distension, before lavage the posterior capsule is distended backwards and filled with milky white fluid (hyperreflective mass behind IOL). Well centred lens without front-to- -back shifting. 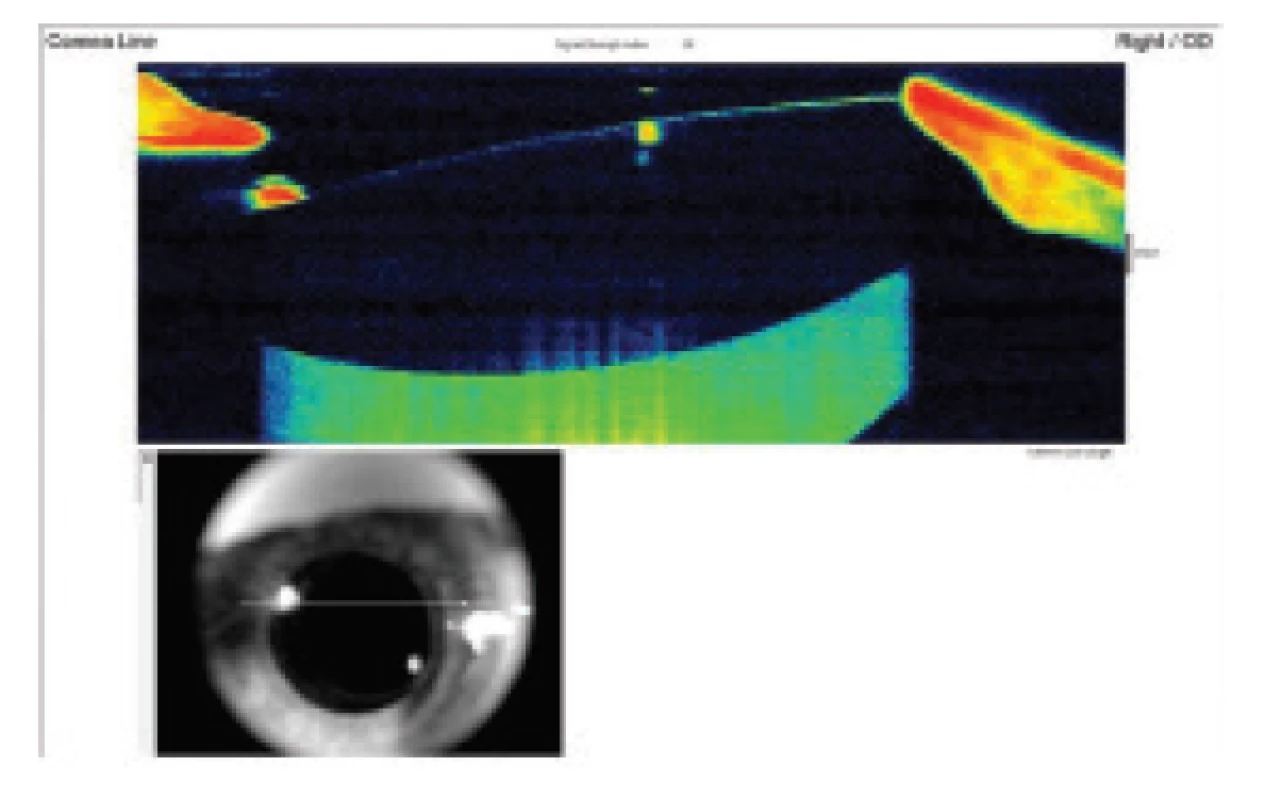
3. Scheimpflug photograph documents backwards distended posterior capsule filled with opalesque fluid. It also documents relatively high density of fluid in the capsule (20%). 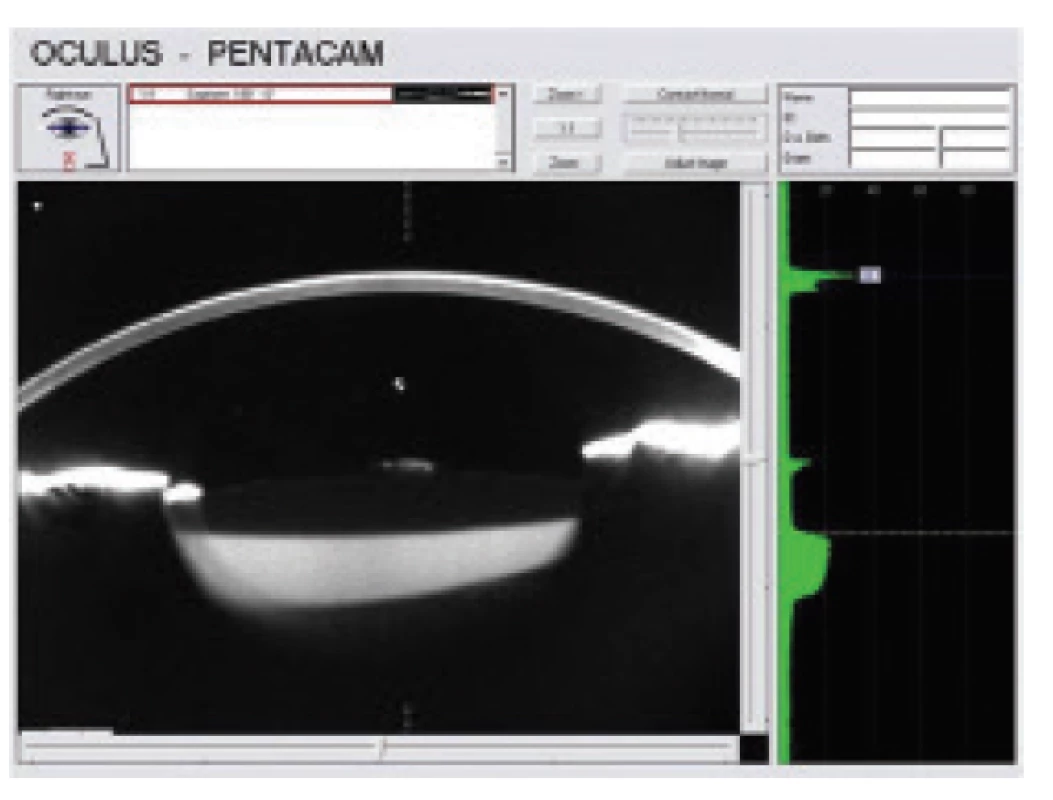
Taking into account the possibility of infection and in an endeavour to prevent the potential penetration of microflora into the vitreous area, instead of laser capsulotomy we selected a surgical procedure. Under a microscope, three incisions of the anterior fibrotic capsule were made from three paracenteses. There followed diagnostic aspiration of the milky white turbid fluid with the aid of a 26G needle inserted by paracentesis into the capsule behind the IOL. We then performed lavage by irrigation and aspiration, and application of cefuroxime (Axetine) solution into the capsule. We did not observe any perioperative complications. Postoperatively corticosteroids and antibiotics were applied locally for a period of one week. The fluid was sent for cultivation and microscopic examination. Microscopy confirmed the presence of G+ rods of coryneform shape, attesting to the Propionibacterium genus. However, the cultivation examination was negative. After the procedure the patient was monitored for a period of 6 months. During this period she was without complaints or signs of recurrence of posterior capsular bag distension, and her visual acuity reached BCVA = 0.80 (Fig. 4, 5, 6).
