-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
An Autopsy case of Poisoning with Selective Serotonin Reuptake Inhibitor, Paroxetine
Pitevní nález otravy selektivním inhibitorem zpětného vychytávání serotoninu (paroxetin)
Dvacetiletá žena byla nalezena mrtvá ve svém pokoji. Byla medikamentózně léčena pro depresivní a panické poruchy, a opakovaně se pokoušela o suicidium. V blízkosti těla bylo nalezeno mnoho balení předepsaných léčiv, včetně paroxetinu. Při pitvě byly plíce edematózní. Orgány vykazovaly známky mírné kongesce a změny způsobené rozkladem. Autolýzou způsobená ruptura, označená jako gastromalacie, byla popsána na přední části stěny žaludku v oblasti kardie. Toxikologické vyšetření stanovilo 0,78, 3,20 a 17,63 μg/ml paroxetinu v kardiální, respektive femorální krvi a v moči. Acetaminophen a phenobarbital byly také stanoveny, a to v terapeutické či subletální koncentraci. Autoři vyhodnotili údaje získané post mortem, při čemž vzali v úvahu posmrtnou difuzi léků a došli k závěru, že smrt byla způsobena toxicitou paroxetinu spolu se serotoninovým syndromem.
Klíčová slova:
paroxetin – otrava – difuze post mortem
Authors: Motonori Takahashi 1; Hiroshi Kinoshita 2; Azumi Kuse 3; Mai Morichika 3; Minori Nishiguchi 1; Harumi Ouchi 1; Takako Minami 1; Kiyoshi Matsui 1; Takehiko Yamamura 1; Hiroyuki Motomura 4; Nao Ohtsu 1; Shie Yoshida 1; Nobuyuki Adachi 1; Yasuhiro Ueno 3; Shigeru Hishida 1; Hajime Nishio 1
Authors place of work: Department of Legal Medicine, Hyogo College of Medicine, 1-1 Mukogawa-cho, Nishinomiya, Hyogo, 663-8501, Japan 1; Department of Forensic Medicine, Faculty of Medicine, Kagawa University, 1750-1 Miki, Kagawa, 761-0793, Japan 2; Division of Legal Medicine, Department of Environmental Health and Safety, Kobe University Graduate School of Medicine, 7-5-1, Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan 3; Forensic Science Laboratory, Hyogo Prefectural Police Headquarters, 5-4-1, Shimoyamate-dori, Chuo-ku, Kobe, 650-8510, Japan 4
Published in the journal: Soud Lék., 55, 2010, No. 1, p. 2-4
Summary
A female in her twenties was found dead in her room. She had received medications for depression and panic disorder, and had attempted suicide several times. Many packets of prescribed drugs, including paroxetine, were found near the corpse. At autopsy, the lungs were edematous. The organs were slightly congested with putrefactive change. Autolytic rupture, considered as gastromalasia, was observed in the anterior cardiac portion of stomach wall. Toxicological examination revealed 0.78, 3.20 and 17.63 μg/ml of paroxetine in the heart blood, femoral blood and urine, respectively. Acetaminophen and phenobarbital were also identified within therapeutic or sub-lethal levels. Taking into consideration postmortem diffusion of drugs, we evaluated postmortem data and concluded that the death was mainly due to toxicity of paroxetine with serotonin syndrome.
Key words:
Paroxetine – Poisoning – Postmortem diffusionIntroduction
Mood disorders (e.g. major depressive disorder and panic disorder) are thought to be associated with heterogeneous dysfunction of biogenic amines. It is suggested that depression results from a functional deficit of either serotonin or norepinephrine at the receptor site in the central nervous system [4, 10]. Tricyclic antidepressants (TCAs) have classically been prescribed for these disorders. Unfortunately, these have poor selectivity for monoamine transporter inhibition, undesirable side effects and significant toxicity [5].