4. Anterior segment after lavage without capsular distension, frilled posterior capsule 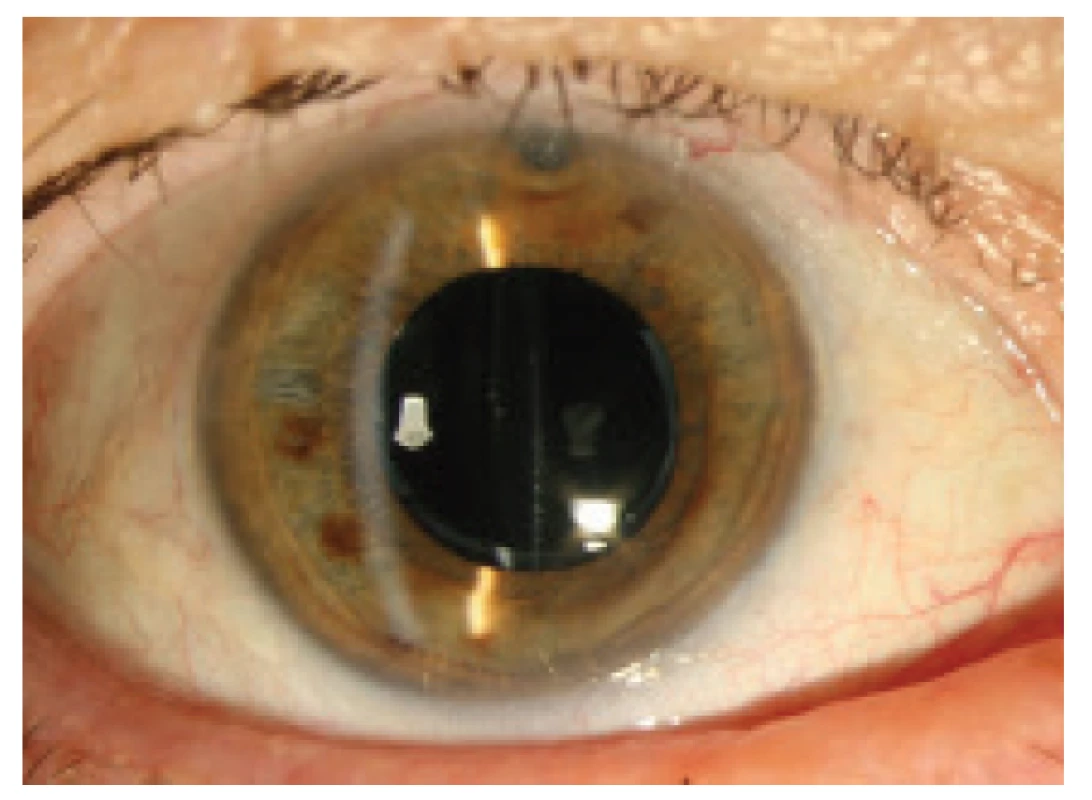
5. Anterior-segment OCT after lavage displays space behind IOL collapsed and bordered with frilled posterior capsule 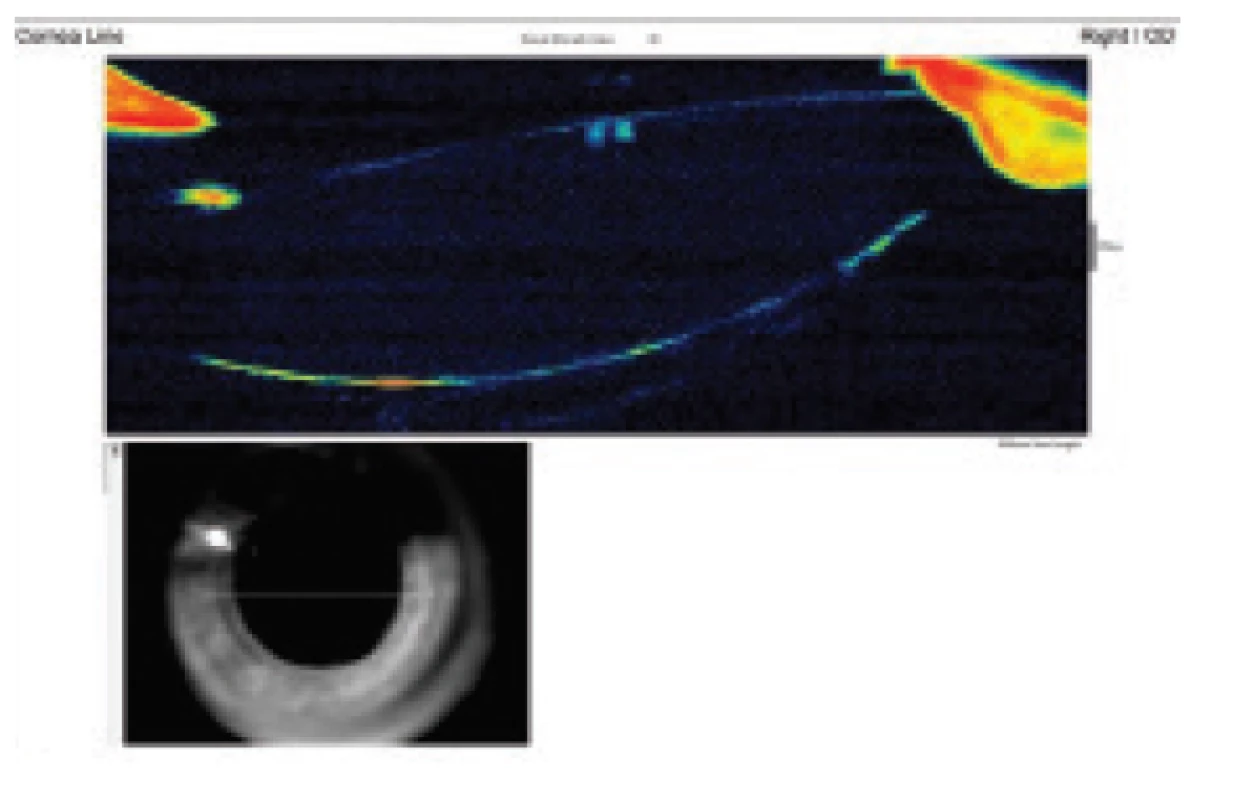
6. Scheimpflug photograph after lavage documents frilled posterior capsule, space behind IOL now without opalesque liquid and posterior capsule adheres to posterior surface of IOL. Anterior hyaloid membrane is displayed behind capsule. 
DISCUSSION
Capsular bag distension syndrome is relatively rarely described and in the past an infrequently identified complication of cataract surgery using the technique of anterior continual curvilinear capsulorhexis with phacoemulsification and implantation of an artificial intraocular posterior capsule lens, which may occur during the operation or in the postoperative period. It is characterised by an accumulation of fluid inside the capsular bag, especially between the posterior capsule and the posterior surface of the IOL (or nucleus of the lens during surgery).
Capsular bag distension syndrome was first described by Davison in 1990 [3] and Holtz in 1992 [7], but it was Masket [15] in 1993 who was the first to use the term “capsular block syndrome” in order to refer to this complication.
In 1998, Miyake et al. compiled the first classification which differentiates capsular bag distension syndrome into three groups on the basis of the time of its origin in connection with surgery: perioperative, early postoperative and late postoperative [16]. The second classification was compiled by Kim and Shin in 2008 [9] with reference to the pathogenesis of the origin, which differentiates postoperative capsular bag distension syndrome into three groups: acellular, inflammatory and fibrotic types.
1. Perioperative type originates upon rapid hydro-dissection, upon the use of high irrigation pressure or the use of a large quantity of irrigation fluid. This leads to a dislocation of the nucleus of the lens in a forward direction and a blockade of the opening of the anterior curvilinear capsulorhexis. It may cause a rupture of the posterior case with luxation of the nucleus into the vitreous area [16].
It occurs more frequently in the case of posterior polar and hyper-mature cataract, and in individuals with an axial length of the eyeball greater than 25 mm [6, 22].
2. Early postoperative type originates most often on the first day after surgery, but may develop during the course of the first two postoperative weeks. [1, 4, 15, 18, 22, 25, 26]. In this type, drainage of fluid from the posterior chamber is prevented by a forward dislocated artificial intraocular lens adhering to the anterior capsule [12].
Miyake et al. [16] were of the opinion that the accumulated fluid behind the IOL is viscoelastic material, which was confirmed by Sugiura et al. [25], who analysed the aspirated fluid with the aid of highly effective liquid chromatography. The result demonstrated that the transparent liquid in the lens sac was diluted sodium hyaluronate. Hyaluronate is a viscoelastic material with a high molecular weight, and so left in the capsule it increases the osmotic gradient and sucks fluid inside via the capsule, which in this situation acts like a semi-permeable membrane [7]. This type of posterior capsular bag distension was classified as the acellular type by the classification according to Kim and Shin [9].
Another possible mechanism is also considered, namely the development of an osmotic gradient manifested by suction of the chamber water into the capsule to retained residues of cortical matter or fragments of the nucleus [9, 16, 25, 26]. With regard to this mechanism, this type of CBDS has been classified as inflammatory postoperative capsular bag distension syndrome according to Kim and Shin [9], who assumed that this originates also as a consequence of an exudative process of epithelial cells of the lens [9].
An accumulation of fluid shifts the IOL forward to the edge of the anterior curvilinear capsulorhexis, thereby causing a blockade leading to a shallowing of the anterior chamber and alteration of the iris-corneal angle. If this process continues, it may lead to an elevation of intraocular tension and acute closed-angle glaucoma [26]. The forward-shifted lens causes a change of position of the focal point, thereby inducing myopia [9, 26]. For this reason, every case of suspected myopic error in the early postoperative period should be examined in artificial mydriasis in order to exclude the possibility of CBDS [13].