In recent years, selective serotonin reuptake inhibitors (SSRIs) have been widely prescribed as first-line agents instead of TCAs [10]. Paroxetine, (-)-(3S, 4R)-4-(4-fluorophenyl)-3-[(3, 4-methylenedioxy) phenoxymethyl] piperidine, is one of the SSRIs used as an antidepressant. It has very mild anti-cholinergic effects, no activity on histamine or @1-adrenergic receptors, and its main metabolites have no pharmacological properties [13]. For these reasons, poisoning with paroxetine is rarely reported compared with other psychiatric drugs [5, 14].
Here, we report a case of poisoning with paroxetine probably accompanied by serotonin syndrome.
Case history
A female in her twenties (153 cm, 47 kg) was found dead in her room with many empty packets of prescribed drugs. Her body was discovered in a prone position. She had been suffering from depression and panic disorder, and was prescribed multiple medications including 30 mg daily of paroxetine. She had a history of several suicide attempts and self-injury. Three days before her corpse was found, she was hospitalized for overdose with acetaminophen-containing drugs and discharged on the next morning.
At autopsy, hesitation mark scarring on her left wrist was the only external injury observed. Putrefactive discoloration of skin was also noted. Both lungs (left 290 g, right 355 g) were edematous and 300 ml of pleural effusion was observed in the thoracic cavities. The brain had no macroscopic abnormality. The heart (220 g) had no lesions such as atherosclerosis, myocardial fibrosis or anatomical abnormalities. It contained 150 ml of blood with chicken fat clots. Both the anterior cardiac portion of stomach and lower portion of esophagus were autolytic, considered as gastromalacia [7], and approximately 80 ml of dark brownish peritoneal fluid was present. The bladder contained approximately 150 ml of slightly yellow clear urine. Organs showed putrefactive changes and were slightly congested. The postmortem interval was speculated to be approximately two days.
Drug screening using Triage® (Biosite Diagnostic Inc, San Diego, USA) was positive for barbiturates. In microscopic examination, all tissues showed postmortem changes. Lungs were edematous and liver showed centrilobular eosinophilic change.
Toxicological examination
Subsequent toxicological examination was performed using a high performance liquid chromatography drug analysis system (Class-VP system, Shimadzu, Kyoto, Japan), operated in accordance with the manufacturer’s specifications [6]. Toxicological analysis identified paroxetine, acetaminophen and phenobarbital in blood and other specimens (Table 1). In addition to these drugs, peritoneal fluid contained chlorpromazine, promethazine and nitrazepam.
Tab. 1. Drug concentrations in each sample (μg/ml) and their fatal and therapeutic levels 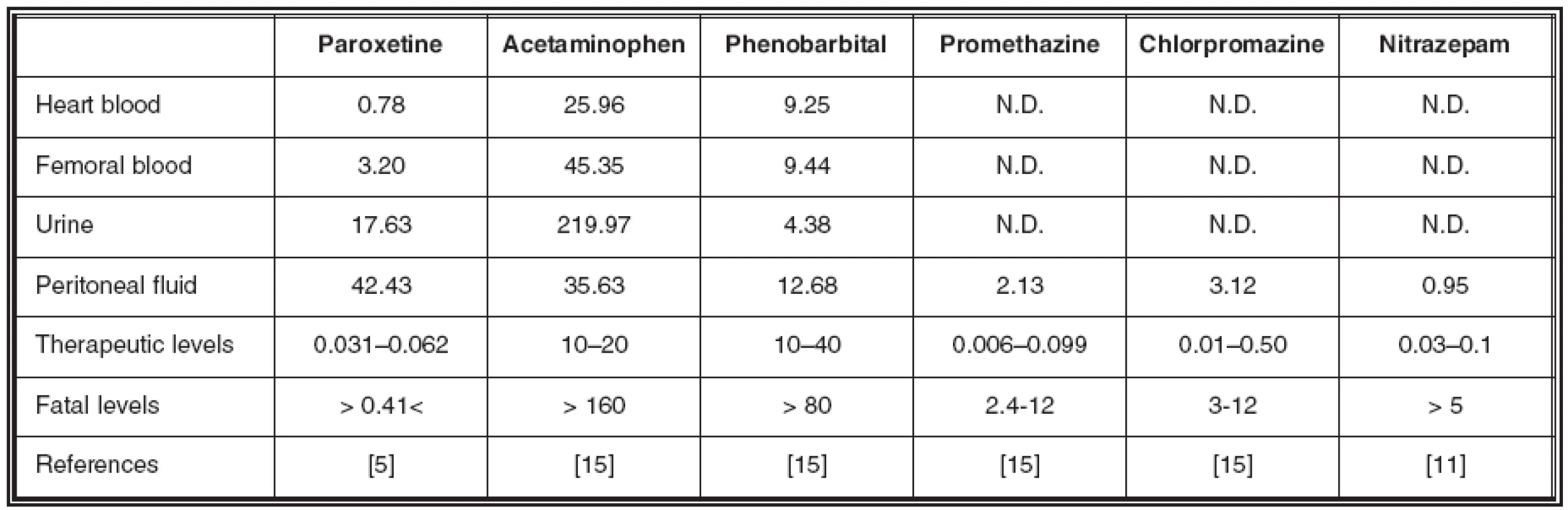