In some cases of early postoperative syndrome, spontaneous absorption may occur [23]. However, the majority of cases require a solution in the sense of anterior or posterior Nd:YAG laser capsulotomy [15].
CBDS has been described following implantation of various types of intraocular lenses [3, 4, 9, 13, 14, 16] of various materials and shapes [3, 4, 7, 12, 15, 16, 19, 20, 24, 25, 28].
3. Late postoperative capsular bag distension syndrome is also known as postoperative liquefaction. It concerns a chronic process occurring secondarily upon fibrous changes and generation of adhesions between the anterior capsule and anterior surface of the optics of an artificial intraocular lens. It originates on average 3.8 years after surgery and is characterised by an accumulation of white material behind the lens, inside the capsule [17].
Eifrig studied the accumulated fluid in the capsule and confirmed a high concentration of alpha-crystallin and relatively low concentration of albumins, which indicates that the accumulated fluid may originate from residual lens epithelial cells (LECs) [5]. Under the influence of various mediators, the cells proliferate, succumb to metaplasia and produce various types of extracellular matrix and collagens, which accumulate in the capsule [27]. This creates an osmotic gradient via the semi-permeable membrane of the capsule, with passage of the chamber fluid into the capsule [9, 16, 17]. A second possible mechanism is that residual cells succumb to apoptosis and necrosis, with the generation of a mixture of proteins and other osmotically active substances [19].
According to the classification compiled by Kim and Shin [9], this type is known as fibrotic postoperative type of CBDS.
The importance of complete cleansing and removal of LECs upon cataract surgery, i.e. polishing of the lens, is emphasised here.
Nevertheless, in this type of CBDS, more serious complications such as protrusion of the IOL, shallowing of the anterior chamber and elevation of intraocular pressure do not occur [5]. This is thanks to the fibrotic ring which forms on the edge of the original capsulorhexis and prevent the protrusion of the artificial intraocular lens, also through the influence of contraction of the capsule as a whole with subsequent tightening of the zonules [19].
Deterioration of visual acuity is caused by a dispersion of light in the opalesque fluid behind the IOL, resembling a piggy-bag effect [2].
In some cases of late postoperative type, microbial analysis of the turbid fluid accumulated behind the IOL has revealed the presence of the bacteria Proprionibacterium acnes [2, 8, 10]. Infection of the content of the capsule is possible upon the primary operation or re-operation. It is practically impossible to determine the precise time of penetration of infection into the capsule in our case report. Anaerobic bacteria may survive for a long time and reproduce only under suitable conditions of hypoxia, i.e. congestion of fluid in the capsule. As a result, in the etiology of the origin of this type, the possibility of infectious components is also considered. With regard to this fact, the choice of Nd:YAG laser posterior capsulotomy in the solution of late postoperative distension of the posterior capsule involves a risk of spreading the potential infection to the vitreous area, and may lead to the onset of endophthalmitis. Aspiration of the fluid from the capsule supplemented by lavage is a technically simple, safe and effective method, in which the posterior capsule remains intact and all the turbid fluid can be drained. Additionally, this procedure enables us to conduct a bacteriological examination and an examination of the composition of the fluid. Naturally, determining the precise cause of occurrence of CBDS will also be a very important factor with regard to deciding on the timing and type of treatment and the prevention of its occurrence.
Although the average time of manifestation of late postoperative type is 3.8 years [16, 17], cases have been published in which patients began to manifest symptoms 10 years after cataract surgery.
It is speculated that late CBDS is subclinical in the early stages and is detected only later, when opacification of the posterior capsule takes place, with a subsequent deterioration of visual acuity [26], despite the fact that according to some authors the deterioration of visual acuity is connected exclusively with the accumulation of fluid. This takes place only in the case of an accumulation of a sufficiently large quantity of fluid, which must be turbid [17]. The presence of milky white fluid in the capsule is typical of the late type of postoperative CBDS.
There is a range of symptoms which may contribute to the correct diagnosis of CBDS. A physical examination on a slit lamp alone is often sufficient in order to determine the diagnosis. Modern methods such as a Scheimpflug camera, UBM or AS-SD OCT are able to determine the diagnosis absolutely unequivocally. The potential presence of CBDS with the use of the aforementioned methods should be considered also in all cases of unexpected postoperative myopia, especially when it is accompanied by a finding of a shallow anterior chamber and distended posterior capsule with protrusion of the IOL.
CONCLUSION
CBDS should be included in differential diagnostics for every patient with changes of vision following cataract surgery, independently of the length of time since the operation [8]. Definitive diagnosis and better display of the anatomical structures can be achieved with the aid of diagnostic examination methods such as Scheimpflug photography, anterior segment UBM and anterior segment OCT. In cases where the posterior capsule is extremely distended, AS-SD OCT or ultrasonic biomicroscopy is a better display method than Scheimpflug photography, which requires extreme mydriasis [11].
However, substantially extended Scheimpflug photography (Pentacam and other instruments) has an important role in documenting the finding and regression after treatment. On the other hand, anterior segment OCT provides the same information even without mydriasis. The doctor must ultimately take into account the diagnostic options and select the optimal display type and subsequent treatment. After the procedure it is necessary to ensure regular monitoring and evaluation of the therapeutic effect.
In the literature CBDS is referred to as a rare complication. The early type is stated as the more common form. We are of the opinion that late postoperative capsular bag distension syndrome is far more common than described, and that a better awareness of this diagnosis will reveal further cases.
Information about the mechanisms sharing in the occurrence of CBDS and an awareness of its manifestations may contribute to the earlier detection of this treatable condition, and to the prevention of adverse consequences of incorrect diagnosis and treatment.
This study was presented in the form of oral communication at the annual congress of the Slovak Ophthalmological Society in Bratislava on 29 September 2016.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received by the Editorial Department on: 12 November 2018
Accepted for printing on: 28 January 2019
Marianna Otrošinová, MUDr.
Štrossova 1338
53003 Pardubice
Email: ivancova.marianna@gmail.com
Sources
1. Basti, S., Nayak, H., Mathur, U.: Capsular bag distension after optic capture of a sulcus-fixated intraocular lens. J Cataract Refract Surg, 25; 1999 : 293–295.
2. Bhattacharjee, H., Bhattacharjee, K., Bhattacharjee, P.: Liquefied after cataract and its surgical treatment. Indian J Ophthalmol, 62; 2014 : 580–584.
3. Davison, JA.: Capsular bag distension after endophacoemulsification and posterior chamber intraocular lens implantation. J Cataract Refract Surgb, 16; 1990 : 99–108.
4. Durack, I., Ozbeck, Z., Ferliel, ST. et al.: Early postoperative capsular block syndrome. J Cataract Refract Surg, 27; 2001 : 555–559.
5. Eifrig, DE.: Capsulorhexis-related lacteocrumenasia. J Cataract Refract Surg, 23; 1997 : 450–454.
6. Hashimoto, T., Izutani, M., Tanaka, Y. et al.: Two cases of posterior capsular rupture and dislocation of lens nucleus following hydrodissection. Folia Ophthalmol Jpn, 45; 1994 : 973–976.
7. Holtz, SJ.: Postoperative capsular bag distension. J Cataract Refract Surg, 18; 1992 : 310–317.
8. Killoran, E., Haugsdal, J., Oetting, TA.: Capsular block syndrome: An unusual presentation. EyeRounds.org [online]. 2016 [cit. 2018-11-03]. Dostupné na WWW: <https://webeye.ophth.uiowa.edu/eyeforum/cases/238-capsular-block-syndrome.htm>.
9. Kim, HK., Shin, JP.: Capsular block syndrome after cataract surgery: clinical analysis and classification. J Cataract Refract Surg, 34; 2008 : 357–363.
10. Kollias, AN., Vogel, MA., de Kaspar, HM. et al.: Grueterich M Proprionibacterium acnes in capsular bag distension syndrome. J Cataract Refract Surg, 36; 2010 : 167–169.
11. Kucukevcilioglu, M., Hurmeric, V., Erdurman, FC. et al.: Imaging late capsular block syndrome: ultrasound biomicroscopy versus Scheimpflug camera. J Cataract Refract Surg, 37; 2011 : 2071–2074.