7-aminonitrazepam, a metabolite of nitrazepam, was not detected from each specimen. N.D.: Not detected. No ethanol was detected from blood or urine using headspace gas chromatography.
Discussion
The incidence of adverse effects associated with SSRIs is reported to be small compared with conventional TCAs. The lowest concentration at which death was attributed to paroxetine alone was reported to be 0.41 μg/ml [5]. In this case, the concentrations of paroxetine in the heart and femoral blood exceeded fatal levels (Table 1). While, blood concentrations of phenobarbital and acetaminophen were within therapeutic or sub-lethal levels [15]. The femoral/heart blood concentration ratio of paroxetine, acetaminophen and phenobarbital were 4.10, 1.75 and 1.02, respectively. These elevated concentrations in femoral blood may be due to postmortem diffusion from urine or peritoneal fluid. Relatively high concentrations of urinary paroxetine and acetaminophen in the bladder could accelerate drug diffusion into the femoral vein [8].
Paroxetine is a substrate for and a potent inhibitor of cytochrome P450 (CYP) 2D6, and a weak inhibitor of CYP3A4 [5, 10, 13]. This inhibition can suppress the metabolism of paroxetine itself and other drugs. In the present case, microscopic analysis of the liver showed centrilobular eosinophilic changes suggesting paroxetine metabolism was reduced by hepatocytic damages. These mechanisms may extend the biological half-life and lead to elevation of paroxetine blood concentration to lethal levels.
SSRIs increase serotonin concentration in the synaptic cleft by inhibiting presynaptic serotonin reuptake [10]. This serotonin overstimulation produces a constellation of symptoms called serotonin syndrome [1, 5, 10, 13]. It results from not only the combined use of SSRIs and monoamine oxidase inhibitors but also from SSRI monotherapy [2, 9]. The syndrome is characterized by a “clinical” triad of mental-state changes, autonomic hyperactivities (e.g. hyperthermia) and neuromuscular abnormalities [3, 12]. As the rectal temperature of the corpse decreased to environmental temperature and antemortem symptoms were unclear in present case, serotonin syndrome could not be diagnosed. However, it is strongly speculated that the deceased suffered from serotonin syndrome due to an excessive intake of paroxetine.
From the autopsy findings and the results of toxicological examination, we concluded that death was mainly due to paroxetine toxicity, with possible partial contribution from acetaminophen and phenobarbital. We took into consideration the postmortem diffusion of drugs when evaluating the postmortem data.
A part of this paper was presented at the 55th Kinki District Conference of the Japanese Society of Legal Medicine.
Address for correspondence:
Motonori Takahashi, M.D., Ph.D.