12. Liu, TY., Chou, PI.: Capsular block syndrome associated with secondary angle-closure glaucoma. J Cataract Refract Surg, 27; 2001 : 1503–1505.
13. Marback, EF., Araújo, RCA., Freitas, MS.: Síndrome do bloqueio capsular precoce relato de caso e especulação sobre o tamanho da parte óptica da lente como fator de risco. Rev Bras Oftalmol, 68; 2009 : 344–347.
14. Mardelli, PG., Mehanna, CJ.: Phacoanaphylactic endophthalmitis secondary to capsular block syndrome. J Catarct Refract Surg, 33; 2007 : 921–922.
15. Masket, S.: Postoperative complications of capsulorhexis. J Cataract Refract Surg, 19; 1993 : 721–724.
16. Miyake, K., Otta, I., Ichihashi, S. et al.: New classification of capsular block syndrome. J Cataract Refract Surg, 24; 1998 : 1230–1234.
17. Miyake, K., Ota, I., Miyake, S. et al.: Liquefied after cataract: a complication of continuous curvilinear capsulorhexis and intraocular lens implantation in the lens Capsule. Am J Ophthalmol, 125; 1998 : 429–435.
18. Miyake, K., Ota, I., Miyake, S. et al.: Capsular block syndrome with external blockage of the capsular opening by a ciliary sulcus fixated posterior chamber lens. Am J Ophthalmol, 127; 1999 : 605–607
19. Nishi, O., Nishi, K., Takahashi, E.: Capsular bag distension syndrome noted 5 years after intraocular lens implantation. Am J Ophthalmol, 125; 1998 : 545–547.
20. Omar, O., Eng, CT., Chang, A. et al.: Capsular bag distension with an acrylic intraocular lens. J Cataract Refract Surg, 22; 1996 : 1365–1367.
21. Osher, RH., Yu, BCY., Koch, DO.: Posterior polar cataracts: a predisposition to intraoperative posterior capsular rupture. J cataract Refract Surg, 16; 1990 : 157–162.
22. Ota, I., Miyake, S., Miyake, K.: Dislocation of the lens nucleus into the vitreous cavity after standard hydrodissection. Am J Ophthalmol, 121; 1996 : 706–708.
23. Qu, J., Bao, Y., Li, M. et al.: Surgical management of late capsular block syndrome. J Cataract Refract Surg, 36; 2010 : 1687–1691.
24. Starr, MB.: Capsular bag distension syndrome noted 5 years after intraocular lens implantation. Am J Ophthalmol, 127; 1999 : 244–245.
25. Sugiura, T., Miyauchi, S., Eguchi, S. et al.: Analysis of liquid accumulated in the distended capsular bag in early postoperative capsular block syndrome. J Cataract Refract Surg, 26; 2000 : 420–425.
26. Theng, JT., Jap, A., Chee, SP.: Capsular block syndrome: a case series. J Cataract Refract Surg, 26; 2000 : 462–467.
27. Wendrix, G., Zeyen, T.: Late-onset capsular bag distension syndrome after cataract surgery: 2 case-reports. Bull Soc Belge Ophthhalmol, 301; 2006 : 67–69.
28. Yeoh, R., Theng, J.: Capsular block syndrome and pseudoexpulsive hemorrhage. J Cataract Refract Surg, 26; 2000 : 1082–1084.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 1-
All articles in this issue
- Usage of shear wave elastography for diagnosis of changes of oculomotor muscles in endocrine orbitopathy
- Treatment of idiopathic choroidal neovascular membrane with ranibizumab - our experience
- RADIATION MACULOPATHY AFTER ONE-DAY SESSION STEREOTACTIC RADIOSURGERY IN PATIENTS WITH CILIARY BODY AND CHOROIDAL MELANOMA
- Effective Tissue Layer Separation of Donor Cornea for DMEK by Fluid Injection Between Descemet
- Primary orbital teratoma – case study
- Late postoperative capsular bag distension syndrome
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Late postoperative capsular bag distension syndrome
- Primary orbital teratoma – case study
- Treatment of idiopathic choroidal neovascular membrane with ranibizumab - our experience
- RADIATION MACULOPATHY AFTER ONE-DAY SESSION STEREOTACTIC RADIOSURGERY IN PATIENTS WITH CILIARY BODY AND CHOROIDAL MELANOMA
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