Department of Legal Medicine, Hyogo College of Medicine,
1-1 Mukogawa-cho, Nishinomiya, Hyogo, 663-8501, Japan
TEL: +81-798-45-6578
FAX: +81-798-49-3279
e-mail: gengring@hyo-med.ac.jp
Zdroje
1. Boyer EW, Shannon M.: The serotonin syndrome. N Engl J Med 2005; 352 : 1112–1120.
2. Canan F, Korkmaz U, Kocer E, Onder E, Yildirim S, Ataoglu A.: Serotonin syndrome with paroxetine overdose: a case report. Prim Care Companion J Clin Psychiatry 2008; 10 : 165–167.
3. Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM.: The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM 2003; 96 : 635–642.
4. Ellenhorn MJ, Barceloux DG.: Cyclic antidepressants. In: Medical Toxicology, Diagnosis and treatment of human poisoning. New York, NY: Elsevier, 1988, pp. 402–415.
5. Goeringer KE, Raymon L, Christian GD, Logan BK.: Postmortem forensic toxicology of selective serotonin reuptake inhibitors: a review of pharmacology and report of 168 cases. J Forensic Sci 2000; 45 : 633–648.
6. Kinoshita H, Taniguchi T, Kubota A, Nishiguchi M, Ouchi H, Minami T, Utsumi T, Motomura H, Nagasaki Y, Ameno K, Hishida S.: An autopsy case of imipramine poisoning. Am J Forensic Med Pathol 2005; 26 : 271–274.
7. Knight B.: Forensic Pathology, (2nd ed). London: Arnold, 1996, pp. 37.
8. Moriya F, Hashimoto Y.: Postmortem diffusion of drugs from the bladder into femoral venous blood. Forensic Sci Int 2001; 123 : 248–253.
9. Paruchuri P, Godkar D, Anandacoomarswamy D, Sheth K, Niranjan S.: Rare case of serotonin syndrome with therapeutic doses of paroxetine. Am J Ther 2006; 13 : 550–552.
10. Sadock BJ, Sadock VA.: Biological Therapies. In: Kaplan & Sadock’s synopsis of psychiatry, (9th ed). Philadelphia, PA: Lippincott Williams & Wilkins, 2003, pp. 1093–1101.
11. Schulz M, Schmoldt A.: Therapeutic and toxic blood concentrations of more than 800 drugs and other xenobiotics. Pharmazie 2003; 58 : 447–474.
12. Sternbach H.: The serotonin syndrome. Am J Psychiatry 1991; 148 : 705–713.
13. Tang SW, Helmeste D.: Paroxetine. Expert Opin Pharmacother 2008; 9 : 787–794.
14. Vermeulen T.: Distribution of paroxetine in three postmortem cases. J Anal Toxicol 1998; 22 : 541–544.
15. Winek CL, Wahba WW, Winek CL Jr, Balzer TW.: Drug and chemical blood-level data 2001. Forensic Sci Int 2001; 122 : 107–123.
Štítky
Patologie Soudní lékařství Toxikologie
Článek vyšel v časopiseSoudní lékařství

2010 Číslo 1-
Všechny články tohoto čísla
- 88. Jahrestagung der Deutschen Gesellschaft für Rechtsmedizin
- Pitevní nález otravy selektivním inhibitorem zpětného vychytávání serotoninu (paroxetin)
- Dvadcať rokov Osteuropaverein Rechtsmedizin
- Zvracanie ako príčina smrteľnej nehody potápača z povolania
- Mezirepubliková česko – slovenská studie korelace výsledků dechových analyzátorů a výsledků laboratorní analýzy při zjišťování hladiny alkoholu v krvi
- Soudní lékařství
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Mezirepubliková česko – slovenská studie korelace výsledků dechových analyzátorů a výsledků laboratorní analýzy při zjišťování hladiny alkoholu v krvi
- Pitevní nález otravy selektivním inhibitorem zpětného vychytávání serotoninu (paroxetin)
- Zvracanie ako príčina smrteľnej nehody potápača z povolania
- Dvadcať rokov Osteuropaverein Rechtsmedizin
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



